Assessing Decision Making Capacity in Adult Protective Services
- Slides: 59
Assessing Decision Making Capacity in Adult Protective Services Clients Jason Schillerstrom, MD schillerstr@uthscsa. edu
Learning Objectives �Describe the process of decisional capacity assessments. �Understand the reluctance of some primary care physicians to evaluate capacity. �Describe the relationship between executive function and self-care abilities.
Scope of the problem and risk assessment
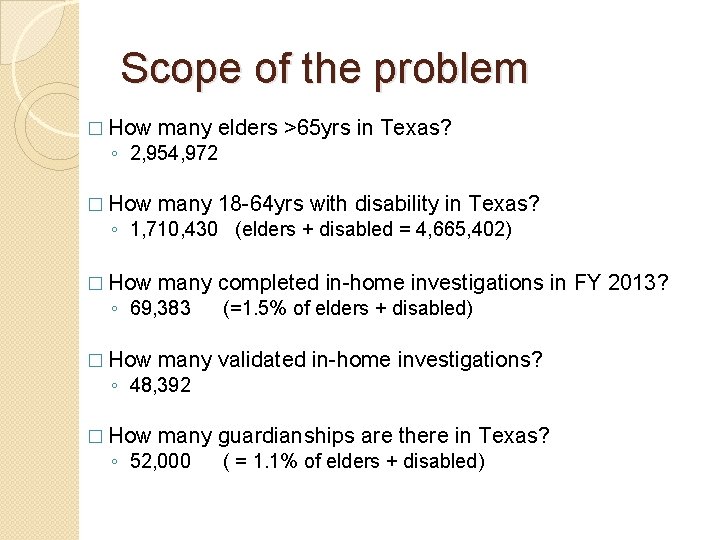
Scope of the problem �How many elders >65 yrs in Texas? �How many 18 -64 yrs with disability in Texas? �How many completed in-home investigations in FY 2013? �How many validated in-home investigations? �How many guardianships are there in
Scope of the problem � How many elders >65 yrs in Texas? � How many 18 -64 yrs with disability in Texas? � How many completed in-home investigations in FY 2013? ◦ 2, 954, 972 ◦ 1, 710, 430 (elders + disabled = 4, 665, 402) ◦ 69, 383 (=1. 5% of elders + disabled) � How many validated in-home investigations? � How many guardianships are there in Texas? ◦ 48, 392 ◦ 52, 000 ( = 1. 1% of elders + disabled)
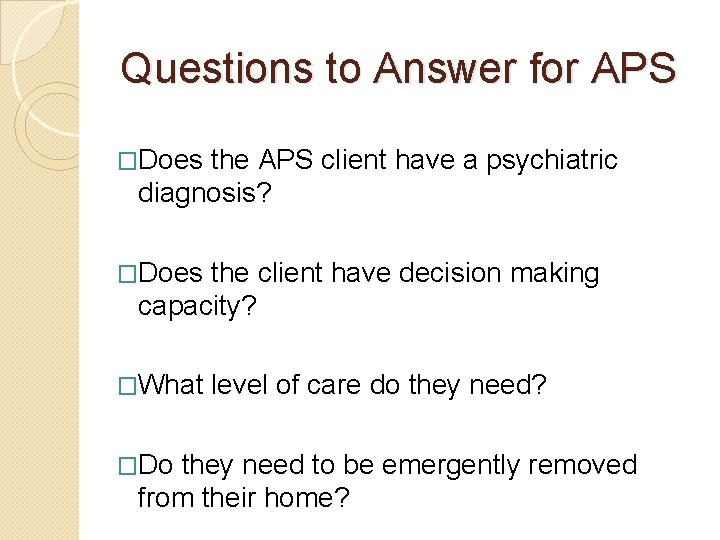
Questions to Answer for APS �Does the APS client have a psychiatric diagnosis? �Does the client have decision making capacity? �What �Do level of care do they need? they need to be emergently removed from their home?
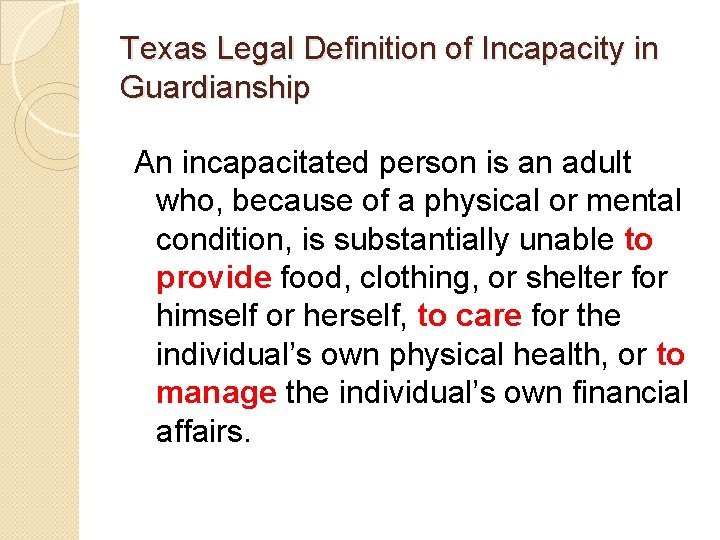
Texas Legal Definition of Incapacity in Guardianship An incapacitated person is an adult who, because of a physical or mental condition, is substantially unable to provide food, clothing, or shelter for himself or herself, to care for the individual’s own physical health, or to manage the individual’s own financial affairs.
Texas Legal Definition of Incapacity in Guardianship An incapacitated person is an adult who, because of a physical or mental condition, is substantially unable to provide food, clothing, or shelter for himself or herself, to care for the individual’s own physical health, or to manage the individual’s own financial affairs.
Ethical, Legal, or Clinical Issues to Consider First � Should the client be notified that I am coming? � Should the client be informed about the purpose of my evaluation? � How much information should I get from APS? Are they biasing my assessment? � Should the capacity assessment be completed by a physician unknown to the client (me) or the client’s physician?
Decisional Capacity and the Primary Care Physician • Is the PCP the best person to do the evaluation? • Should the PCP have to do the capacity evaluation? • What are reasons the PCP may not want to do the evaluation?
