Asymptomatic Bacteriuria To Treat or Not to Treat
Asymptomatic Bacteriuria: To Treat or Not to Treat Amy Robertson, Pharm. D PGY-1 Pharmacy Resident – UAMS NW
Disclosure and Conflict of Interest • I have no relevant financial or nonfinancial relationships or conflicts of interest to disclose. 2
Objectives • Describe appropriate management of asymptomatic bacteriuria in various patient populations • Identify risks associated with inappropriate treatment of asymptomatic bacteriuria • Understand the evidence supporting the recommendation not to treat asymptomatic bacteriuria in certain patient populations 3
Guidelines • “Infectious Diseases Society of America Guidelines for the Diagnosis and Treatment of Asymptomatic Bacteriuria in Adults” Update in progress Projected publication in Spring 2017 4
Definitions • Asymptomatic bacteriuria (ASB) – isolation of a specified quantitative count of bacteria in appropriately collected urine specimens obtained from a person without symptoms or signs referable to urinary infection • Acute uncomplicated urinary tract infection (UTI) – symptomatic bladder infection characterized by frequency, urgency, dysuria, or suprapubic pain in women with a normal genitourinary (GU) tract • Complicated urinary tract infection – symptomatic urinary infection in individuals with functional or structural abnormalities of the GU tract; may involve either the bladder or kidneys • Acute non-obstructive pyelonephritis – renal infection characterized by costovertebral angle pain and tenderness, often with fever 5
