AspirationInjection Crystalline Arthritis Kathryn Dao MD Arthritis Consultation


- Slides: 56

Aspiration/Injection & Crystalline Arthritis Kathryn Dao, MD Arthritis Consultation Center July 26, 2007
Outline • • General Principles Technique Fluid Analysis Crystalline Diseases
General Principles • Almost any articular/peri-articular structure (e. g. , bursa) can be aspirated/injected Intern question: Why should you do an aspiration/injection? • Primary goals of arthrocentesis/injection: 1. Aid in diagnosis 2. Provide therapy (relieve pressure/inject medicine)
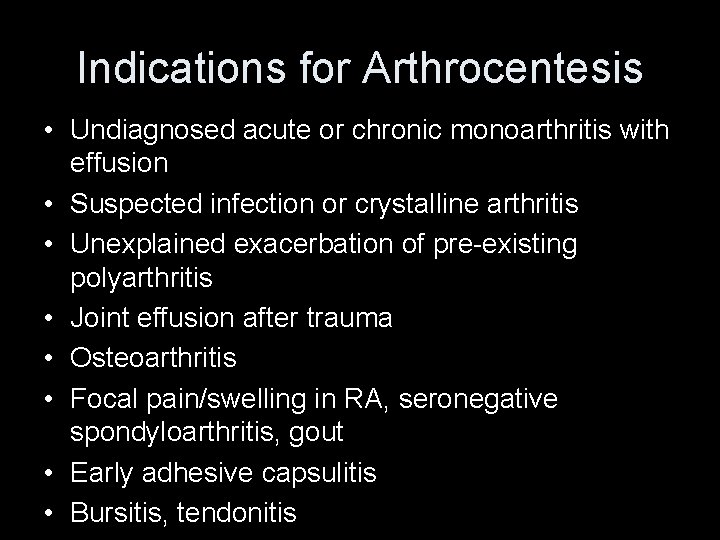
Indications for Arthrocentesis • Undiagnosed acute or chronic monoarthritis with effusion • Suspected infection or crystalline arthritis • Unexplained exacerbation of pre-existing polyarthritis • Joint effusion after trauma • Osteoarthritis • Focal pain/swelling in RA, seronegative spondyloarthritis, gout • Early adhesive capsulitis • Bursitis, tendonitis
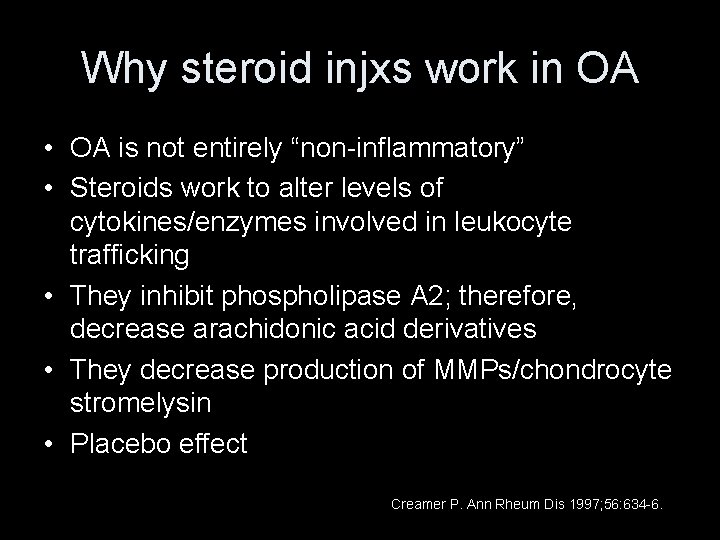
rd 3 year resident question: Why do steroid injections work in OA?
