Assessment and management of skin tears SARA BEST
Assessment and management of skin tears SARA BEST DISTRICT NURSE – WOUND CARE 2012

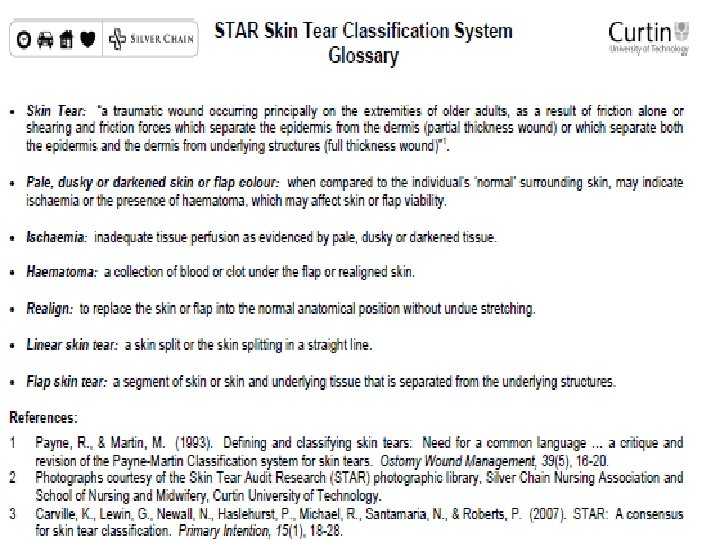
Skin Tears ‘the result of shearing, friction, or blunt trauma that causes separation of the skin layers. The subsequent wounds are partial or full thickness depending on the degree of tissue damage’ (Le. Blanc et al, 2008) Traumatic wounds have a greater risk of becoming infected

Skin Tears Dependency requiring total care for all activities of daily living = greater risk for upper limbs v. Skin tears involving independent patients usually occur on the lower extremities and are commonly associated with ambulation v 80% of patients have a history of a previous skin tear

Age related skin changes Decrease in dermal, epidermal and subcutaneous layers Lower perfusion rates and increased risk of oedema Reduction in sebum production causing dryness Impaired thermoregulation Cell turnover slower
At risk population Shared characteristics: ØSensory loss (68%) ØCompromised nutrition (68%) ØAdvanced age (76%) ØCognitive impairment (77%) ØDependency (82%) ØSteroids/polypharmacy

Skin tears
Management Control the bleeding (consider pressure, elevation and/or alginate) Cleanse the wound bed using irrigation with sterile water or saline Cleanse under the flap if dirt or blood remains post haemostasis.

Tissue alignment If the skin flap is viable, roll back into place using a moistened cotton tip or gauze Do not stretch any remaining skin flap in order to approximate the flap edges Gently lie the remaining flap over the wound bed
Assess and dress Assess the degree of tissue loss and flap colour using the STAR classification system Easy to apply Provides a protective anti-shear barrier Optimises the physiological healing environment Flexible and moulds to contours Does not cause trauma on removal Optimises quality of life and cosmesis Cost effective
Which dressings? Silicone dressings – security of approximated flap Calcium alginate – controls minor haemostasis Antimicrobials – prevention of bacterial contamination eg immunocompromised. Local infection +/- systemic antibiotics Non-adhesive dressings – need x 2 layers Hydrocolloids – with caution

Dressings cont. Films – not recommended Adhesive strips – not recommended current treatment of choice. 1 cm apart Sutures and staples – may be required for deep, full thickness lacerations Retention bandages – where adhesives contraindicated

