Assessing Vasoplegia Syndrome After Heart Transplantation in Pediatric


- Slides: 21
Assessing Vasoplegia Syndrome After Heart Transplantation in Pediatric Patients Bridged with Ventricular Assist Devices vs Medical Therapy Madeleine Townsend, MD Cleveland Clinic Pediatric Cardiology Fellow
Ventricular Assist Devices (VAD) • Increasingly used as a bridge therapy to heart transplant − Decrease waitlist mortality & improve survival to transplant • 2 types: pulsatile and continuous − Pulsatile, e. g. Berlin EXCOR − Continuous, e. g. Heart. Ware, Heart. Mate Shuhaiber J et al. BMJ. 2010
VAD Prevalence in Pediatrics • From Pedimacs database: − Between 2012 -2016, 42 hospitals implanted 432 devices in 364 patients less than 19 years of age − Diagnoses included: • Cardiomyopathy 61% • Myocarditis 11% • Congenital heart disease 21% − ~50% underwent heart transplant within 6 months Blume ED, et al. Inten. J Heart Lung Transplant. 2018
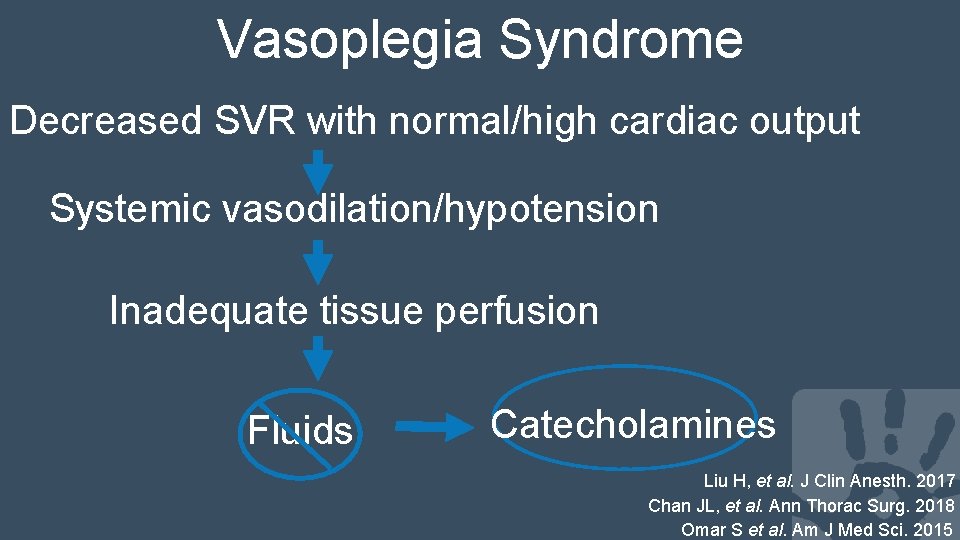
Vasoplegia Syndrome • Potential complication following cardiac surgery • Risk factors include time on cardiopulmonary bypass (CBP), need for vasopressors prior to CBP, preoperative meds (ACEI, ARB, beta blockers) • Pre-surgery VAD use in adult literature • With known predisposing factors, rate 30 -50% • No universally accepted definition Shaefi S, et al. J Cardiothorac Vasc Anesth. 2018
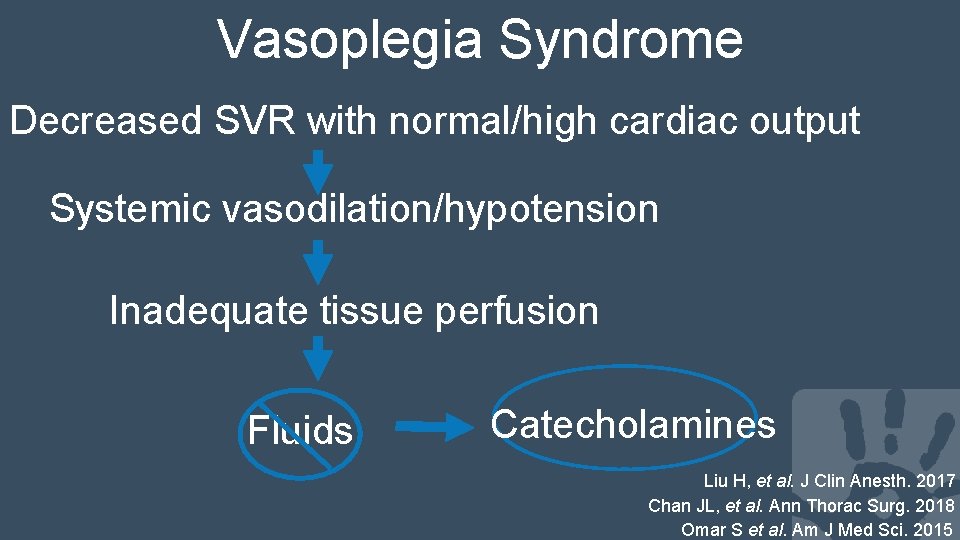
Vasoplegia Syndrome Decreased SVR with normal/high cardiac output Systemic vasodilation/hypotension Inadequate tissue perfusion Fluids Catecholamines Liu H, et al. J Clin Anesth. 2017 Chan JL, et al. Ann Thorac Surg. 2018 Omar S et al. Am J Med Sci. 2015