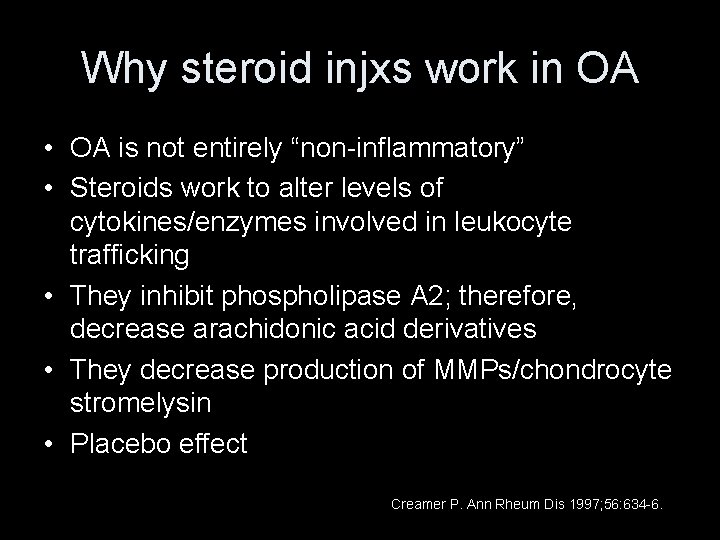
Why steroid injxs work in OA • OA is not entirely “non-inflammatory” • Steroids work to alter levels of cytokines/enzymes involved in leukocyte trafficking • They inhibit phospholipase A 2; therefore, decrease arachidonic acid derivatives • They decrease production of MMPs/chondrocyte stromelysin • Placebo effect Creamer P. Ann Rheum Dis 1997; 56: 634 -6.
nd 2 year resident question: Name at least 5 nonfinancial reasons not to inject.
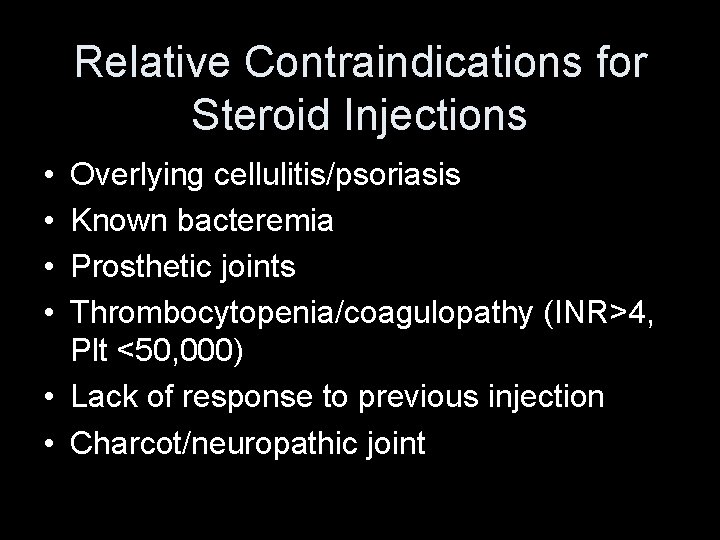
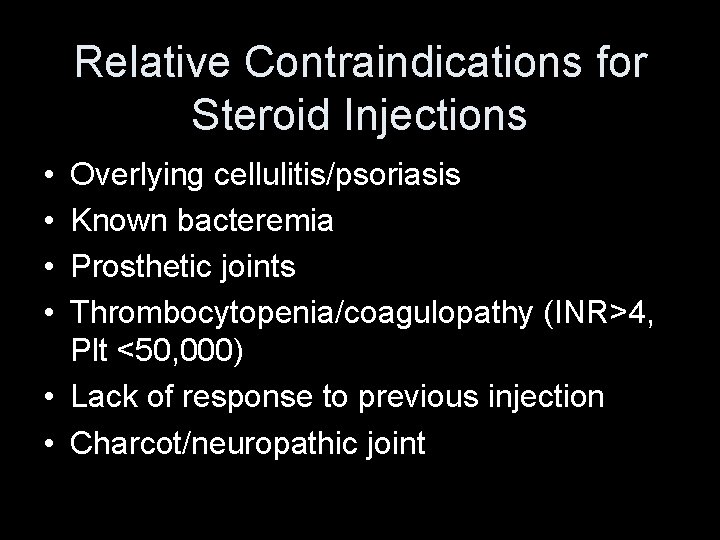
