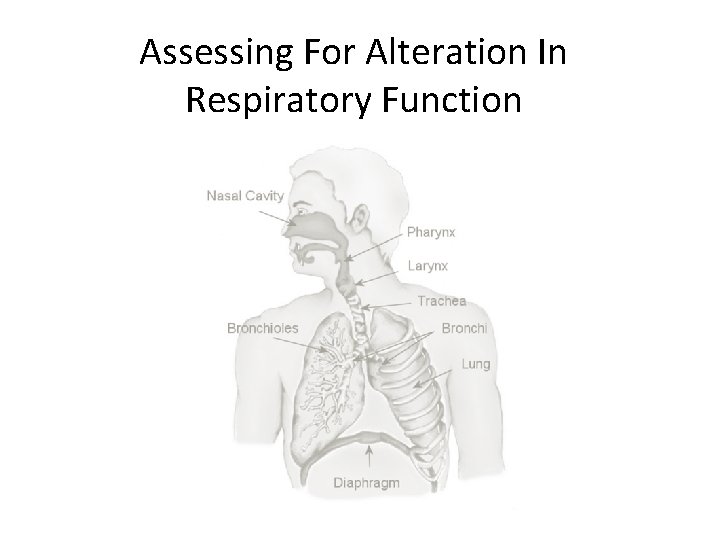
Assessing For Alteration In Respiratory Function Respiratory Alterations
- Slides: 31
Assessing For Alteration In Respiratory Function
Respiratory Alterations Risk Factors • • Age Sex Ethnic origin Family History Smoking History Medications Use Allergies Diet
History of Present Illness • In relation to cough, sputum production, chest pain, and SOB at rest and exertion. – Onset – Duration – Location – Frequency – Progression and radiation – Aggravating and relieving factors – Associated signs and symptoms – Treatment
Assessment Techniques • • Inspection Palpation Percussion Auscultation
Assessment of Upper Respiratory Tract • Nose and sinuses – Inspect: symmetry, nasal flaring, deformities, swelling, redness, or drainage? – Palpate: tenderness or swelling over sinuses? • Pharynx, Trachea, and Larynx – Inspect: symmetry, discharge, inflammation of mouth or pharynx? Masses, swelling, or palpable lymph nodes? Vocal changes? – Palpate: deviations, tenderness, or masses of trachea?
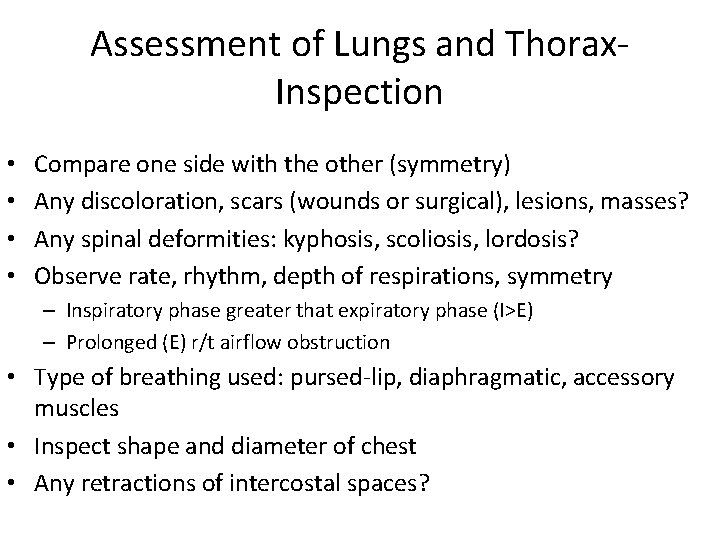
Assessment of Lungs and Thorax. Inspection • • Compare one side with the other (symmetry) Any discoloration, scars (wounds or surgical), lesions, masses? Any spinal deformities: kyphosis, scoliosis, lordosis? Observe rate, rhythm, depth of respirations, symmetry – Inspiratory phase greater that expiratory phase (I>E) – Prolonged (E) r/t airflow obstruction • Type of breathing used: pursed-lip, diaphragmatic, accessory muscles • Inspect shape and diameter of chest • Any retractions of intercostal spaces?
