Assessing Decision Making Capacity Within Healthcare Erin M






- Slides: 54
Assessing Decision Making Capacity Within Healthcare Erin M. Miles, Psy. D. , HSPP August 9, 2019
Objectives What is Neuropsychology? What does a Neuropsychological Evaluation Involve? History of Consent and Capacity within a Healthcare Setting Practical ways for non clinical providers to assess capacity Other Relevant Forms of Capacity
Neuropsychology Defined Neuropsychology is the study of how the brain affects an individual’s behavior, emotions, and abilities. When an illness or injury has been diagnosed or identified, it is important to determine exactly what functions or abilities have been affected. This will help answer questions concerning returning to work or school, safe driving, independent living, emotional problems, and how to treat any of these difficulties. A Neuropsychological Evaluation is used to diagnose learning disabilities, attention deficit disorders, autism, and dementing illnesses such as Alzheimer’s disease. The effects of traumatic brain injury, stroke, tumors, or seizures on cognitive, social, and emotional functioning can also be determined. The neuropsychologist often helps people adapt to life changes as a result of chronic illnesses, injuries, or other medical conditions.
Common Referral Questions Does a person have dementia? If so, what is the likely cause based on the testing pattern? Are they safe to live alone? Pseudodementia? Guardianship? Are they safe to drive? Can the person manage their own medications, finances, medical care? Placement (alone, assisted living, nursing home) Determine level of impairment to be able to suggest appropriate therapies/medications

What Does the Neuropsychological Evaluation Involve? Initial meeting: Educational history Establishing Social history Medical history Current Hx a baseline medications and treatment of head injury, concussion, stroke or seizure Psychiatric history Current symptoms Level of functioning with ADL/IADL Determine what tests to order
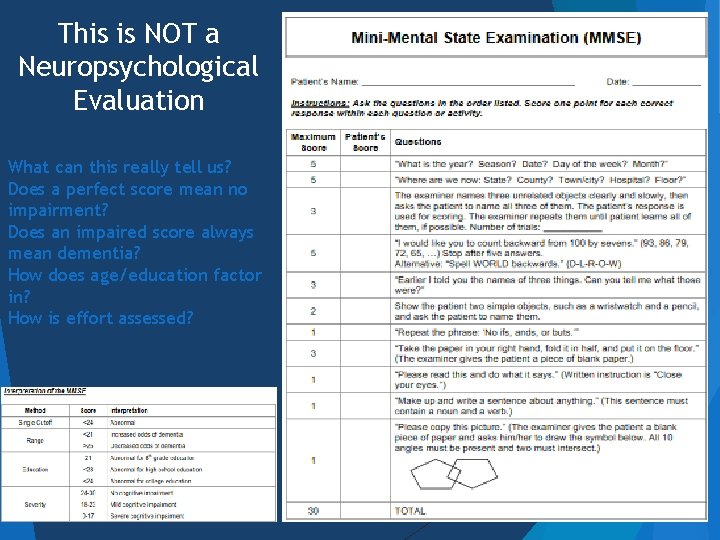
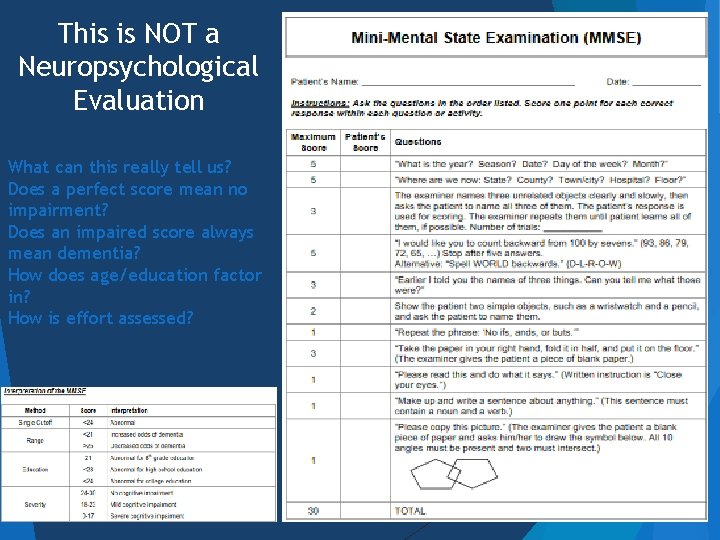
This is NOT a Neuropsychological Evaluation What can this really tell us? Does a perfect score mean no impairment? Does an impaired score always mean dementia? How does age/education factor in? How is effort assessed?