PCP’s and Capacity Determinations � No compensation � Risk of subpoena � Little training in capacity assessments and not a routine assignment � These assessments are very different from the medical model � Potential fracturing of the doctor-patient relationship
Scientific Dilemmas? �How reliable is IADL self report? Proxy report? �What is the best way to measure functional status in these cases? �What cognition(s) are essential to functional and decisional capacity?
Which Cognitive Functions are most Essential to Decisional Capacity? �Memory �Orientation �Language �Math �Visuospatial �Executive Function
Executive Function �That set of cognitive processes that allow one to act independent of the environment instead of displaying behaviors mediated by the environment. �When executive processes deteriorate, people become dependent on habits and routine.
Executive Screens �Verbal Fluency Task ◦ FAS - >10 words in 1 minute �Verbal Trailmaking Task ◦ Past “ 5 E”
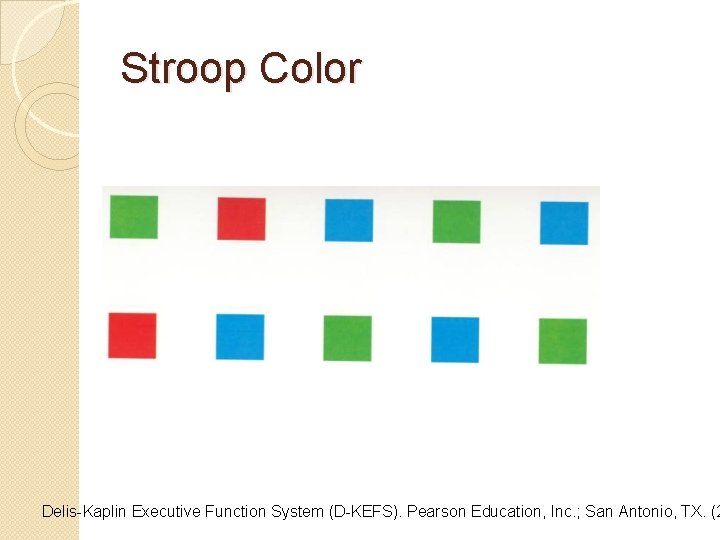
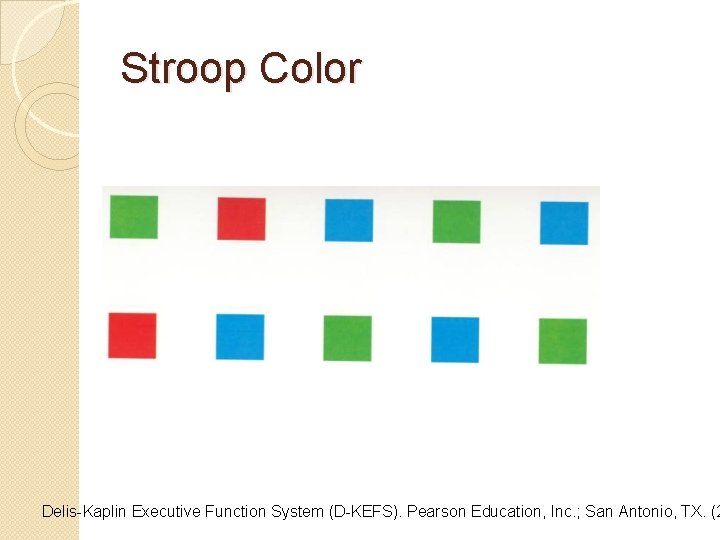
Stroop Color Delis-Kaplin Executive Function System (D-KEFS). Pearson Education, Inc. ; San Antonio, TX. (2
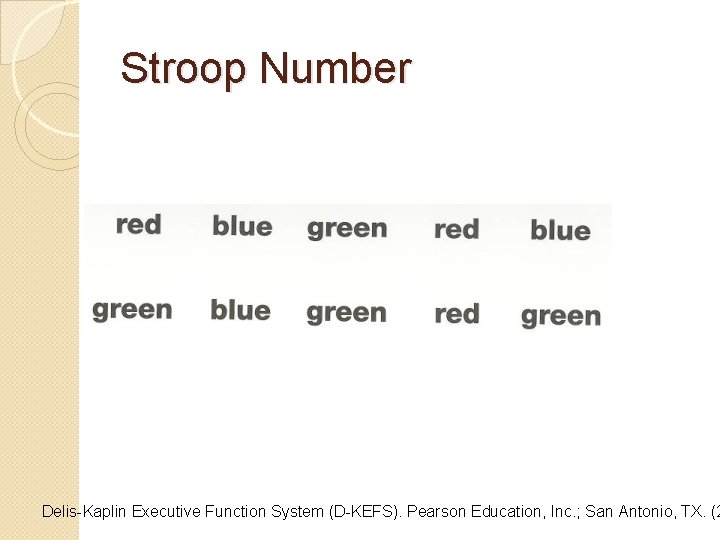
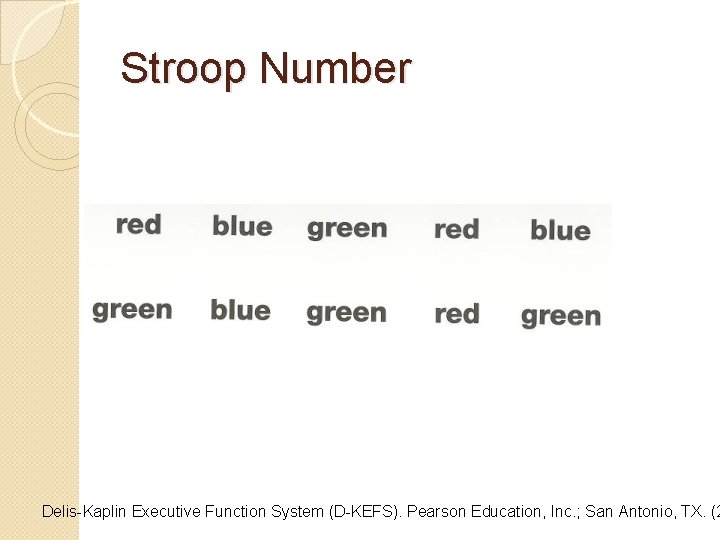
Stroop Number Delis-Kaplin Executive Function System (D-KEFS). Pearson Education, Inc. ; San Antonio, TX. (2
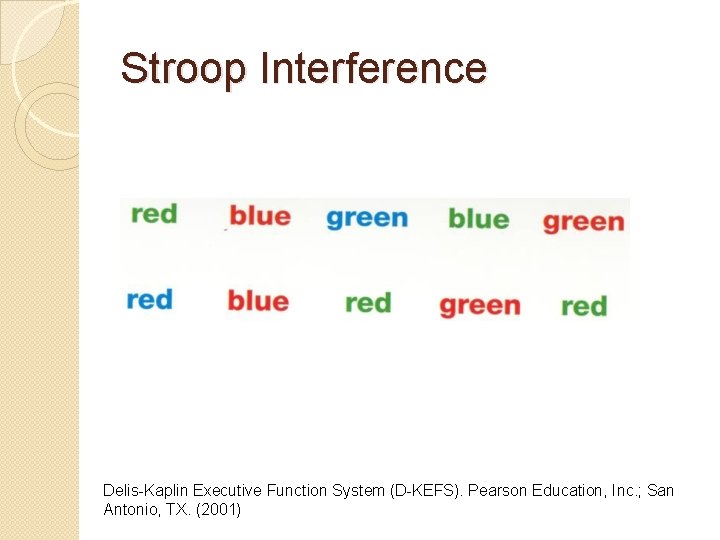
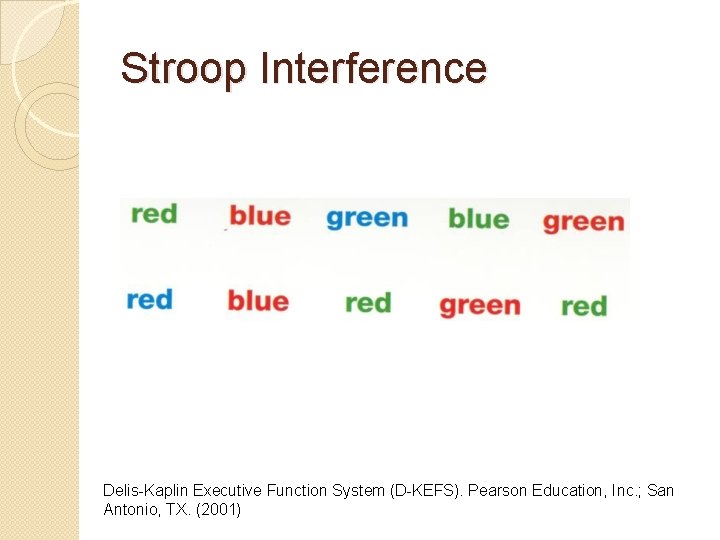
Stroop Interference Delis-Kaplin Executive Function System (D-KEFS). Pearson Education, Inc. ; San Antonio, TX. (2001)
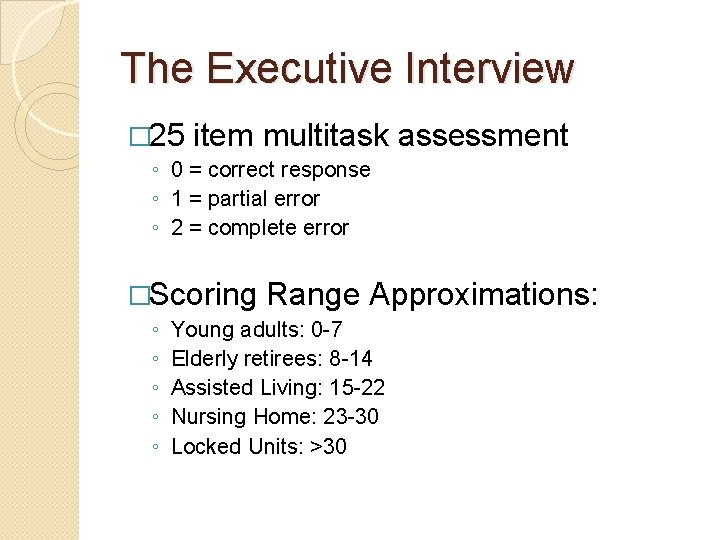
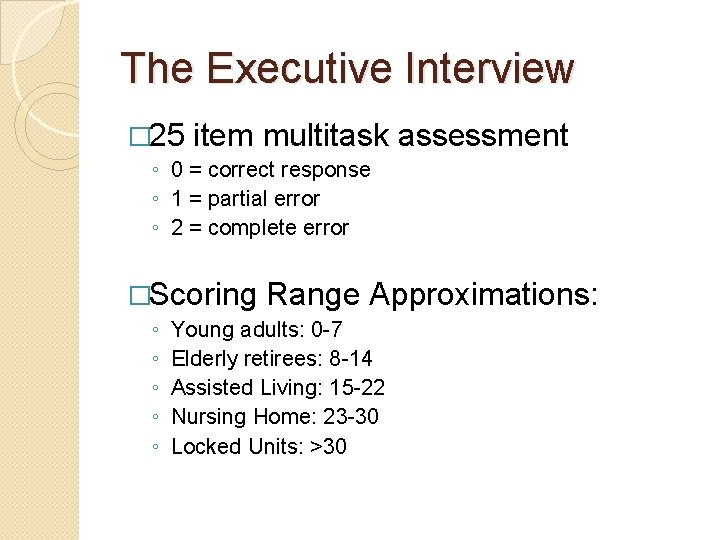
The Executive Interview � 25 item multitask assessment ◦ 0 = correct response ◦ 1 = partial error ◦ 2 = complete error �Scoring ◦ ◦ ◦ Range Approximations: Young adults: 0 -7 Elderly retirees: 8 -14 Assisted Living: 15 -22 Nursing Home: 23 -30 Locked Units: >30
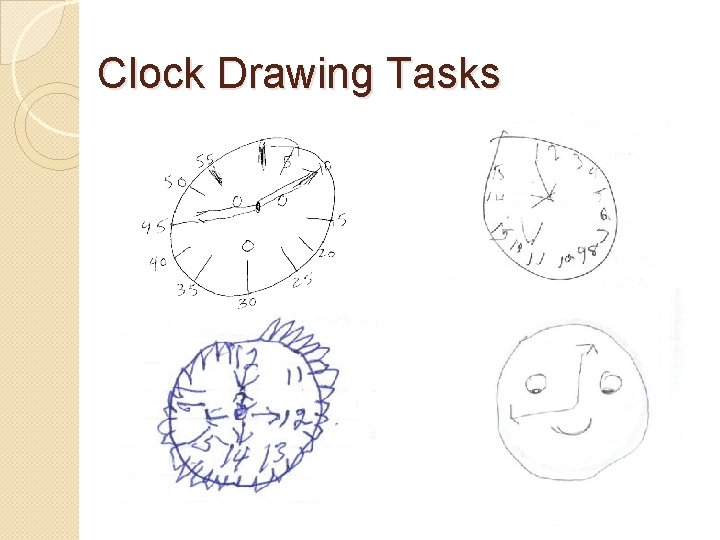
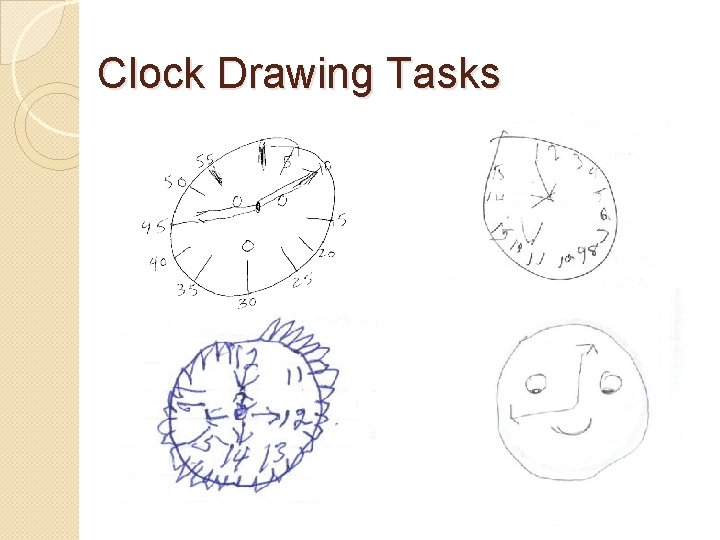
Clock Drawing Tasks
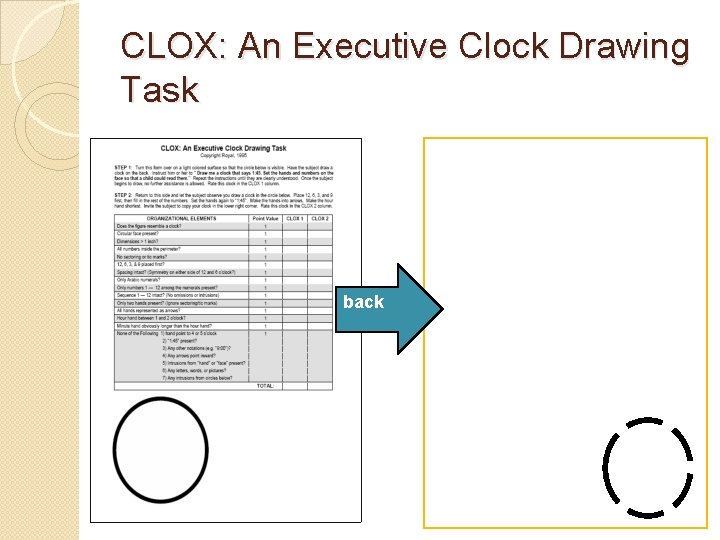
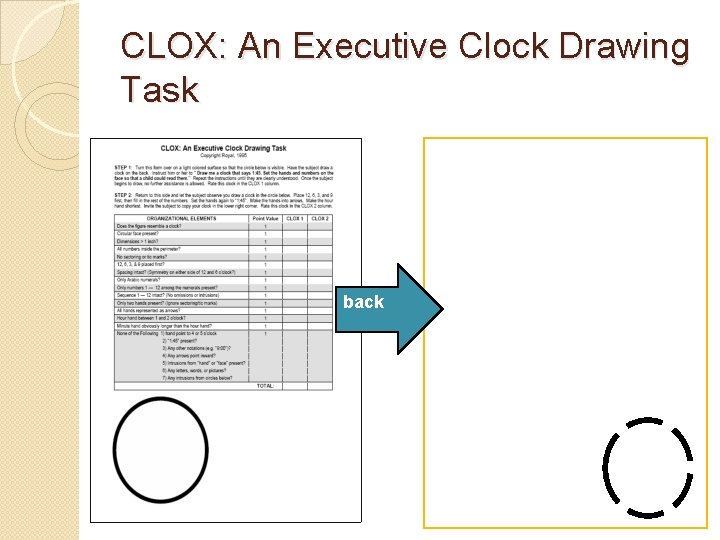
CLOX: An Executive Clock Drawing Task back
Instructions: CLOX 1 1) Place the blank (back) side of the CLOX form in front of the subject. 2) State “Draw me a clock that says 1: 45. Set the hands and numbers on the face so that a child could read them. ” 3) Once the subject begins the task, no further assistance is allowed (i. e. no prompting or repeat instructions). State “Sir/Ma’am, it’s up to you” for each question.