Assessment of Lungs and Thorax. Palpation • Symmetry of respiratory movement • Areas of tenderness, masses, lesions, swelling • Thoracic expansion • Crepitus
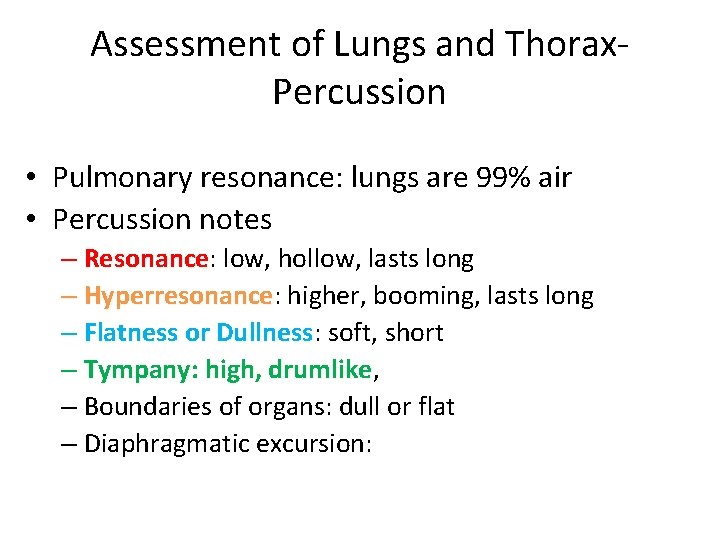
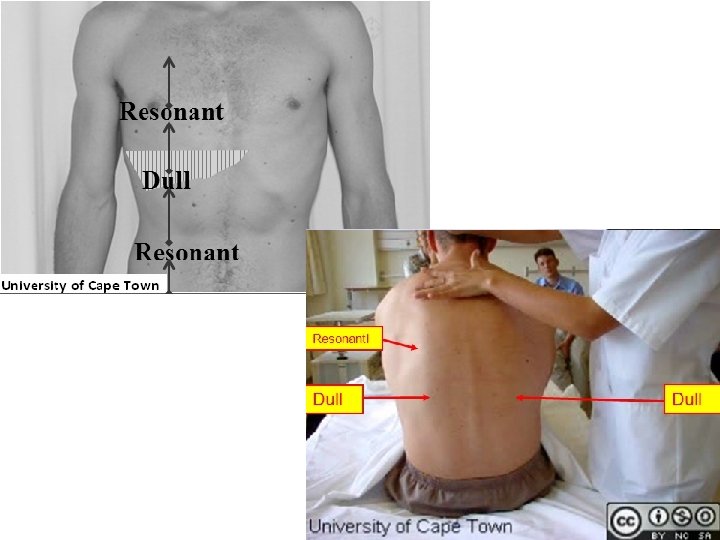
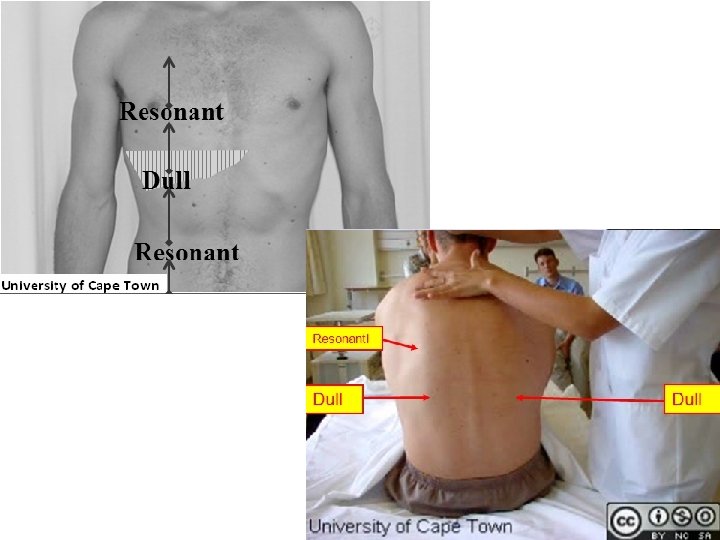
Assessment of Lungs and Thorax. Percussion • Pulmonary resonance: lungs are 99% air • Percussion notes – Resonance: Resonance low, hollow, lasts long – Hyperresonance: Hyperresonance higher, booming, lasts long – Flatness or Dullness: Dullness soft, short – Tympany: high, drumlike – Boundaries of organs: dull or flat – Diaphragmatic excursion:
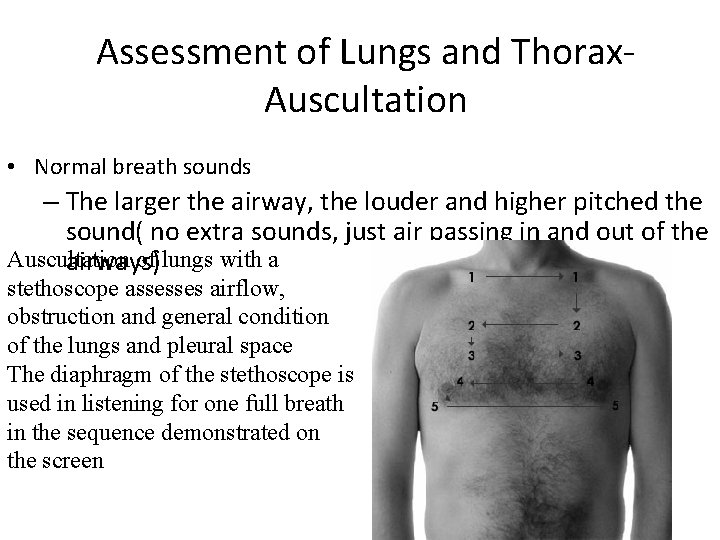
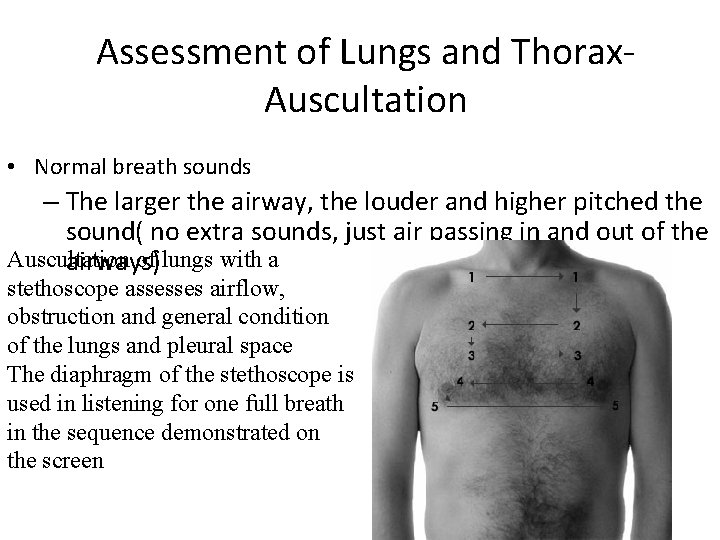
Assessment of Lungs and Thorax. Auscultation • Normal breath sounds – The larger the airway, the louder and higher pitched the sound( no extra sounds, just air passing in and out of the Auscultation of lungs with a airways) stethoscope