Skin tears Mark the date for removal Assess and address further factors which delay healing Tubular support bandages – straight or shaped, can be a good choice to support wounds on the lower leg but must be applied toe-knee to prevent problems with oedema displacement (vascular status) - Full thickness flaps (where fat, muscle or other underlying tissues are seen), OR those with large haematomas need medical review
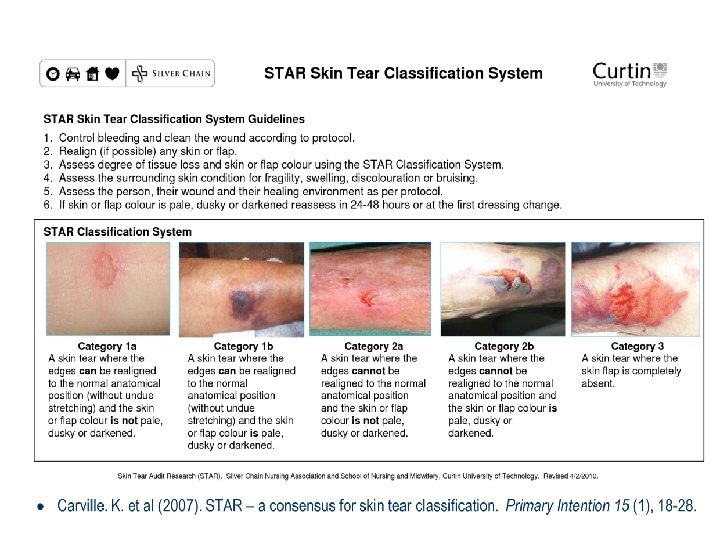
Classification System
Review and re-assess If the skin flap is pale, dusky or darkened, reassess in 24 -48 hours to ensure that the flap is viable (attached and pink in colour). If not viable, remove the non-viable tissue with sterile scissors Unless clinical signs of infection, leave the primary dressing intact for 5 -7 days The secondary dressing should be changed earlier if indicated - Strikethrough - Leakage - Signs of infection

Skin tears

Common Issues
Chronic Wound Categorised as a wound that fails to progress through the phases of healing in an orderly or timely manner More than 90% on non-healing wounds can be categorised as venous ulcers, pressure sores or diabetic ulcers Chronic wounds become ‘arrested’ in the inflammatory phase May be due to tissue hypoxia or ischaemia or presence of bacteria
When to refer Remember – if the underlying aetiology and factors which affect healing are not addressed then product selection alone is unlikely to improve healing. If the skin tear is on an oedematous leg or a leg with venous disease, assess suitability for compression No progress by 4 - 6 weeks – refer to GP/CHS History of slow to heal wounds lower limb History of venous leg ulcers

Useful website links http: //www. awma. com. au Australian Wound Association http: //www. worldwidewounds. com/ Wound management practice resource centre http: //www. ewma. org European wound management association http: //www. wounds-uk. com/ Wound management resource and e-learning site http: //www. cochranewounds. org Reviews by Cochrane group
References Caville K, Lewin G. (2007) STAR: a consensus for skin tear classification. Primary Intention, 15(1), 18 -28 Flour M. (2009) The pathophysiology of vulnerable skin. Accessed from: www. worldwidewounds. com/2009/September/Flour/vu lnerable-skin-1. html Lawt 0 n S, Langoen A. (2009) Assessing and managing vulnerable skin. Accessed from: www. worldwidewounds. com/2009/October/Lawton. Langoen/vulnerable-skin-2. html
References Silver Chain Nursing Association and School of Nursing and Midwifery, Curtin University of technology. (2007). Skin Tear Audit Research (STAR) Joanna Briggs Institute 2010 Best Practice Reviews: Stomski, Norman. Skin Tears: Management. Joanna Briggs Institute - JBI COn. NECT+. [Online] 22 February 2010. [Cited: 17 March 2011. ] http: //www. jbiconnectplus. org. au.
Skin p. H Normal skin p. H is 5. 4 – 5. 9 Elderly people tend to have more alkaline skin (increase PH). Moist body folds increased alkalinity, more prone to yeast and fungal infections Occlusive dressings and exposure to skin irritants can raise PH disrupting the skin barrier Skin acidity is bacteriostatic for some strains & most grow better in a neutral PH
- Slides: 23