Vasoactive Index Score (VIS) Wernowsky Index Score (IS) = Dopa (μg/kg/min) + Dobutamine (μg/kg/min) +100× Epi (μg/kg/min) VIS = IS + 10× Milrinone (μg/kg/min) +10, 000× Vasopressin (U/kg/min) + 100× Norepi (μg/kg/min) Davidson J, et al. Intensive Care Med. 2012
Hypothesis VAD use may predispose patients to an increased rate of vasoplegia syndrome following pediatric heart transplantation relative to medical therapy alone.
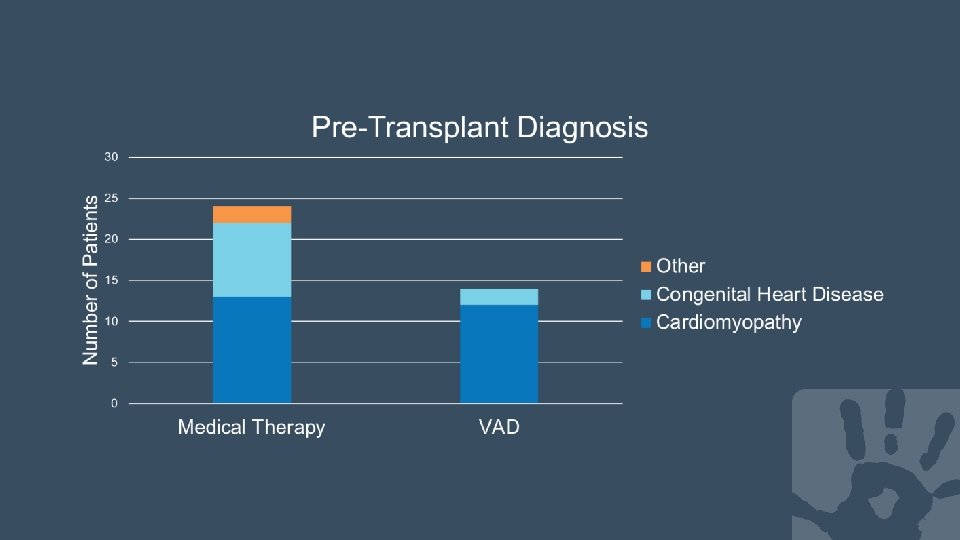
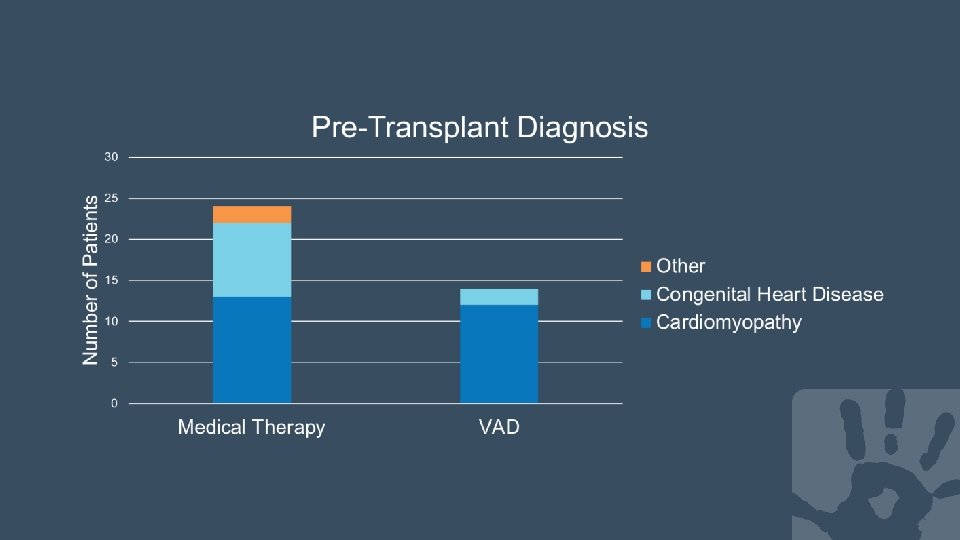
Study Design • Retrospective chart review of the pediatric heart transplant patients (0 - 21 years of age) at Cleveland Clinic Children’s Hospital from December 2010 to December 2016 • Patients divided based on VAD use pre-transplant vs medical therapy. VAD group subdivided into continuous vs pulsatile type
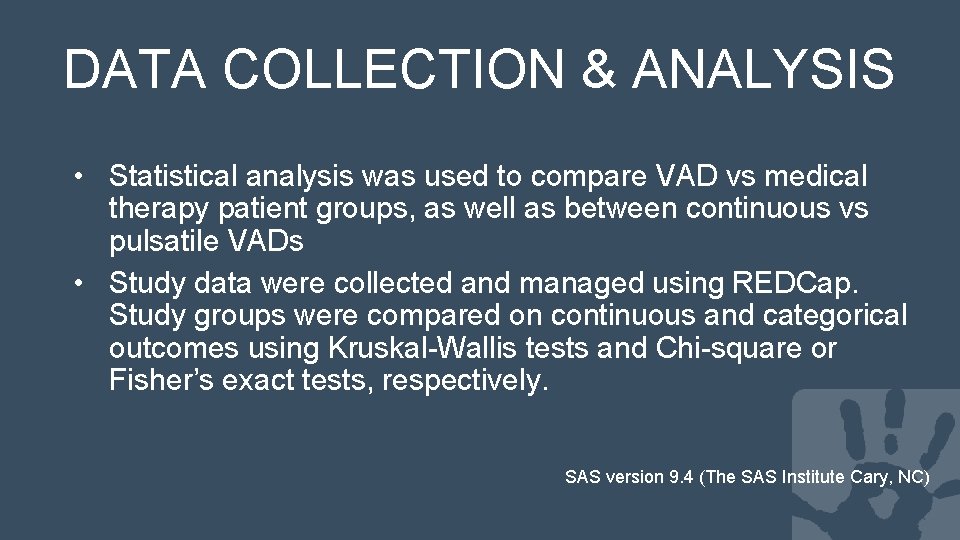
