Assessment of a patient with a GI disorder

- Slides: 15
Assessment of a patient with a GI disorder By Gabie Gomez
Assessment (subjective) • Past history: smoking, alcohol use, medication abuse, recent travel, food intake. • Pain (oral, tongue, throat, abdominal) • Appetite • Pyrosis • Dysphagia • Dyspepsia (nausea, eructation, distention) • Weakness • Diarrhea or Constipation
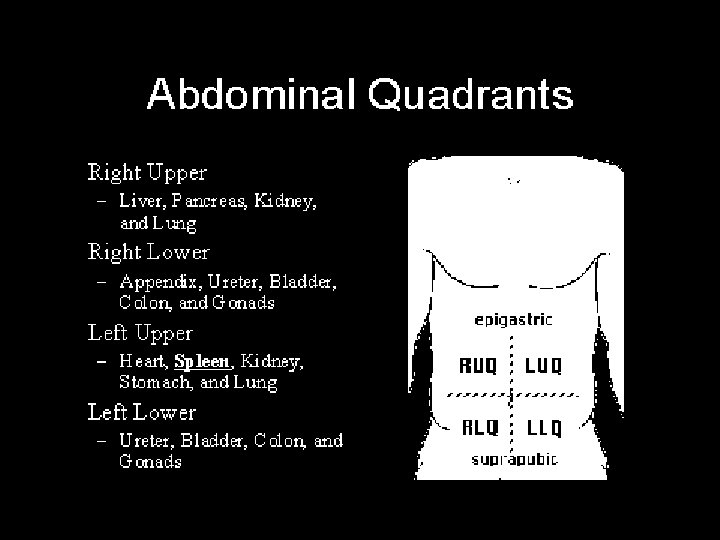
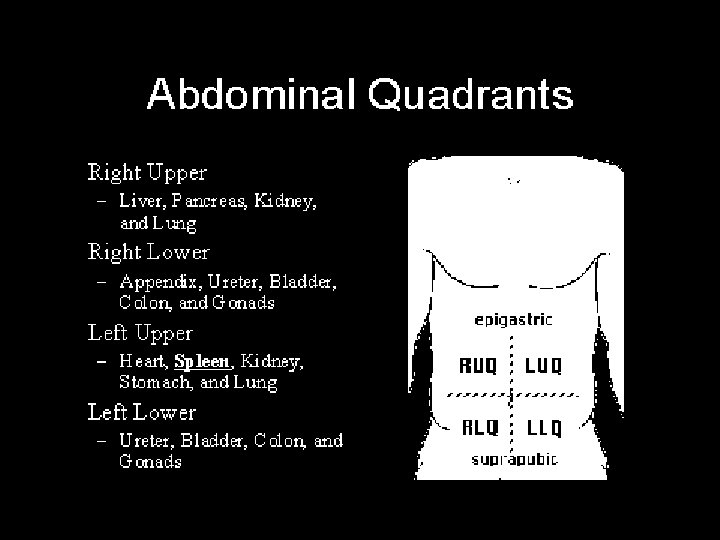
Assessment (objective) • • Vitals signs Feel for hard spots/distention(palpitate 4 quadrants) Skin color Edema Abdomen distention Wheezing Weight Loss Stool color, consistency, presence of ascites, frequency, blood, and last BM • Hematemesis

Outcomes/Planning • • • Relief pain and discomfort Stabilization of fluid and electrolyte imbalance Having no complications Resume normal activity If possible return to normal pancreatic and liver function • Patient will feel rested and assist in ADL’s.
Implementation • • • Assessment Monitor nutritional status Administer medication Relieving pain Managing fluid and electrolyte imbalance Prevent wound infections Eliminate smoking, and excessive alcohol abuse Promote normal bowel elimination Stoma care
Meds • Antacids ( maalox, mylanta, titrialac) Action: Neutralizes gastric acid. Side Effects: Constipation, chalky taste, diarrhea, increased thirst, stomach cramps Nursing Implication: Monitor electrolyte with long tem use Intervention: Do not take antacids if you have signs of appendicitis or an inflamed bowel.
Meds • Antiemtic: (Dramamine, Compazine, Promethazine, Reglan) Action: Blocks central vomiting center. Side Effects: Drowsiness, dry mouth, constipation Nursing Implication: Avoid the use with other CNS depressants and alcohol. Intervention: They may produce hypotension when used with antihypertensives, nitrates, or acute ingestion of alcohol.
Meds • H 2 receptor blockers (Zantac, Pepcid, axid, Tagamet) Action: decrease acid by blockingthe production of gastric acid, used to heal ulcers and relieve the symptoms of pain Side Effects: confusion, headache, constipation, diarrhea. Nursing Implications: Increases serum levels, effects anticoagulants Interventions: Do not give histamine receptor antagonist within 2 hours of antiacids.
Meds • Antibacterial therapy (Flagyl, tetracycline, biaxin, prilosec) Action: kills or prevents the growth of certain bacteria and protozoa (single cell animals). Side Effects: clumsiness, dizziness, or unsteadiness fever or chills, sore throat, numbness, tingling, pain or weakness in the hands or feet, seizures (convulsions) skin rash, itching Nursing Implications: Smoking should be eliminated Interventions: Dietary modifications are necessary, foods and beverages irritating to the pt. should be avoided.
Meds • Proton pump inhibitor: ( Zantac, Pepcic, Nexium) Action: antisecretory agent that inhibits secretion of gastrin by the parietal cell of the stomach. Side effects: Headache, dizziness, abdominal pain, nausea, vomiting, bone marrow suppression(rare). Nursing Implications: Inhibits hepatic metabolism of warfarin, phenytonin and other drugs. Interventions: Do not chew or crush capsule contents
Meds • Mucosal healing agents (Carafete) Action: Heals ulcers without antisecretory properties, possibly by adhering to the proteins in the ulcer base. Side effects: Constipation, hypophosphatemia Nursing Implication: Take Carafate 2 a other drugs can interfere with absorption. Intervention: If Carafate is taken with certain other drugs, the effects of either could be increased, decreased, or altered.
Meds • Antisecretory and cytoprotective: (Cytotec) Action: prostaglandin (hormone-like substance), reduces the production of stomach acid and protects the stomach lining against NSAID induced ulcers. Side effects: Constipation, gas, indigestion, headache, heavy menstrual bleeding, cramps, paleness, stomach or intestinal bleeding, vomiting Nursing Implications: Avoid with the use of alcohol or sedatives Interventions: To reduce the risk of diarrhea, take Cytotec with food and avoid taking it with a magnesiumcontaining antacid
THE END ? ? ? ? ?