assesses airflow, obstruction and general condition of the lungs and pleural space The diaphragm of the stethoscope is used in listening for one full breath in the sequence demonstrated on the screen
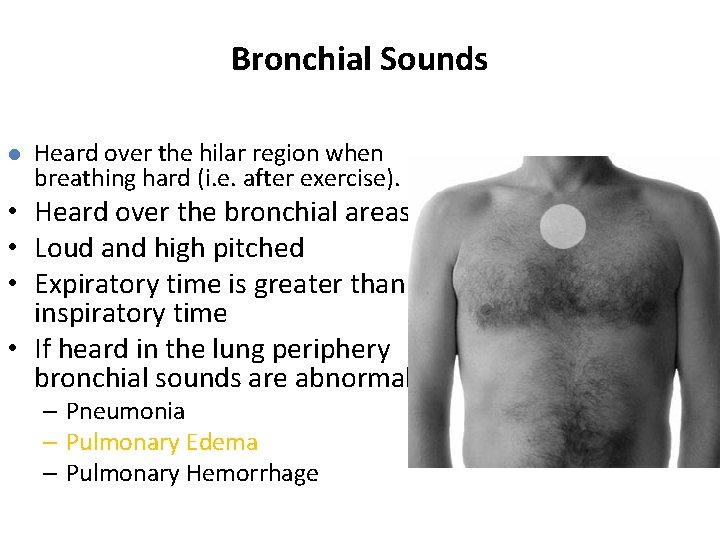
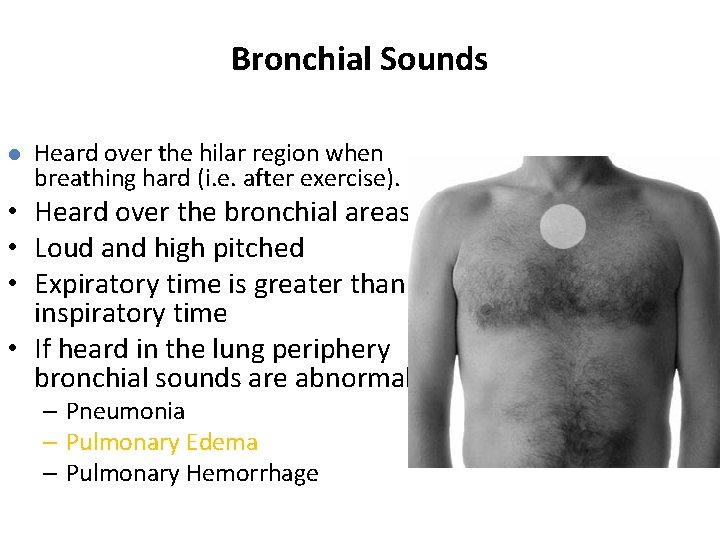
Bronchial Sounds l Heard over the hilar region when breathing hard (i. e. after exercise). • Heard over the bronchial areas • Loud and high pitched • Expiratory time is greater than inspiratory time • If heard in the lung periphery bronchial sounds are abnormal – Pneumonia – Pulmonary Edema – Pulmonary Hemorrhage
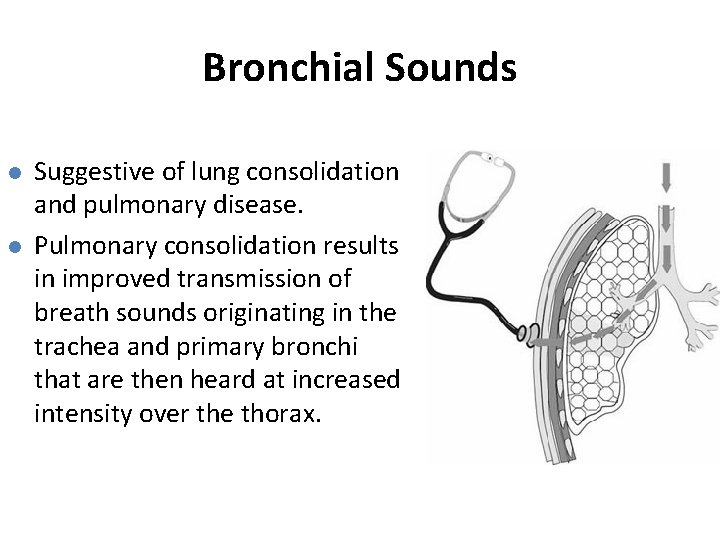
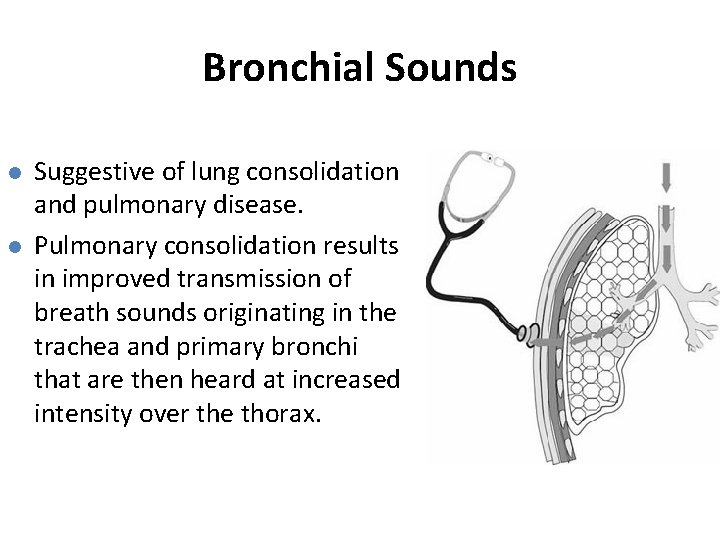
Bronchial Sounds l l Suggestive of lung consolidation and pulmonary disease. Pulmonary consolidation results in improved transmission of breath sounds originating in the trachea and primary bronchi that are then heard at increased intensity over the thorax.