DATA COLLECTION & ANALYSIS • Statistical analysis was used to compare VAD vs medical therapy patient groups, as well as between continuous vs pulsatile VADs • Study data were collected and managed using REDCap. Study groups were compared on continuous and categorical outcomes using Kruskal-Wallis tests and Chi-square or Fisher’s exact tests, respectively. SAS version 9. 4 (The SAS Institute Cary, NC)
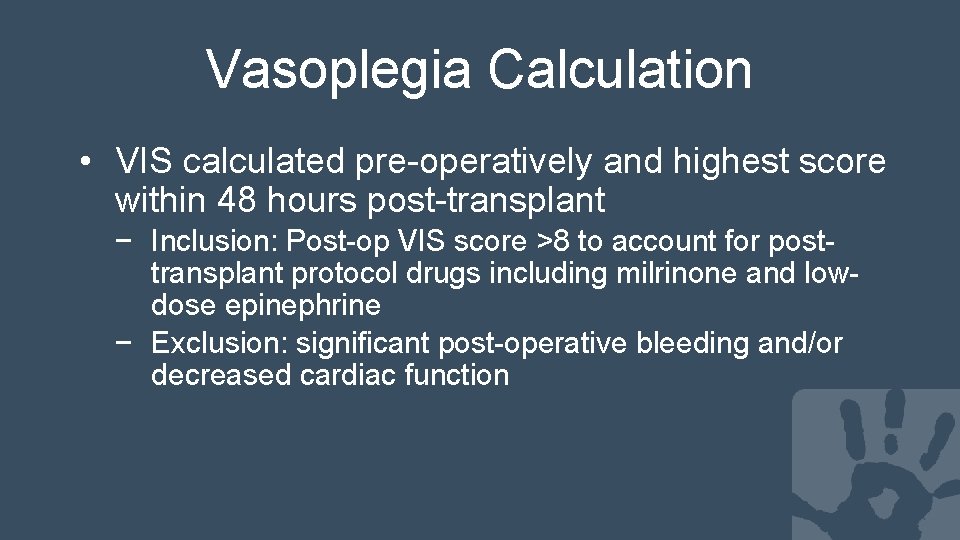
Vasoplegia Calculation • VIS calculated pre-operatively and highest score within 48 hours post-transplant − Inclusion: Post-op VIS score >8 to account for posttransplant protocol drugs including milrinone and lowdose epinephrine − Exclusion: significant post-operative bleeding and/or decreased cardiac function
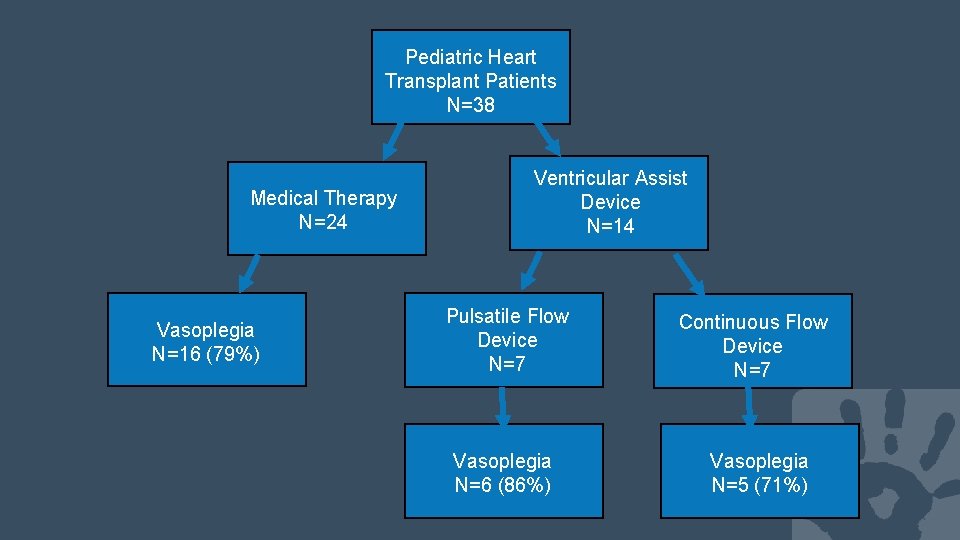
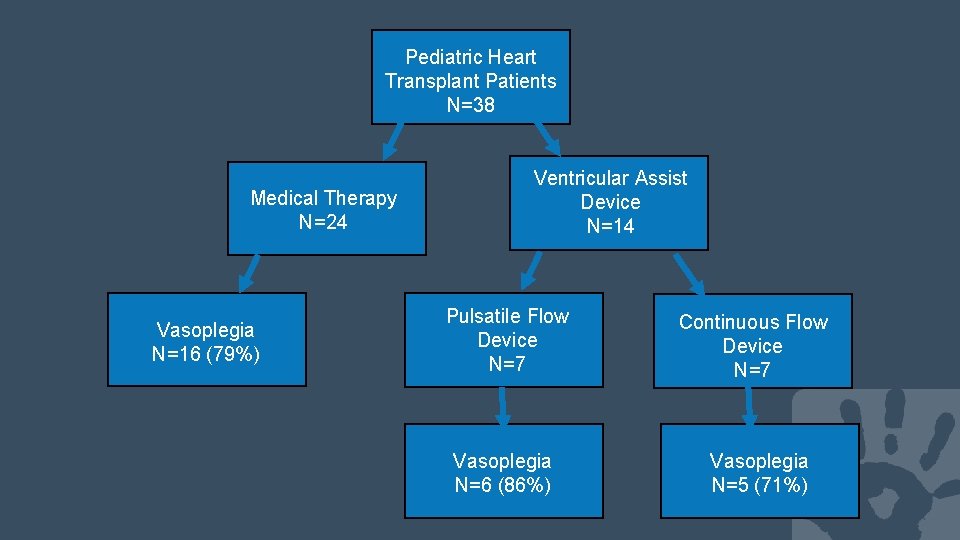