Definitions Continued • Relapse – recurrent UTI after therapy resulting from persistence of the pre-therapy isolate in the urinary tract • Reinfection – recurrent UTI with an organism originating from outside of the urinary tract, either a new bacterial strain or strain previously isolated that persisted in the colonizing flora • Pyuria – presence of increased numbers of polymorphonuclear leukocytes in the urine; evidence of inflammatory response in the urinary tract 6
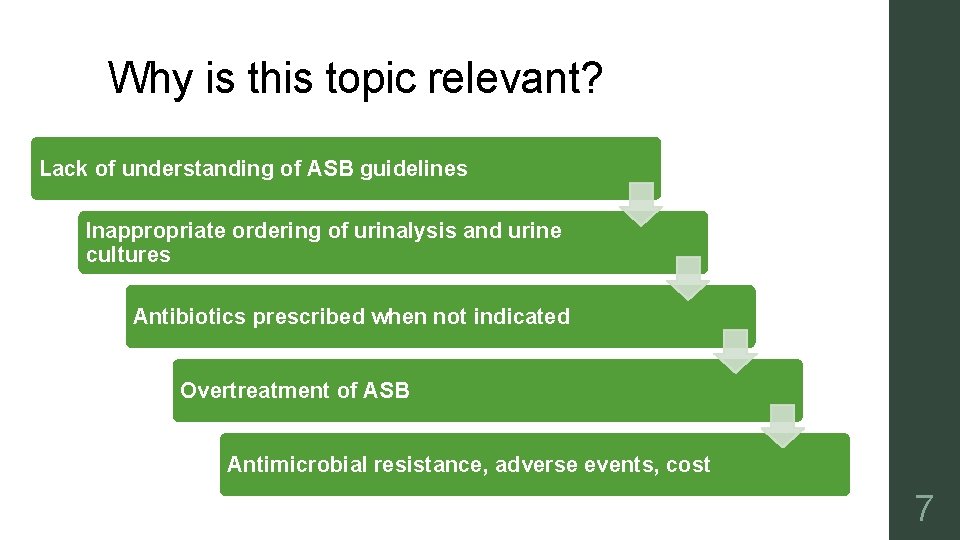
Why is this topic relevant? Lack of understanding of ASB guidelines Inappropriate ordering of urinalysis and urine cultures Antibiotics prescribed when not indicated Overtreatment of ASB Antimicrobial resistance, adverse events, cost 7

Diagnosis • Asymptomatic Women Two consecutive voided urine specimens with: Isolation of the same bacterial strain AND ≥ 105 cfu/m. L • Asymptomatic Men Single voided urine specimen (clean-catch) with: Isolation of 1 bacterial species AND ≥ 105 cfu/m. L • Catheterized Women or Men Single voided urine specimen with: Isolation of 1 bacterial species AND ≥ 102 cfu/m. L 8
ASB versus UTI Bacteriuria Urinary Tract Infection 9
ASB versus UTI Bacteriuria Symptoms Urinary Tract Infection Frequency Urgency Dysuria Suprapubic pain 10
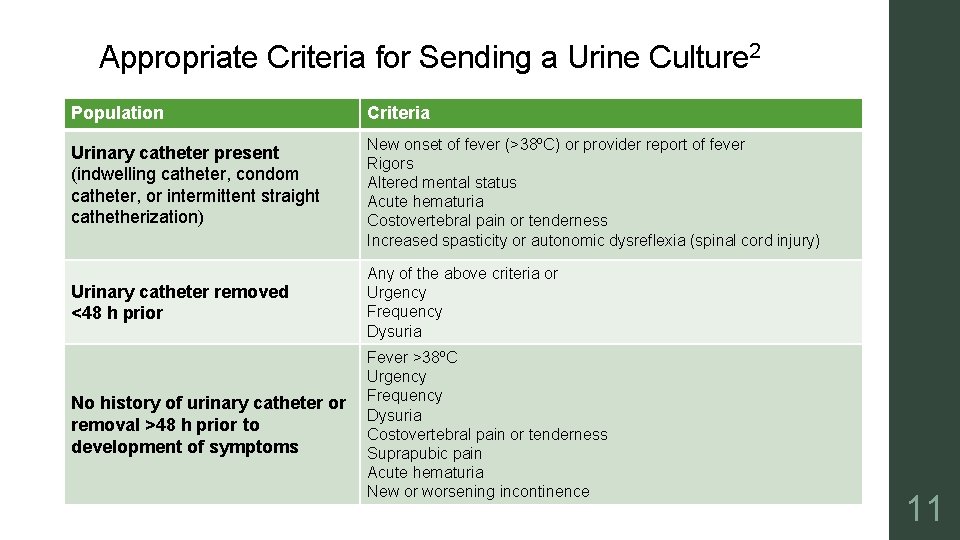
Appropriate Criteria for Sending a Urine Culture 2 Population Criteria Urinary catheter present (indwelling catheter, condom catheter, or intermittent straight cathetherization) New onset of fever (>38ºC) or provider report of fever Rigors Altered mental status Acute hematuria Costovertebral pain or tenderness Increased spasticity or autonomic dysreflexia (spinal cord injury) Urinary catheter removed <48 h prior Any of the above criteria or Urgency Frequency Dysuria No history of urinary catheter or removal >48 h prior to development of symptoms Fever >38ºC Urgency Frequency Dysuria Costovertebral pain or tenderness Suprapubic pain Acute hematuria New or worsening incontinence 11