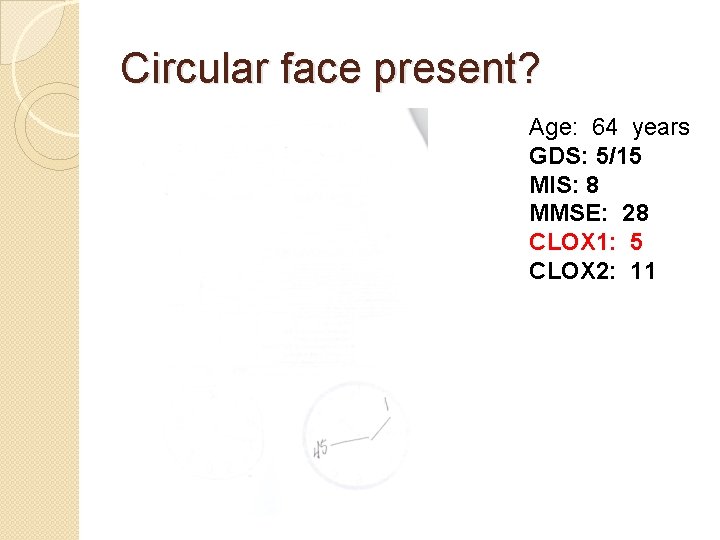
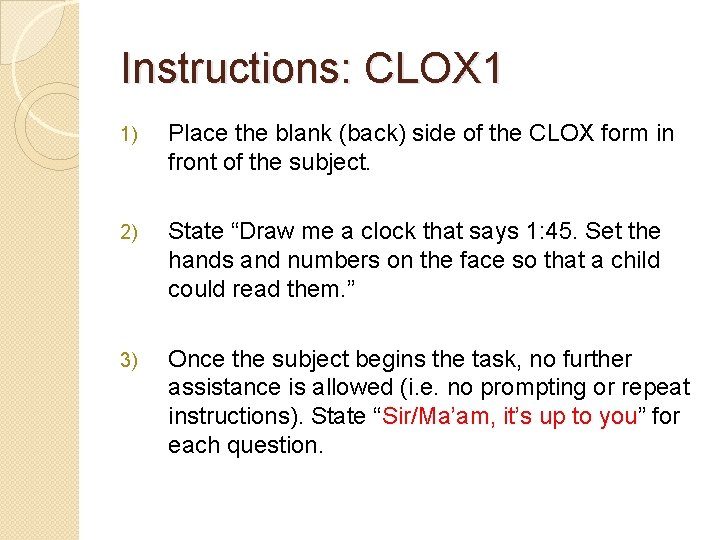
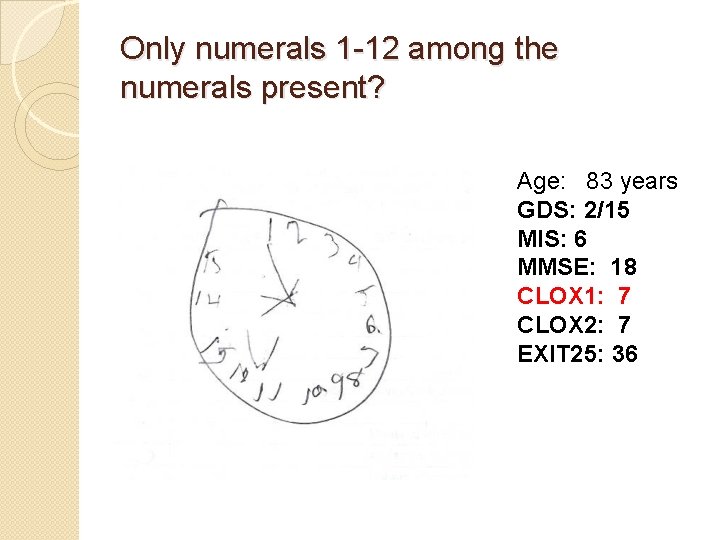
Circular face present? Age: 64 years GDS: 5/15 MIS: 8 MMSE: 28 CLOX 1: 5 CLOX 2: 11
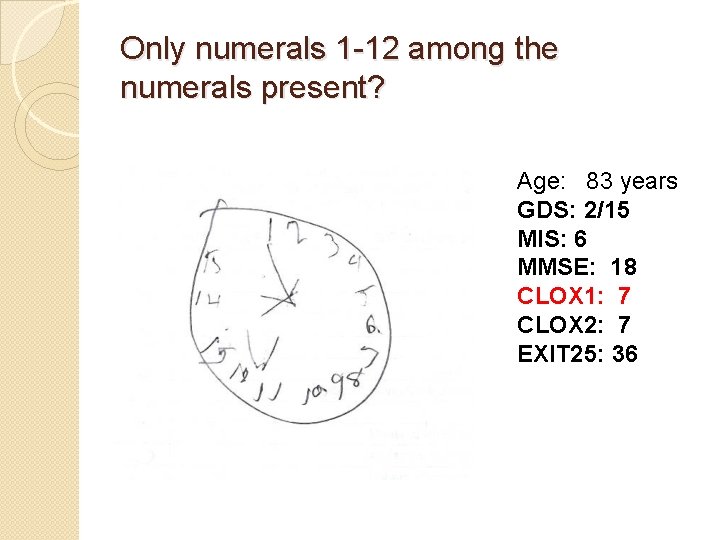
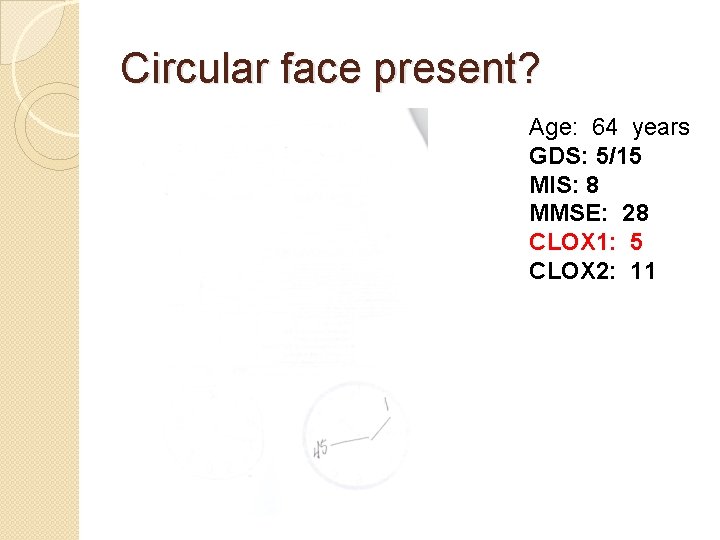
Only numerals 1 -12 among the numerals present? Age: 83 years GDS: 2/15 MIS: 6 MMSE: 18 CLOX 1: 7 CLOX 2: 7 EXIT 25: 36
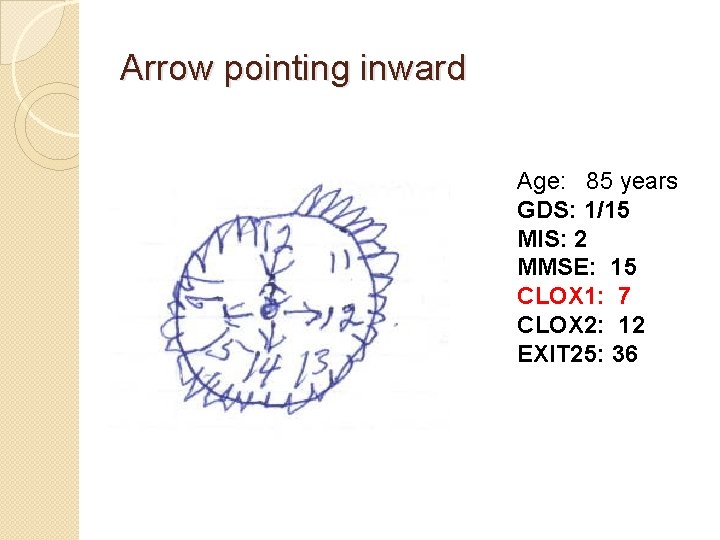
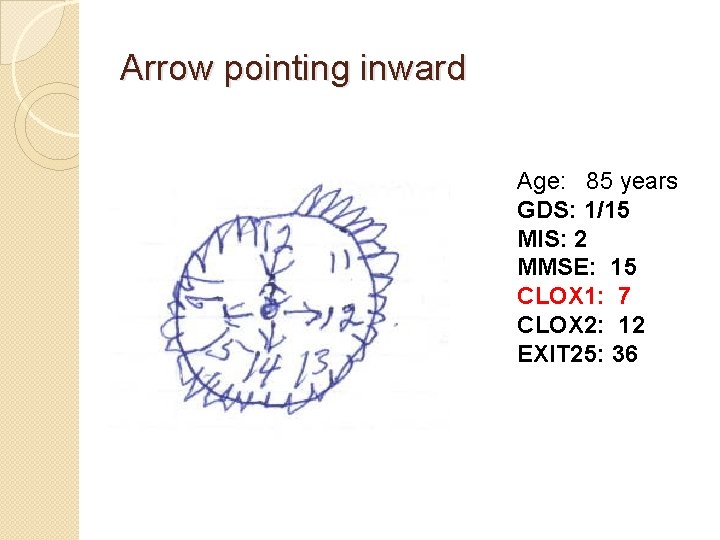
Arrow pointing inward Age: 85 years GDS: 1/15 MIS: 2 MMSE: 15 CLOX 1: 7 CLOX 2: 12 EXIT 25: 36
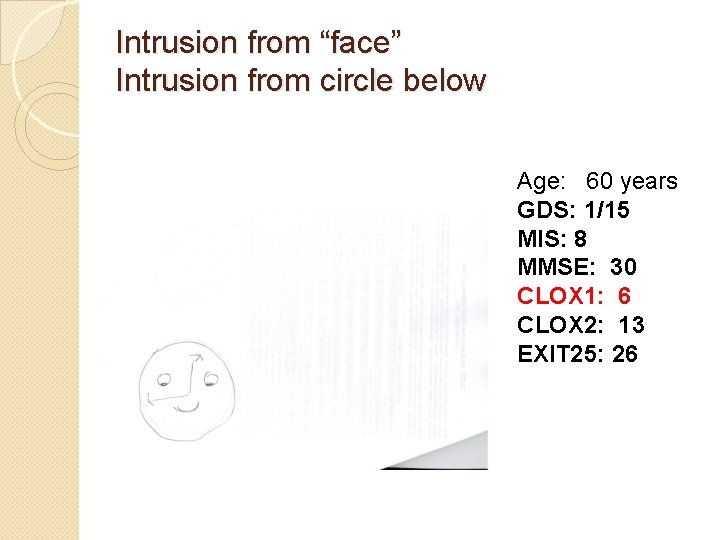
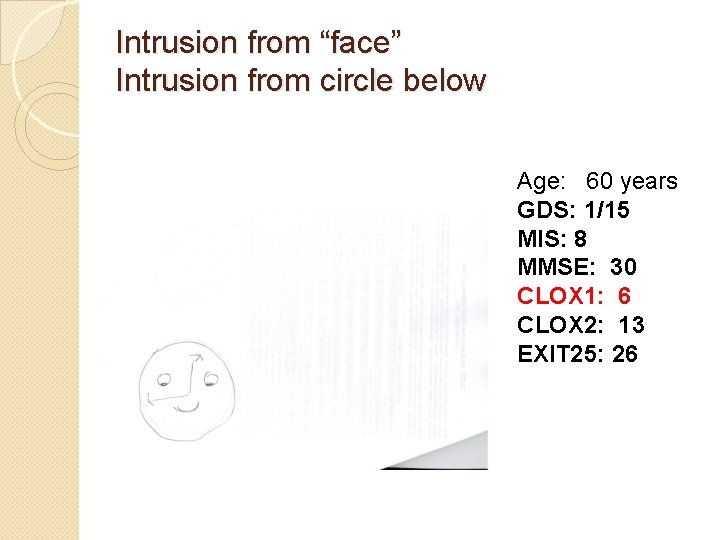
Intrusion from “face” Intrusion from circle below Age: 60 years GDS: 1/15 MIS: 8 MMSE: 30 CLOX 1: 6 CLOX 2: 13 EXIT 25: 26
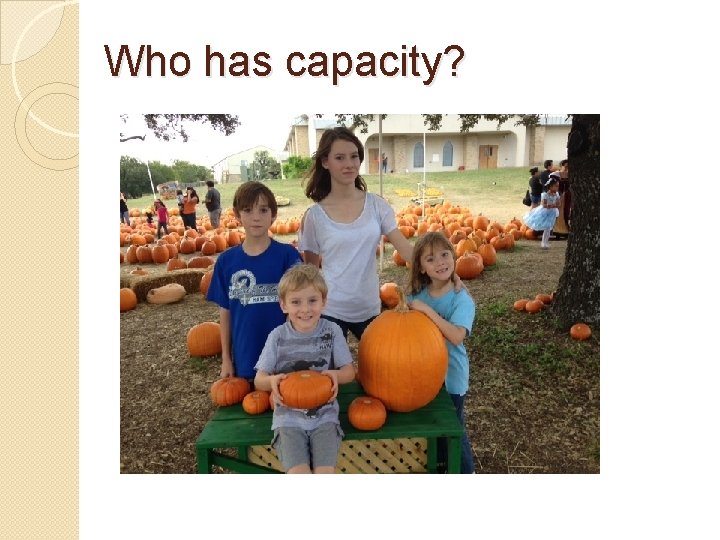
Who has capacity?