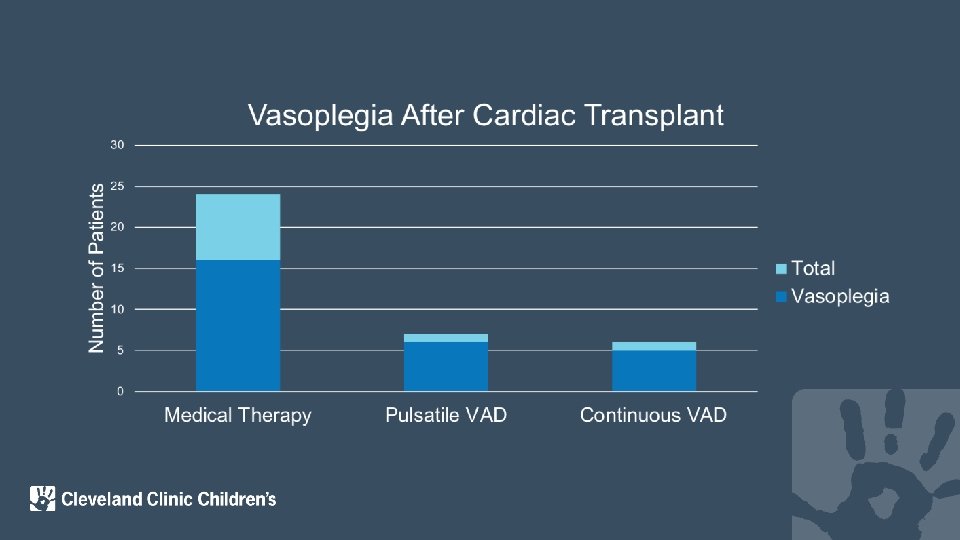
Pediatric Heart Transplant Patients N=38 Medical Therapy N=24 Vasoplegia N=16 (79%) Ventricular Assist Device N=14 Pulsatile Flow Device N=7 Vasoplegia N=6 (86%) Continuous Flow Device N=7 Vasoplegia N=5 (71%)
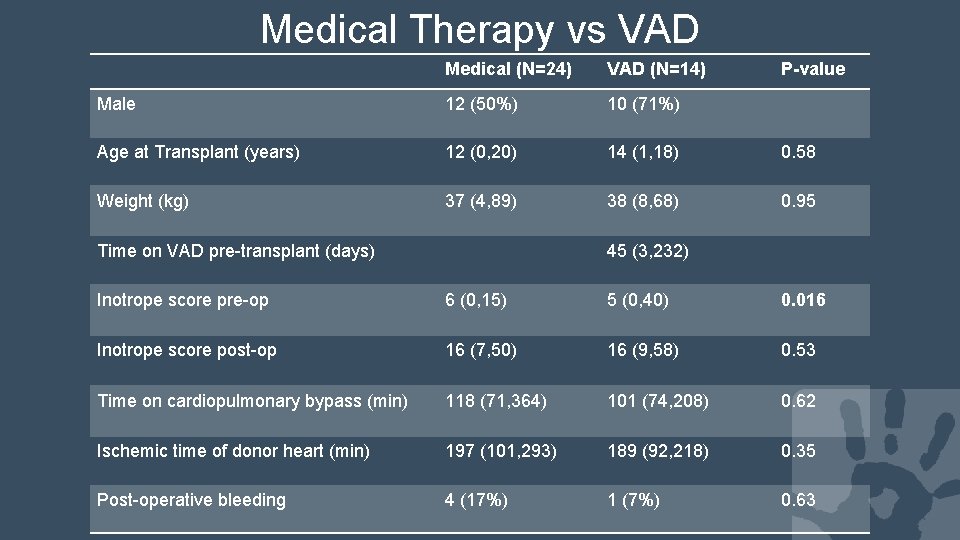
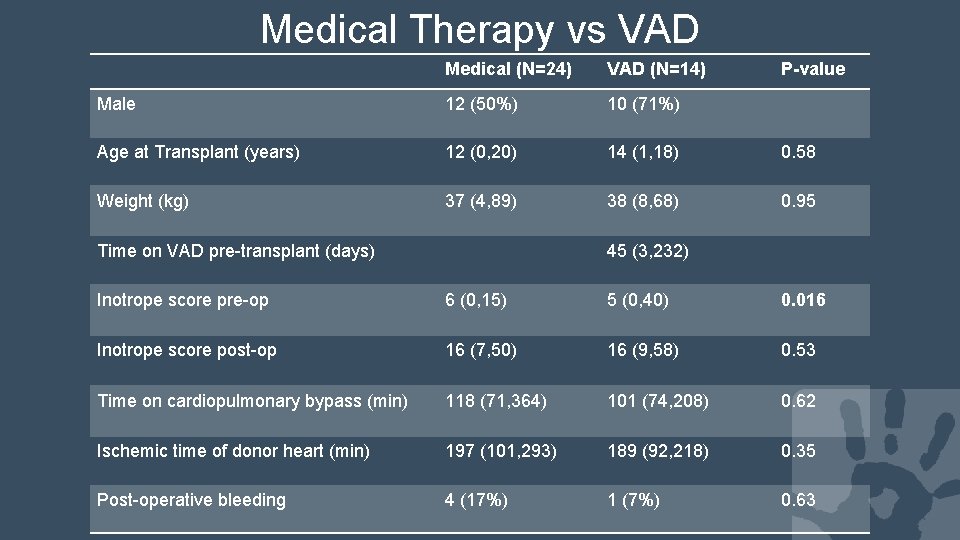
Medical Therapy vs VAD Medical (N=24) VAD (N=14) Male 12 (50%) 10 (71%) Age at Transplant (years) 12 (0, 20) 14 (1, 18) 0. 58 Weight (kg) 37 (4, 89) 38 (8, 68) 0. 95 Time on VAD pre-transplant (days) P-value 45 (3, 232) Inotrope score pre-op 6 (0, 15) 5 (0, 40) 0. 016 Inotrope score post-op 16 (7, 50) 16 (9, 58) 0. 53 Time on cardiopulmonary bypass (min) 118 (71, 364) 101 (74, 208) 0. 62 Ischemic time of donor heart (min) 197 (101, 293) 189 (92, 218) 0. 35 Post-operative bleeding 4 (17%) 1 (7%) 0. 63