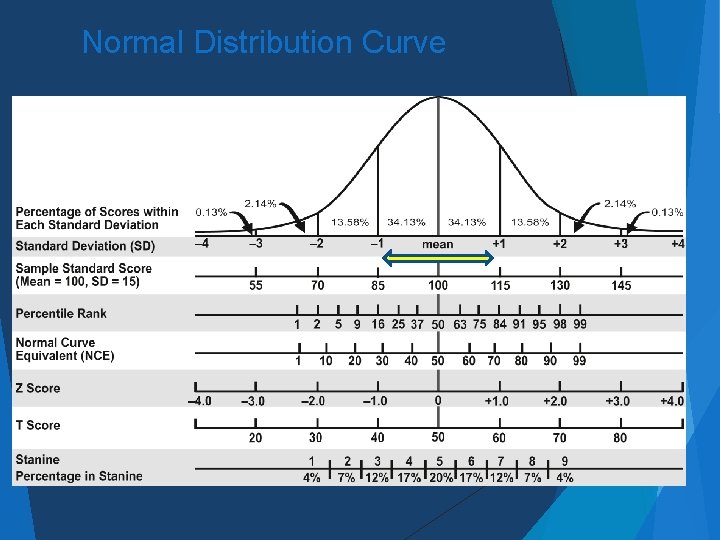
Neuropsychological Testing The appointment for neuropsychological testing involves working one-on-one with the neuropsychologist or, more regularly, a trained technician or intern under his or her supervision. Testing can last anywhere from one to six hours depending on the nature and extent of problems and the request of the referring physician. Testing for dementia in the elderly usually does not last more than an hour and a half (possibly even less) Scores are based on age and at times education level, race and sex
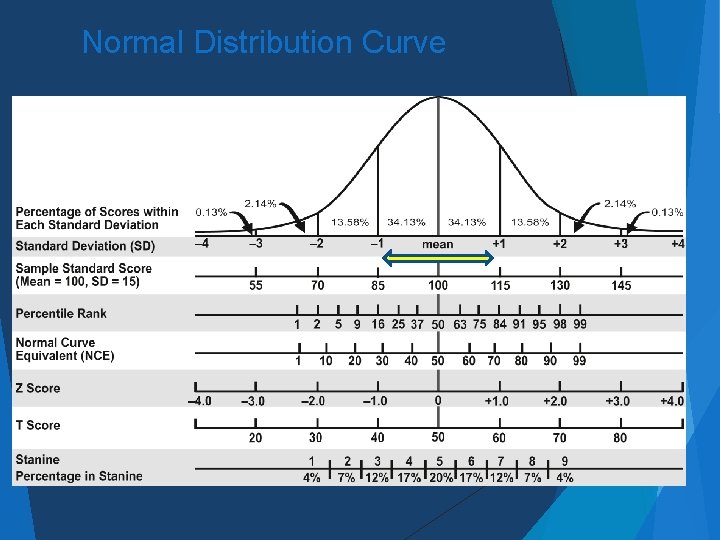
Normal Distribution Curve
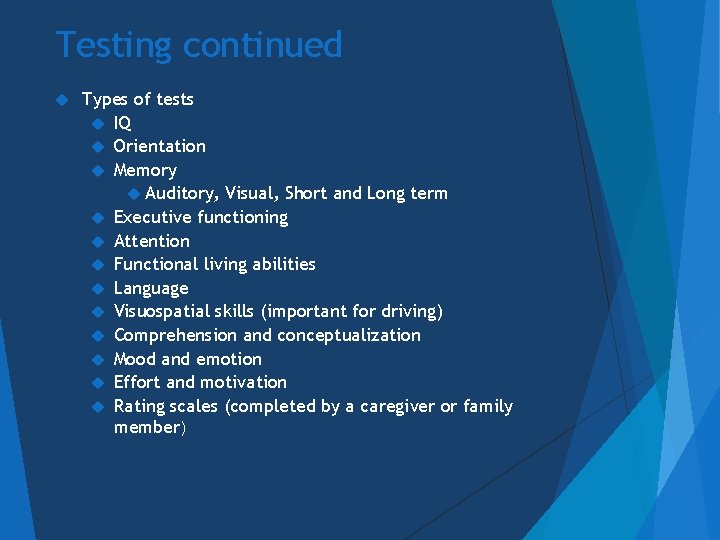
Testing continued Types of tests IQ Orientation Memory Auditory, Visual, Short and Long term Executive functioning Attention Functional living abilities Language Visuospatial skills (important for driving) Comprehension and conceptualization Mood and emotion Effort and motivation Rating scales (completed by a caregiver or family member)
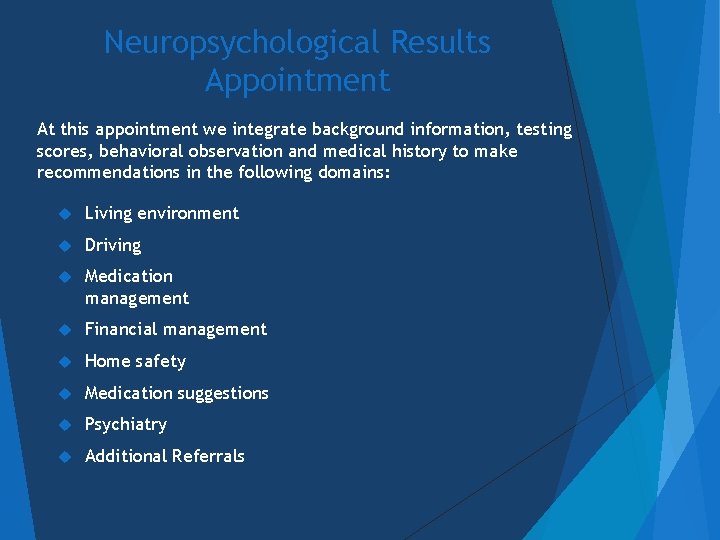
Neuropsychological Results Appointment At this appointment we integrate background information, testing scores, behavioral observation and medical history to make recommendations in the following domains: Living environment Driving Medication management Financial management Home safety Medication suggestions Psychiatry Additional Referrals
Dementia, Delirium & Anosognosia
Common Conditions that Affect Capacity Dementia Traumatic Brain Injury Intellectual Disability Severe psychiatric conditions Substance Abuse Delirium Medication effects
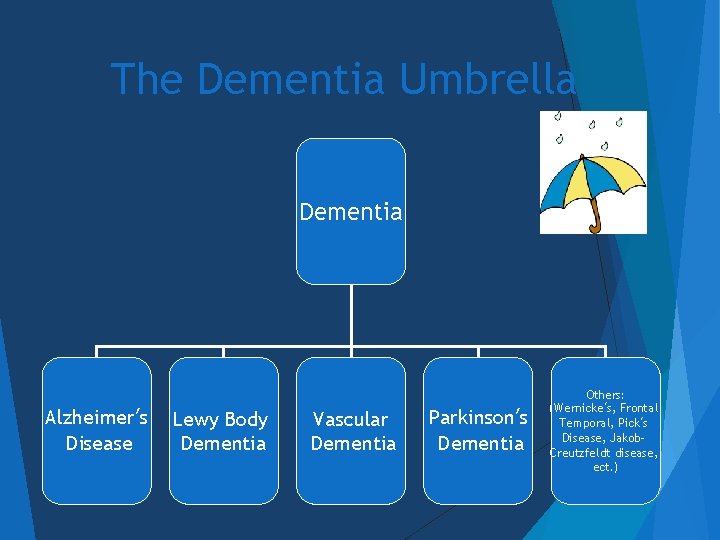
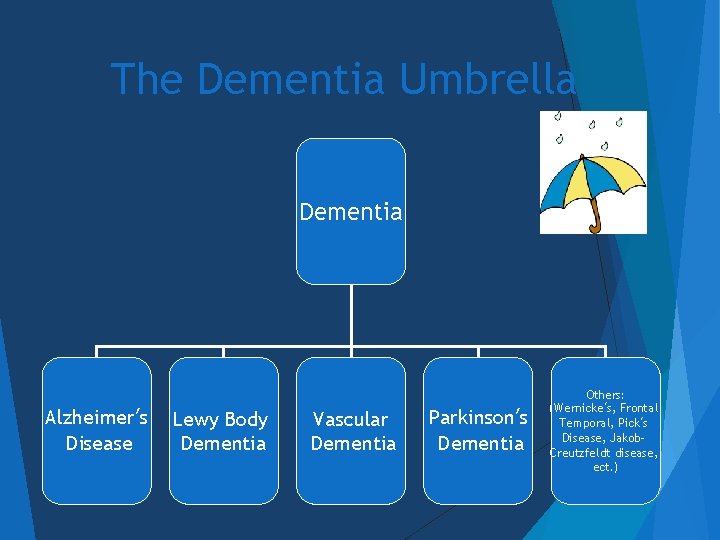
The Dementia Umbrella Dementia Alzheimer’s Disease Lewy Body Dementia Vascular Dementia Parkinson’s Dementia Others: (Wernicke’s, Frontal Temporal, Pick’s Disease, Jakob. Creutzfeldt disease, ect. )
Conditions Where Capacity is Obviously Compromised Unconsciousness Moderate to Severe Intellectual Disability Non communicative by any medium Delirious state Psychotic state Significant Dementia (what is significant? !!)
“Treatable” Dementia Medication reactions Metabolic abnormalities Nutritional deficiencies Pseudo-dementia Infection Normal-pressure hydrocephalus *Capacity determination should always be after the treatable causes have been addressed
Anosognosia

History: Consent to Treat
Informed Consent Informed consent has 3 elements 1) Consent must be voluntarily provided 2) The patient must be provided with sufficient knowledge in order to be able to make a decision 3) The patient must have the capacity to make a competent decision Often what we are really trying to decide is if the person has the capacity to consent Melton, 2007, p. 377
