Assessment of the Older Adult Utilizing Standardized Tools















- Slides: 48
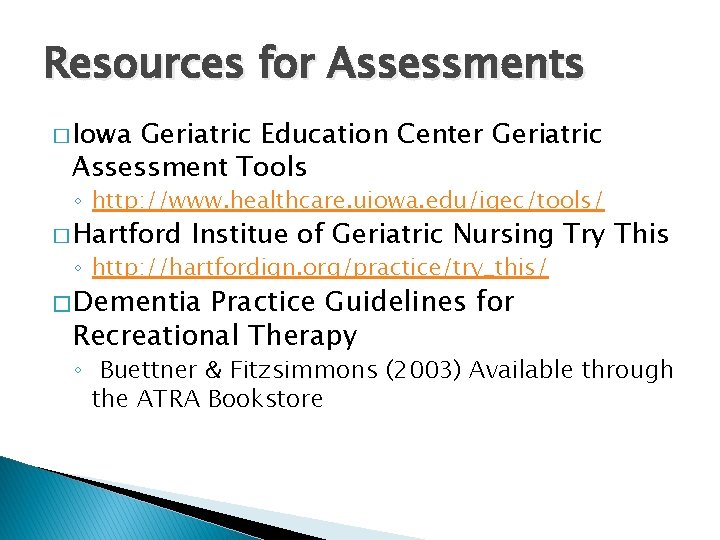
Assessment of the Older Adult: Utilizing Standardized Tools for Recreational Therapy Treatment With Geriatric Clients Jo Lewis, MS/CTRS Megan Janke, Ph. D. , LRT/CTRS
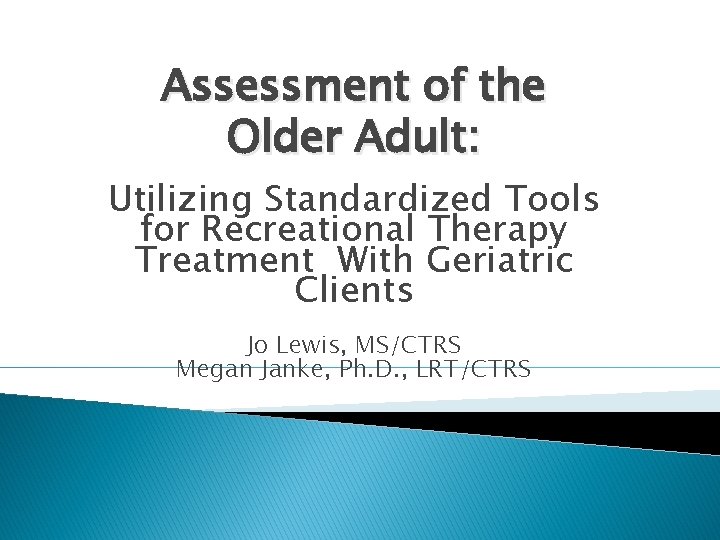
Objectives Upon successful completion of this session, the participant will be able to: � Identify 3 standardized assessment tools that may be utilized in Recreational Therapy treatment with older adults. � Verbalize 2 benefits of utilizing standardized assessments during Recreational Therapy treatment � Utilize internet resources for standardized assessment tools in Recreational Therapy practice with older adults.
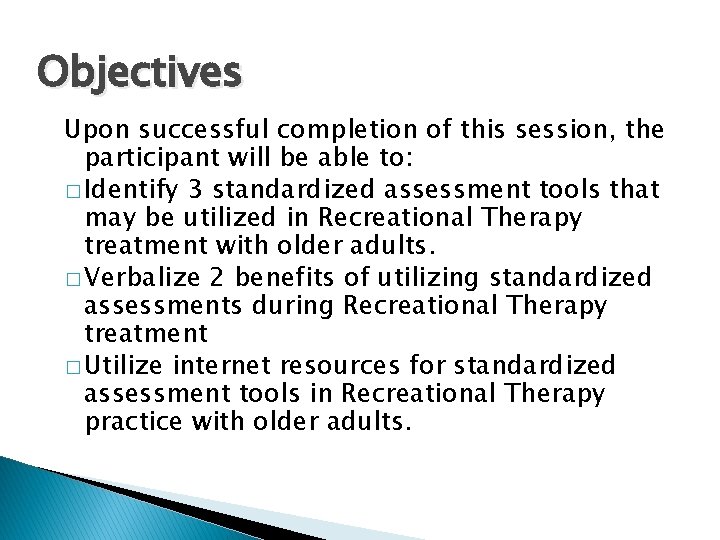
Key Concepts For Assessments � Validity ◦ Does it measure what it is intended to measure? �External �Internal � Reliability ◦ Does it consistently measure what is intended? �Internal Consistency �Inter-rater Reliability �Responsiveness �Can it detect real change when it happens?
Why Use Standardized Assessments? � Measure what you intend to measure � Justification of Services � Accepted across discipline boundaries
Cognitive Scales � Brief Interview for Mental Status � Short Portable Mental Status Questionnaire � Blessed Orientation-Memory-Concentration Test � Global Deterioration Scale � Brief Cognitive Rating Scale � Clock Drawing Test � Montreal Cognitive Assessment (Mo. CA)
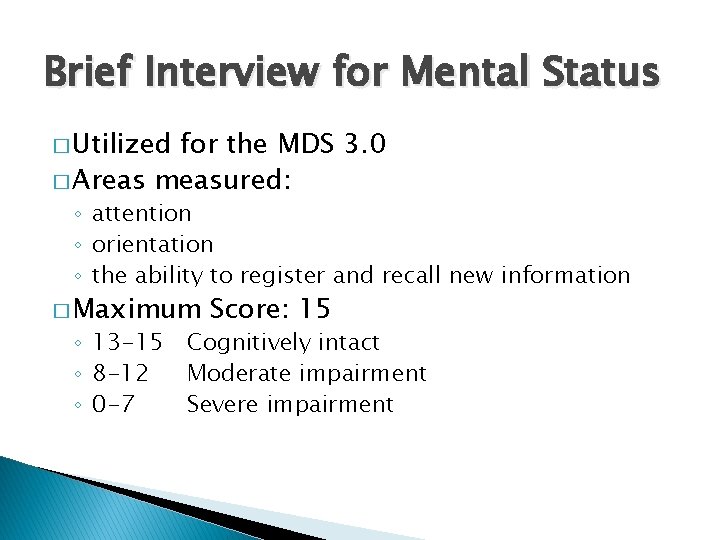
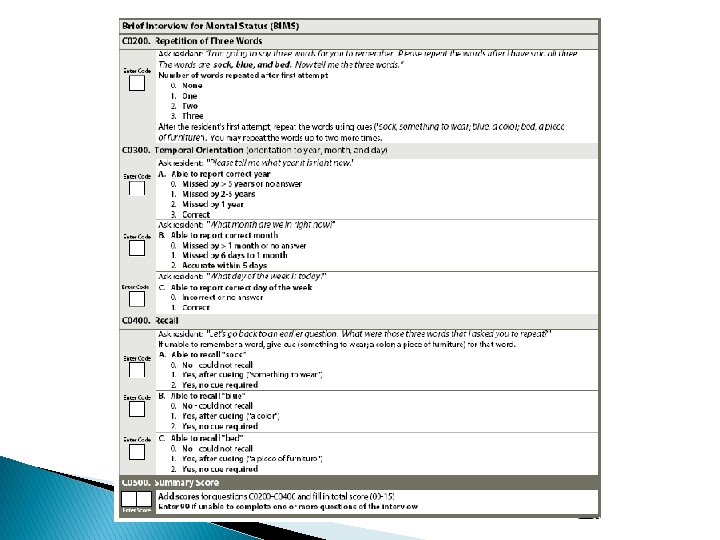
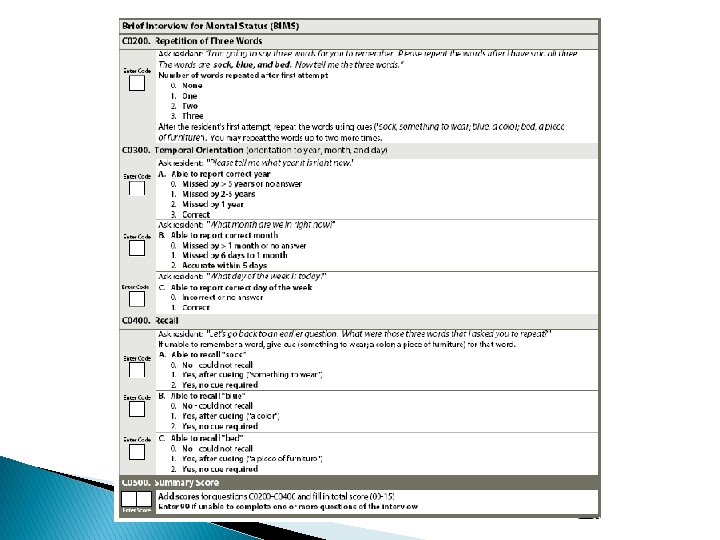
Brief Interview for Mental Status � Utilized for the MDS 3. 0 � Areas measured: ◦ attention ◦ orientation ◦ the ability to register and recall new information � Maximum ◦ 13 -15 ◦ 8 -12 ◦ 0 -7 Score: 15 Cognitively intact Moderate impairment Severe impairment