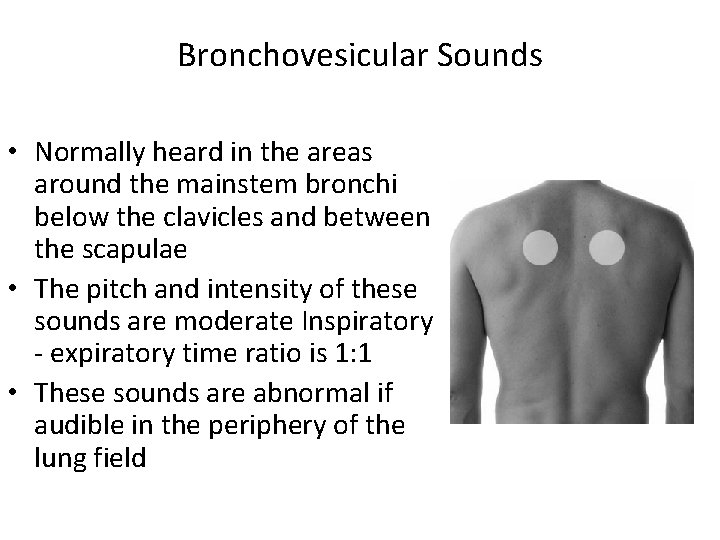
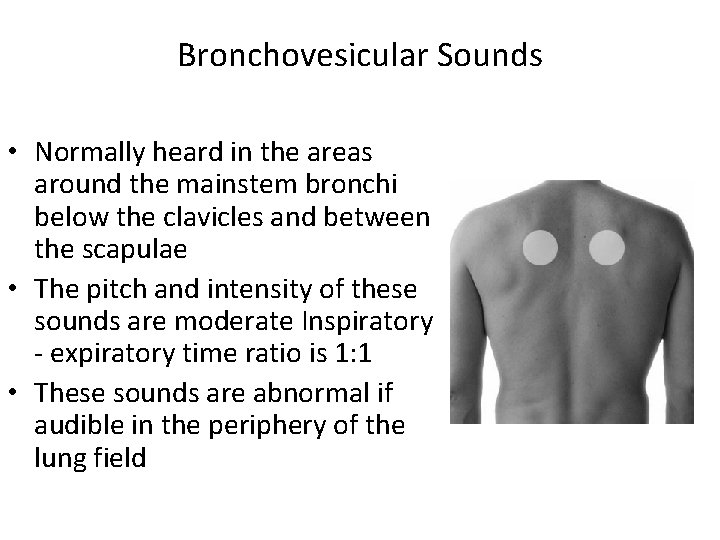
Bronchovesicular Sounds • Normally heard in the areas around the mainstem bronchi below the clavicles and between the scapulae • The pitch and intensity of these sounds are moderate Inspiratory - expiratory time ratio is 1: 1 • These sounds are abnormal if audible in the periphery of the lung field
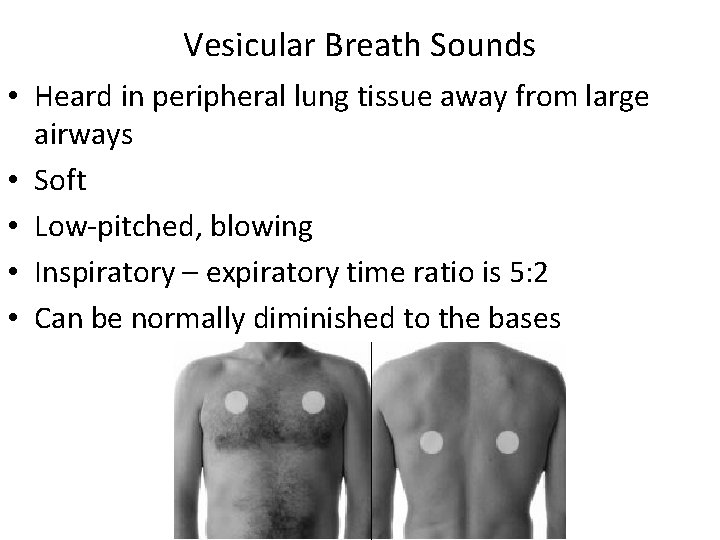
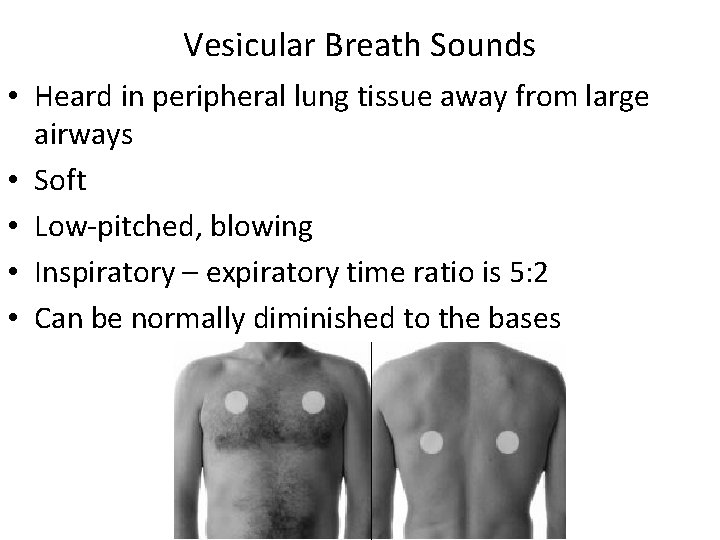
Vesicular Breath Sounds • Heard in peripheral lung tissue away from large airways • Soft • Low-pitched, blowing • Inspiratory – expiratory time ratio is 5: 2 • Can be normally diminished to the bases
Adventitious Breath Sounds • Adventitious breath sounds are superimposed over normal breath sounds • When crackles, wheezes or rubs are heard note loudness, duration, pitch location and whether they are audible with every breath • If possible have patient cough to see if it produces any changes in breath sounds
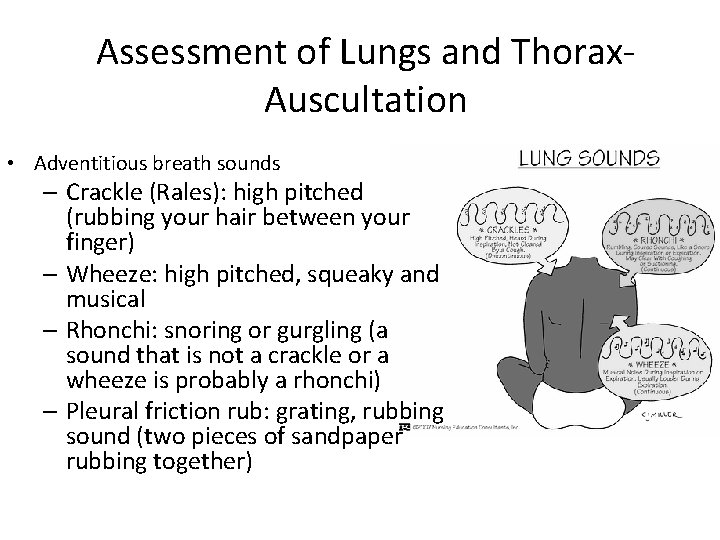
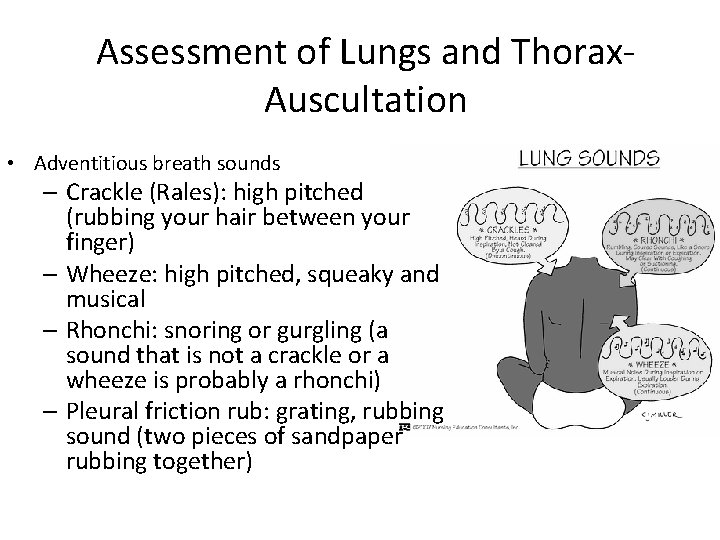