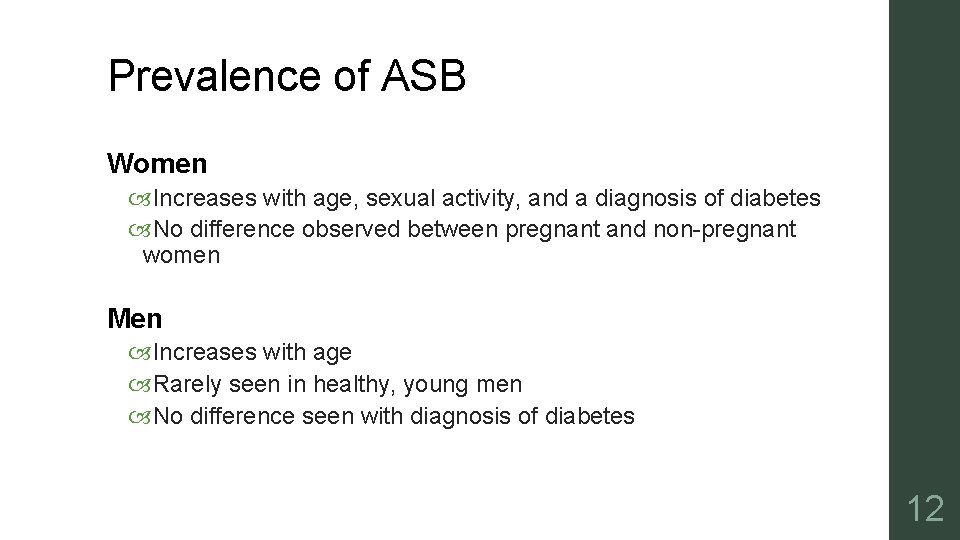
Prevalence of ASB Women Increases with age, sexual activity, and a diagnosis of diabetes No difference observed between pregnant and non-pregnant women Men Increases with age Rarely seen in healthy, young men No difference seen with diagnosis of diabetes 12
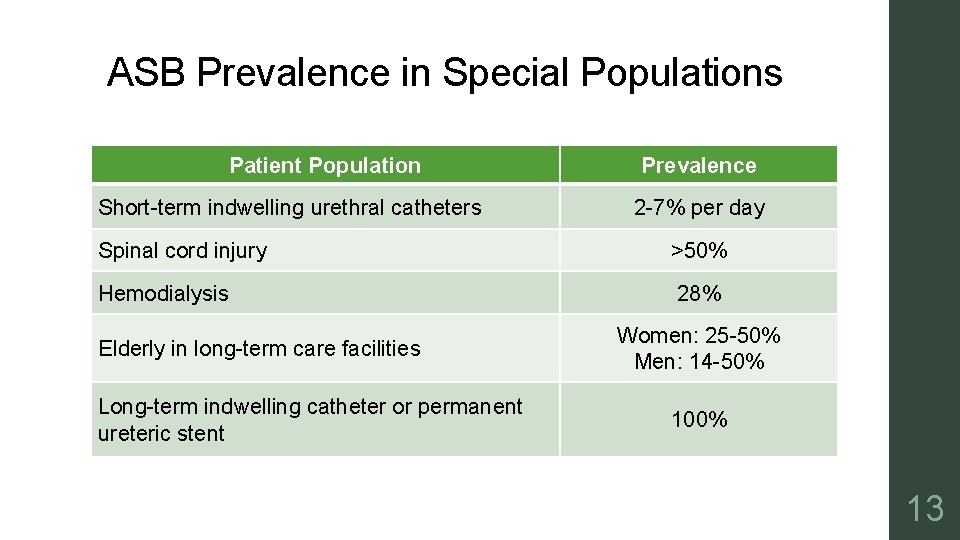
ASB Prevalence in Special Populations Patient Population Short-term indwelling urethral catheters Prevalence 2 -7% per day Spinal cord injury >50% Hemodialysis 28% Elderly in long-term care facilities Long-term indwelling catheter or permanent ureteric stent Women: 25 -50% Men: 14 -50% 100% 13
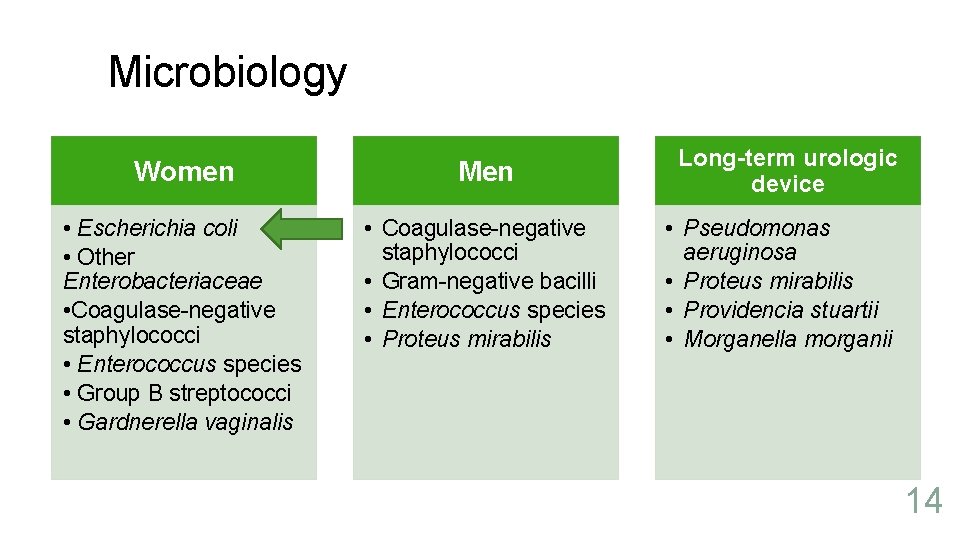
Microbiology Women Men • Escherichia coli • Other Enterobacteriaceae • Coagulase-negative staphylococci • Enterococcus species • Group B streptococci • Gardnerella vaginalis • Coagulase-negative staphylococci • Gram-negative bacilli • Enterococcus species • Proteus mirabilis Long-term urologic device • Pseudomonas aeruginosa • Proteus mirabilis • Providencia stuartii • Morganella morganii 14
To Treat or Not to Treat? 15
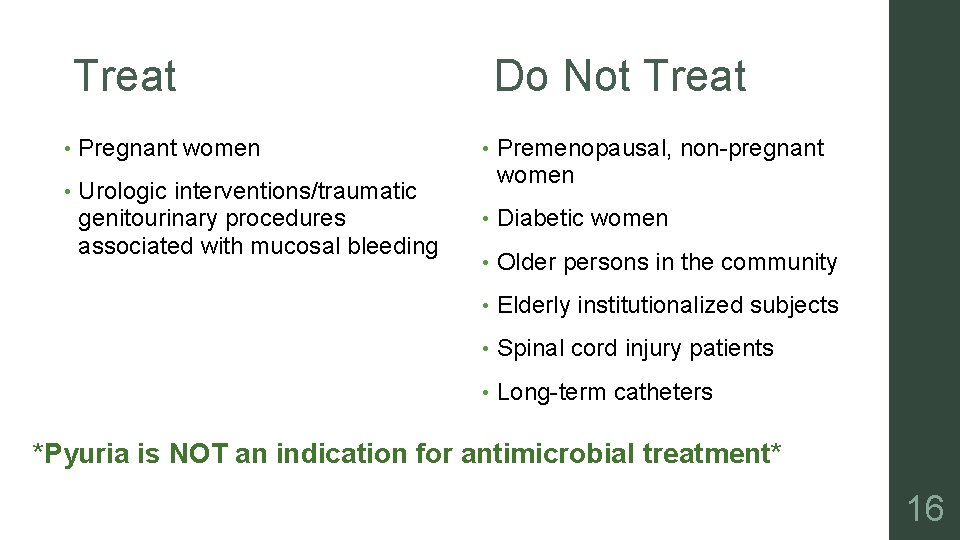
Treat Do Not Treat • Pregnant women • • Urologic interventions/traumatic genitourinary procedures associated with mucosal bleeding Premenopausal, non-pregnant women • Diabetic women • Older persons in the community • Elderly institutionalized subjects • Spinal cord injury patients • Long-term catheters *Pyuria is NOT an indication for antimicrobial treatment* 16
Treatment Populations 17