Slater v. Baker & Stapleton (1767) Two physicians were charged with assault and battery for breaking a patient’s healing facture without consent The Judge stated “indeed it is reasonable that a patient should be told what is about to be done to him that he may take courage and put himself in such a situation as to enable him to undergo the operation” Appelbaum et al. , 1987, P. 37
Schloendorff v Society of N. Y. Hospital (1914) Judge Cardozo ruled “every human being of adult years and sound mind has the right to determine what shall be done with his own body and a surgeon who performs an operation without the patient’s consent, commits an assault, for which he is liable in damages” (p. 93) Schloendorff v. Society of New York Hospital, 211 125, 105 NE 92 (NY 1914)
Nuremberg Trials & Nuremberg Code Informed consent would now include research on patients 23 German Physicians (Nazi Germany during WWII) were tried for crimes against humanity for the human experimentation that they conducted The Nuremberg code was written after this trial 15 of the 23 found guilty (7 death sentences) Guidelines for ethical human experiment The code states that participants should be informed of the “nature, duration and purpose of the experiment; the method and means by which it is to be conducted; all inconvenience and hazards reasonably to be expected; and the effects upon his person which may possibly come from his participation in the experiment” Reiser, Dyck, & Curran, 1977, pp. 272 -273; Demakis, 2012
Capacity to Accept or Refuse Treatment Rennie v. Klein (1978)- Involuntary psychiatric commitment does not mean that you do not need consent to medicate Unless the person is a danger to self or others Charles S. Soper, as Director of Newark Developmental center et al. V. Dorothy Storar, 1981 -A guardian cannot refuse a medical lifesaving treatment
Consent & Assent The APA has laid out guidelines for what to do when an individual does not have the capacity to consent 1) Provide an appropriate explanation 2) Seek the individual’s assent 3)Consider such persons’ preference and best interests 4) Obtain appropriate permission from a legally authorized person This should be done with every patient
Capacity Within Healthcare
Competency vs. Capacity is a clinical term based on expert’s opinion- This is often determined by using subjective and objective data/information Capacity refers to the patient’s cognitive abilities, or in the treatment setting, the ability to make a given treatment decision (Rosenfeld, 2004, p 112) Capacity is not always a fixed construct Competency is a legal term that is typically determined by a judge An assessment of capacity may lead to specific judgments of competence by a court

The Million Dollar Question Does the patient have sufficient capacity to make a competent decision? Types of capacity Capacity to Accept or Refuse Treatment Testamentary Capacity Financial Capacity Driving Capacity Independent Living Functional Elements Sexual Consent Capacity Petrila, 2003; (Rosenfeld, 2004, p 112).