Assessment of Lungs and Thorax. Auscultation • Adventitious breath sounds – Crackle (Rales): high pitched (rubbing your hair between your finger) – Wheeze: high pitched, squeaky and musical – Rhonchi: snoring or gurgling (a sound that is not a crackle or a wheeze is probably a rhonchi) – Pleural friction rub: grating, rubbing sound (two pieces of sandpaper rubbing together)
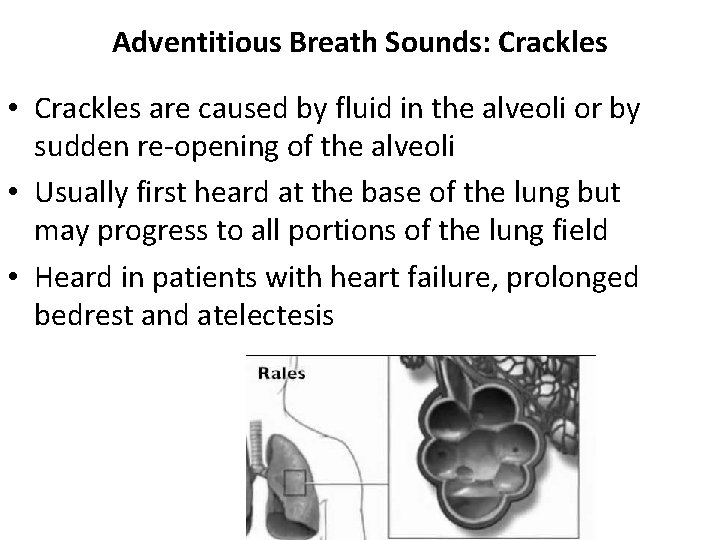
Adventitious Breath Sounds: Crackles • Crackles are caused by fluid in the alveoli or by sudden re-opening of the alveoli • Usually first heard at the base of the lung but may progress to all portions of the lung field • Heard in patients with heart failure, prolonged bedrest and atelectesis
Adventitious Breath Sounds: Wheezes • Caused by rapid air movement through constricted airways • Continuous, often musical sounds • Heard most often on expiration but can be heard during both inspiration and expiration • Usually associated with underlying respiratory disorders such as asthma and obstructive lung disease but can also be caused by interstitial pulmonary edema that compresses small airways • Wheezes that are ‘fixed’ is characteristic of a bronchial mass or tumor