Pregnant Women • Why? 20 to 30 -fold increased risk of pyelonephritis Increased risk of premature delivery of infants with low birth weight • Screening Urine culture at least once in early pregnancy Must test for cure once treated for ASB Periodic screening for recurrent bacteriuria following antibiotic therapy No recommendation on repeated screening of culture-negative women • Treatment If urine culture is positive give antibiotics Optimal antibiotic duration has not been determined May consider 3 -7 days 18
Urologic Interventions • Why? Higher rate of post-procedure bacteremia and sepsis Antibiotics prevent complications of bacteriuria • Screening Prior to transurethral resection of the prostate is recommended Prior to other urologic procedures for which mucosal bleeding is anticipated • Treatment Initiate antibiotics shortly before the procedure Antibiotics should not be continued after the procedure Exception: indwelling catheter remains in place 19
Non-treatment Populations 20
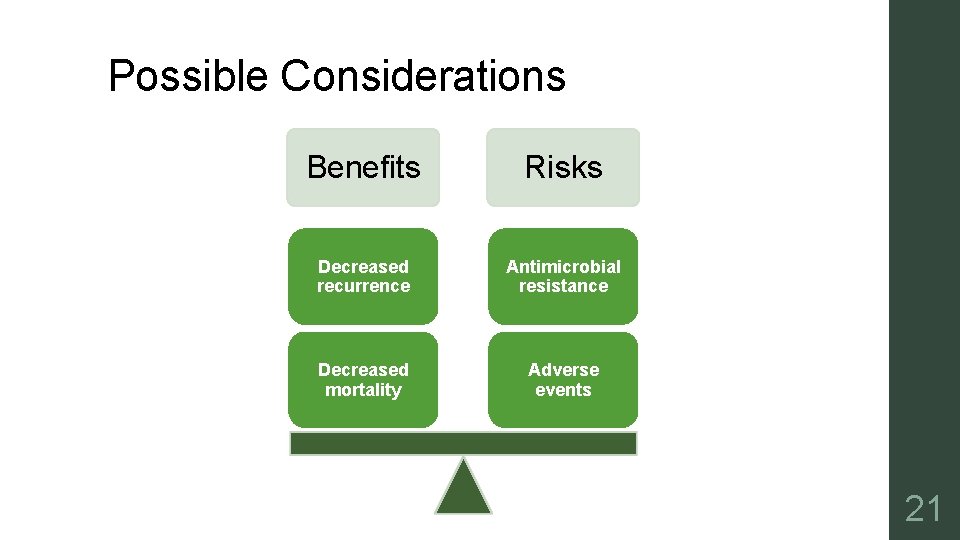
Possible Considerations Benefits Risks Decreased recurrence Antimicrobial resistance Decreased mortality Adverse events 21
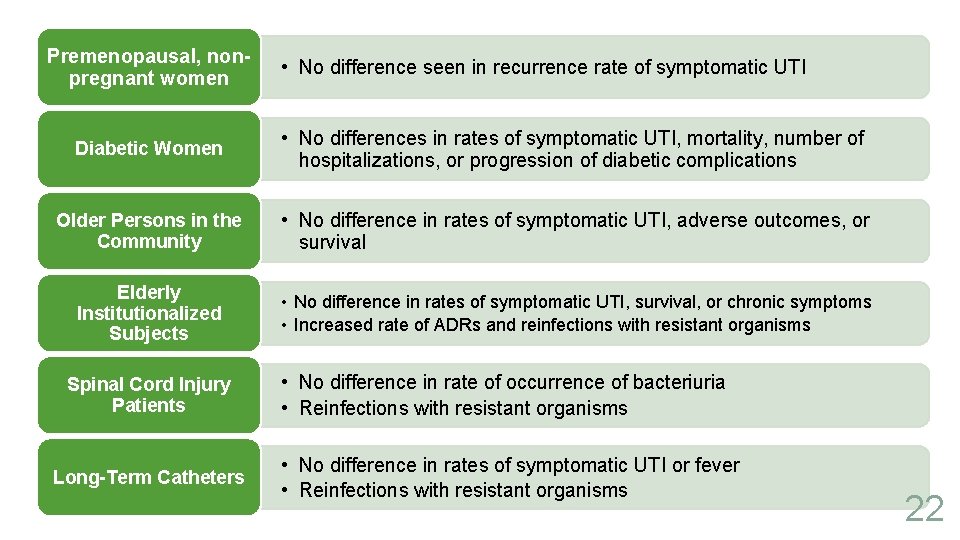
Premenopausal, nonpregnant women • No difference seen in recurrence rate of symptomatic UTI Diabetic Women • No differences in rates of symptomatic UTI, mortality, number of hospitalizations, or progression of diabetic complications Older Persons in the Community • No difference in rates of symptomatic UTI, adverse outcomes, or survival Elderly Institutionalized Subjects • No difference in rates of symptomatic UTI, survival, or chronic symptoms • Increased rate of ADRs and reinfections with resistant organisms Spinal Cord Injury Patients Long-Term Catheters • No difference in rate of occurrence of bacteriuria • Reinfections with resistant organisms • No difference in rates of symptomatic UTI or fever • Reinfections with resistant organisms 22