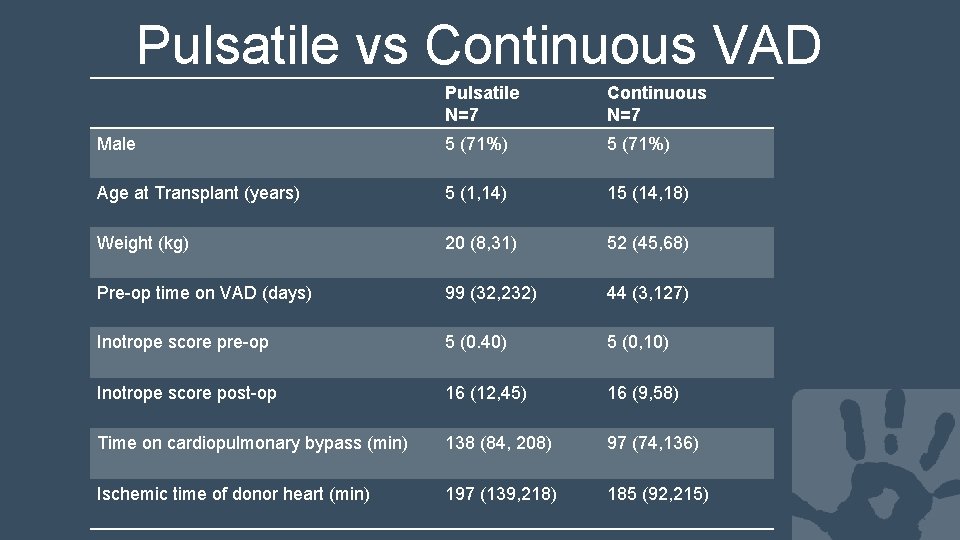
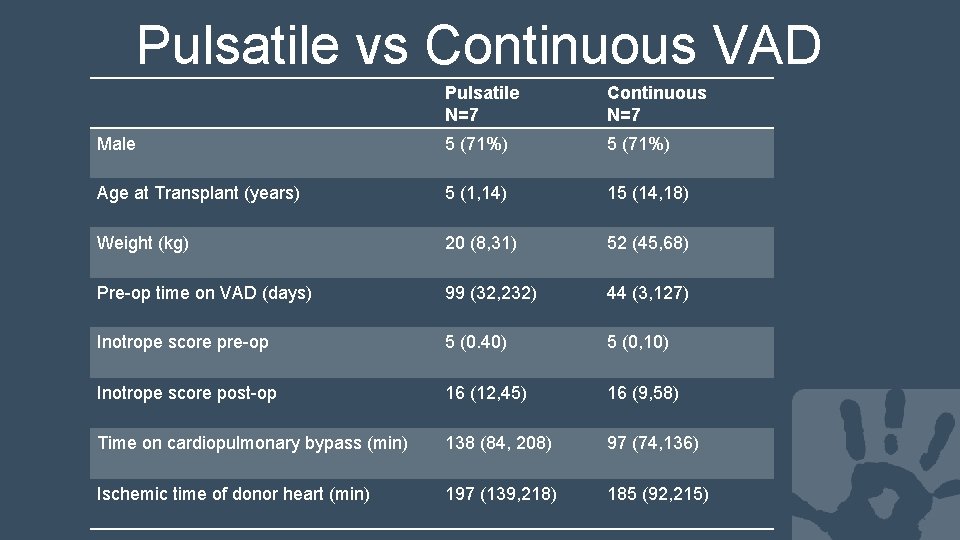
Pulsatile vs Continuous VAD Pulsatile N=7 Continuous N=7 Male 5 (71%) Age at Transplant (years) 5 (1, 14) 15 (14, 18) Weight (kg) 20 (8, 31) 52 (45, 68) Pre-op time on VAD (days) 99 (32, 232) 44 (3, 127) Inotrope score pre-op 5 (0. 40) 5 (0, 10) Inotrope score post-op 16 (12, 45) 16 (9, 58) Time on cardiopulmonary bypass (min) 138 (84, 208) 97 (74, 136) Ischemic time of donor heart (min) 197 (139, 218) 185 (92, 215)
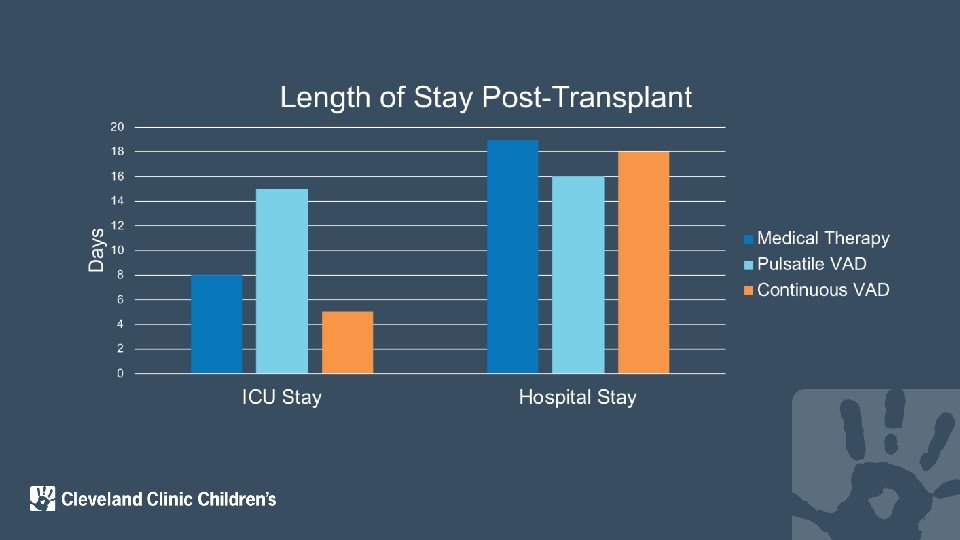
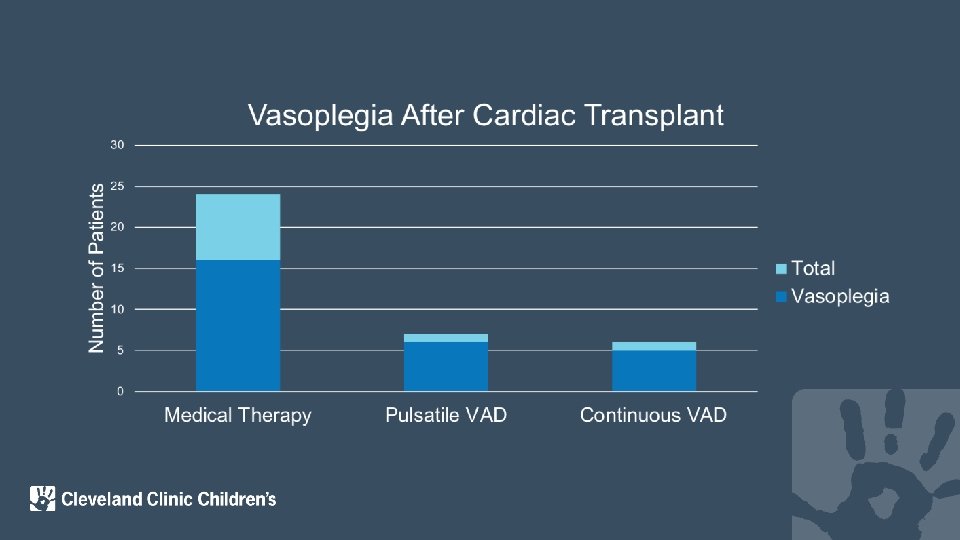
Conclusion • High incidence of vasoplegia syndrome in pediatric post-transplant patients • No significant difference between medical therapy & VAD groups − Trend toward increased rate in VAD group, small sample size may be impacting results • Similar finding to that seen in adult literature