Four Core Elements of Capacity to Consent Ability to understand relevant information Ability to appreciate implications of a situation and consequences Ability to rationally manipulate Information Ability to make a consistent choice and express it Roth et al. , 1977
Capacity to Consent to Treat: Understanding Can the person reasonably understand comprehend their condition, treatment options and the implications of failing to treat? Do they understand the risks and benefits of treatment or deciding not to treat? Anosognosia and neurological impairment
Informal ways to assess Understanding Start with the basics: Why are you here today? What medical conditions have you been diagnosed with? What is your doctor treating you for? How do you make sure you do not miss medications/appointments? What do you do if you miss your medication? Can they provide autobiographical information? Can they follow the conversation? Are they constantly talking about the past? Do they have a general understanding of their medical needs and does it line up with what is reported by their physicians?
Capacity to Consent to treat: Appreciation The ability to take what you know and apply it to your own situation For example an individual with Alzheimer’s may actually know a lot about Alzheimer’s but if they cannot apply what they know to their situation they do not have full appreciation Factual knowledge versus seeing their situation for what it truly is
Appreciation Continued Common fallacies of reasoning (anosognosia)-Do the facts line up with perception? “I’ll know when I should stop driving” (studies show that AD patients consistently rate their driving abilities as much better than they actually are) “I never miss taking my medications” “I have no problems taking care of my home” “I shower ever single day” Have you ever tried to reason with someone who holds one of these beliefs? Wild K, Cotrell V. Identifying driving impairment in Alzheimer disease: a comparison of self and observer reports versus driving evaluation. Alzheimer Dis Assoc Disord. 2003; 17: 27– 34. [Pub. Med] [Google Scholar]
Capacity to Consent to Treat: Reasoning Can the person utilize all of the information that you have just given them to be able to make a decision? Weigh options and make comparisons All persons have the “right to folly”-The decision that a patient makes is not the determining factor of if they can reason-what really matters is if they are capable of using a process of reasoning to get to that decision Acceptable reasoning: “I do not wish to keep receiving treatment for cancer. I fully understand that there is no cure and the treatment is prolonging the inevitable. I am in a lot of pain and I have no quality of life” Poor reasoning: “I do not want to keep treating my cancer (even if treatment is likely to be curative) because I need to go home and be with my dog”
Capacity to Consent to Treat: Expression of a Choice Expression by any means Speech, writing, gestures or sign language Can they make a consistent choice and stick to it? Delirium Mental health conditions with fluctuation Aphasia Expressive Receptive Mixed