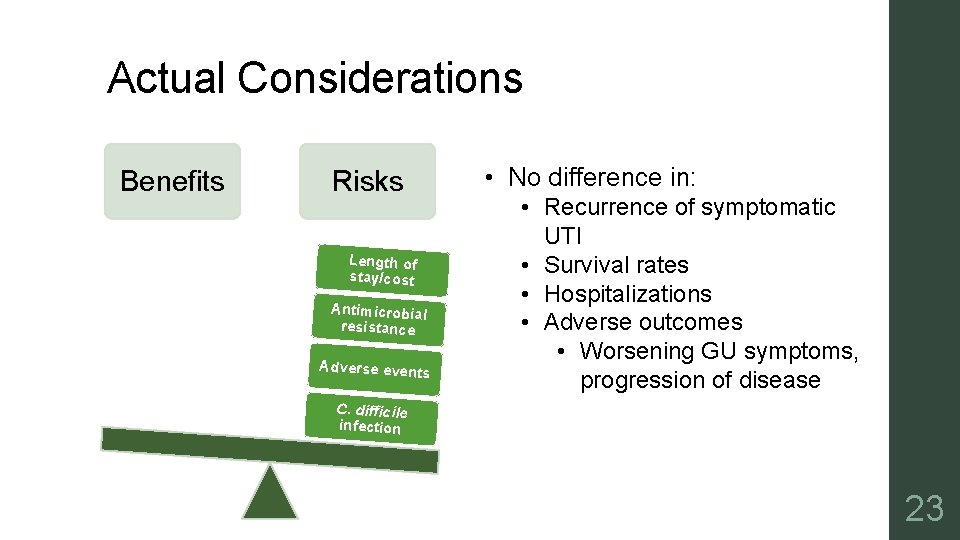
Actual Considerations Benefits Risks Length of stay/cost Antimicrobial resistance Adverse events • No difference in: • Recurrence of symptomatic UTI • Survival rates • Hospitalizations • Adverse outcomes • Worsening GU symptoms, progression of disease C. difficile infection 23
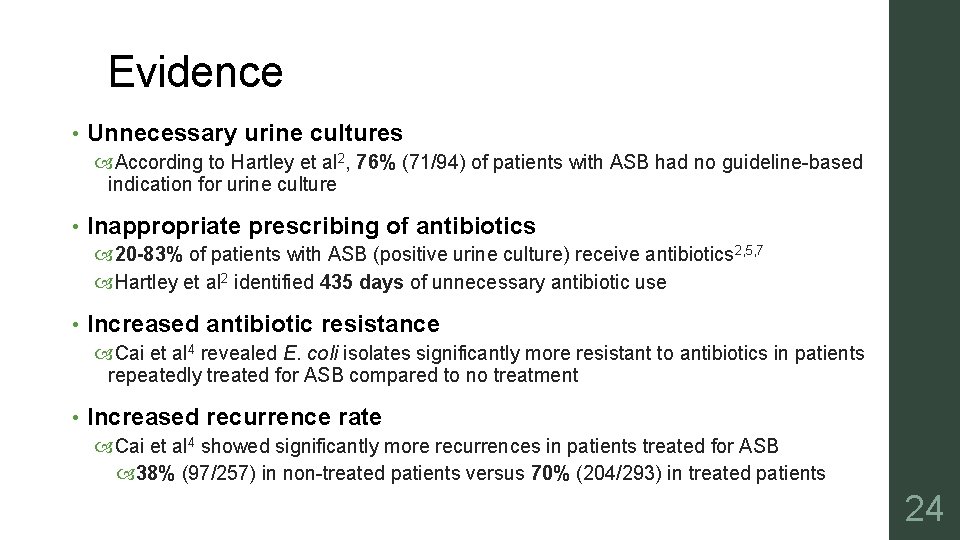
Evidence • Unnecessary urine cultures According to Hartley et al 2, 76% (71/94) of patients with ASB had no guideline-based indication for urine culture • Inappropriate prescribing of antibiotics 20 -83% of patients with ASB (positive urine culture) receive antibiotics 2, 5, 7 Hartley et al 2 identified 435 days of unnecessary antibiotic use • Increased antibiotic resistance Cai et al 4 revealed E. coli isolates significantly more resistant to antibiotics in patients repeatedly treated for ASB compared to no treatment • Increased recurrence rate Cai et al 4 showed significantly more recurrences in patients treated for ASB 38% (97/257) in non-treated patients versus 70% (204/293) in treated patients 24
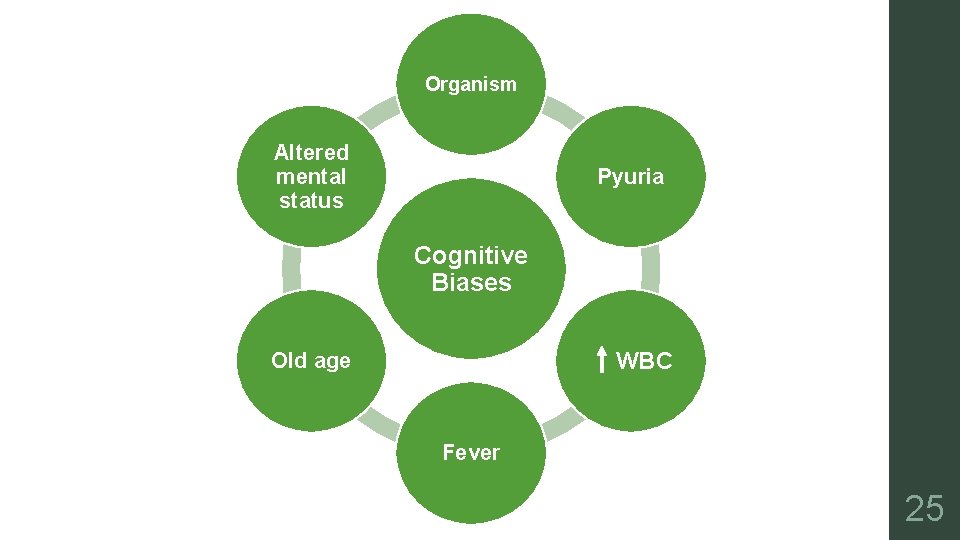
Organism Altered mental status Pyuria Cognitive Biases WBC Old age Fever 25
What needs to be done? • “Multimodal interventions are needed to improve antimicrobial use” 2 • Possible mechanisms 2 for decreasing inappropriate treatment of ASB include: Education Audit and feedback Computer-based reminders Antibiotic “timeouts” • Multiple studies have shown improvements in prescribing practices after implementation of various interventions • Grigoryan et al 3 administered a pre- and post-intervention survey that revealed: Significant increase in knowledge scores Decreased utilization of inaccurate prescribing cues 26