Limitations • Small sample sizes • Retrospective review • No universally accepted definition of vasoplegia syndrome
Future Directions • Multicenter prospective design or use of the current heart transplant databases could contribute a larger population size
Thank you to Dr. Boyle and the Pediatric Heart Transplant team, as well as the support of the CCF Biostatistics department

 Vasoplegia
Vasoplegia After me after me after me
After me after me after me John 14
John 14 Bone marrow transplantation sri lanka
Bone marrow transplantation sri lanka Law of transplantation
Law of transplantation Patrick evrard mont godinne
Patrick evrard mont godinne Cultural transposition
Cultural transposition Types of transplantation
Types of transplantation Stem cell phuket
Stem cell phuket Pediatric heart rate chart
Pediatric heart rate chart Pediatric heart rate chart
Pediatric heart rate chart Hyperoxitest
Hyperoxitest Btec sport unit 3
Btec sport unit 3 Unit 18 assessing children's development support needs
Unit 18 assessing children's development support needs Assessing grammar effectively
Assessing grammar effectively What is the difference between ncbts and ppst?
What is the difference between ncbts and ppst? Task analysis in hrd
Task analysis in hrd Formal reading
Formal reading Aashto manual for assessing safety hardware
Aashto manual for assessing safety hardware Cultural dynamics in assessing global markets
Cultural dynamics in assessing global markets Assessing a new venture's financial strength and viability
Assessing a new venture's financial strength and viability Assessing cardiorespiratory fitness
Assessing cardiorespiratory fitness