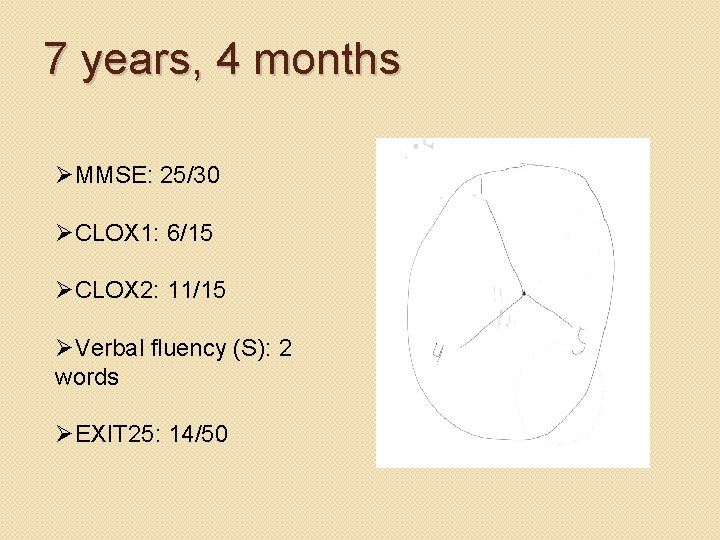
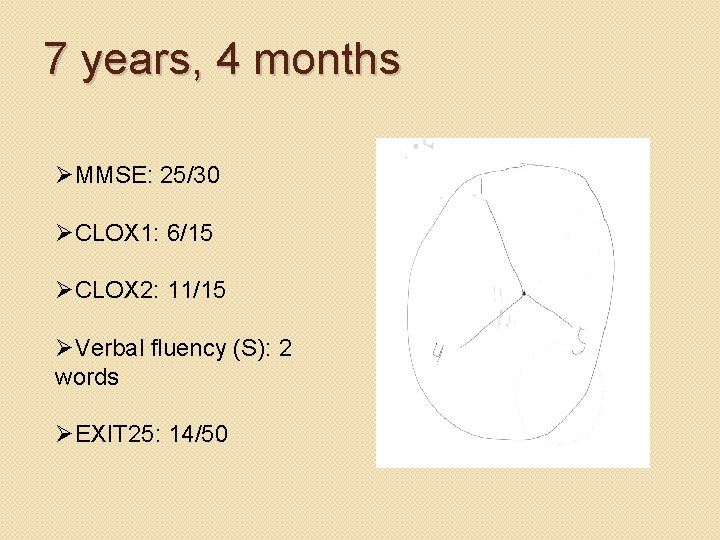
7 years, 4 months ØMMSE: 25/30 ØCLOX 1: 6/15 ØCLOX 2: 11/15 ØVerbal fluency (S): 2 words ØEXIT 25: 14/50
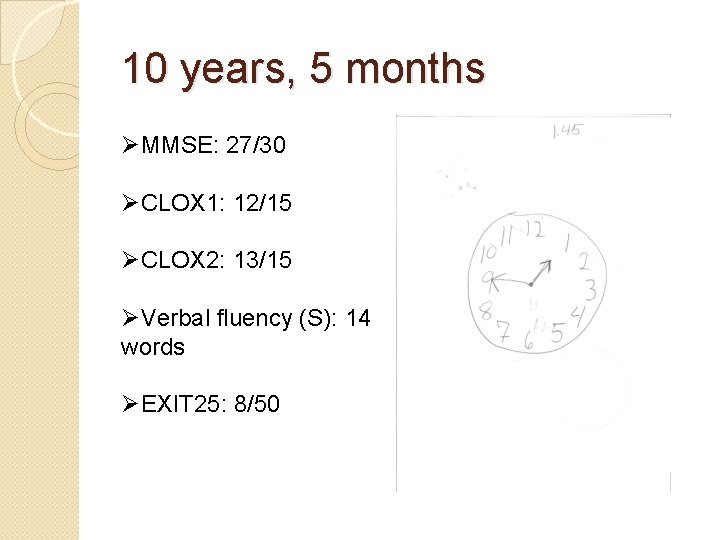
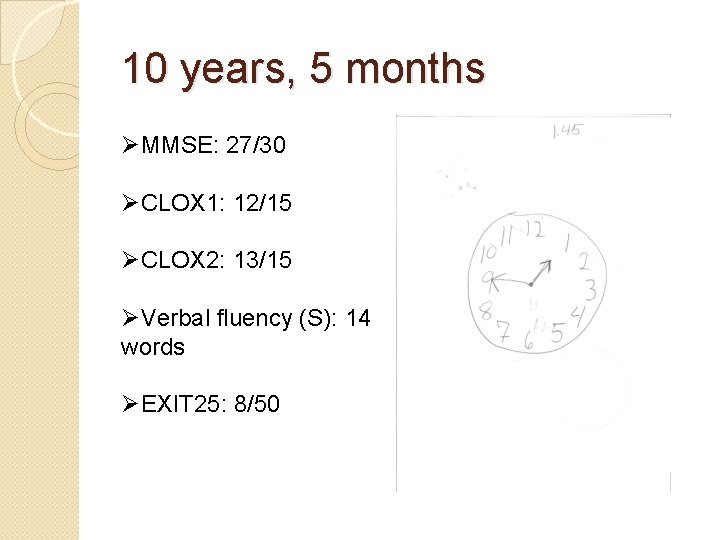
10 years, 5 months ØMMSE: 27/30 ØCLOX 1: 12/15 ØCLOX 2: 13/15 ØVerbal fluency (S): 14 words ØEXIT 25: 8/50
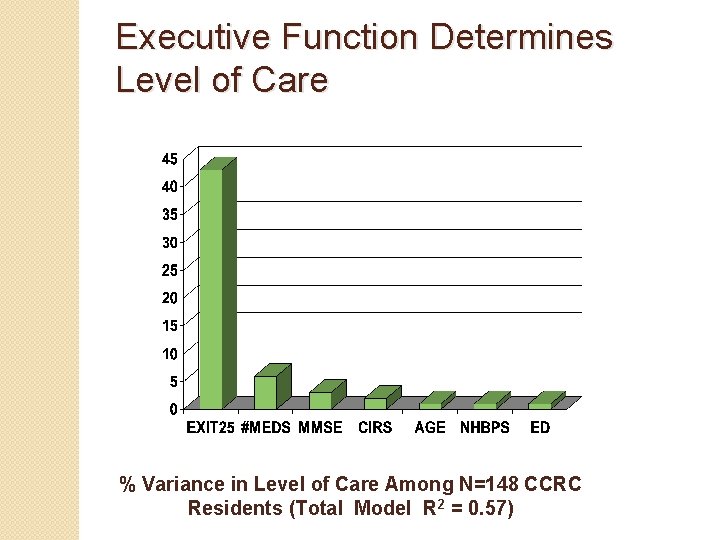
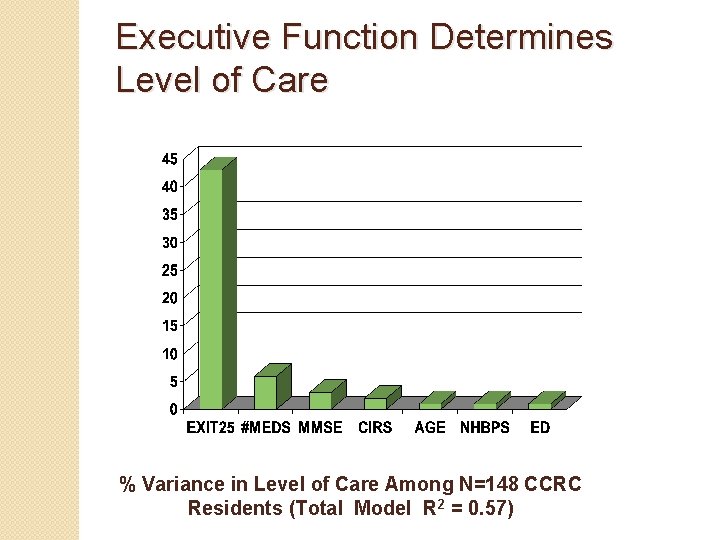
Executive Function Determines Level of Care % Variance in Level of Care Among N=148 CCRC Residents (Total Model R 2 = 0. 57)
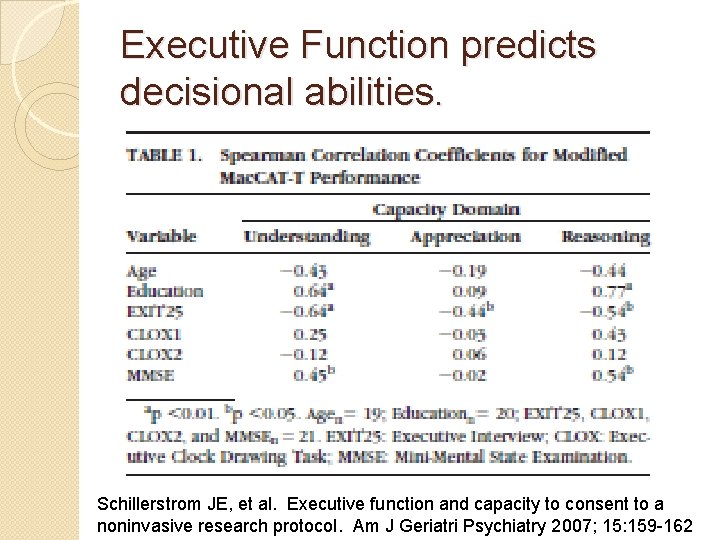
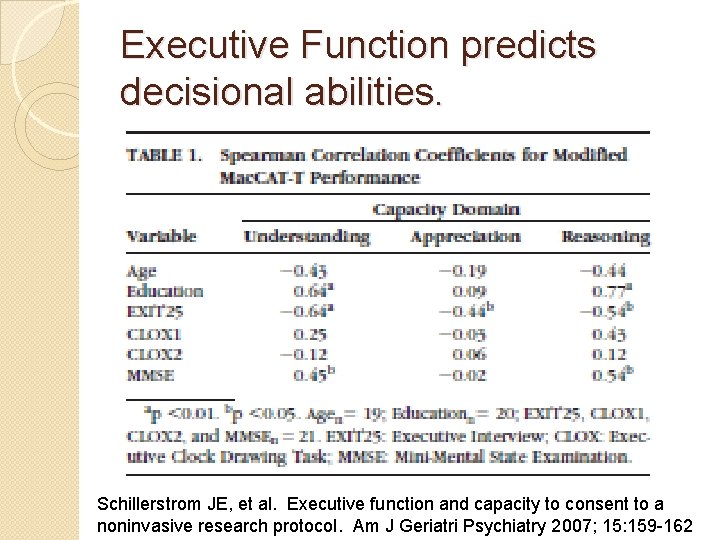
Executive Function predicts decisional abilities. Schillerstrom JE, et al. Executive function and capacity to consent to a noninvasive research protocol. Am J Geriatri Psychiatry 2007; 15: 159 -162
Key Points �Guardianships are common and rare. �Executive function is the cognitive domain that best predicts self care abilities. �Executive function predicts a person’s ability to understand, appreciate, and use reasoning to make personal decisions.