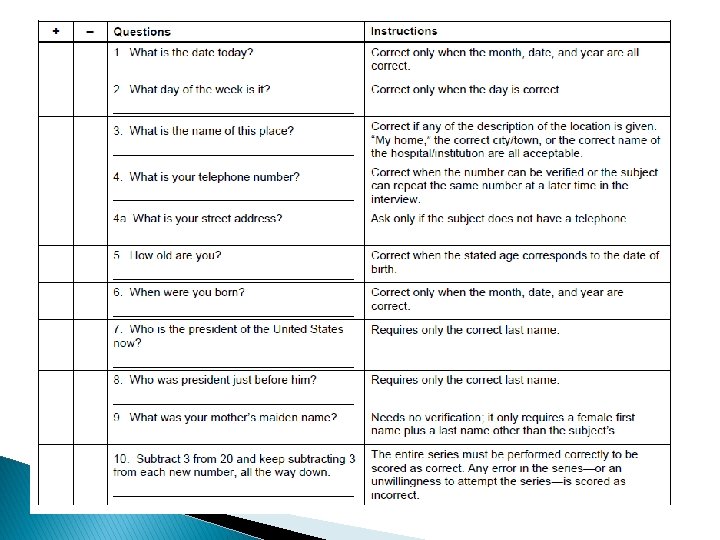
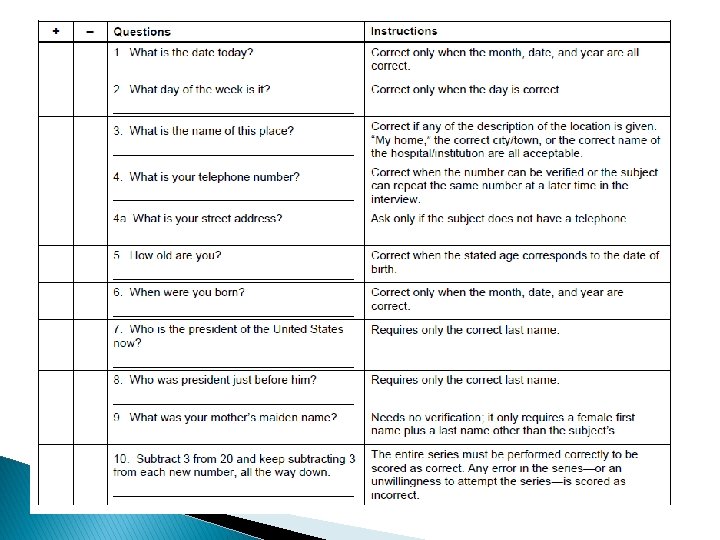
Short Portable Mental Status Questionnaire (SPMSQ) � 10 Items � Maximum Score: 10 ◦ ◦ 0 -2 errors 3 -4 errors 5 -7 errors 8 -10 errors � 5 -10 Intact Mild impairment Moderate impairment Severe impairment minutes to administer
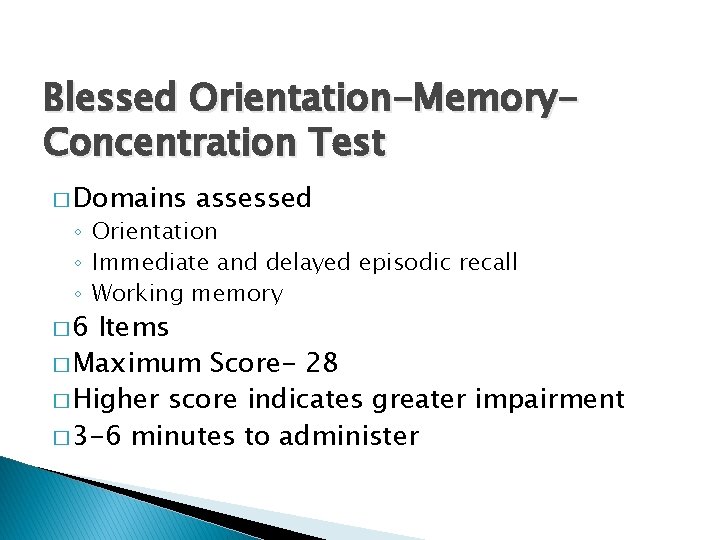
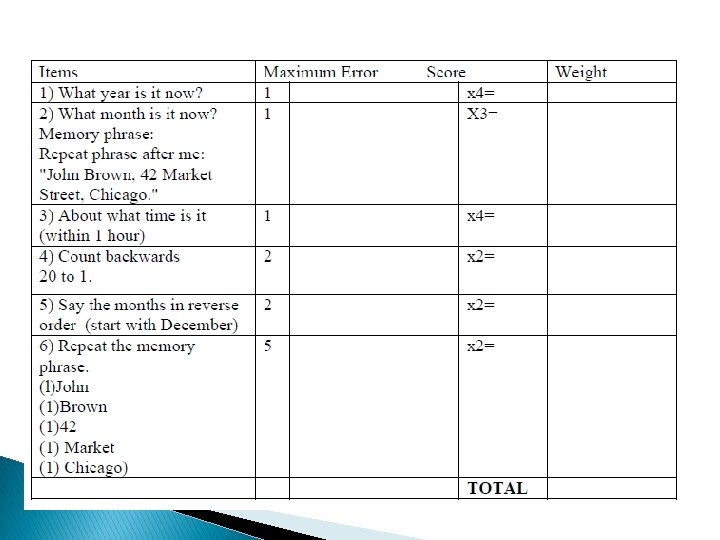
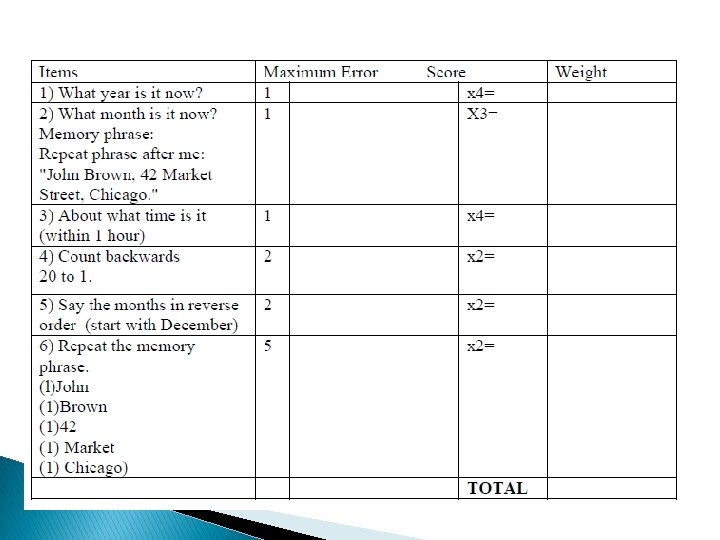
Blessed Orientation-Memory. Concentration Test � Domains assessed ◦ Orientation ◦ Immediate and delayed episodic recall ◦ Working memory � 6 Items � Maximum Score- 28 � Higher score indicates greater impairment � 3 -6 minutes to administer
Global Deterioration Scale � Rating � 1: � 2: � 3: � 4: � 5: � 6: � 7: scale No cognitive impairment Very mild cognitive decline Moderately severe cognitive decline Severe cognitive decline Very severe cognitive decline � Used with Brief Cognitive Rating Scale
