Asthma Asthma Definition w Reactive airway disease w
![Asthma Drug Therapy w Bronchodilators n -adrenergic agonists (e. g. , albuterol, salbutamol[Ventolin]) l Asthma Drug Therapy w Bronchodilators n -adrenergic agonists (e. g. , albuterol, salbutamol[Ventolin]) l](https://slidetodoc.com/presentation_image/266e2f492e6950c85bcbaef8d8d465b9/image-24.jpg)
- Slides: 48
Asthma
Asthma Definition w Reactive airway disease w Chronic inflammatory lung disease Inflammation causes varying degrees of obstruction in the airways w Asthma is reversible in early stages
Triggers of Asthma n n n n Allergens Exercise Respiratory Infections Nose and Sinus problems Drugs and Food Additives GERD Emotional Stress
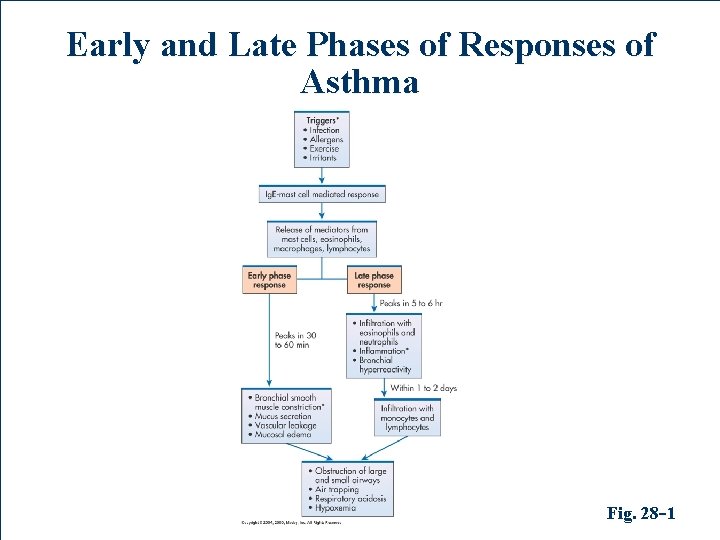
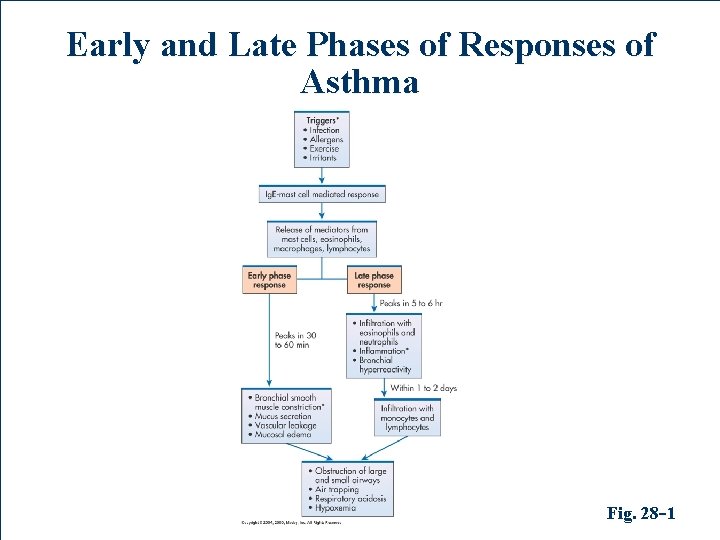
Early and Late Phases of Responses of Asthma Fig. 28 -1
Asthma Pathophysiology w Bronchospasm w Airway inflammation
Asthma Pathophysiology Early-Phase Response n Peaks 30 -60 minutes post exposure, subsides 3090 minutes later n Characterized primarily by bronchospasm n Increased mucous secretion, edema formation, and increased amounts of tenacious sputum n Patient experiences wheezing, cough, chest tightness, and dyspnea
Asthma Pathophysiology Late-Phase Response w Characterized primarily by inflammation w Histamine and other mediators set up a selfsustaining cycle increasing airway reactivity causing hyperresponsiveness to allergens and other stimuli w Increased airway resistance leads to air trapping in alveoli and hyperinflation of the lungs w If airway inflammation is not treated or does not resolve, may lead to irreversible lung damage
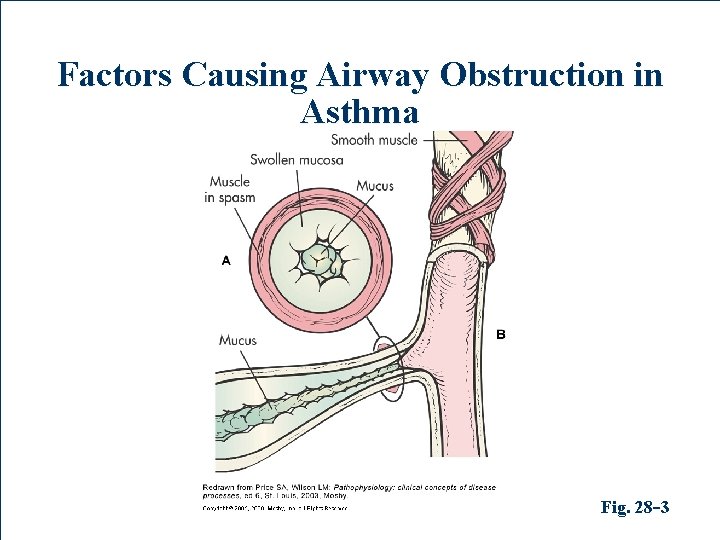
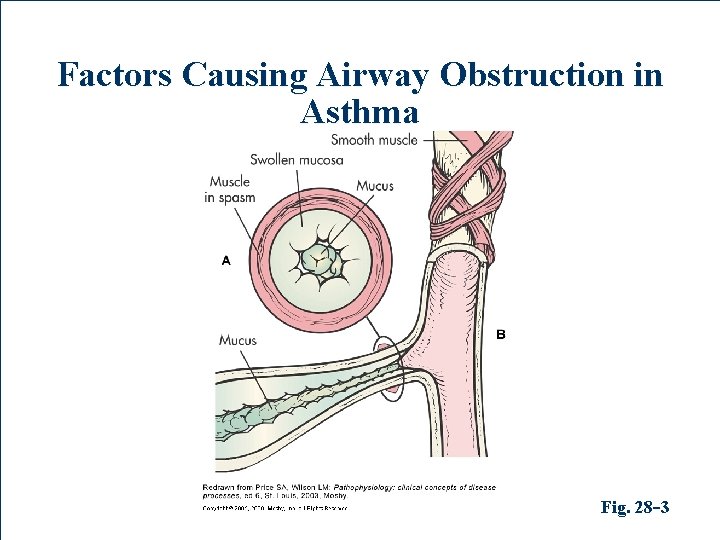
Factors Causing Airway Obstruction in Asthma Fig. 28 -3
Summary of Pathophysiologic Features w Reduction in airway diameter w Increase in airway resistance r/t n n n Mucosal inflammation Constriction of smooth muscle Excess mucus production
Asthma Clinical Manifestations w Unpredictable and variable w Recurrent episodes of wheezing, breathlessness, cough, and tight chest
Asthma Clinical Manifestations w Expiration may be prolonged from a inspiration-expiration ratio of 1: 2 to 1: 3 or 1: 4 w Between attacks may be asymptomatic with normal or near-normal lung function
Asthma Clinical Manifestations w Wheezing is an unreliable sign to gauge severity of attack w Severe attacks can have no audible wheezing due to reduction in airflow w “Silent chest” is ominous sign of impending respiratory failure
Asthma Clinical Manifestations Difficulty with air movement can create a feeling of suffocation n n Patient may feel increasingly anxious Mobilizing secretions may become difficult
Asthma Clinical Manifestations Examination of the patient during an acute attack usually reveals signs of hypoxemia n n n Restlessness Increased anxiety Inappropriate behavior Increased pulse and blood pressure Pulsus paradoxus (drop in systolic BP during inspiratory cycle >10)
Asthma Complications Status asthmaticus n Severe, life-threatening attack refractory to usual treatment where patient poses risk for respiratory failure
Asthma Diagnostic Studies w Detailed history and physical exam w Pulmonary function tests w Peak flow monitoring w Chest x-ray w ABGs
Asthma Diagnostic Studies w Oximetry w Allergy testing w Blood levels of eosinophils w Sputum culture and sensitivity