Recommendations Every effort should be made to allow the person to make a decision regarding their own treatment Clarify the referral question What decision do they need to make? You do not need the same level of capacity to decide if you want a medication for pain compared to which cancer treatment is best Make sure that various attempts have been made to improve comprehension Is there another way that the information could be explained? Visual cues Graphs Simplified explanations
Misconceptions about Mental Capacity Old age means memory & cognitive impairment It is not normal for Grandma to get lost in her own home because she is “old” When impairment is expected with age, family often fail to realize the level of need Certain diagnoses automatically lead to incompetency Many people with cognitive limitations do not have or need a guardian If a person has an average IQ, they have average capacity All individuals with dementia lack capacity Individual variation in severity and progression of dementia is extremely variable Making a bad decision means that a person lacks capacity
Considerations Was an individual born with a certain level of impaired capacity or was it acquired? Down Syndrome vs. Alzheimer’s Are they used to relying on others for assistance or have they lived their entire life independently up until this point? Are they aware of their own limitations or are they unable to see what they cannot do? In my professional experience, patients who were born with an intellectual disability are much more agreeable with receiving help and less likely to require a competency evaluation by the court Understanding the diagnosis as well as the pattern that the disorder typically takes will help to establish if a person has had a change in their decision making capacity
Other Forms of Capacity
Testamentary Capacity The mental or legal capacity to make or alter a will You can maintain testamentary capacity even if a guardian has been assigned This form of capacity is less restrictive than others Do they: Understand the consequences of executing a will? Know the nature of what will be included in the will? Know who will be receiving their assets once the will is executed? Possess the ability to make a decision consistent to what they would have done before a diagnosis? (Demakis, 2012)
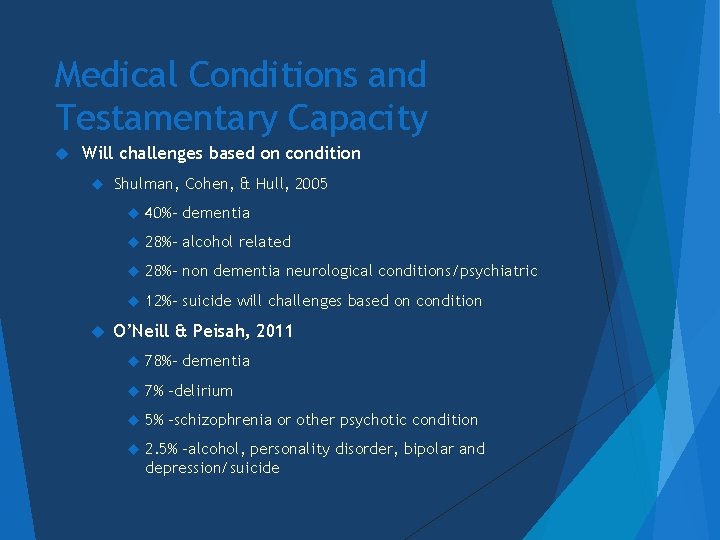
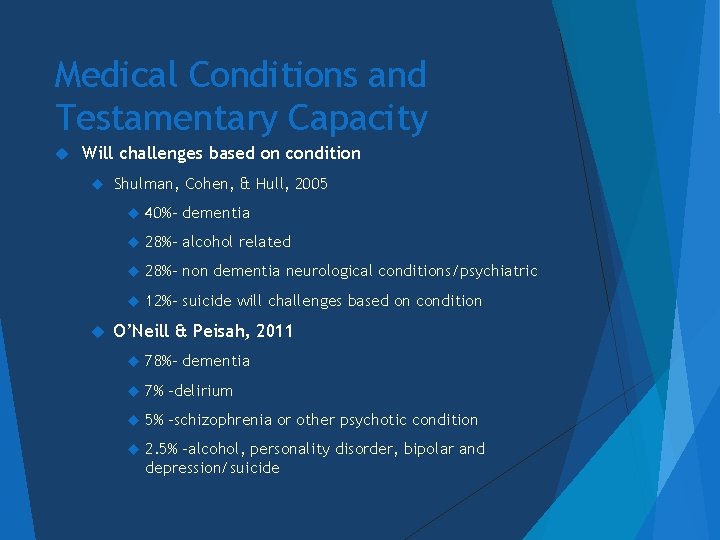
Medical Conditions and Testamentary Capacity Will challenges based on condition Shulman, Cohen, & Hull, 2005 40%- dementia 28%- alcohol related 28%- non dementia neurological conditions/psychiatric 12%- suicide will challenges based on condition O’Neill & Peisah, 2011 78%- dementia 7% -delirium 5% -schizophrenia or other psychotic condition 2. 5% -alcohol, personality disorder, bipolar and depression/suicide
Example: Testamentary Capacity Elderly female diagnosed early stage Alzheimer’s Disease (memory scores in the severely impaired range) Following diagnosis (probably years after the disease actually began) caregiver had her alter her will so that they would be the beneficiary Family members contacted a lawyer and APS to argue that she did not have the capacity to make such a decision Everyone agreed that she was receiving excellent care and that her funds were being utilized appropriately Based on her neuropsychological assessment it was advised that she did not have the capacity to appreciate the nature of the choice she had made She was functioning at a level that made her susceptible to manipulation