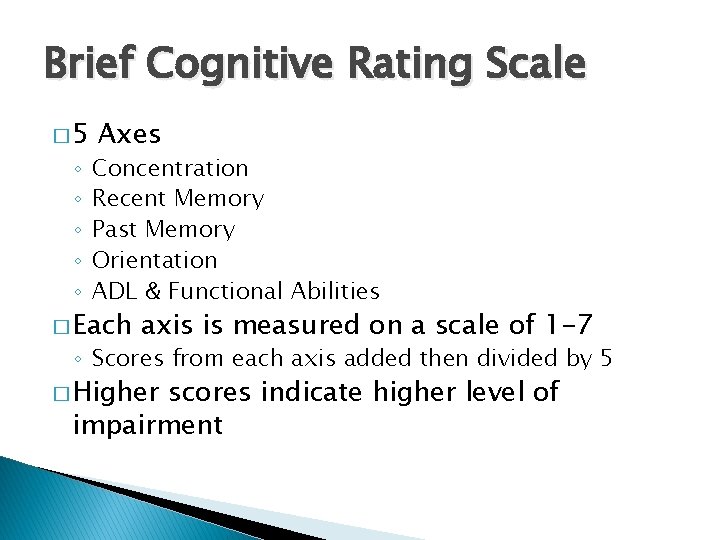
Brief Cognitive Rating Scale � 5 ◦ ◦ ◦ Axes Concentration Recent Memory Past Memory Orientation ADL & Functional Abilities � Each axis is measured on a scale of 1 -7 ◦ Scores from each axis added then divided by 5 � Higher scores indicate higher level of impairment
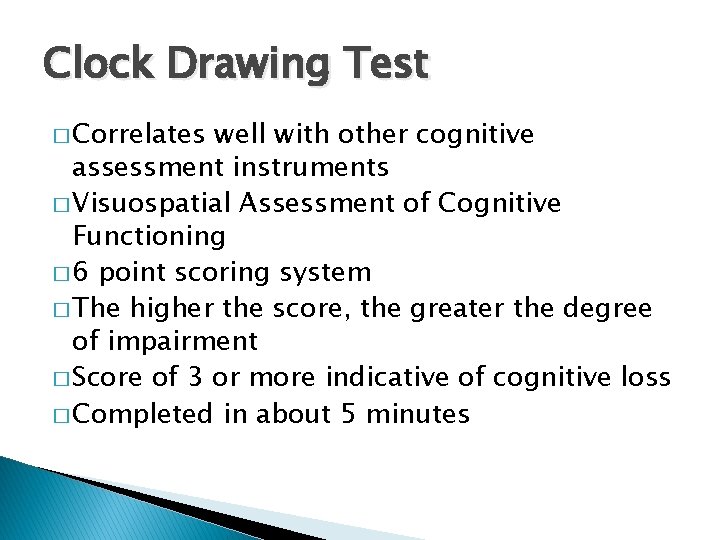
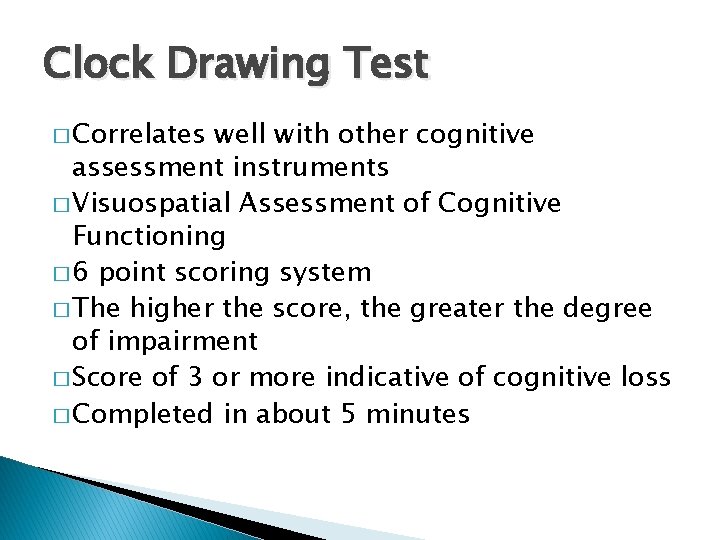
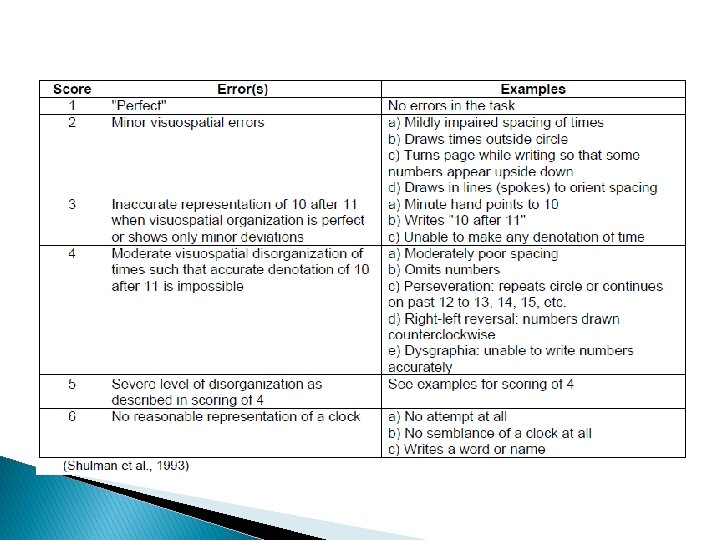
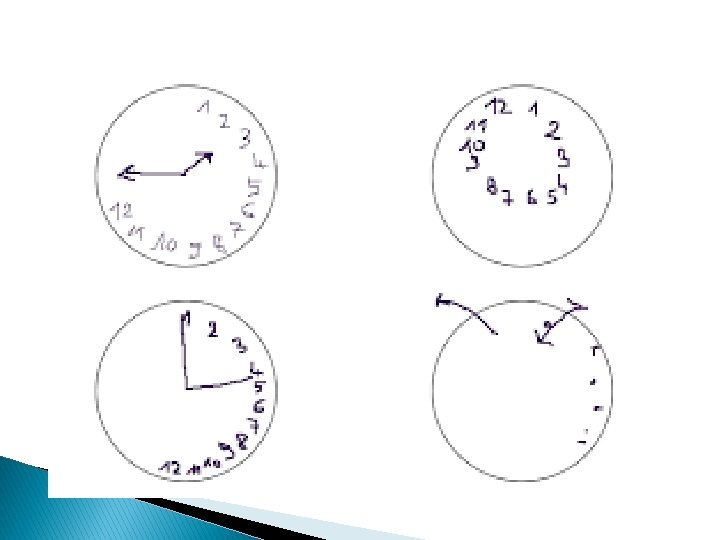
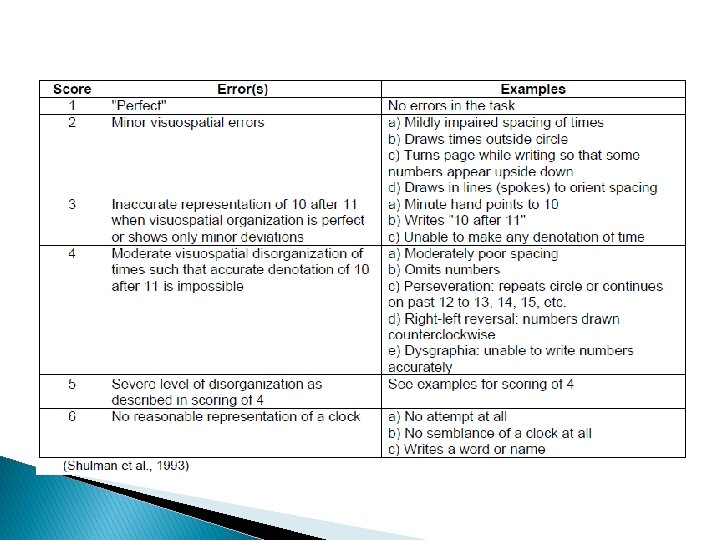
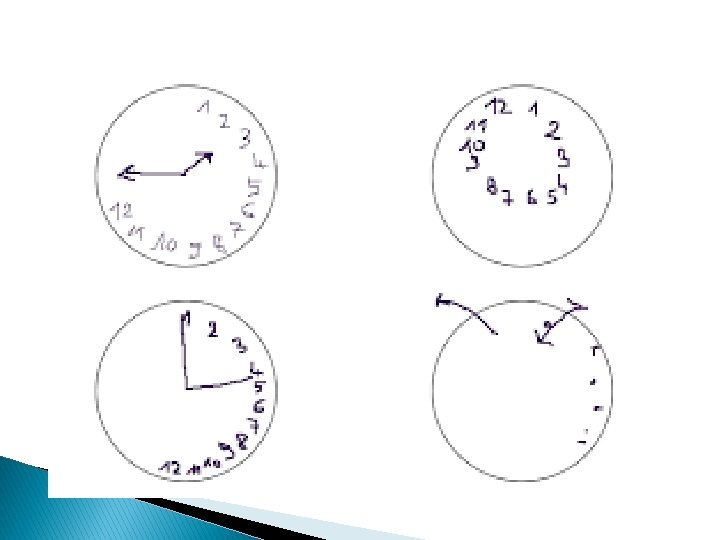
Clock Drawing Test � Correlates well with other cognitive assessment instruments � Visuospatial Assessment of Cognitive Functioning � 6 point scoring system � The higher the score, the greater the degree of impairment � Score of 3 or more indicative of cognitive loss � Completed in about 5 minutes