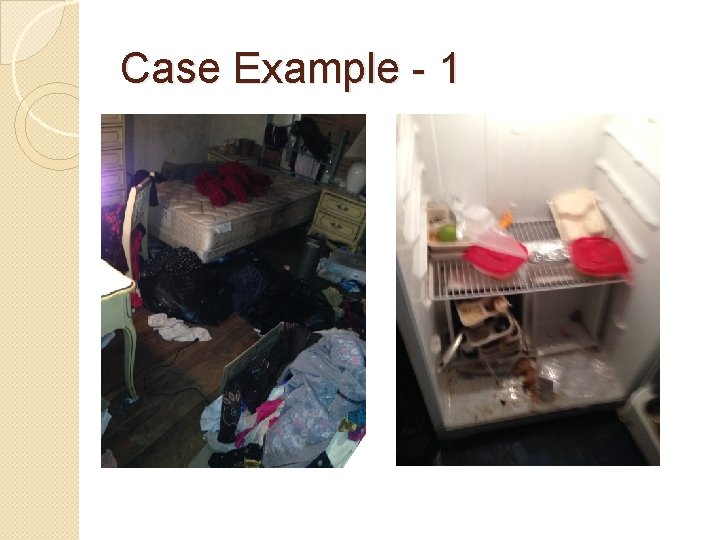
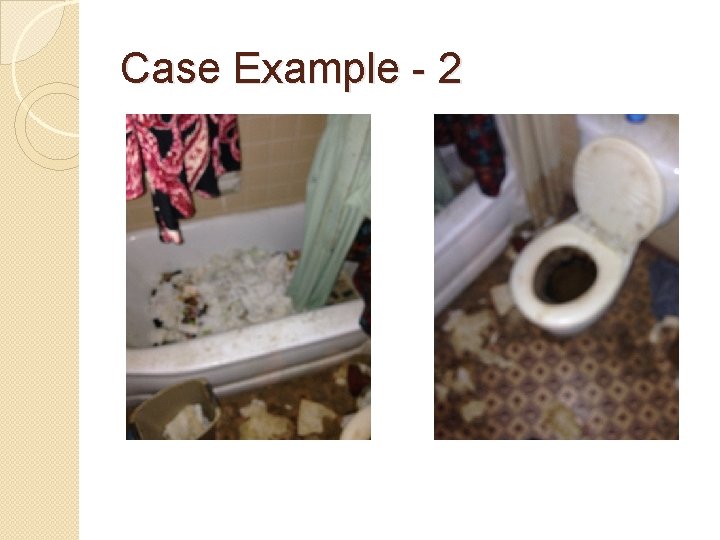
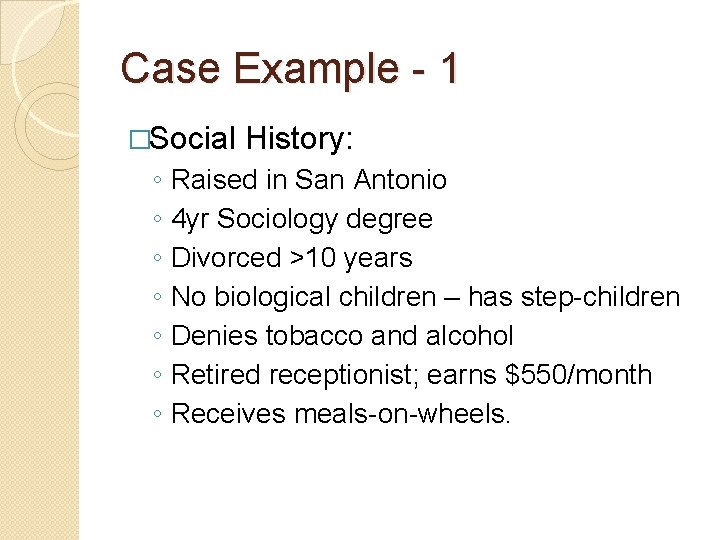
Case Example - 1 � 88 yr HF referred for neglect – recidivistic case. Lives by self in San Antonio. � House is in severe disrepair, squalorous, animal feces throughout, human waste in toilet and bathtub, severe insect infestation, dead dog recently discovered. � PCP knows patient and believes she may have capacity (“She misses appt’s but takes her meds. She has bad hygiene but she has capacity. ”). � Family seems to either underestimate health/safety hazards or overestimate her abilities. They brought her a broom 4 days ago. � Utilities are frequently disconnected. APS and family have had them paid and reconnected on multiple
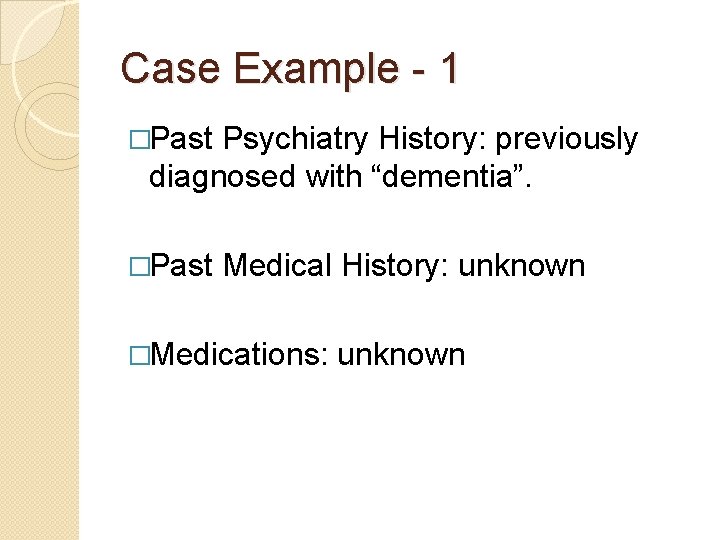
Case Example - 1 �Past Psychiatry History: previously diagnosed with “dementia”. �Past Medical History: unknown �Medications: unknown
Case Example - 1 �Social ◦ ◦ ◦ ◦ History: Raised in San Antonio 4 yr Sociology degree Divorced >10 years No biological children – has step-children Denies tobacco and alcohol Retired receptionist; earns $550/month Receives meals-on-wheels.
Case Example - 1
Case Example - 2
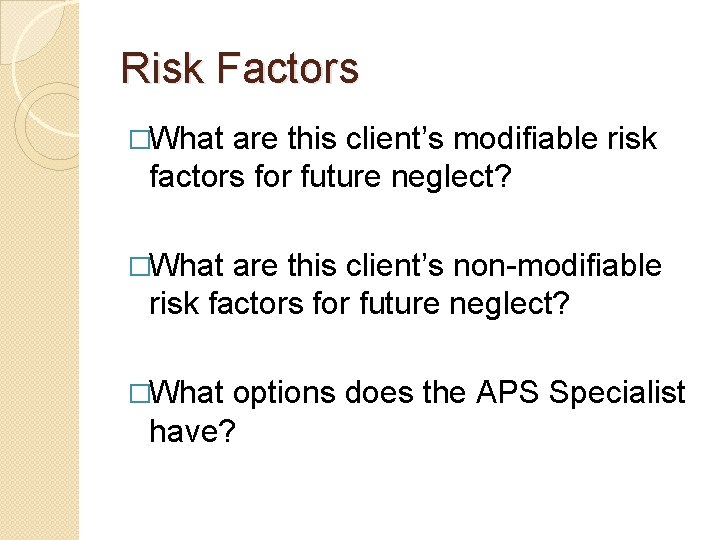
Risk Factors �What are this client’s modifiable risk factors for future neglect? �What are this client’s non-modifiable risk factors for future neglect? �What options does the APS Specialist have?
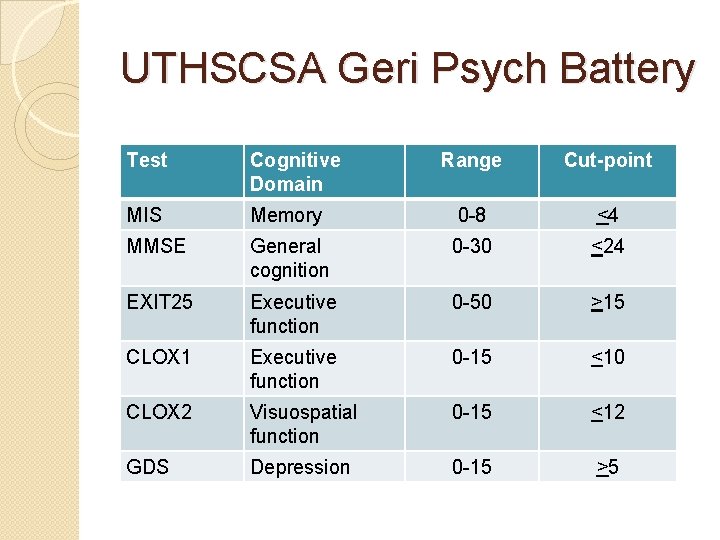
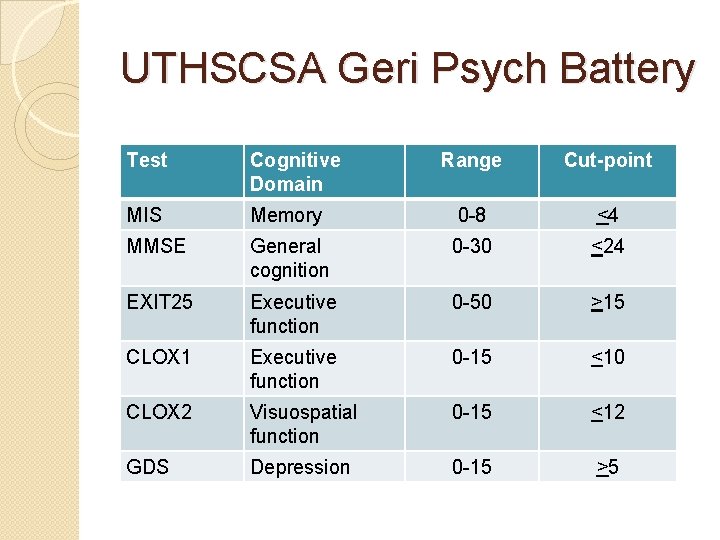
UTHSCSA Geri Psych Battery Test Cognitive Domain Range Cut-point MIS Memory 0 -8 <4 MMSE General cognition 0 -30 <24 EXIT 25 Executive function 0 -50 >15 CLOX 1 Executive function 0 -15 <10 CLOX 2 Visuospatial function 0 -15 <12 GDS Depression 0 -15 >5
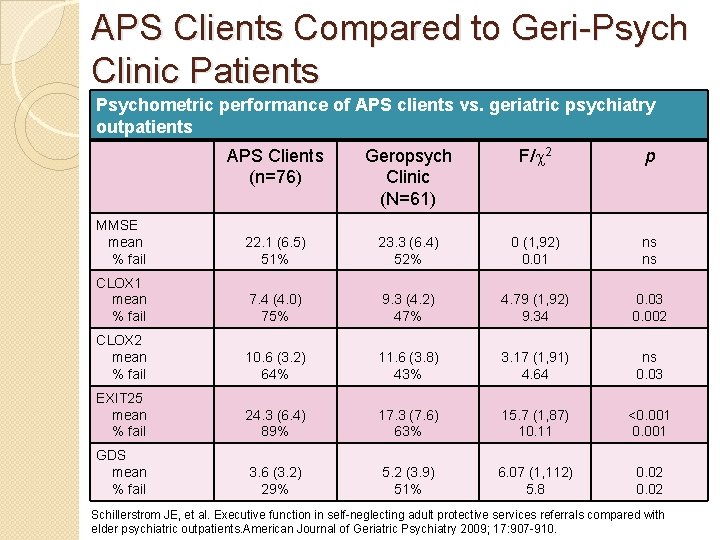
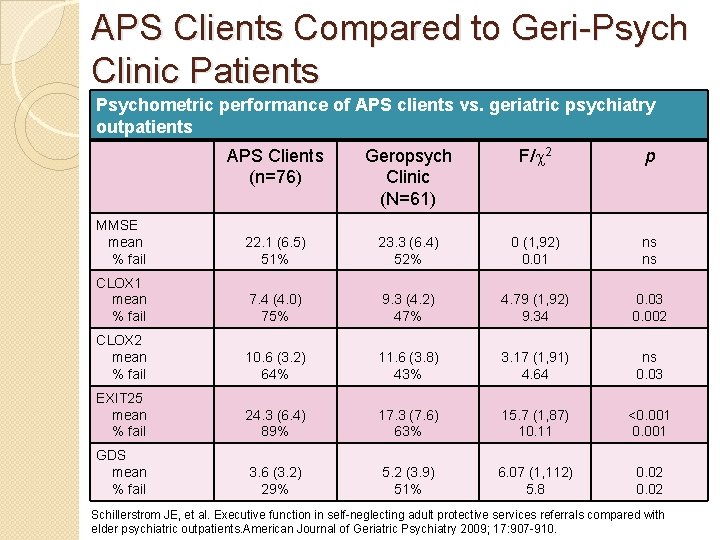
APS Clients Compared to Geri-Psych Clinic Patients Psychometric performance of APS clients vs. geriatric psychiatry outpatients APS Clients (n=76) Geropsych Clinic (N=61) F/c 2 p MMSE mean % fail 22. 1 (6. 5) 51% 23. 3 (6. 4) 52% 0 (1, 92) 0. 01 ns ns CLOX 1 mean % fail 7. 4 (4. 0) 75% 9. 3 (4. 2) 47% 4. 79 (1, 92) 9. 34 0. 03 0. 002 CLOX 2 mean % fail 10. 6 (3. 2) 64% 11. 6 (3. 8) 43% 3. 17 (1, 91) 4. 64 ns 0. 03 EXIT 25 mean % fail 24. 3 (6. 4) 89% 17. 3 (7. 6) 63% 15. 7 (1, 87) 10. 11 <0. 001 GDS mean % fail 3. 6 (3. 2) 29% 5. 2 (3. 9) 51% 6. 07 (1, 112) 5. 8 0. 02 Schillerstrom JE, et al. Executive function in self-neglecting adult protective services referrals compared with elder psychiatric outpatients. American Journal of Geriatric Psychiatry 2009; 17: 907 -910.