Relative Contraindications for Steroid Injections • • Overlying cellulitis/psoriasis Known bacteremia Prosthetic joints Thrombocytopenia/coagulopathy (INR>4, Plt <50, 000) • Lack of response to previous injection • Charcot/neuropathic joint
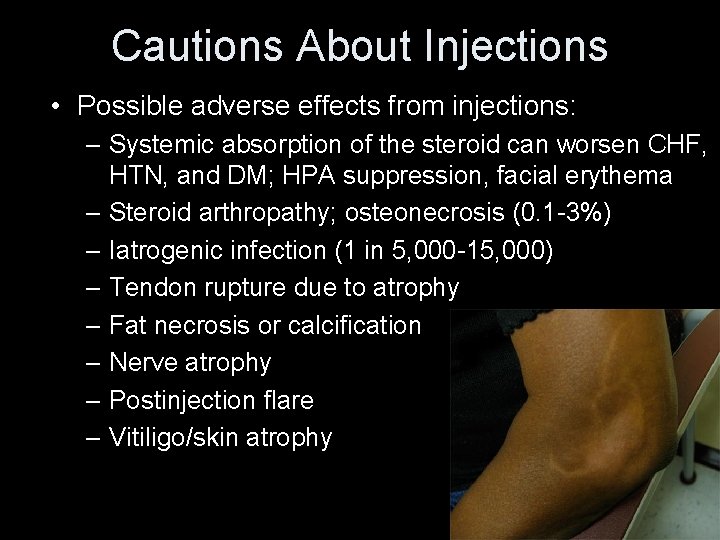
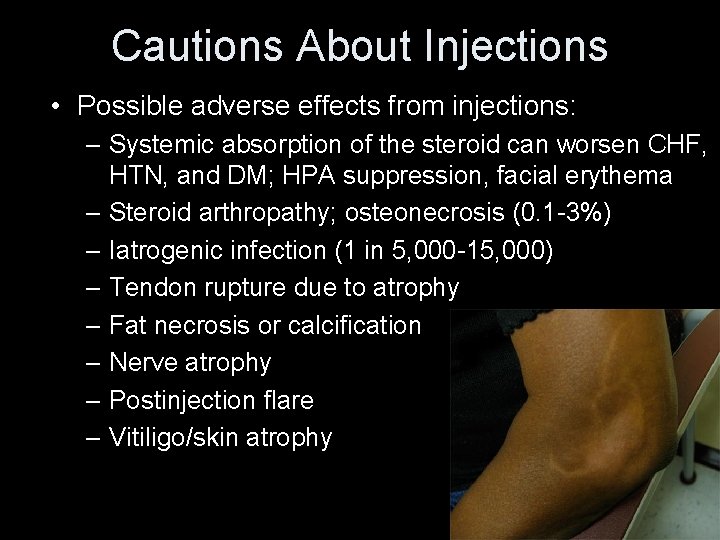
Cautions About Injections • Possible adverse effects from injections: – Systemic absorption of the steroid can worsen CHF, HTN, and DM; HPA suppression, facial erythema – Steroid arthropathy; osteonecrosis (0. 1 -3%) – Iatrogenic infection (1 in 5, 000 -15, 000) – Tendon rupture due to atrophy – Fat necrosis or calcification – Nerve atrophy – Postinjection flare – Vitiligo/skin atrophy