Montreal Cognitive Assessment (Mo. CA) � Screening tool for mild cognitive dysfunction � Cognitive Domains ◦ ◦ ◦ ◦ Attention and concentration Executive functioning Memory Language Visuoconstructional skills Conceptual thinking Calculations Orientation � 10 Minutes to Administer � Possible score of 30 ◦ 26 or above is considered normal
Physical/ ADL Functioning � Barthel Index � Berg Balance Scale � Katz Index of Independence in Activities of Daily Living � Lawton Instrumental Activities of Daily Living � Tinetti Mobility Scale ◦ Performance-Oriented Assessment of Balance ◦ Performance-Oriented Assessment of Gait � Get-Up & Go Test

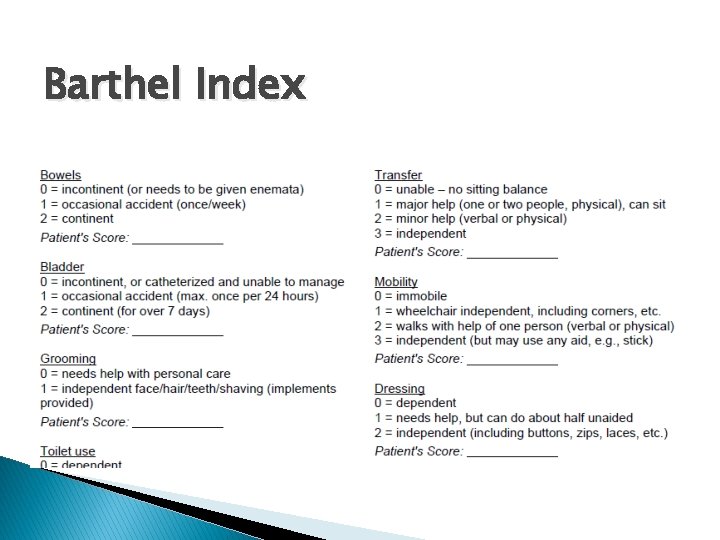
Barthel Index � Self-report ◦ 2 -3 minutes � Trained observation ◦ 10 -15 minutes � 3 point scale for each item � Assesses: �Feeding �Grooming �Bowel & Bladder Continence �Dressing �Toileting �Walking �Stairs �Bathing
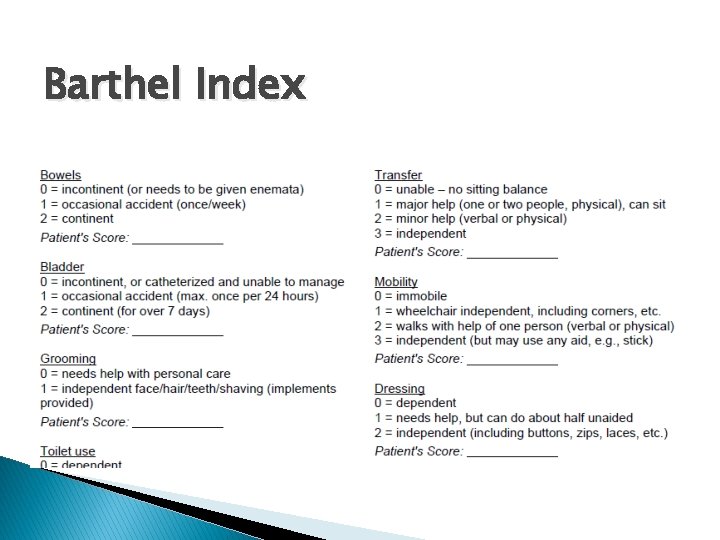
Barthel Index

Katz Index of Independence in Activities of Daily Living � Performance measure ◦ Self-report ◦ Trained observer � Scoring ◦ Letter score from A-G �A= Most independent �G= Most dependent � Bathing � Dressing � Toilet use � Transfer ability � Feed self � Maintenance of bowel & bladder continence
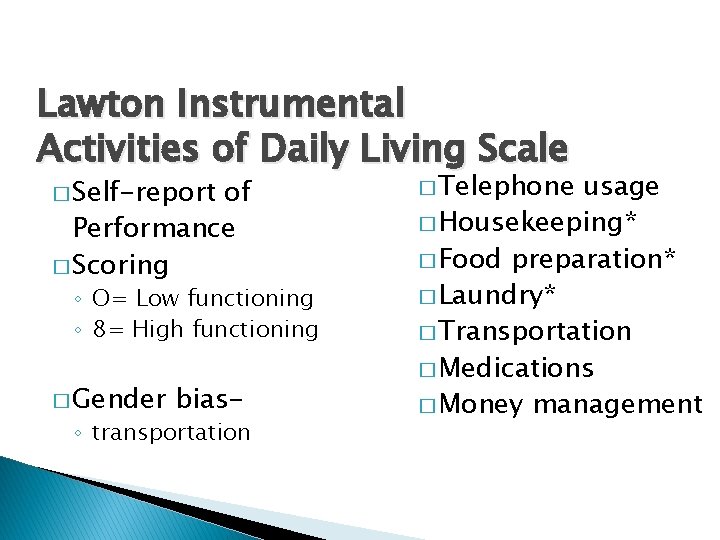
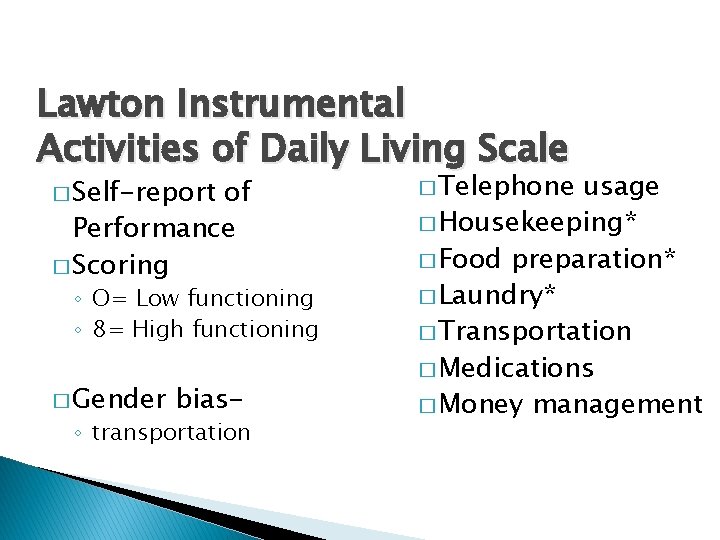
Lawton Instrumental Activities of Daily Living Scale � Self-report of Performance � Scoring ◦ O= Low functioning ◦ 8= High functioning � Gender bias- ◦ transportation � Telephone usage � Housekeeping* � Food preparation* � Laundry* � Transportation � Medications � Money management
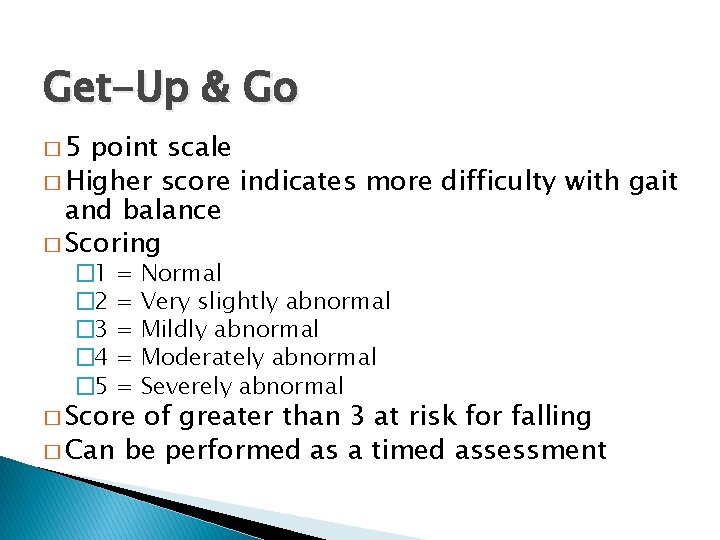
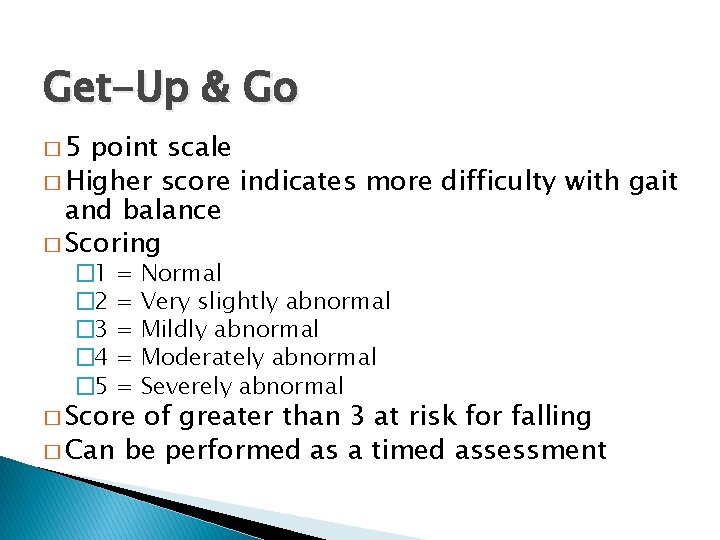
Get-Up & Go � 5 point scale � Higher score indicates more difficulty with gait and balance � Scoring � 1 � 2 � 3 � 4 � 5 = = = � Score Normal Very slightly abnormal Mildly abnormal Moderately abnormal Severely abnormal of greater than 3 at risk for falling � Can be performed as a timed assessment