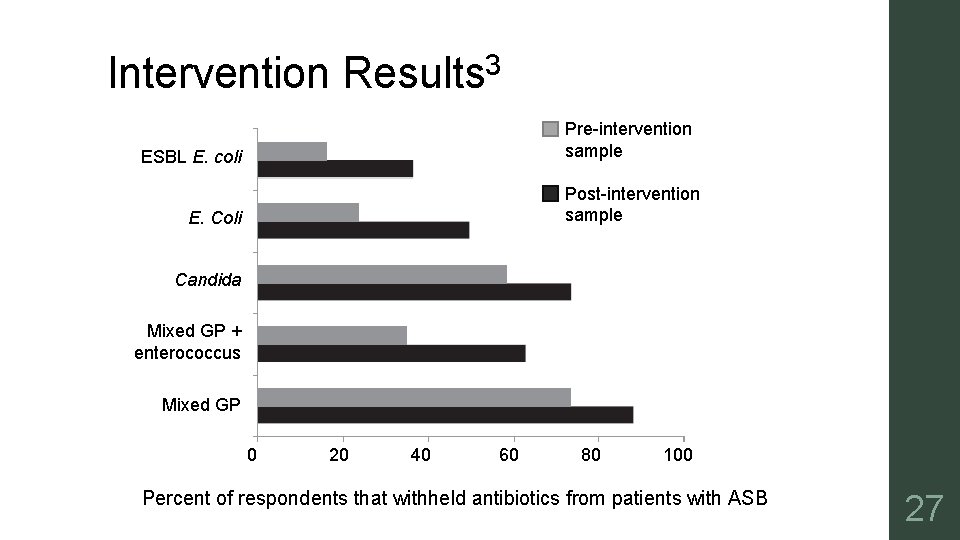
Intervention Results 3 Pre-intervention sample ESBL E. coli Post-intervention sample E. Coli Candida Mixed GP + enterococcus Mixed GP 0 20 40 60 80 100 Percent of respondents that withheld antibiotics from patients with ASB 27
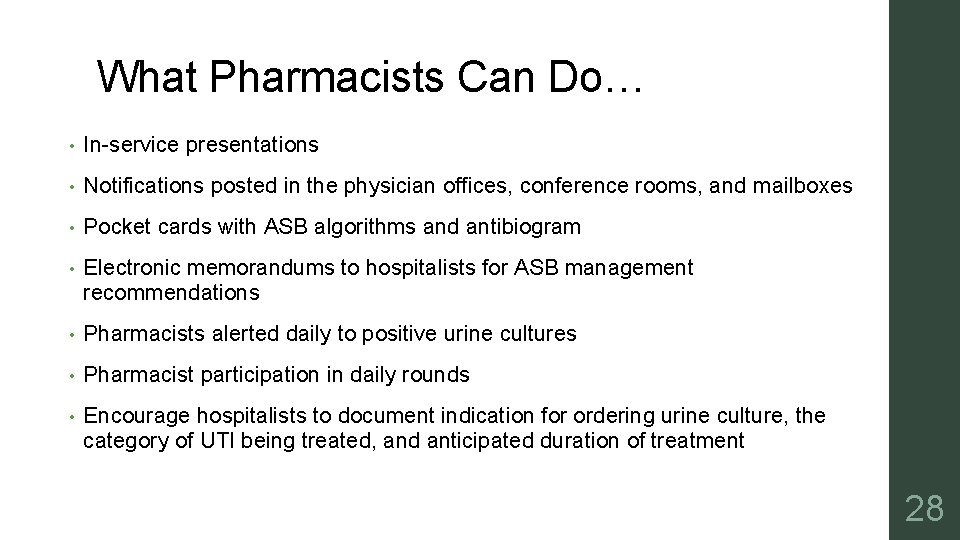
What Pharmacists Can Do… • In-service presentations • Notifications posted in the physician offices, conference rooms, and mailboxes • Pocket cards with ASB algorithms and antibiogram • Electronic memorandums to hospitalists for ASB management recommendations • Pharmacists alerted daily to positive urine cultures • Pharmacist participation in daily rounds • Encourage hospitalists to document indication for ordering urine culture, the category of UTI being treated, and anticipated duration of treatment 28
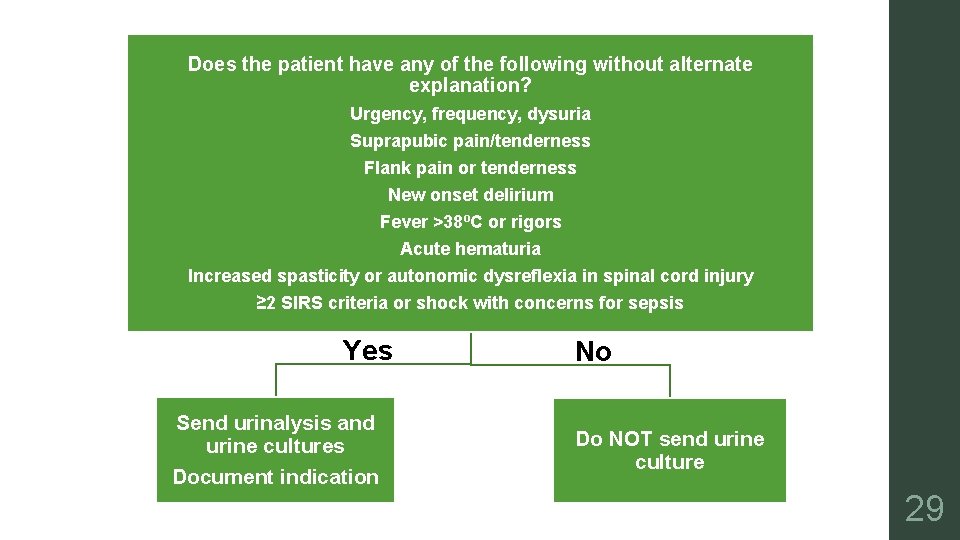
Does the patient have any of the following without alternate explanation? Urgency, frequency, dysuria Suprapubic pain/tenderness Flank pain or tenderness New onset delirium Fever >38ºC or rigors Acute hematuria Increased spasticity or autonomic dysreflexia in spinal cord injury ≥ 2 SIRS criteria or shock with concerns for sepsis Yes Send urinalysis and urine cultures Document indication No Do NOT send urine culture 29
What Pharmacists Can Do… • Multi-modal pharmacist-driven interventions led to a significant decrease in treatment of ASB Hartley SE et al 6 revealed decrease in inappropriate antibiotics from 76. 8% (76/99) to 53. 3% (49/92) Hartley SE et al 6 revealed decrease in antimicrobial days of therapy per patient from 4. 6 (455 days/99 patients) to 3. 3 (305 days/92 patients) Kelley et al 7 revealed decrease in empiric antibiotics from 62% (66/107) to 26% (28/107) 30