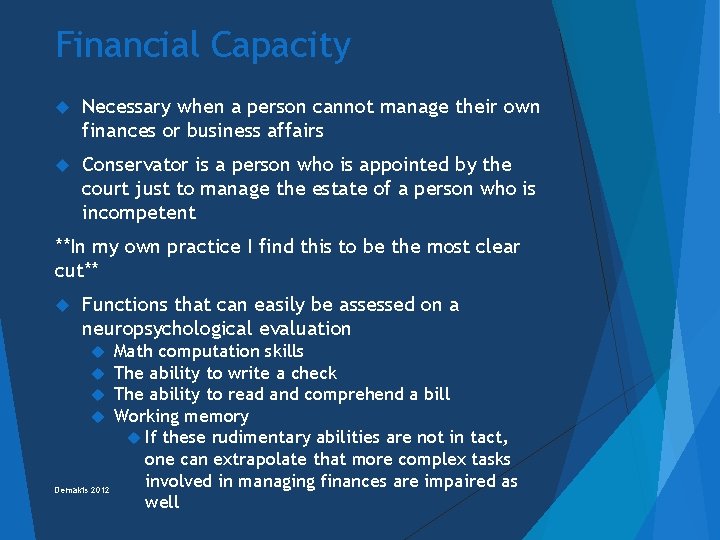
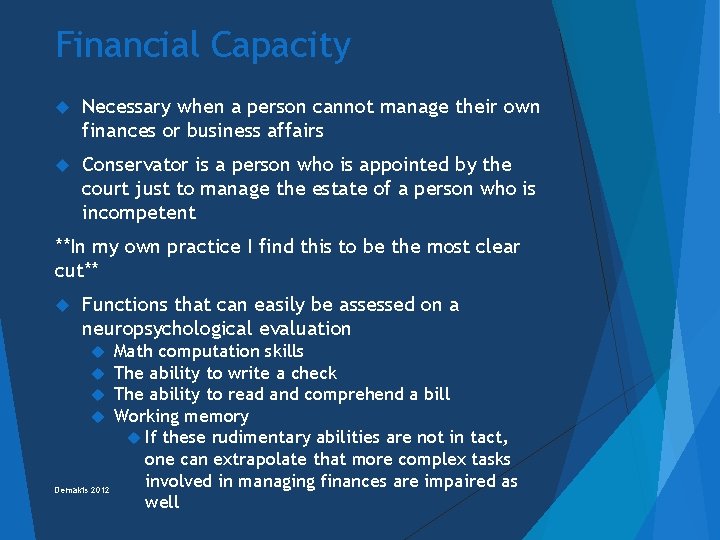
Financial Capacity Necessary when a person cannot manage their own finances or business affairs Conservator is a person who is appointed by the court just to manage the estate of a person who is incompetent **In my own practice I find this to be the most clear cut** Functions that can easily be assessed on a neuropsychological evaluation Math computation skills The ability to write a check The ability to read and comprehend a bill Working memory If these rudimentary abilities are not in tact, one can extrapolate that more complex tasks involved in managing finances are impaired as Demakis 2012 well
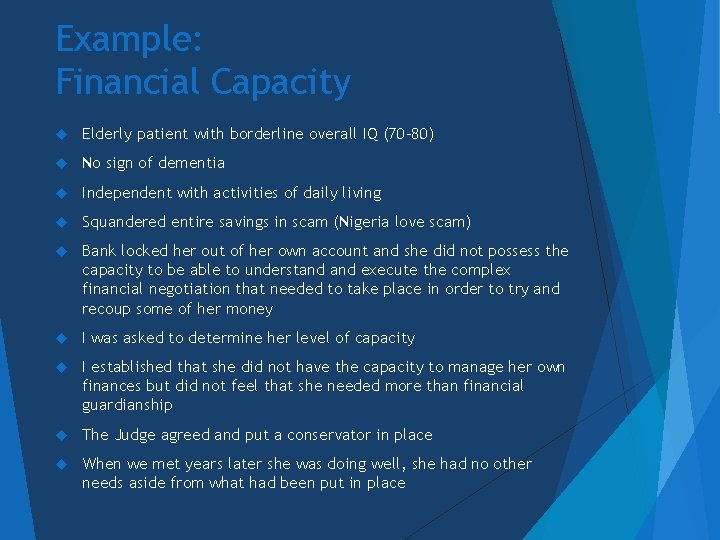
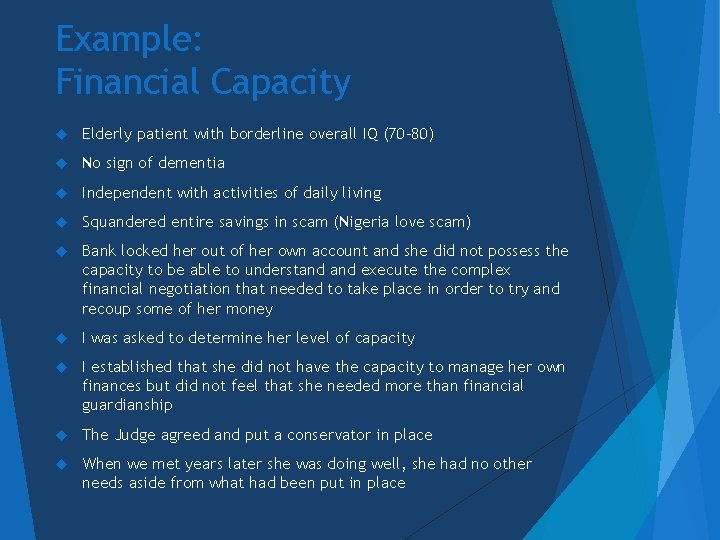
Example: Financial Capacity Elderly patient with borderline overall IQ (70 -80) No sign of dementia Independent with activities of daily living Squandered entire savings in scam (Nigeria love scam) Bank locked her out of her own account and she did not possess the capacity to be able to understand execute the complex financial negotiation that needed to take place in order to try and recoup some of her money I was asked to determine her level of capacity I established that she did not have the capacity to manage her own finances but did not feel that she needed more than financial guardianship The Judge agreed and put a conservator in place When we met years later she was doing well, she had no other needs aside from what had been put in place

Capacity to Live Independently Activities of Daily Living Dressing, grooming, toileting, hygiene, transferring, eating Instrumental Activities of Daily Living Medication management, finances, cooking, laundry, housekeeping, shopping, communication (telephone) Neuropsychological tests are not always the best way to measure activities of daily living There is not always a direct correlation between ADL abilities and cognitive scores Moderate stage dementia but able to maintain hygiene and a clean personal space Borderline to Mild stage dementia but cannot manage very basic skills such as dressing In my experience personality style and past patterns play a large role Physical, Speech & Occupational Therapists are often better equipped to make determinations in this domain Direct observation is best
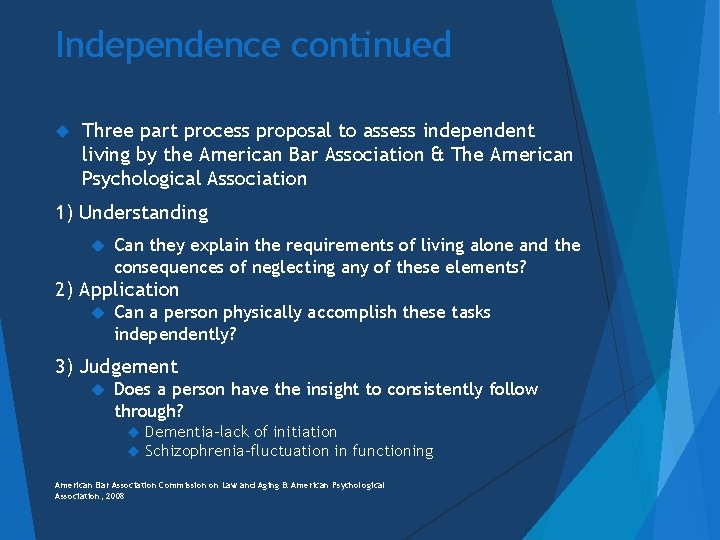
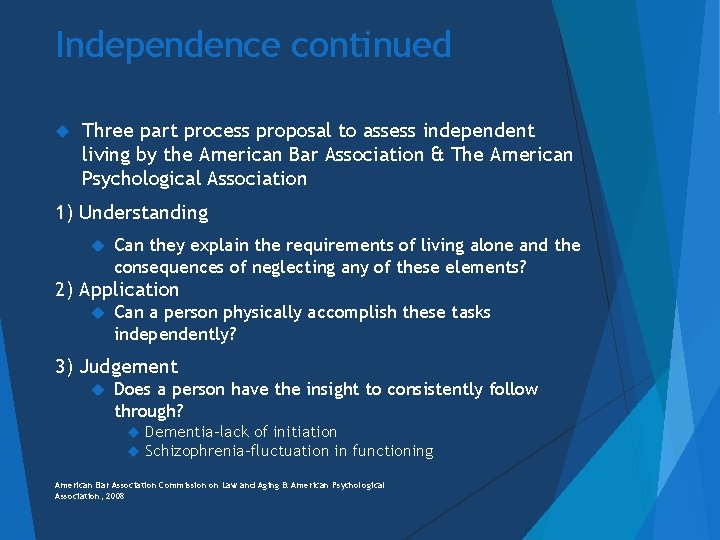
Independence continued Three part process proposal to assess independent living by the American Bar Association & The American Psychological Association 1) Understanding Can they explain the requirements of living alone and the consequences of neglecting any of these elements? 2) Application Can a person physically accomplish these tasks independently? 3) Judgement Does a person have the insight to consistently follow through? Dementia-lack of initiation Schizophrenia-fluctuation in functioning American Bar Association Commission on Law and Aging & American Psychological Association, 2008
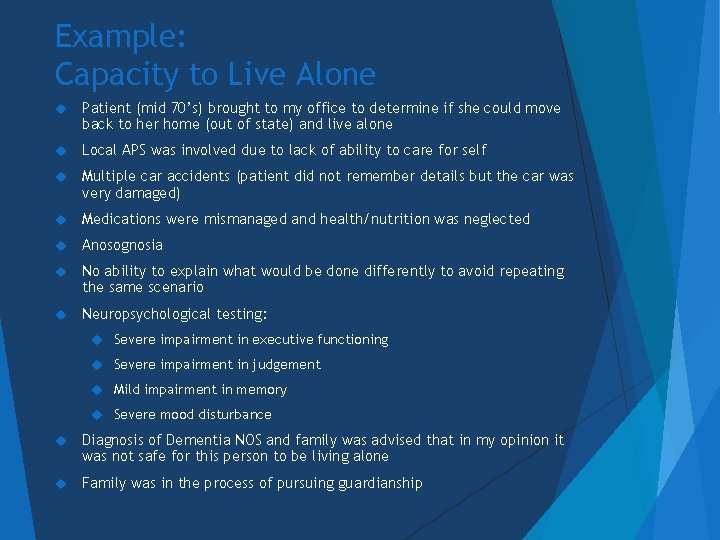
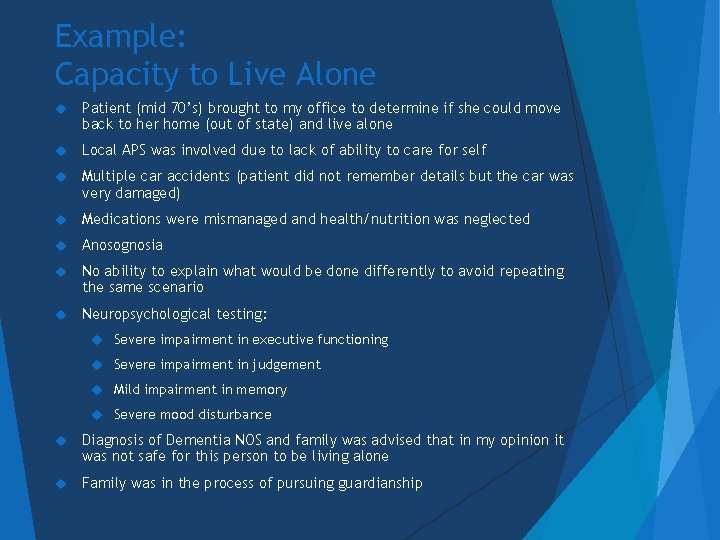