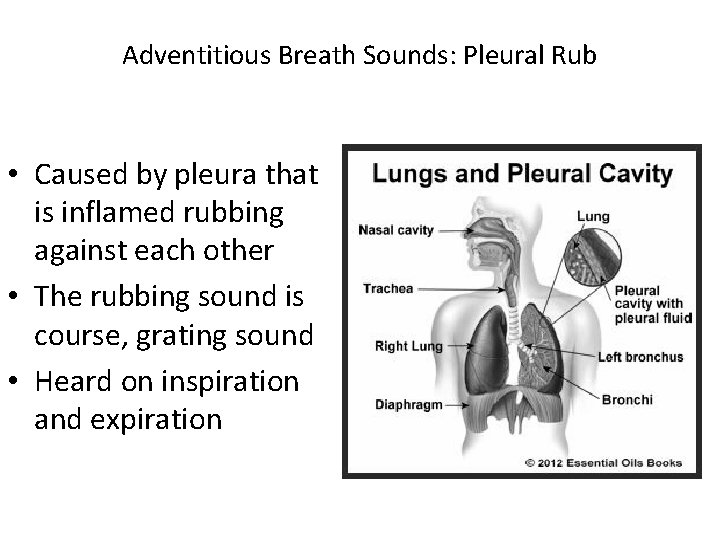
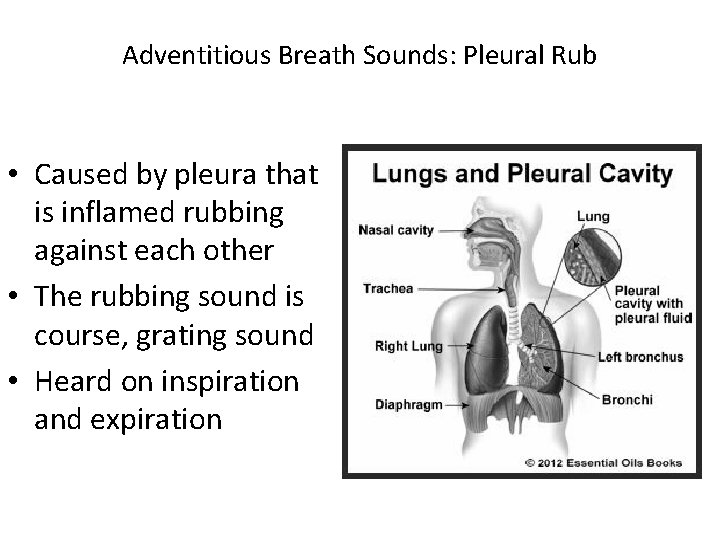
Adventitious Breath Sounds: Pleural Rub • Caused by pleura that is inflamed rubbing against each other • The rubbing sound is course, grating sound • Heard on inspiration and expiration
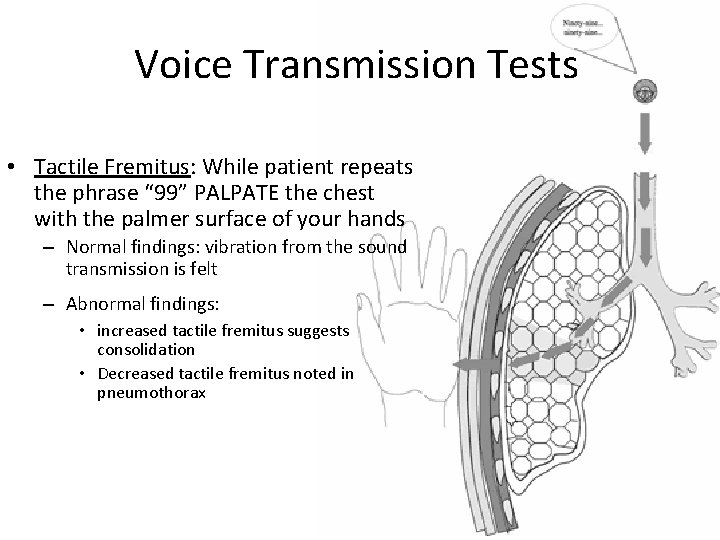
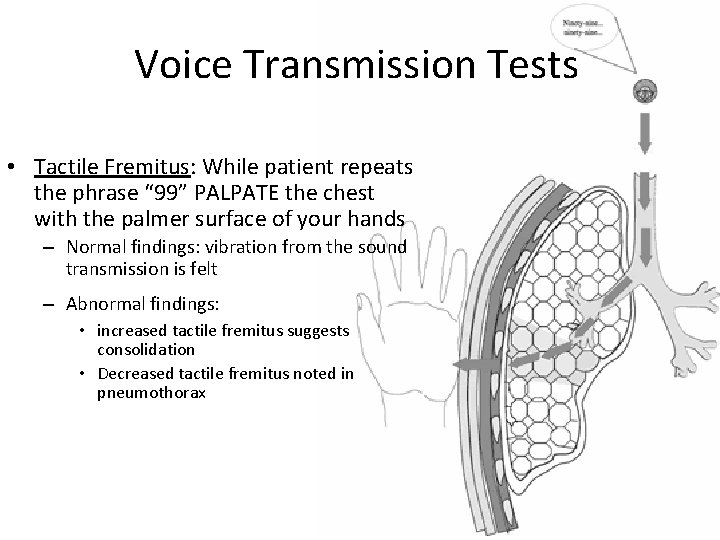
Voice Transmission Tests • Tactile Fremitus: While patient repeats the phrase “ 99” PALPATE the chest with the palmer surface of your hands – Normal findings: vibration from the sound transmission is felt – Abnormal findings: • increased tactile fremitus suggests consolidation • Decreased tactile fremitus noted in pneumothorax
Voice Transmission Tests • Egophony: While patient repeats the phrase “EE” AUSCULTATE the lungs – Normal findings: “EE” heard – Abnormal findings: “AY” heard