ASB Resource • Nebraska Medicine Antimicrobial Stewardship Urinary Tract Infection and Asymptomatic Bacteriuria Guidance http: //www. nebraskamed. com/careers/education-programs/asp/plans 31
Which patient should not receive antimicrobial treatment? A. 28 -year-old asymptomatic pregnant female with urine revealing bacteriuria culture B. 72 -year-old male with urine culture revealing >100, 000 cfu/m. L, new-onset altered mental status, fever, and costovertebral pain C. 20 -year-old female with positive urinalysis, urgency, and dysuria D. 45 -year-old asymptomatic diabetic female with pyuria and urine culture revealing >100, 000 cfu/m. L E. 65 -year-old male with planned transurethral resection of the prostate found to have asymptomatic bacteriuria 32
Conclusions • There are select patient populations that warrant treatment of ASB Pregnant women Urologic interventions • Risks of treating ASB outweigh benefits in other patient populations • Interventions are needed to bridge the gap between recommendations in clinical guidelines and prescribing habits 33
References • 1 Nicolle LE, Bradley S, Colgan R, et al. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis 2005; 40: 643– 654. • 2 Hartley • 3 Grigoryan • 4 Cai • 5 Lee • 6 Hartley • 7 Kelley • 8 Trautner • 9 Irfan • 10 Colgan S, Valley S, Kuhn L, et al. Overtreatment of Asymptomatic Bacteriuria: Identifying Targets for Improvement. Infect Control Hosp Epidemiol 2015; 36(4): 470– 473. doi: 10. 1017/ice. 2014. 