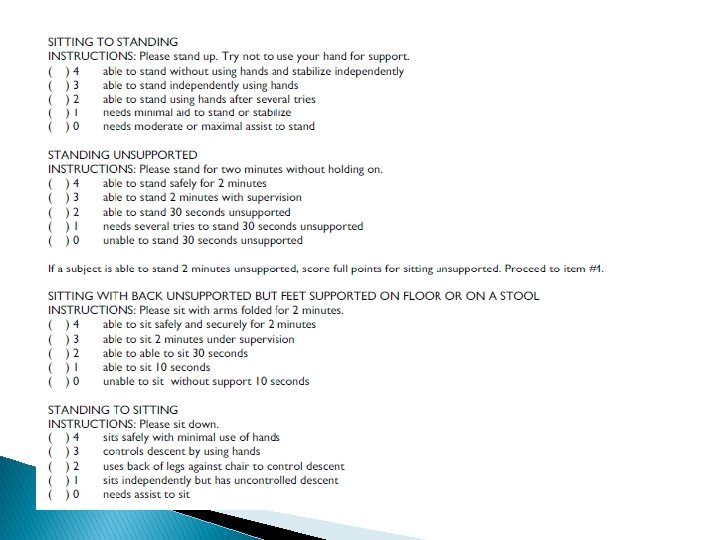
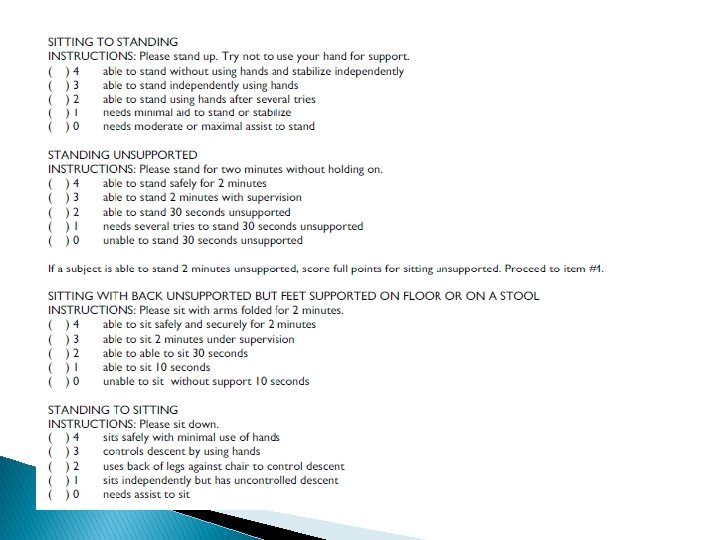
Berg Balance Scale � 14 item scale � 5 point scale, ranging from 0 -4 � Completion time: 15 -20 minutes � Equipment needed: �Ruler �Two standard chairs �Footstool or step �Stopwatch or wristwatch � Scoring � 41 -56: Low fall risk � 21 -40: Medium fall risk � 0 -20: High fall risk
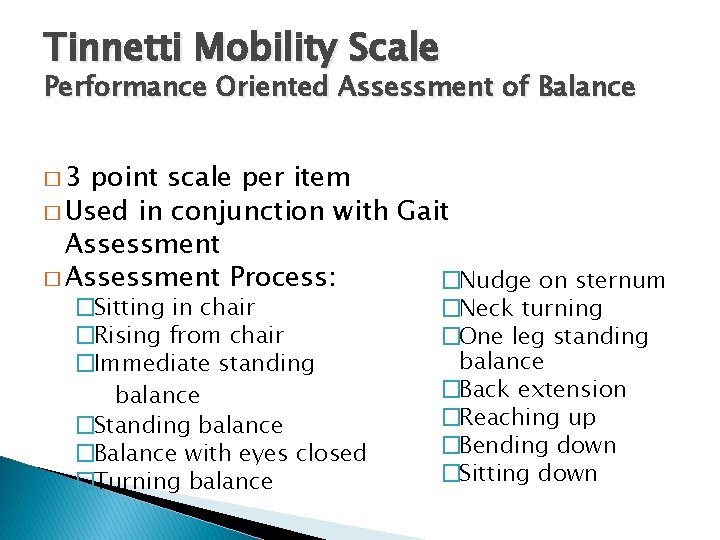
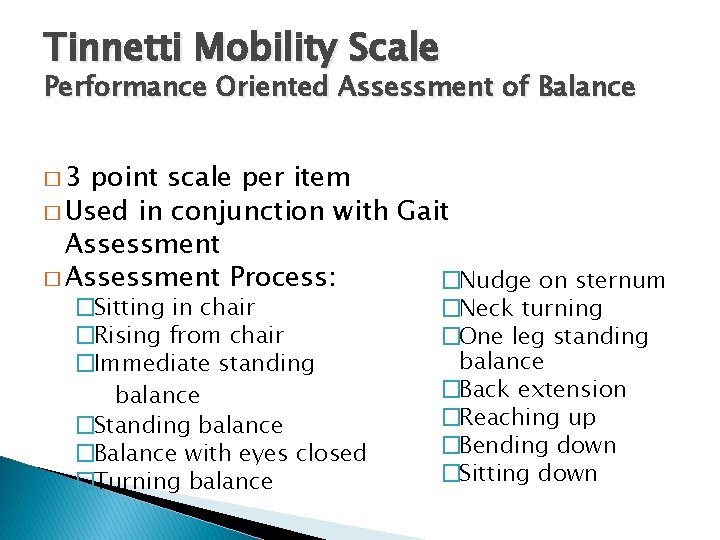
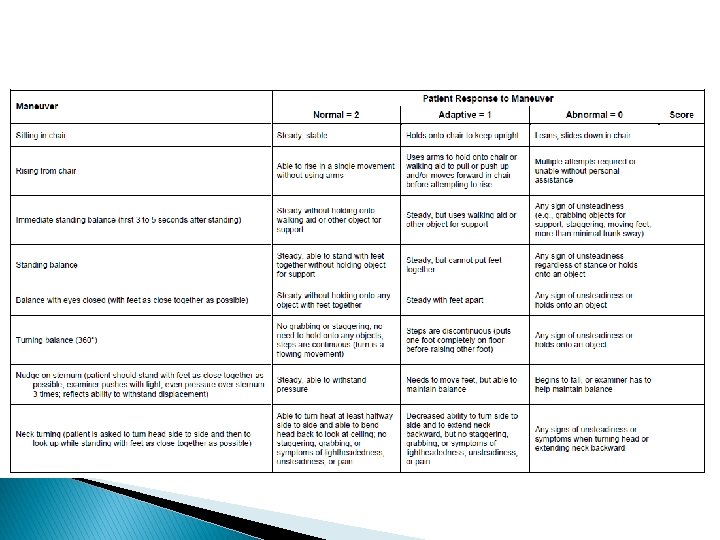
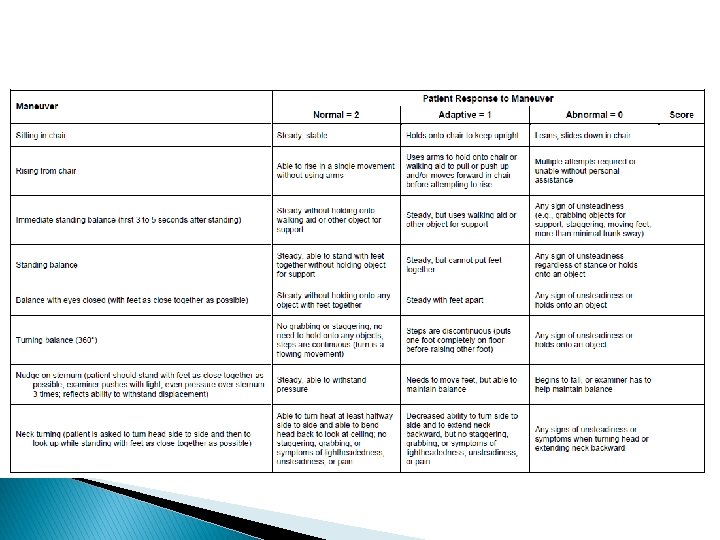
Tinnetti Mobility Scale Performance Oriented Assessment of Balance � 3 point scale per item � Used in conjunction with Gait Assessment � Assessment Process: �Nudge on sternum �Sitting in chair �Rising from chair �Immediate standing balance �Standing balance �Balance with eyes closed �Turning balance �Neck turning �One leg standing balance �Back extension �Reaching up �Bending down �Sitting down
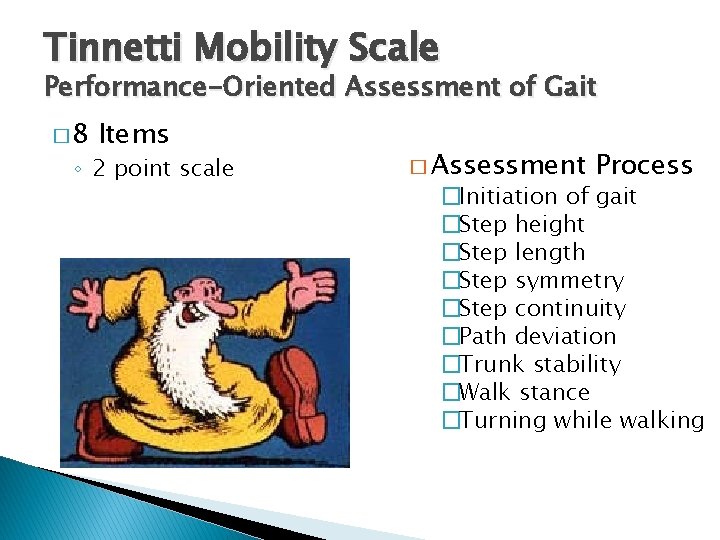
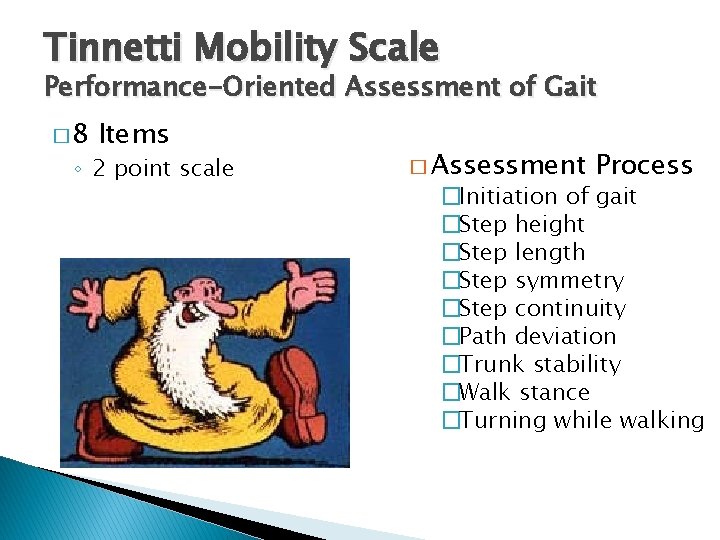
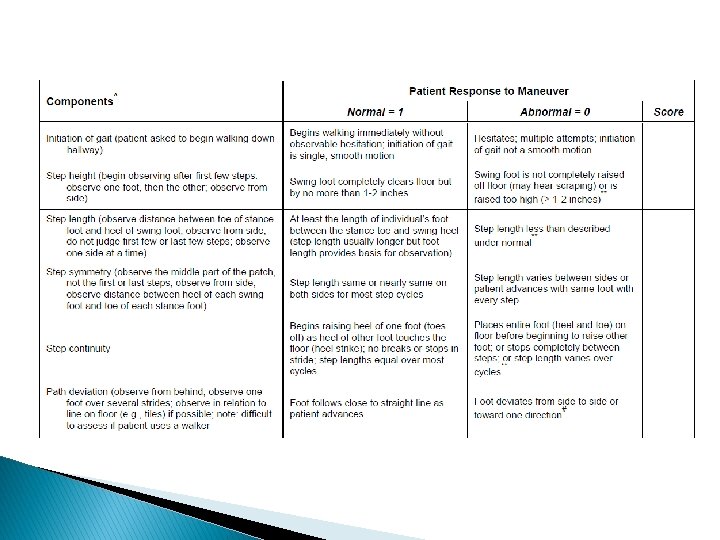
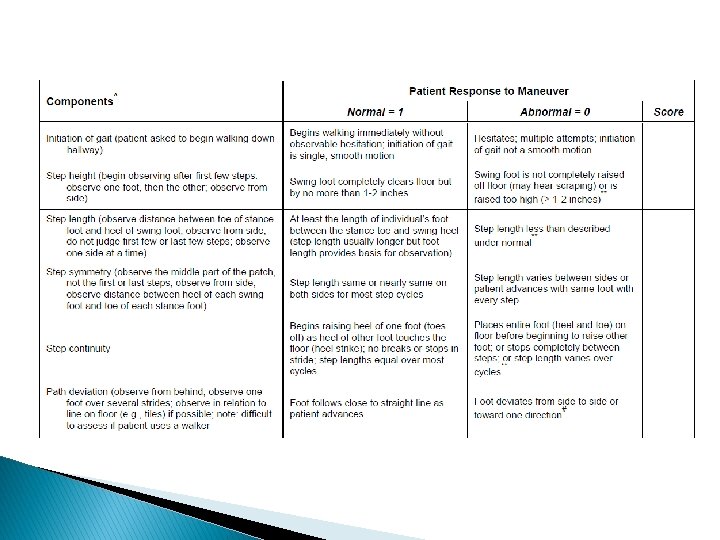
Tinnetti Mobility Scale Performance-Oriented Assessment of Gait � 8 Items ◦ 2 point scale � Assessment Process �Initiation of gait �Step height �Step length �Step symmetry �Step continuity �Path deviation �Trunk stability �Walk stance �Turning while walking
Emotional/ Psychosocial � PHQ-9 � Geriatric Depression Scale � Zung Self-Rating Depression Scale � Cornell Scale for Depression in Dementia � Zung Self-Rating Anxiety Scale � WHOQOL-BREF