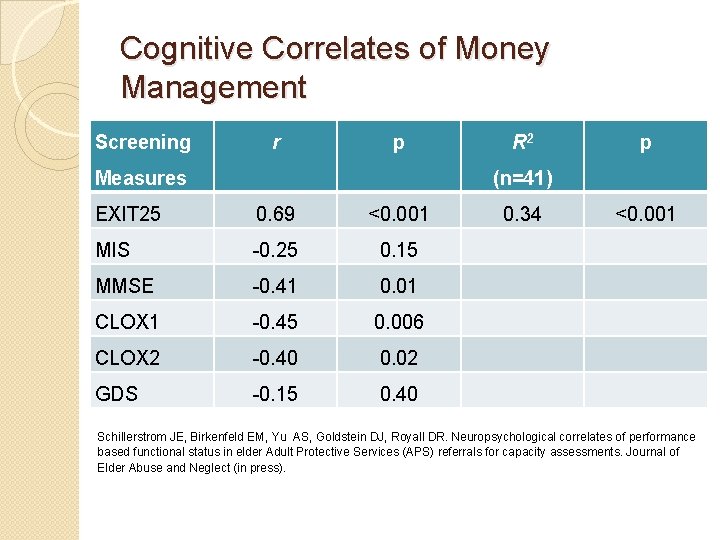
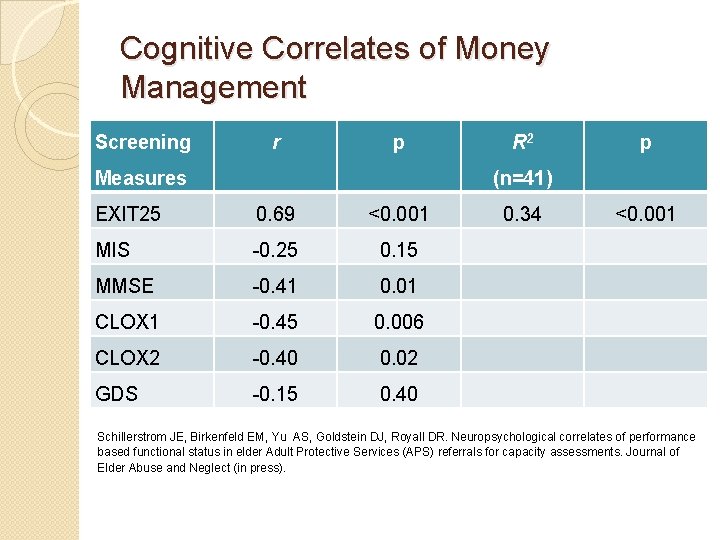
Cognitive Correlates of Money Management Screening r p Measures R 2 p (n=41) EXIT 25 0. 69 <0. 001 MIS -0. 25 0. 15 MMSE -0. 41 0. 01 CLOX 1 -0. 45 0. 006 CLOX 2 -0. 40 0. 02 GDS -0. 15 0. 40 0. 34 <0. 001 Schillerstrom JE, Birkenfeld EM, Yu AS, Goldstein DJ, Royall DR. Neuropsychological correlates of performance based functional status in elder Adult Protective Services (APS) referrals for capacity assessments. Journal of Elder Abuse and Neglect (in press).
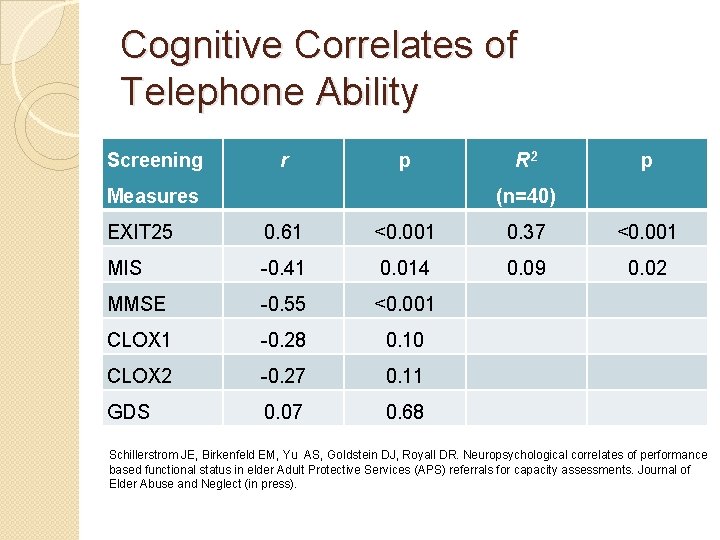
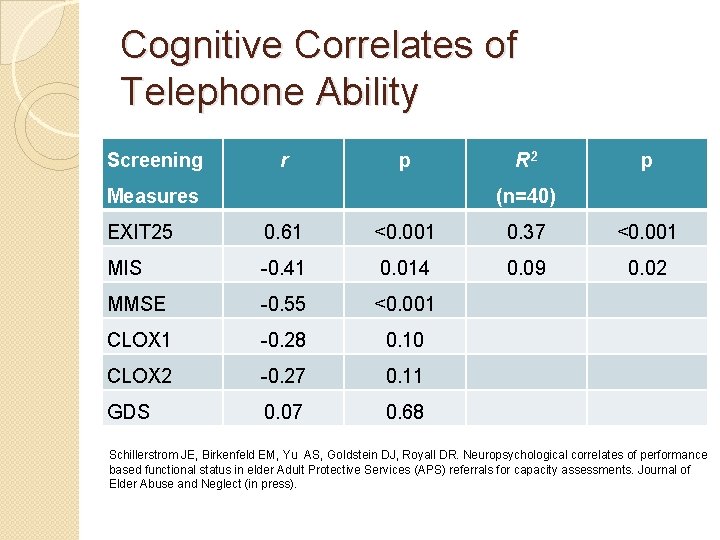
Cognitive Correlates of Telephone Ability Screening r p Measures R 2 p (n=40) EXIT 25 0. 61 <0. 001 0. 37 <0. 001 MIS -0. 41 0. 014 0. 09 0. 02 MMSE -0. 55 <0. 001 CLOX 1 -0. 28 0. 10 CLOX 2 -0. 27 0. 11 GDS 0. 07 0. 68 Schillerstrom JE, Birkenfeld EM, Yu AS, Goldstein DJ, Royall DR. Neuropsychological correlates of performance based functional status in elder Adult Protective Services (APS) referrals for capacity assessments. Journal of Elder Abuse and Neglect (in press).
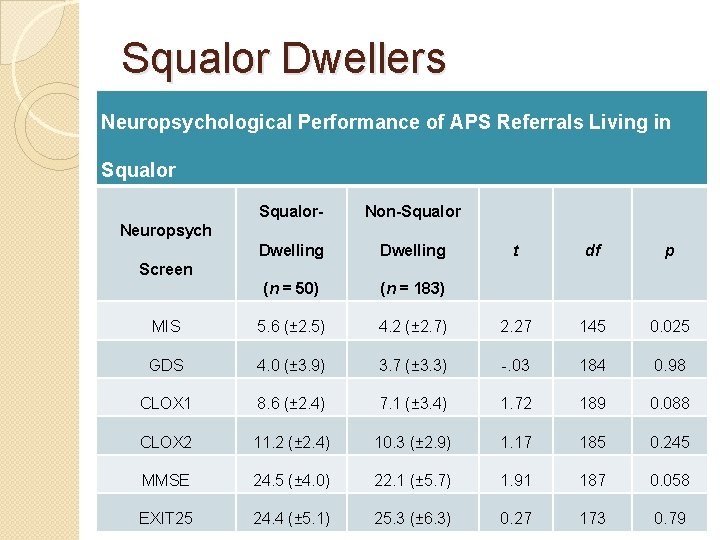
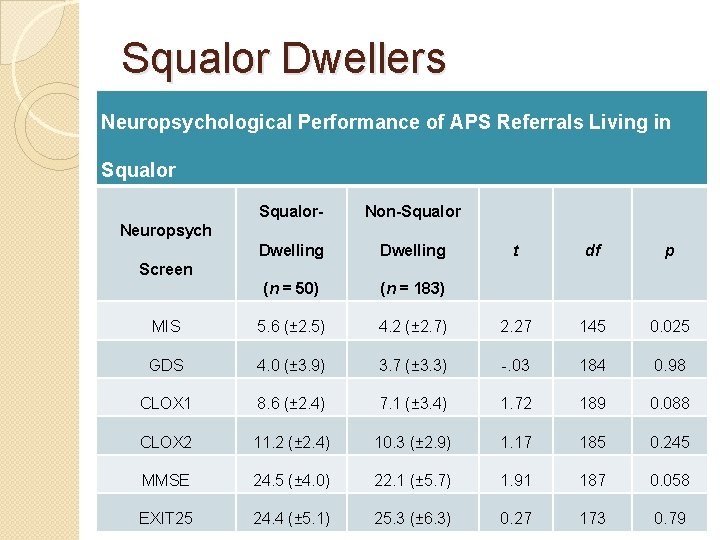
Squalor Dwellers Neuropsychological Performance of APS Referrals Living in Squalor- Non-Squalor Dwelling (n = 50) (n = 183) MIS 5. 6 (± 2. 5) GDS Neuropsych t df p 4. 2 (± 2. 7) 2. 27 145 0. 025 4. 0 (± 3. 9) 3. 7 (± 3. 3) -. 03 184 0. 98 CLOX 1 8. 6 (± 2. 4) 7. 1 (± 3. 4) 1. 72 189 0. 088 CLOX 2 11. 2 (± 2. 4) 10. 3 (± 2. 9) 1. 17 185 0. 245 MMSE 24. 5 (± 4. 0) 22. 1 (± 5. 7) 1. 91 187 0. 058 EXIT 25 24. 4 (± 5. 1) 25. 3 (± 6. 3) 0. 27 173 0. 79 Screen
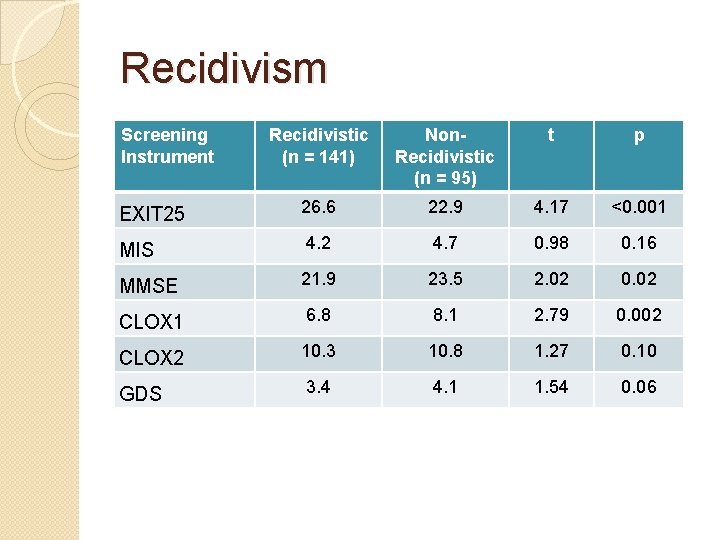
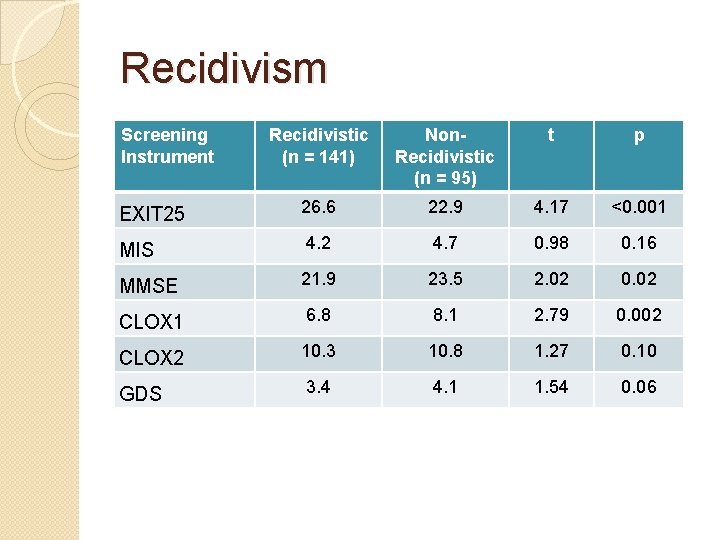
Recidivism Screening Instrument Recidivistic (n = 141) Non. Recidivistic (n = 95) t p EXIT 25 26. 6 22. 9 4. 17 <0. 001 MIS 4. 2 4. 7 0. 98 0. 16 MMSE 21. 9 23. 5 2. 02 0. 02 CLOX 1 6. 8 8. 1 2. 79 0. 002 CLOX 2 10. 3 10. 8 1. 27 0. 10 GDS 3. 4 4. 1 1. 54 0. 06
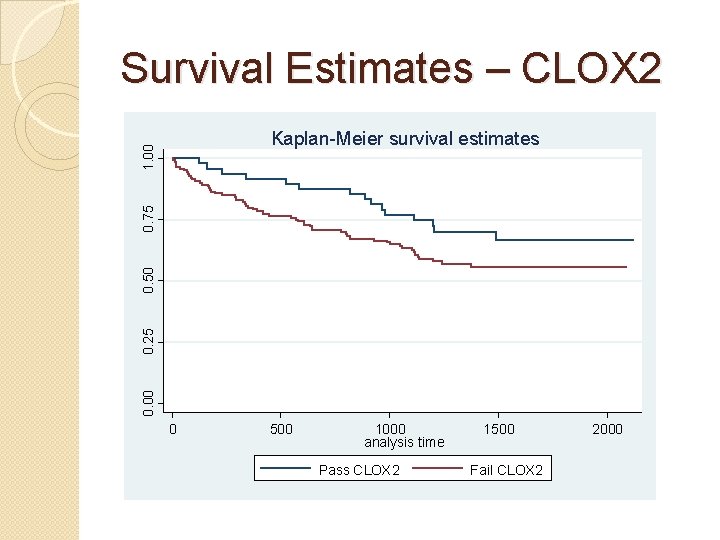
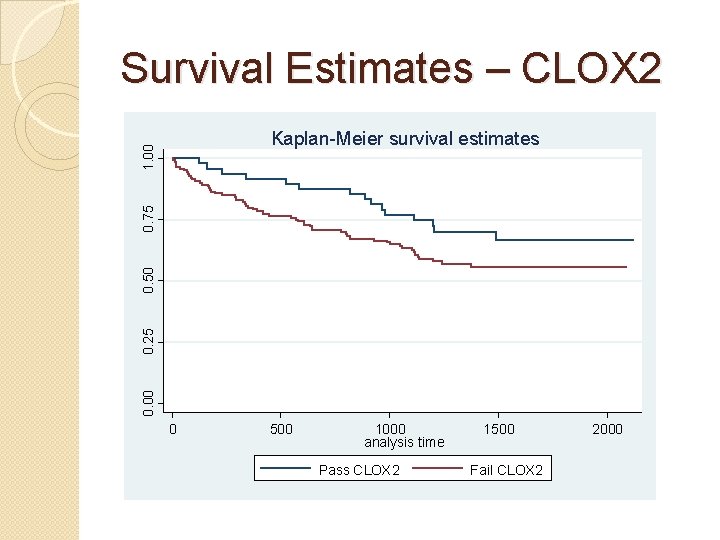
Survival Estimates – CLOX 2 0. 00 0. 25 0. 50 0. 75 1. 00 Kaplan-Meier survival estimates 0 500 1000 analysis time Pass CLOX 2 1500 Fail CLOX 2 2000
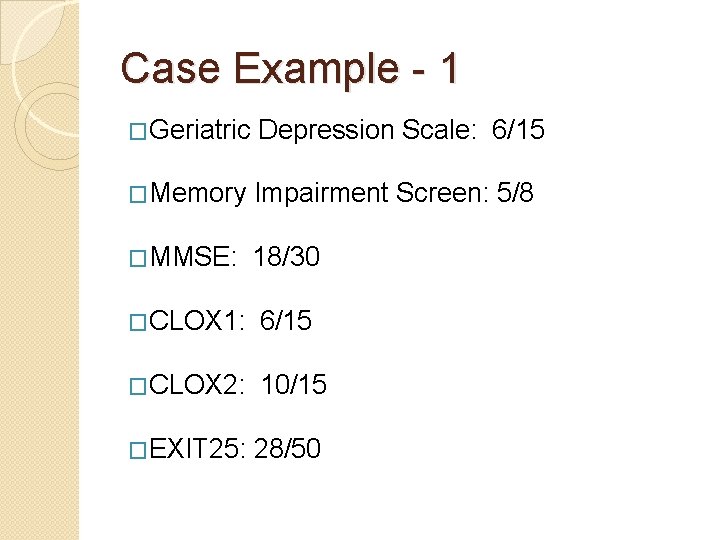
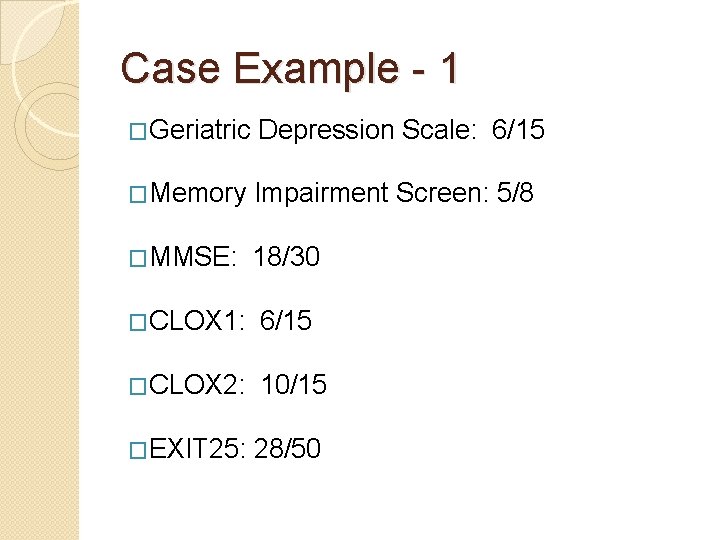
Case Example - 1 �Geriatric Depression Scale: 6/15 �Memory Impairment Screen: 5/8 �MMSE: 18/30 �CLOX 1: 6/15 �CLOX 2: 10/15 �EXIT 25: 28/50
Does this client have capacity? An incapacitated person is an adult who, because of a physical or mental condition, is substantially unable to provide food, clothing, or shelter for himself or herself, to care for the individual’s own physical health, or to manage the individual’s own financial affairs.
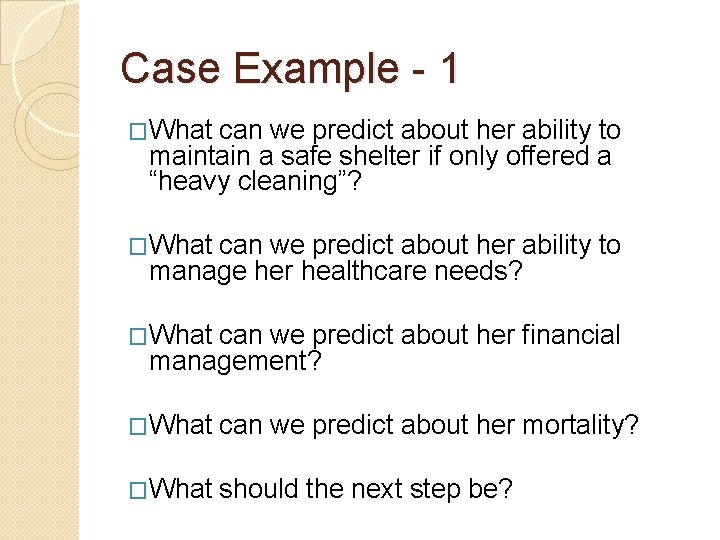