73. L, Naik AD, Horwitz D, et al. Survey find improvement in cognitive biases that drive overtreatment of asymptomatic bacteriuria after a successful antimicrobial stewardship intervention. Am J Infect Control 2016. T, Nesi G, Mazzoli S, et al. Asymptomatic Bacteriuria Treatment Is Associated With a Higher Prevalence of Antibiotic Resistant Strains in Women With Urinary Tract Infections. Clin Infect Dis 2015; 61(11): 1655– 61. MJ, Kim M, Kim NH, et al. Why is asymptomatic bacteriuria overtreated? : A tertiary care institutional survey of resident physicians. BMC Infect Dis 2015; 15: 289. doi: 10. 1186/s 12879 -015 -1044 -3. SE, Kuhn L, Valley S, Washer LL, Gandhi T, Meddings J, Robida M, Sabnis S, Chenoweth C, Malani AN, Saint S, Flanders SA. Evaluating a Hospitalist-Based Intervention to Decrease Unnecessary Antimicrobial Use in Patients with Asymptomatic Bacteriuria. Infect Control Hosp Epidemiol 2016; 37: 1044– 1051. D, Aaronson P, Poon E, Mc. Carter YS, Bato B, Jankowski CA. Evaluation of an Antimicrobial Stewardship Approach to Minimize Overuse of Antibiotics in Patients with Asymptomatic Bacteriuria. Infect Control Hosp Epidemiol 2014; 35(2): 193 -195. BW, Grigoryan L, Petersen NJ, et al. Effectiveness of an Antimicrobial Stewardship Approach for Urinary Catheter-Associated Asymptomatic Bacteriuria. JAMA Intern Med 2015; 175(7): 1120 -1127. doi: 10. 1001/jamainternmed. 2015. 1878. N, Brooks A, Mithoowani S, et al. A Controlled Quasi-Experimental Study of an Educational Intervention to Reduce the Unnecessary Use of Antimicrobials For Asymptomatic Bacteriuria. PLo. S ONE 10(7): e 0132071. doi: 10. 1371/journal. pone. 0132071. R, Nicolle LE, Mc. Glone A, Hooton TM. Asymptomatic Bacteriuria in Adults. Am Fam Physician 2006; 74: 985 -90. 34
Questions? 35
Asymptomatic Bacteriuria: To Treat or Not to Treat Amy Robertson, Pharm. D PGY-1 Pharmacy Resident – UAMS NW
- Slides: 36