Assisted Vaginal Birth AVB Learning objectives Classification for

Assisted Vaginal Birth (AVB)
Learning objectives • • • Classification for assisted vaginal birth Indications / contra-indications Preparation and safety criteria for AVB Consent Your training in AVB Where should AVB be undertaken Choosing your instrument to undertake AVB Role of episiotomy Care of mother and baby afterwards © Royal College of Obstetricians and Gynaecologists
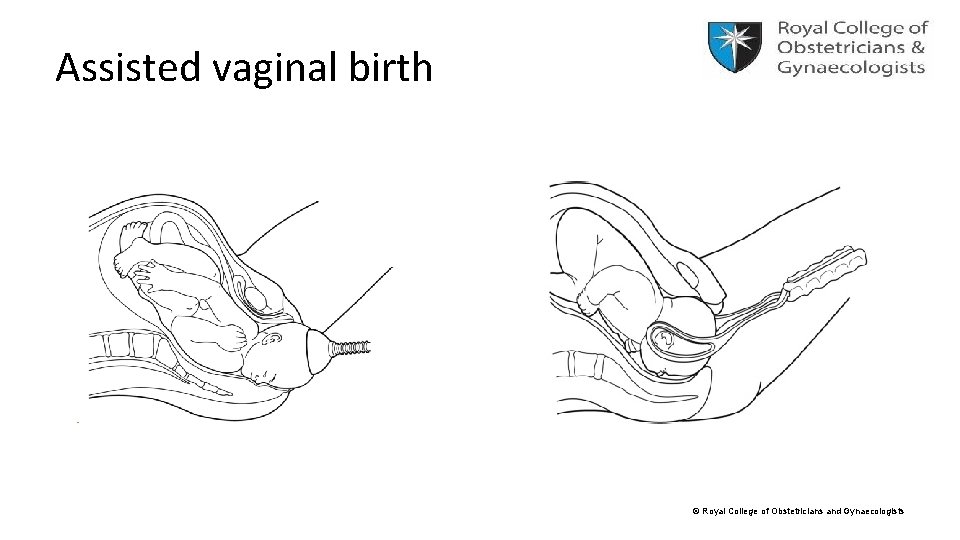
Assisted vaginal birth © Royal College of Obstetricians and Gynaecologists
Classification for assisted vaginal birth • Outlet – Fetal skull has reached perineum • Low – Fetal skull at station +2 cm (below the ischial spines) but not on perineum • Mid – Fetal head is no more than 1/5 th palpable per abdomen – Leading point of skull at station 0 or +1 cm (below the ischial spines) © Royal College of Obstetricians and Gynaecologists
AVB INSTRUMENTS Non-rotational instruments: • Outlet forceps – Wrigley’s forceps • Non-rotational forceps – e. g. Neville-Barnes / Simpson forceps • Ventouse – metal / soft cup / Kiwi Rotational instruments: • Rotational forceps – Kielland forceps • Ventouse – metal / soft cup / Kiwi © Royal College of Obstetricians and Gynaecologists
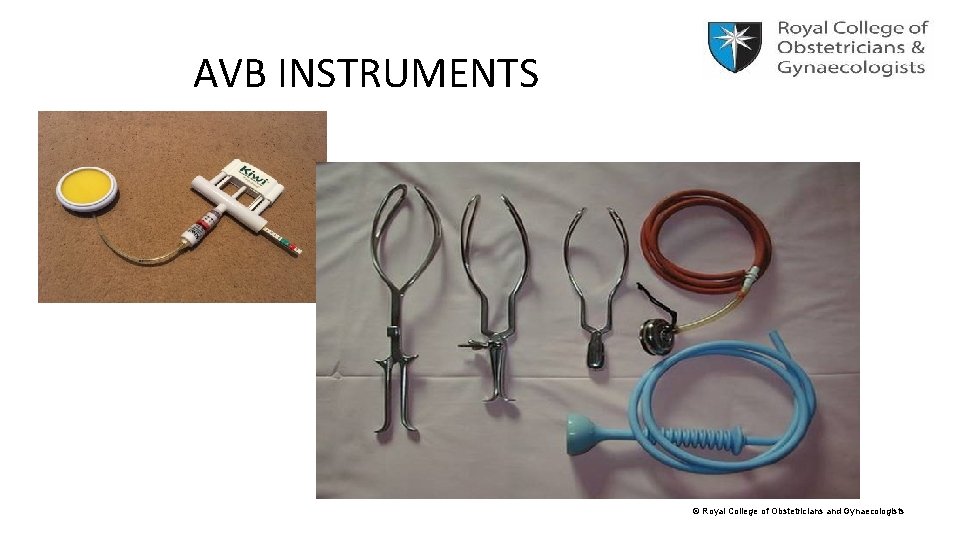
AVB INSTRUMENTS © Royal College of Obstetricians and Gynaecologists
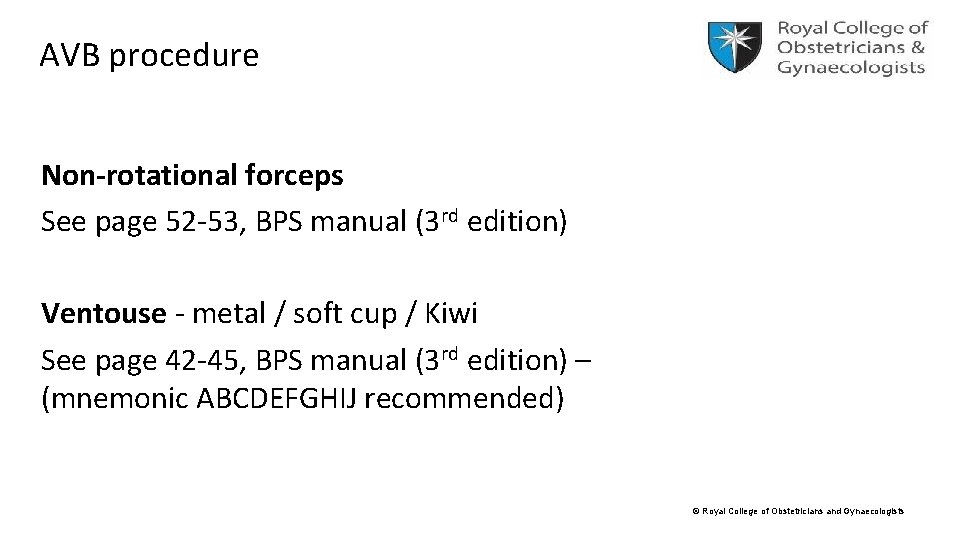