PHQ-9 � Part of the Patient Health Questionnaire (PHQ) ◦ PHQ-9 - Depression Module � Self-report � Multiple choice � Measures severity of depression � Implemented in the MDS 3. 0

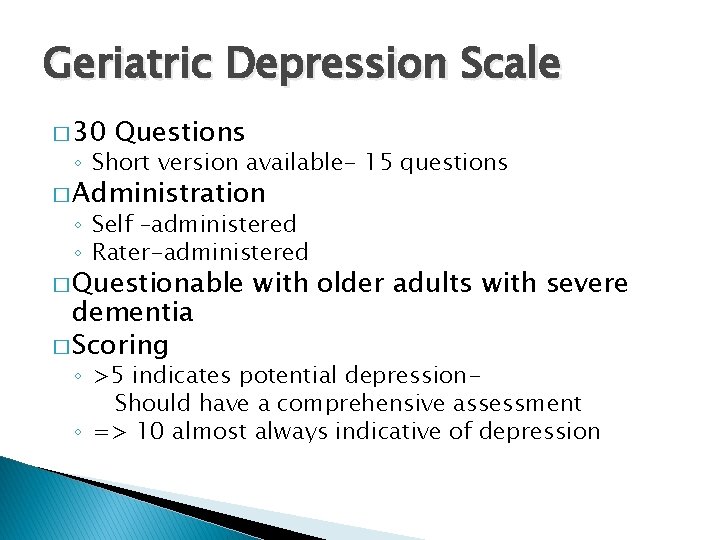
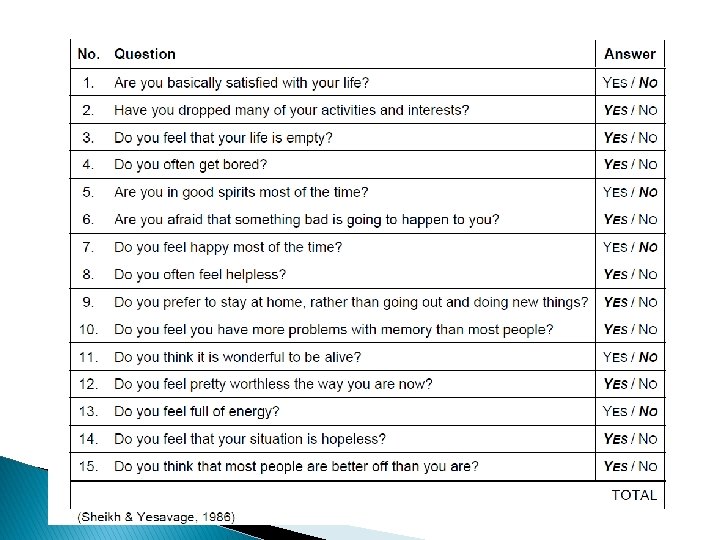
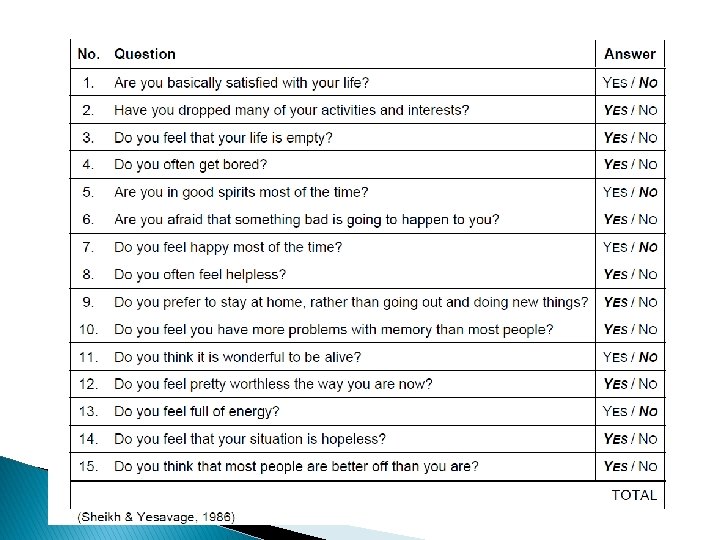
Geriatric Depression Scale � 30 Questions ◦ Short version available- 15 questions � Administration ◦ Self –administered ◦ Rater-administered � Questionable dementia � Scoring with older adults with severe ◦ >5 indicates potential depression. Should have a comprehensive assessment ◦ => 10 almost always indicative of depression
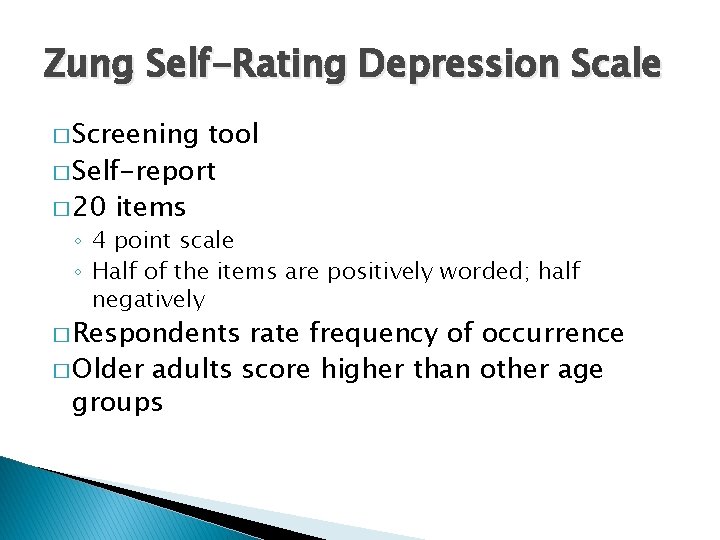
Zung Self-Rating Depression Scale � Screening tool � Self-report � 20 items ◦ 4 point scale ◦ Half of the items are positively worded; half negatively � Respondents rate frequency of occurrence � Older adults score higher than other age groups

Cornell Scale for Depression in Dementia � Administration ◦ Observation ◦ Interview � 3 �Patient �Caregiver Point Scale ◦ 0 - Absent ◦ 1 - Mild or intermittent ◦ 2 - Severe � Assessment Areas ◦ Mood related signs ◦ Behavioral disturbances ◦ Physical signs ◦ Cyclic functions ◦ Ideational disturbance

Zung Self-Rating Anxiety Scale � Self-report � 20 items ◦ 5 affective ◦ 15 somatic � Score range: 20 -80 � Administration Time: 10 -15 minutes � Used in psychiatric and medical patients and with normal older adults

World Health Organization Quality of Life (WHOQOL-BREF) � Measures the impact of disease ◦ Impact of disease and impairment of daily activities and behavior ◦ Perceived health measures ◦ Disability/ functional status measures � 26 Questions � Self-Administered � Interviewer assisted or administered � Manual is recommended to score the assessment