Example: Capacity to Live Alone Patient (mid 70’s) brought to my office to determine if she could move back to her home (out of state) and live alone Local APS was involved due to lack of ability to care for self Multiple car accidents (patient did not remember details but the car was very damaged) Medications were mismanaged and health/nutrition was neglected Anosognosia No ability to explain what would be done differently to avoid repeating the same scenario Neuropsychological testing: Severe impairment in executive functioning Severe impairment in judgement Mild impairment in memory Severe mood disturbance Diagnosis of Dementia NOS and family was advised that in my opinion it was not safe for this person to be living alone Family was in the process of pursuing guardianship
Example: Capacity to Live Alone Patient in early 80’s with reported memory problems Family visits each day Short term memory loss was the biggest concern Absence of wandering, confusion or difficulty with ADL’s Family already helping with finances and patient was not driving Patient able to accurately discuss his difficulties with memory Neuropsychological Testing Average executive functioning Average problem solving abilities Low Average attention Mild impairment in both immediate and delayed memory Average language abilities Lack of dyspraxias Diagnosis: Mild Cognitive Impairment Based on all of the available information I did not feel that it was unsafe for this person to continue to live alone with the supports that were in place
Driving Capacity Driving is a privilege not a right Various medical and mental conditions can impact driving Visual impairment Neurological Intellectual disability Traumatic Brain Injury Dementia Seizure Stroke Psychiatric Schizophrenia Psychosis Alcoholism Medications Physical limitations Arthritis Parkinson's Disease Orthopedic injuries
Occupational Therapy Driving Evaluation Examples “Patient crossed left of center on well marked roadways and/or consistently drove on the yellow line” “Patient demonstrated decreased divided attention, stopping one time unnecessarily at a green traffic light. The patient demonstrated no awareness of a near-miss rear end collision directly behind us due to the unanticipated action. ” In this instance the evaluator had to take control of the vehicle to avoid a collision “Patient demonstrated excessive and unnecessary deceleration prior to changing lanes causing confusion for other roadway users” “Patient attempted to merge with other traffic, but did not visually scan. As a result, patient nearly collided with another vehicle. ” Evaluator had to take control of vehicle to avoid collision in this instance as well Therapeutic Mobility Services
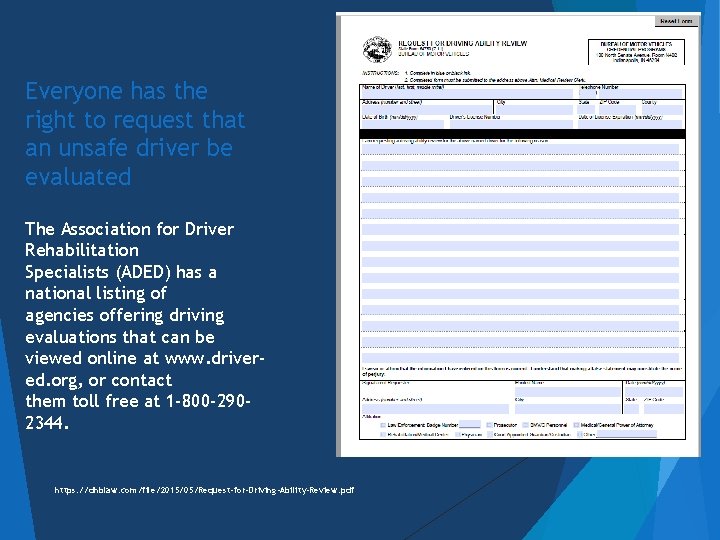
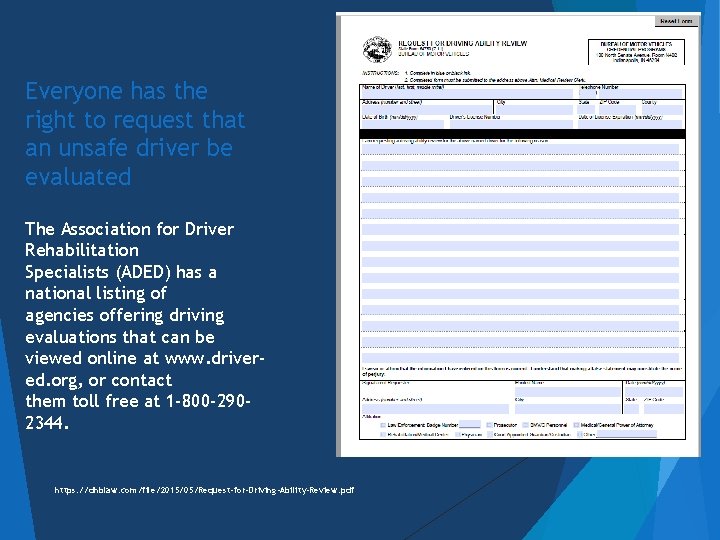
Everyone has the right to request that an unsafe driver be evaluated The Association for Driver Rehabilitation Specialists (ADED) has a national listing of agencies offering driving evaluations that can be viewed online at www. drivered. org, or contact them toll free at 1 -800 -2902344. https: //dhblaw. com/file/2015/05/Request-for-Driving-Ability-Review. pdf