AVB procedure Non-rotational forceps See page 52 -53, BPS manual (3 rd edition) Ventouse - metal / soft cup / Kiwi See page 42 -45, BPS manual (3 rd edition) – (mnemonic ABCDEFGHIJ recommended) © Royal College of Obstetricians and Gynaecologists
Indications / contra-indications Indications for AVB • Fetal - compromise • Maternal – lack of progress; maternal disease e. g. cardiac; cerebral vasc. malformation; myasthenia • Combined fetal and maternal indications (Relative) contra-indications for AVB • Suspected fetal bleeding disorders e. g. allo-immune thrombocytpaenia; male fetus with haemophilia • Predisposition to fracture e. g. OI • Vacuum birth should be avoided < 32 weeks’ and used with caution between 32 -36 weeks’ © Royal College of Obstetricians and Gynaecologists
Safe criteria and preparation for AVB - 1 1) Full abdominal and vaginal examination • • Head 1/ 5 th palpable Cx – fully dilated, membranes ruptured Station at level of ‘spines’ or below Position determined Caput and moulding no more than moderate (or +2) Pelvis ‘adequate’ Role of U/S to assess fetal head position © Royal College of Obstetricians and Gynaecologists
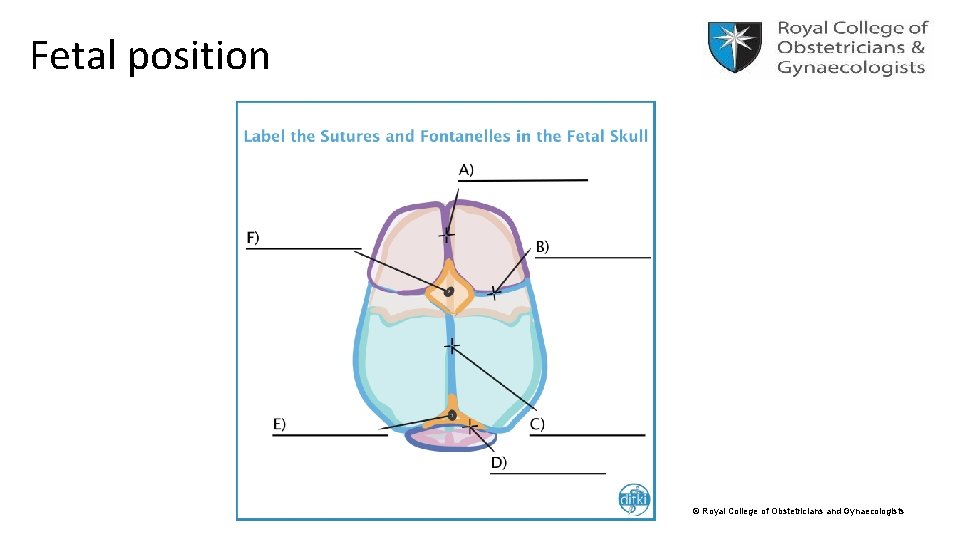
Fetal position © Royal College of Obstetricians and Gynaecologists
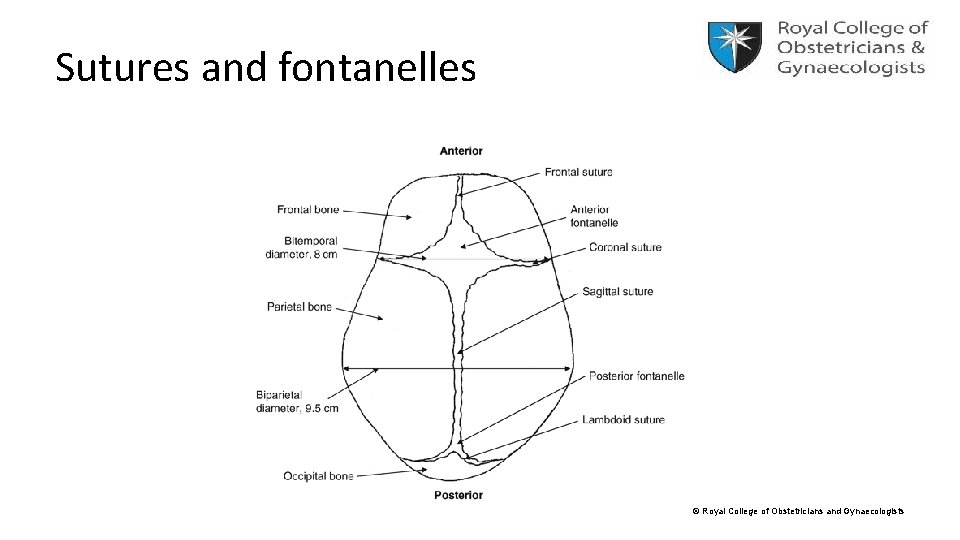
Sutures and fontanelles © Royal College of Obstetricians and Gynaecologists
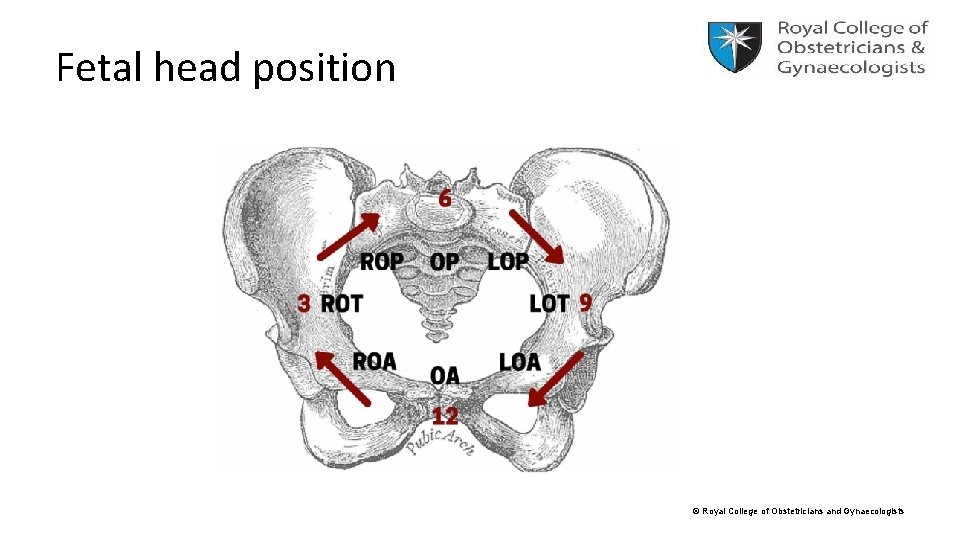
Fetal head position © Royal College of Obstetricians and Gynaecologists