Case Example - 1 �What can we predict about her ability to maintain a safe shelter if only offered a “heavy cleaning”? �What can we predict about her ability to manage her healthcare needs? �What can we predict about her financial management? �What can we predict about her mortality? �What should the next step be?
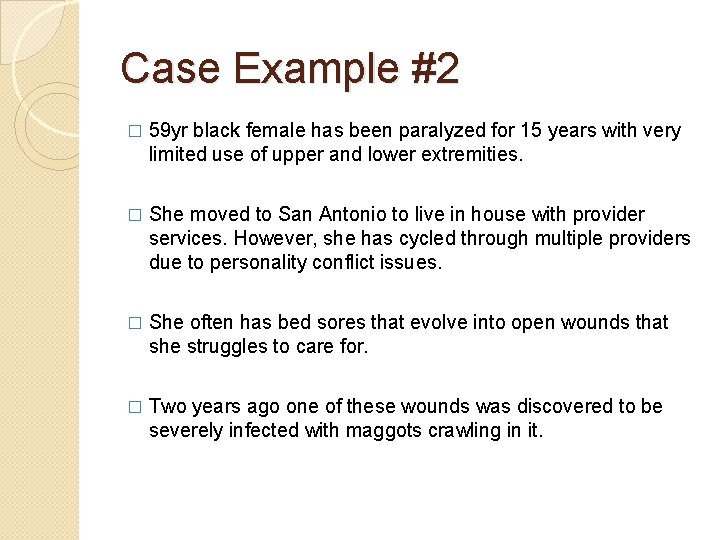
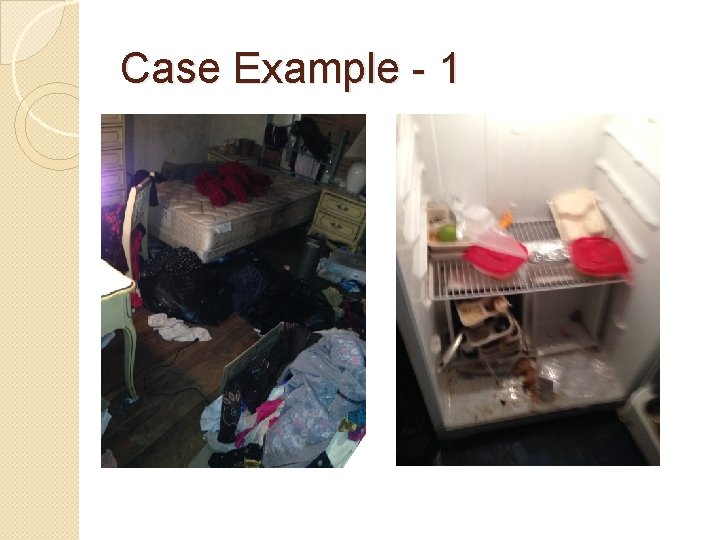
Case Example #2 � 59 yr black female has been paralyzed for 15 years with very limited use of upper and lower extremities. � She moved to San Antonio to live in house with provider services. However, she has cycled through multiple providers due to personality conflict issues. � She often has bed sores that evolve into open wounds that she struggles to care for. � Two years ago one of these wounds was discovered to be severely infected with maggots crawling in it.
Case Example #2 � Her primary care physician is frustrated with the client’s ambivalence regarding her medical needs. � She struggles to use her wound vacuum appropriately which results in delayed healing. � She is a frequent 911 caller. Calls 911 for inappropriate requests such as to come light a cigarette for her. � She frequently calls state agencies to complain about the care she receives. � She owes $13, 000 in taxes. � She depends on neighbors for general support.
Case Example #2 – Client’s Home �Her home appears to be poorly maintained. �It is cluttered, the fence is falling down, and significant repairs need to be made (the door for example is significantly warped). �Her refrigerator is crammed with food. kitchen is messy and does not appear safe for food preparation in its current state.
Case Example #2 – Collateral Info � Assisted living social worker reports that the patient has a difficult personality and requires extensive hands-on care. � Her judgment is questionable in that she becomes angry when others offer to help. � However, her moods have improved with time and the client seems generally happy. � The client seems to understand her limitations and reluctantly accepts help. � The client has not seemed confused or disoriented since being admitted.
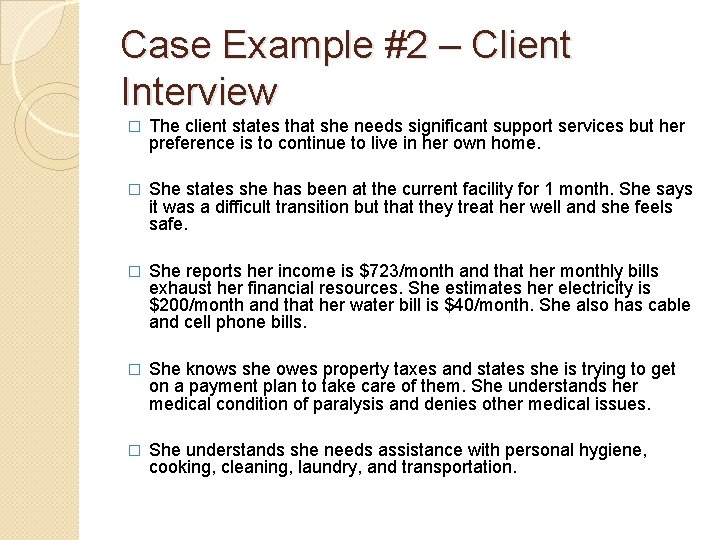
Case Example #2 – Client Interview � The client states that she needs significant support services but her preference is to continue to live in her own home. � She states she has been at the current facility for 1 month. She says it was a difficult transition but that they treat her well and she feels safe. � She reports her income is $723/month and that her monthly bills exhaust her financial resources. She estimates her electricity is $200/month and that her water bill is $40/month. She also has cable and cell phone bills. � She knows she owes property taxes and states she is trying to get on a payment plan to take care of them. She understands her medical condition of paralysis and denies other medical issues. � She understands she needs assistance with personal hygiene, cooking, cleaning, laundry, and transportation.