Asthma Collaborative Care w Education n n Start at time of diagnosis Integrated into every step of clinical care w Self-management n n Tailored to needs of patient Emphasis on evaluating outcome in terms of patient’s perceptions of improvement
Asthma Collaborative Care Acute Asthma Episode n n n O 2 therapy should be started and monitored with pulse oximetry or ABGs in severe cases Inhaled -adrenergic agonists by metered dose using a spacer or nebulizer Corticosteroids indicated if initial response is insufficient
Asthma Collaborative Care Acute Asthma Episode Therapy should continue until patient • is breathing comfortably • wheezing has disappeared • pulmonary function study results are near baseline values
Asthma Collaborative Care Status asthmaticus n n n Most therapeutic measures are the same as for acute Increased frequency & dose of bronchodilators Continuous -adrenergic agonist nebulizer therapy may be given
Asthma Collaborative Care Status asthmaticus n n n IV corticosteroids Continuous monitoring Supplemental O 2 to achieve values of 90% IV fluids are given due to insensible loss of fluids Mechanical ventilation is required if there is no response to treatment
Asthma Drug Therapy w Long-term control medications n Achieve and maintain control of persistent asthma w Quick-relief medications n Treat symptoms of exacerbations
![Asthma Drug Therapy w Bronchodilators n adrenergic agonists e g albuterol salbutamolVentolin l Asthma Drug Therapy w Bronchodilators n -adrenergic agonists (e. g. , albuterol, salbutamol[Ventolin]) l](https://slidetodoc.com/presentation_image/266e2f492e6950c85bcbaef8d8d465b9/image-24.jpg)
Asthma Drug Therapy w Bronchodilators n -adrenergic agonists (e. g. , albuterol, salbutamol[Ventolin]) l Acts in minutes, lasts 4 to 8 hours l Short-term relief of bronchoconstriction l Treatment of choice in acute exacerbations
Asthma Drug Therapy w Bronchodilators l Useful in preventing bronchospasm precipitated by exercise and other stimuli l Overuse may cause rebound bronchospasm l Too frequent use indicates poor asthma control and may mask severity
Asthma Drug Therapy w Bronchodilators (longer acting) l 8 n n – 12 or 24 hr; useful for nocturnal asthma Avoid contact with tongue to decrease side effects Can be used in combination therapy with inhaled corticosteroid
Asthma Drug Therapy Antiinflammatory drugs n Corticosteroids (e. g. , beclomethasone, budesonide) l Suppress inflammatory response l Inhaled form is used in long-term control l Systemic form to control exacerbations and manage persistent asthma
Asthma Drug Therapy Antiinflammatory drugs n Corticosteroids l Do not block immediate response to allergens, irritants, or exercise l Do block late-phase response to subsequent bronchial hyperresponsiveness l Inhibit release of mediators from macrophages and eosinophils
Asthma Drug Therapy Anti-inflammatory drugs n Mast cell stabilizers (e. g. , cromolyn, nedocromil) l Inhibit release of histamine l Inhibit late-phase response l Long-term administration can prevent and reduce bronchial hyper-reactivity l Effective in exercise-induced asthma when used 10 to 20 minutes before exercise
Asthma Drug Therapy w Leukotriene modifiers (e. g. Singulair) n n Leukotriene – potent bronchco-constrictors and may cause airway edema and inflammation Have broncho-dilator and anti-inflammatory effects