Preparation for AVB - 2 • • • 2) Preparation of mother Explanation and informed consent Appropriate analgesia (regional / pudendal / perineal block) Maternal bladder emptied If present indwelling catheter removed Aseptic technique © Royal College of Obstetricians and Gynaecologists
Preparation for AVB - 3 3) Preparation of staff • AVB performed by, or in presence of, an operator who has knowledge, skills and experience necessary to assess woman, complete the procedure and manage any complications that arise • Adequate facilities • Back-up plan • Anticipation of complications (e. g. shoulder dystocia; PPH) • Personnel trained in neonatal resuscitation © Royal College of Obstetricians and Gynaecologists
A/N information about AVB and Consent • A/N information about AVB especially in first pregnancy or if they have specific restrictions / preferences (signposting RCOG ‘Information for you – AVB’) • Birth room procedures – usually verbal consent • Trial of vaginal delivery; mid-cavity or rotational forceps – written consent © Royal College of Obstetricians and Gynaecologists
Your training in AVB • GTG anchor statement “AVB performed by, or in presence of, an operator who has knowledge, skills and experience necessary to assess woman, complete the procedure and manage any complications that arise” • RCOG GTG recommends trainees achieve expertise in spontaneous vaginal birth prior to commencing training in AVB • As Trainers / Educational Supervisor we must ensure you receive appropriate training in AVB including: – – Theory Simulation Clinical training under direct supervision Assessment of competency © Royal College of Obstetricians and Gynaecologists
Where should AVB be undertaken? • Non-rotational low-pelvic and lift-out AVBs – low probability of failure – in a birth room • AVBs with higher risk failure (‘trial of vaginal delivery’) – in theatre e. g. o mid-pelvic birth o OP position o EFW > 4 kg etc © Royal College of Obstetricians and Gynaecologists
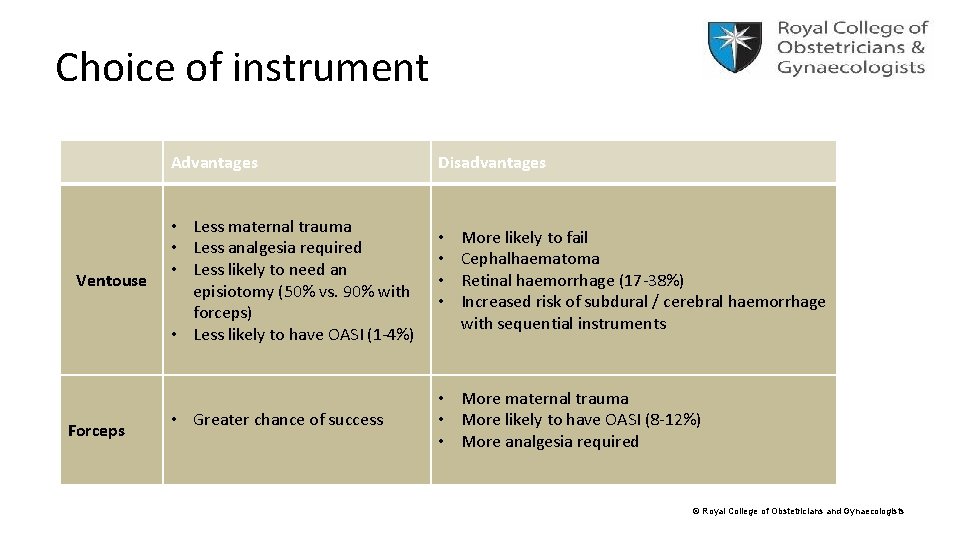
Choice of instrument Advantages Ventouse Forceps • Less maternal trauma • Less analgesia required • Less likely to need an episiotomy (50% vs. 90% with forceps) • Less likely to have OASI (1 -4%) • Greater chance of success Disadvantages • • More likely to fail Cephalhaematoma Retinal haemorrhage (17 -38%) Increased risk of subdural / cerebral haemorrhage with sequential instruments • More maternal trauma • More likely to have OASI (8 -12%) • More analgesia required © Royal College of Obstetricians and Gynaecologists
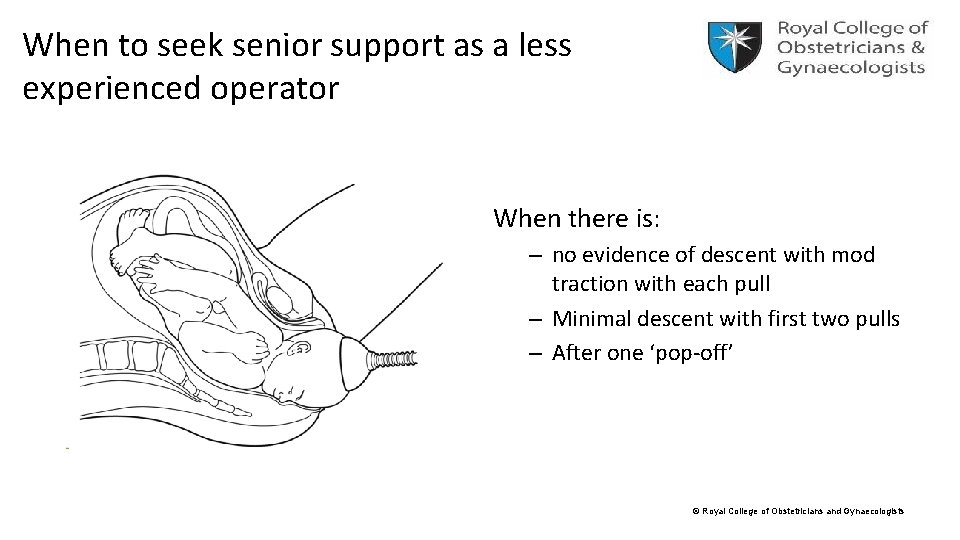
When to seek senior support as a less experienced operator When there is: – no evidence of descent with mod traction with each pull – Minimal descent with first two pulls – After one ‘pop-off’ © Royal College of Obstetricians and Gynaecologists
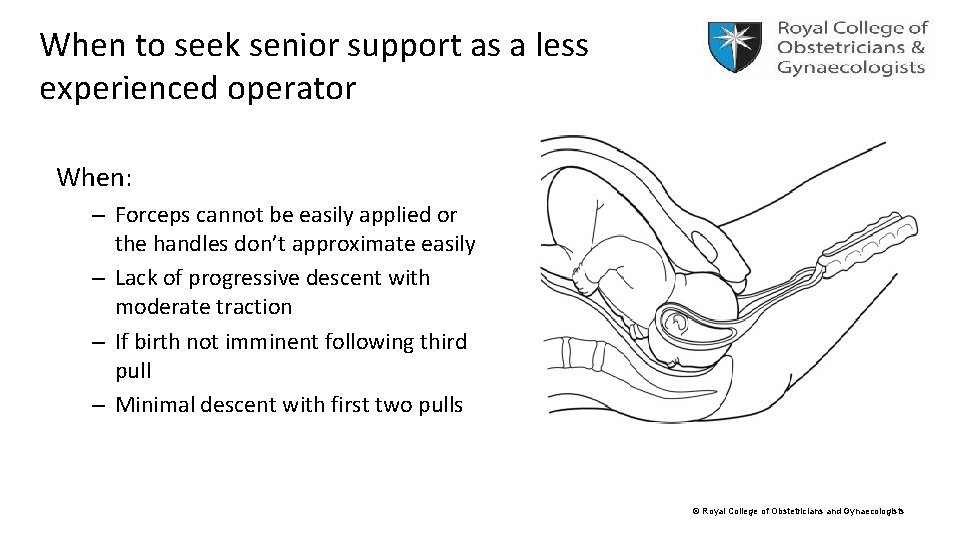