Sexual Capacity There are no universally accepted criteria for what constitutes the ability to consent to sexual relations Proposed Criteria include: (1) Knowledge of relevant information, including risks and benefits; (2) understanding or rational reasoning that reveals a decision that is consistent with the individual’s values (competence); and (3) voluntariness (a stated choice without coercion) (Grisso, 2003; Kennedy, 1999; Stavis, 1991;
Helpful Resources -Assessment of Older Adults with Diminished Capacity: A Handbook for Psychologists © American Bar Association Commission on Law and Aging – American Psychological Association https: //www. apa. org/pi/aging/programs/assessment/capacity-psychologist-handbook. pdf -Adult Protective Service State hotline: 800 -992 -6978 -The Association for Driver Rehabilitation Specialists (ADED) has a national listing of agencies offering driving evaluations that can be viewed online at www. driver-ed. org, or contact them toll free at 1 -800 -290 -2344. -Aging and In-Home Services of Northeast Indiana 2927 Lake Avenue Fort Wayne, IN 46805 -5414 260 -745 -1200 or 800 -552 -3662 FAX 260 -422 -4916 E-mail: info@agingihs. org
References Assessment of Older Adults with Diminished Capacity: A Handbook for Psychologists© American Bar Association Commission on Law and Aging – American Psychological Association (2008) American Bar Association Commission on Law and Aging & American Psycholocial Association, (2008). Assessment of older adults with dimished capacity: A handbook for psychologists. Washington, D. C. : American Bar Association Commission on Law and Aging. American Psychological Association. Appelbaum, P. S. , & Grisso, T. (1988). Assessing patients’ capacities to consent to treatment. New England Journal of Medicine, 319, 1635 -1638. Appelbaum, P. S, Lidz, C W. , & Meisel, A (1987). Informed Consent: Legal theory and clinical practice. New York: Oxford University Press. Charles S. Soper, as Director of Newark Developmental Center et al. Dorothy Storar, N. Y. , 420 N. E. 2 d 64, 1981. Demakis, G. J. , (2012). Civil Capacities in Clinical Neuropsychology. Research Findings and Practical Applications. New York: Oxford University Press. Melton, G. B. , Petrilla, J. , Poythress, N. G. , & Slobogin, C. Psychological evaluations for the courts. New York: The Guilford Press. Petrilla, J. (2003). The emerging debate over the shape of informed consent: Can the doctrine bear the weight? Behavioral Sciences and the Law, 21, 121 -133. Reiser, S. J. , Dyck, A. J. , & Curran, W. J (1977). Ethics in medicine: Historical perspectives and contemporary concerns. Cambridge, MA: The MIT Press. Rennie v. Klein, 462 F Supp 1131(D NJ, 1978), 476 F Supp 1294 (D NJ, 1979), affirmed in part 653 F 2 d 836 (3 rd Cir, 1981), vacated and remanded, 102 S Ct 3505 (1982), 700 F 2 d 266 (3 rd Cir, 1983). Roth, L. H. , Meisel, A. , & Lids, C. W. (1977). Tests of competence to consent to treatment. American Journal of Psychiatry, 134, 279 -284. Slater v. Baker & Stapelton, 95 860 (Eng. 1767) Schloendorff v. Society of New York Hospital, 211 125, 105 NE 92 (NY 1914)
Ronald N. Williams, Ph. D. , HSPP, ABN - Neuropsychology Tasha H. Williams, Ph. D. , HSPP, ABPd. N - Neuropsychology Christina Stemmler, Psy. D. , HSPP - Neuropsychology Erin M. Miles, Psy. D. , HSPP - Neuropsychology Jacob Lutz, Ph. D. , HSPP – Neuropsychology Peter Dodzik, Psy. D. , HSPP, ABN, ABPd. N - Neuropsychology https: //www. fwneuropsych. com