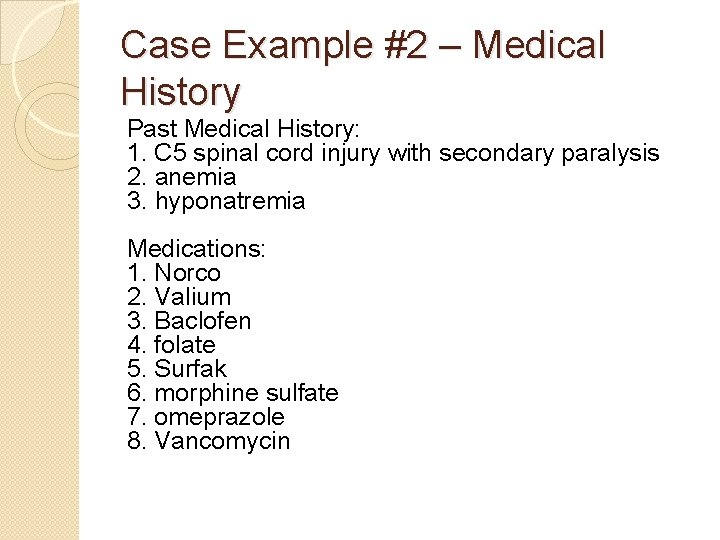
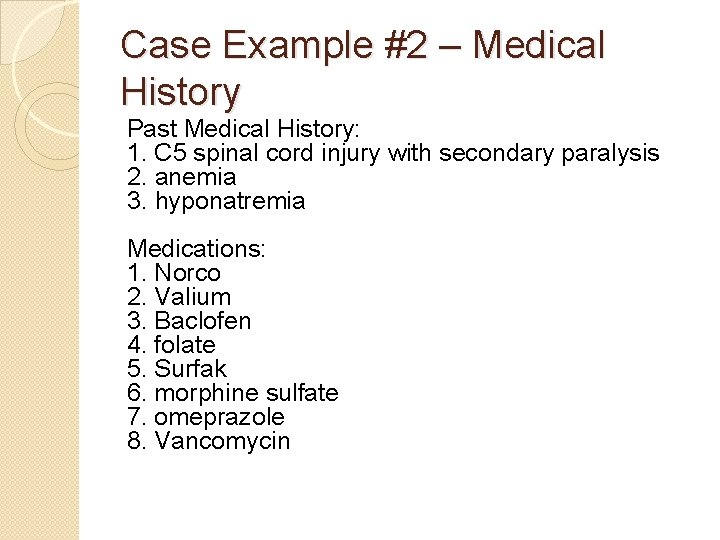
Case Example #2 – Medical History Past Medical History: 1. C 5 spinal cord injury with secondary paralysis 2. anemia 3. hyponatremia Medications: 1. Norco 2. Valium 3. Baclofen 4. folate 5. Surfak 6. morphine sulfate 7. omeprazole 8. Vancomycin
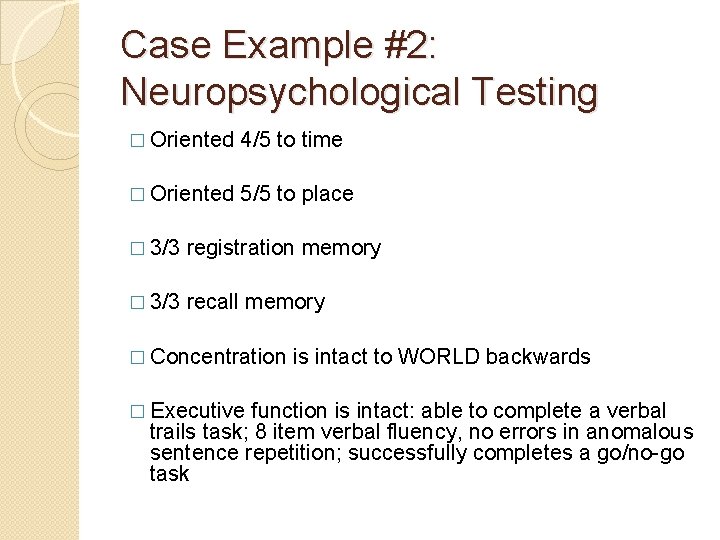
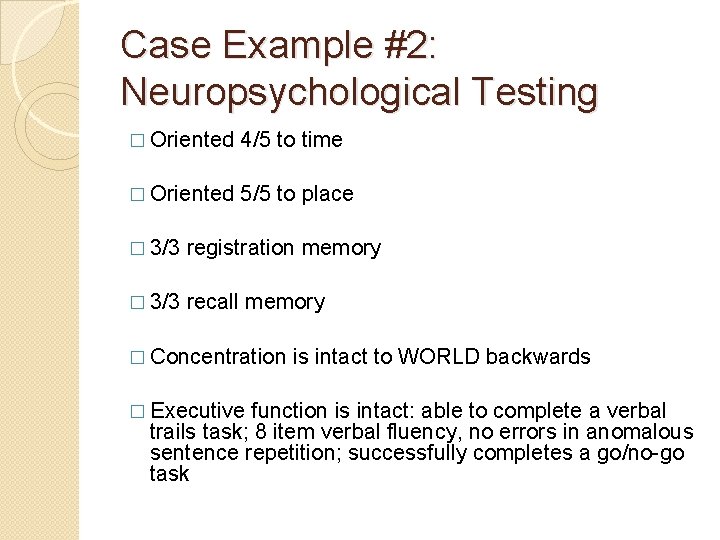
Case Example #2: Neuropsychological Testing � Oriented 4/5 to time � Oriented 5/5 to place � 3/3 registration memory � 3/3 recall memory � Concentration � Executive is intact to WORLD backwards function is intact: able to complete a verbal trails task; 8 item verbal fluency, no errors in anomalous sentence repetition; successfully completes a go/no-go task
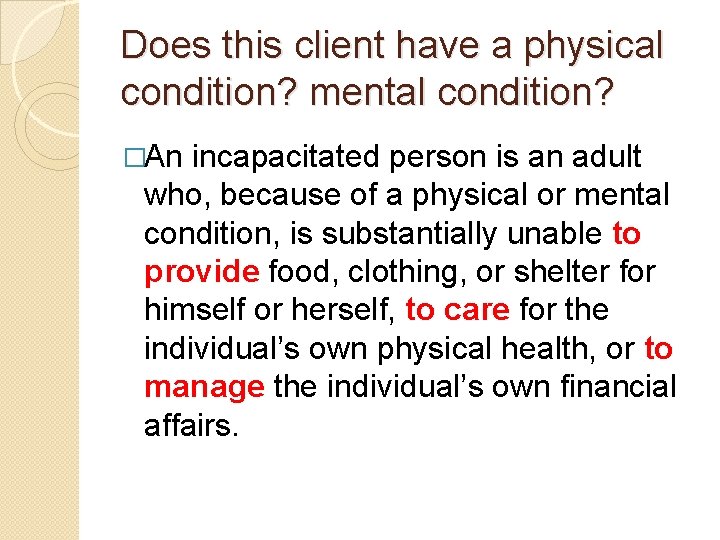
Does this client have a physical condition? mental condition? �An incapacitated person is an adult who, because of a physical or mental condition, is substantially unable to provide food, clothing, or shelter for himself or herself, to care for the individual’s own physical health, or to manage the individual’s own financial affairs.
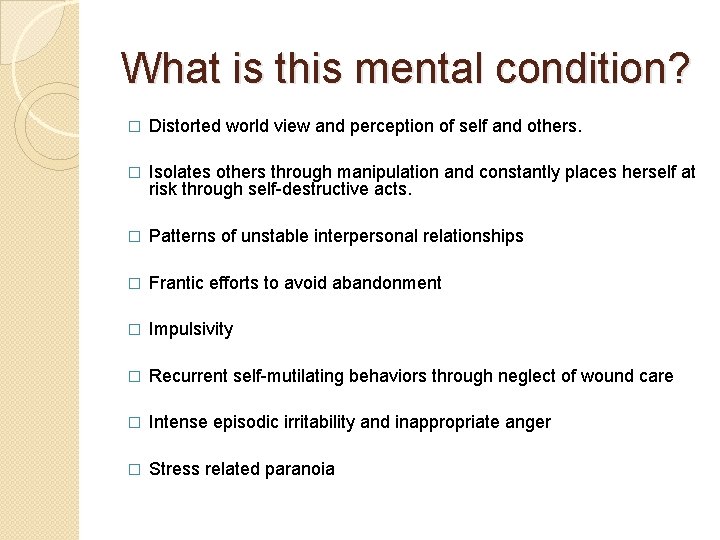
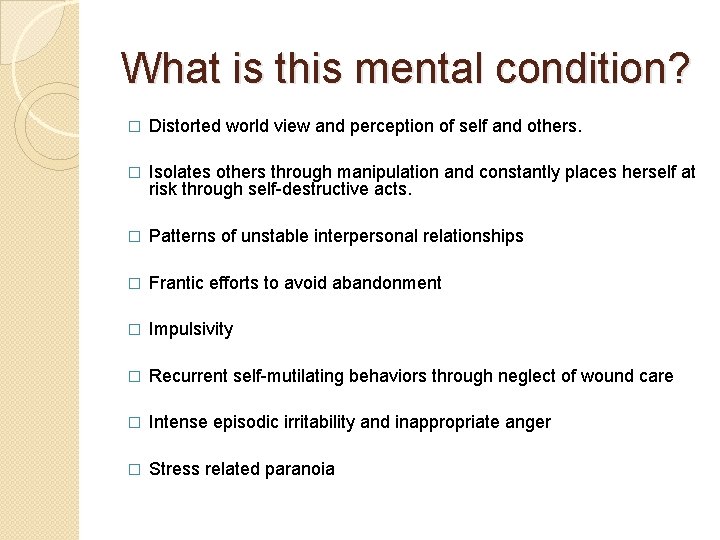
What is this mental condition? � Distorted world view and perception of self and others. � Isolates others through manipulation and constantly places herself at risk through self-destructive acts. � Patterns of unstable interpersonal relationships � Frantic efforts to avoid abandonment � Impulsivity � Recurrent self-mutilating behaviors through neglect of wound care � Intense episodic irritability and inappropriate anger � Stress related paranoia
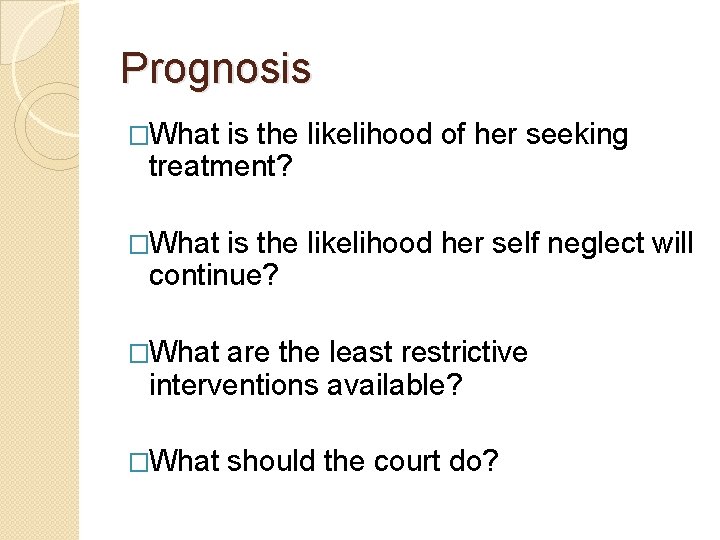
Prognosis �What is the likelihood of her seeking treatment? �What is the likelihood her self neglect will continue? �What are the least restrictive interventions available? �What should the court do?
Questions and Discussion