Voice Transmission Tests • Bronchophony: While the patient repeats the phrase “ 99” AUSCULTATE the lungs – Normal findings: sounds are muffled and distinct – Abnormal findings: sounds are louder and phrase is clear • Whispered Pectoriloquy: While the patient whispers the phrase “ 1, 2, 3” AUSCULTATE the lungs – Normal findings: faint or no sound – Abnormal findings: phrase is clearly heard or loud
Other Indicators of Respiratory Adequacy • Skin and mucous membranes: pallor, cyanosis • Clubbing of fingers • Muscle development: weight loss, muscle mass loss • Physical endurance: SOB, DOE
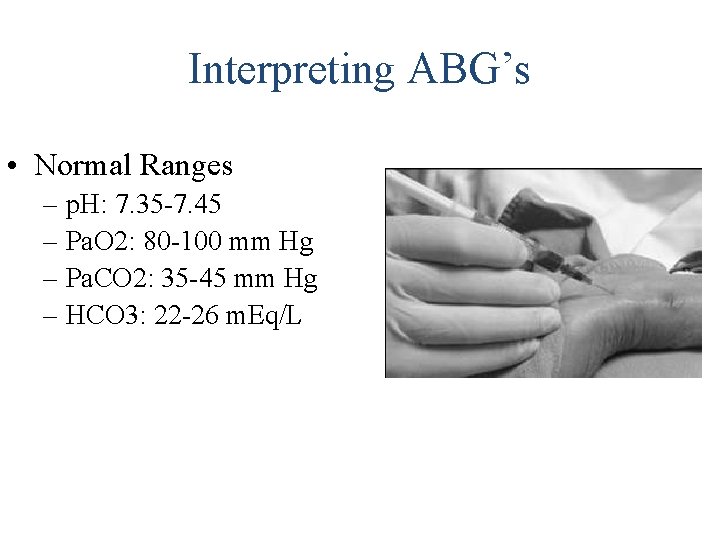
Interpreting ABG’s • Normal Ranges – p. H: 7. 35 -7. 45 – Pa. O 2: 80 -100 mm Hg – Pa. CO 2: 35 -45 mm Hg – HCO 3: 22 -26 m. Eq/L
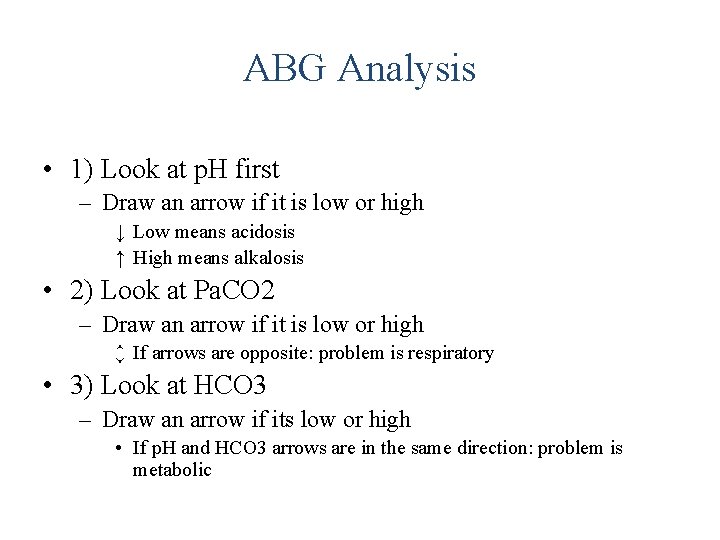
ABG Analysis • 1) Look at p. H first – Draw an arrow if it is low or high ↓ Low means acidosis ↑ High means alkalosis • 2) Look at Pa. CO 2 – Draw an arrow if it is low or high ↕ If arrows are opposite: problem is respiratory • 3) Look at HCO 3 – Draw an arrow if its low or high • If p. H and HCO 3 arrows are in the same direction: problem is metabolic