When to seek senior support as a less experienced operator When: – Forceps cannot be easily applied or the handles don’t approximate easily – Lack of progressive descent with moderate traction – If birth not imminent following third pull – Minimal descent with first two pulls © Royal College of Obstetricians and Gynaecologists
Care of mother and baby afterwards • • • Paired cord p. Hs Documentation (standardised proforma as per GTG) Single shot antibiotics Thromboprophylaxis assessment Analgesia Bladder care © Royal College of Obstetricians and Gynaecologists
Summary • We have looked at: o o o o Classification for assisted vaginal birth Indications / contra-indications Preparation and safety criteria for AVB Your training in AVB Where should AVB be undertaken Choosing your instrument to undertake AVB When you should call for help • Now it is time for you to: o gain expertise in spontaneous vaginal births o Train in simulated AVB o Embark on clinical training under direct supervision © Royal College of Obstetricians and Gynaecologists
References • BPS Manual (3 rd edition) – Module 2, page 34 – 45 • Assisted Vaginal Birth RCOG Green-top Guideline No. 26 April 2020 • RCOG “Information for you - Assisted vaginal birth (ventouse or forceps)”published April 2020 • RCOG e-learning - Forceps and ventouse within the Core Knowledge Management of labour and birth tutorials © Royal College of Obstetricians and Gynaecologists
- Slides: 23