Asthma Patient Teaching Related to Drug Therapy Correct administration of drugs is a major factor in determining success in asthma management n n Some persons may have difficulty using an MDI and therefore should use a spacer or nebulizer DPI (dry powder inhaler) requires less manual dexterity and coordination
Asthma Patient Teaching Related to Drug Therapy n n Inhalers should be cleaned by removing dust cap and rinsing with warm water -adrenergic agonists should be taken first if taking in conjunction with corticosteroids
Nursing Management Nursing Diagnoses w Ineffective airway clearance w Anxiety w Ineffective therapeutic regimen management
Nursing Management Planning w Normal or near-normal pulmonary function w Normal activity levels w No recurrent exacerbations of asthma or decreased incidence of asthma attacks w Adequate knowledge to participate in and carry out management
Nursing Management Health Promotion n Teach patient to identify and avoid known triggers l Use dust covers l Use of scarves or masks for cold air l Avoid aspirin or NSAIDs n Desensitization can decrease sensitivity to allergens
Nursing Management Health Promotion n n Prompt diagnosis and treatment of upper respiratory infections and sinusitis may prevent exacerbation Fluid intake of 2 to 3 L every day
Nursing Management Health Promotion Adequate nutrition n Adequate sleep n Take -adrenergic agonist 10 to 20 minutes prior to exercising n
Nursing Management Nursing Implementation Acute Intervention n Monitor respiratory and cardiovascular systems l Lung sounds l Respiratory rate l Pulse l BP
Nursing Management Nursing Implementation l ABGs l Pulse n oximetry l FEV and PEFR l Work of breathing Response to therapy
Nursing Management Nursing Implementation n Nursing Interventions l Administer O 2 l Bronchodilators l Chest physiotherapy l Medications (as ordered) l Ongoing patient monitoring
Nursing Management Nursing Implementation An important goal of nursing is to decrease the patient’s sense of panic n n n Stay with patient Encourage slow breathing using pursed lips for prolonged expiration Position comfortably
Nursing Management Nursing Implementation l The patient must learn about medications and develop self-management strategies l Patient and health care professional must monitor responsiveness to medication l Patient must understand importance of continuing medication when symptoms are not present
Nursing Management Nursing Implementation w Important patient teaching: n n n Seek medical attention for bronchospasm or when severe side effects occur Maintain good nutrition Exercise within limits of tolerance
Nursing Management Nursing Implementation w Important patient teaching (cont. ): n n Patient must learn to measure their peak flow at least daily Asthmatics frequently do not perceive changes in their breathing
Nursing Management Nursing Implementation w Counseling may be indicated to resolve problems w Relaxation therapies may help relax respiratory muscles and decrease respiratory rate
Nursing Management Nursing Implementation Peak Flow Results w Green zone n n Usually 80 -100% of personal best Remain on medications
Nursing Management Nursing Implementation Peak Flow Results w Yellow zone n n n Usually 50 -80% of personal best Indicates caution Something is triggering asthma
Nursing Management Nursing Implementation Peak Flow Results w Red zone n n n 50% or less of personal best Indicates serious problem Definitive action must be taken with health care provider