ABG Analysis • Additional Analysis – Compensation: If the arrows of Pa. CO 2 and HCO 3 are opposite – Partial Compensation: If the arrows of Pa. CO 2 and HCO 3 are in the same direction
Diagnostic Studies • Blood Studies – Hemoglobin – Hematocrit – Arterial Blood Gas • Oximetry – Noninvasive monitor Sp. O 2 and Sv. O 2
Diagnostic Studies • Sputum Studies – Culture and Sensitivity • Identifies infecting organism • Confirms diagnosis – Observe for color, blood, volume, viscosity
Diagnostic Studies • Skin Tests – Allergic reactions – Exposure to tuberculosis – Antigen • Positive- has been exposed • induration
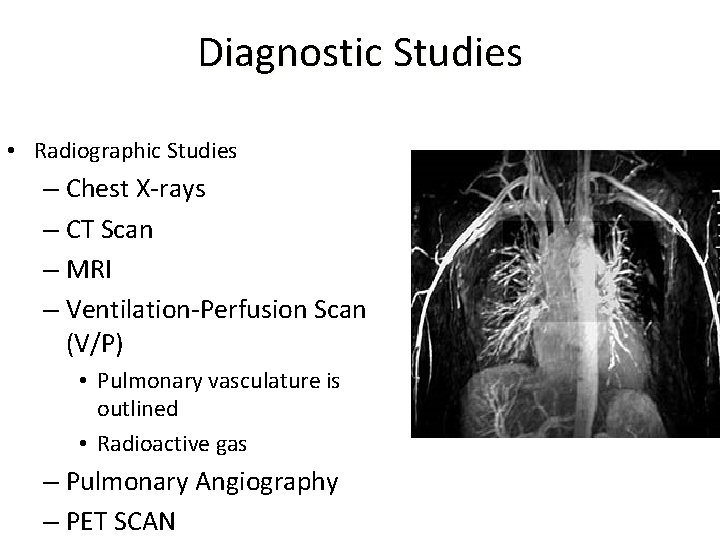
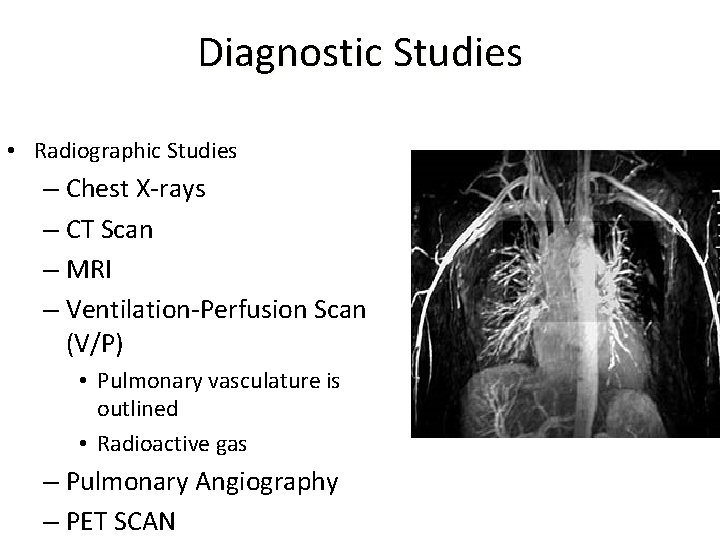
Diagnostic Studies • Radiographic Studies – Chest X-rays – CT Scan – MRI – Ventilation-Perfusion Scan (V/P) • Pulmonary vasculature is outlined • Radioactive gas – Pulmonary Angiography – PET SCAN
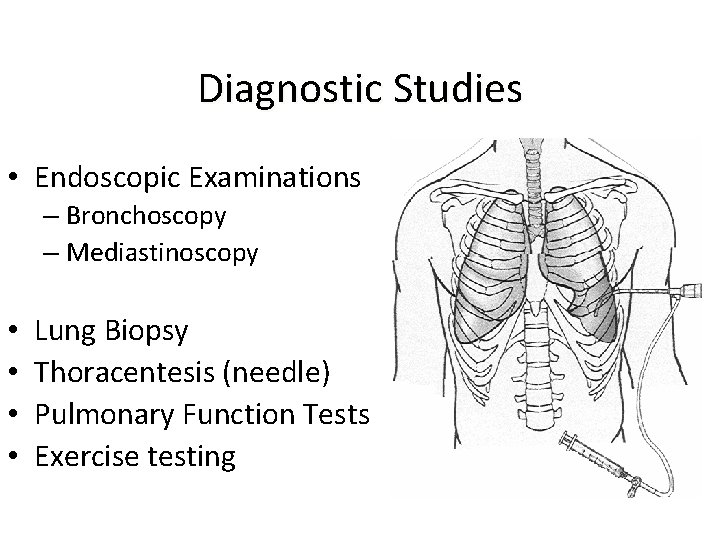
Diagnostic Studies • Endoscopic Examinations – Bronchoscopy – Mediastinoscopy • • Lung Biopsy Thoracentesis (needle) Pulmonary Function Tests Exercise testing