Pain � Faces Pain Scale � Numeric Scale � Pain Thermometer � Brief Pain Inventory � Checklist of Nonverbal Pain Indicators � Pain Assessment in Advanced Dementia Scale
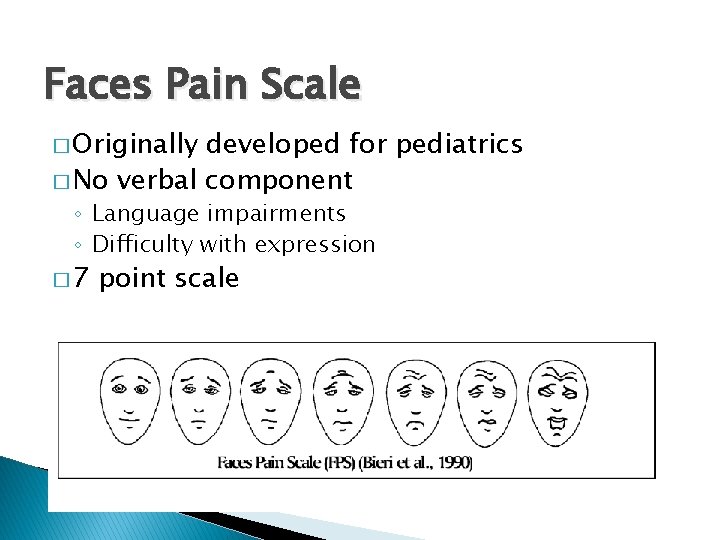
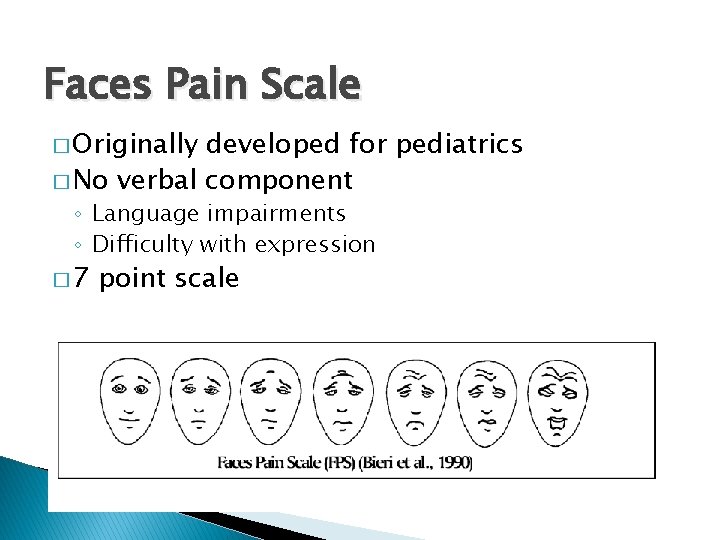
Faces Pain Scale � Originally developed for pediatrics � No verbal component ◦ Language impairments ◦ Difficulty with expression � 7 point scale
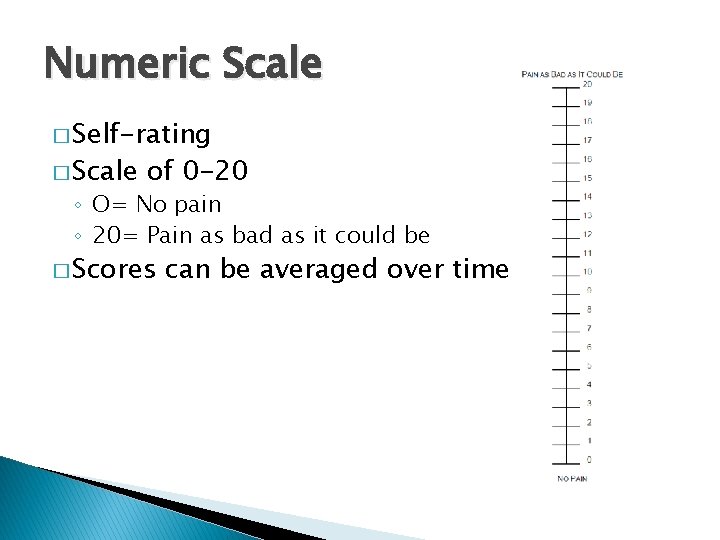
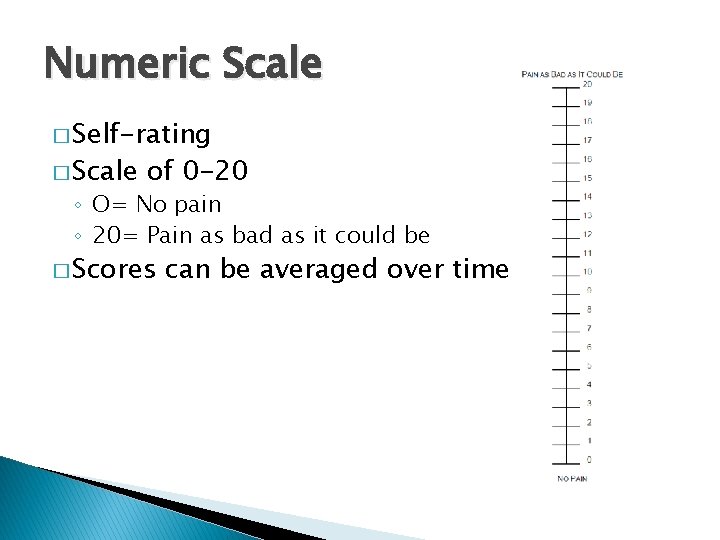
Numeric Scale � Self-rating � Scale of 0 -20 ◦ O= No pain ◦ 20= Pain as bad as it could be � Scores can be averaged over time
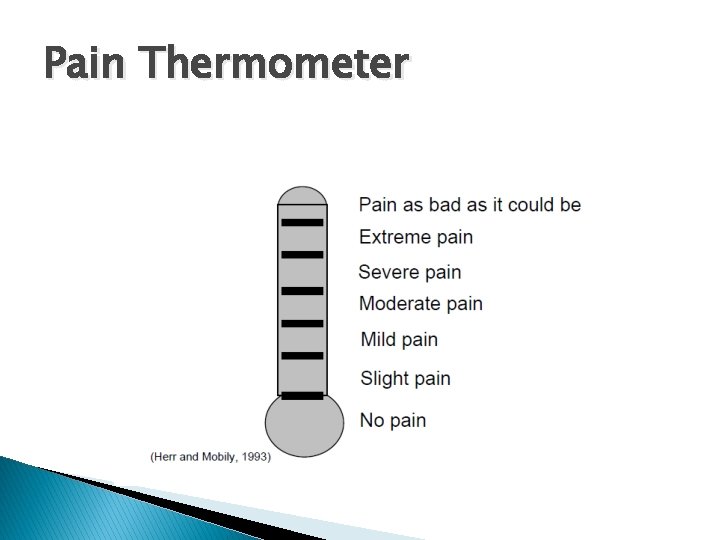
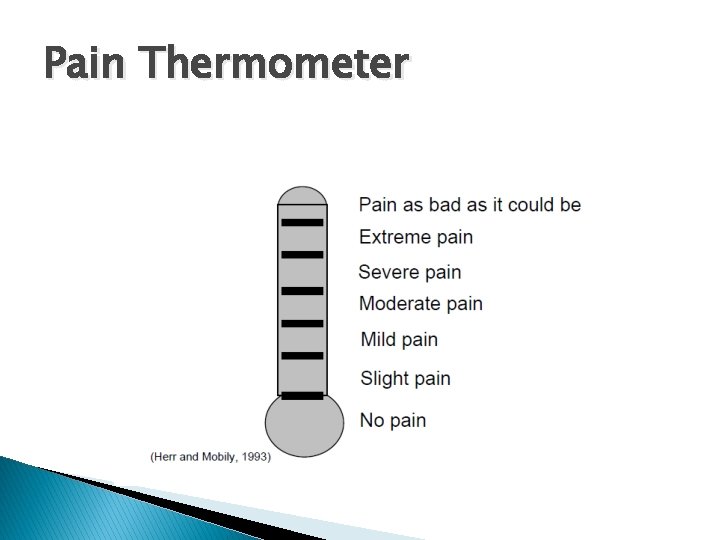
Pain Thermometer
Brief Pain Inventory � Widely used in clinical and research settings � Originally developed for used with cancer patients � Currently used with individuals experiencing chronic nonmalignant pain � 16 items ◦ Measures pain and impact on daily function � Completion time: 5 minutes (short form)

Checklist of Nonverbal Pain Indicators � Measures pain in older adults with cognitive impairment � Observation during movement and at rest � Scoring: 0 or 1 � 6 items �Nonverbal, vocal complaints �Facial grimacing �Bracing �Restlessness �Rubbing �Verbal, vocal complaints

Pain Assessment in Advanced Dementia � Observation � Score ranges from 0 -10 points � 1 -3 Mild pain � 4 -6 Moderate pain � 7 -10 Severe pain � 5 Areas Assessed �Breathing �Negative vocalization �Facial expression �Body language �Consolabilty

Buettner Assessment of Needs, Diagnosis, and Interests for Recreational Therapy in LTC � BANDI-RT � Utilizes information from MDS 3. 0 � Guides therapist ◦ ◦ Identified problems Care plan Physician’s Orders RT treatment �Flow sheet
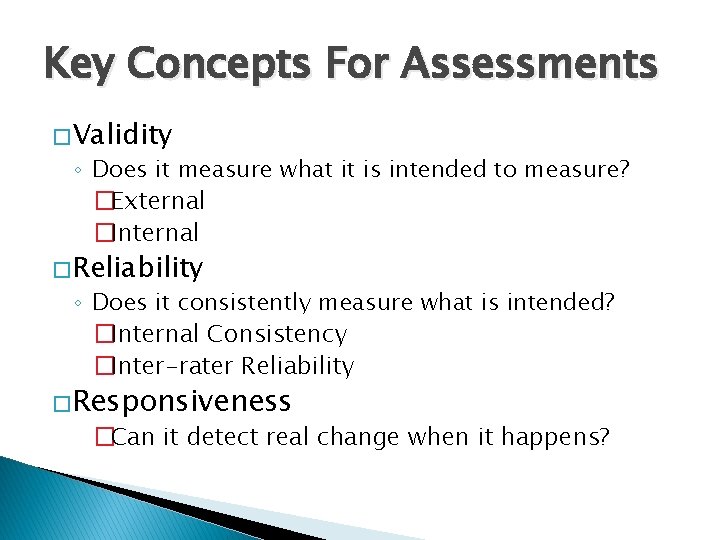
Resources for Assessments � Iowa Geriatric Education Center Geriatric Assessment Tools ◦ http: //www. healthcare. uiowa. edu/igec/tools/ � Hartford Institue of Geriatric Nursing Try This ◦ http: //hartfordign. org/practice/try_this/ � Dementia Practice Guidelines for Recreational Therapy ◦ Buettner & Fitzsimmons (2003) Available through the ATRA Bookstore

Questions