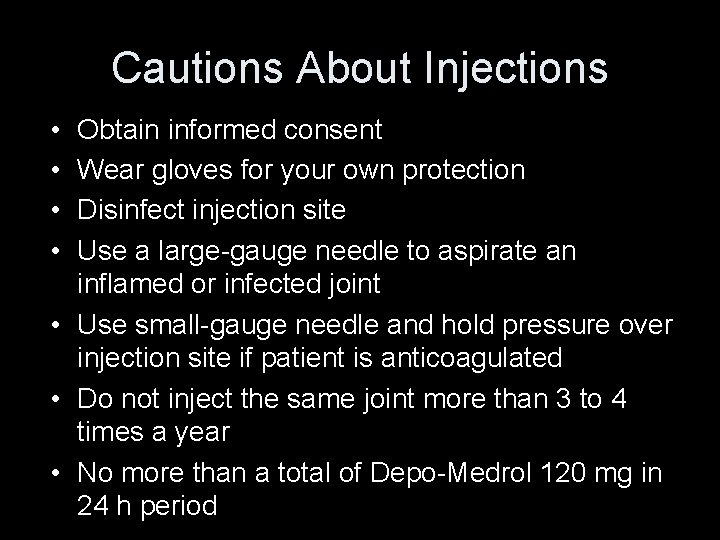
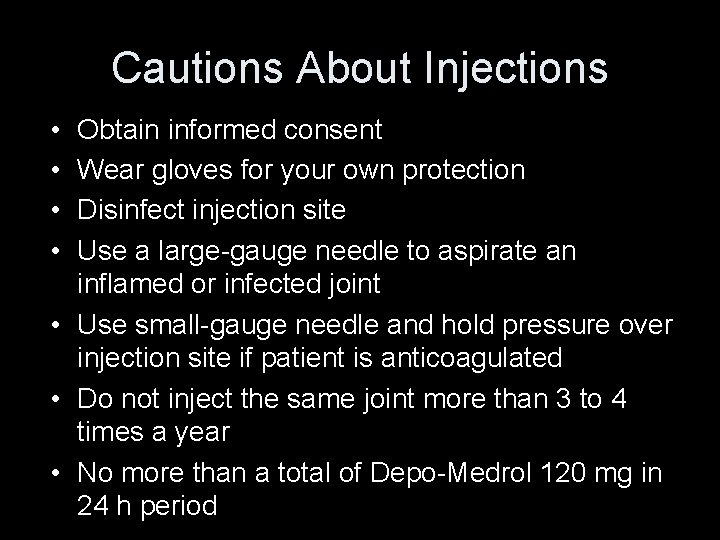
Cautions About Injections • • Obtain informed consent Wear gloves for your own protection Disinfect injection site Use a large-gauge needle to aspirate an inflamed or infected joint • Use small-gauge needle and hold pressure over injection site if patient is anticoagulated • Do not inject the same joint more than 3 to 4 times a year • No more than a total of Depo-Medrol 120 mg in 24 h period
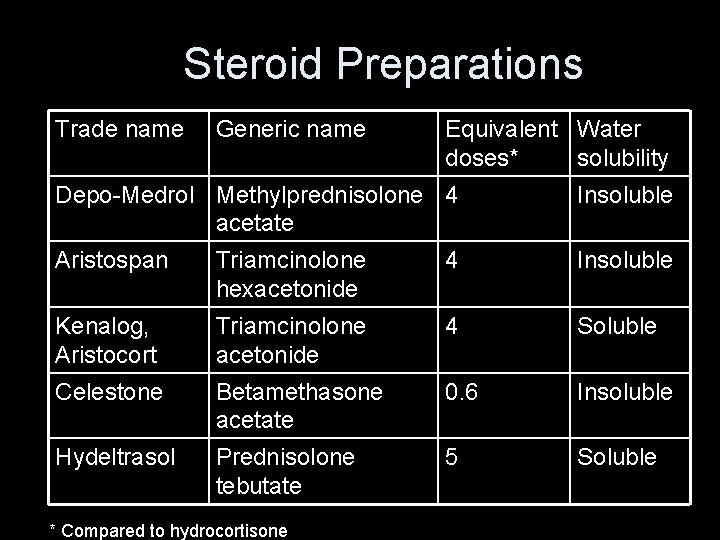
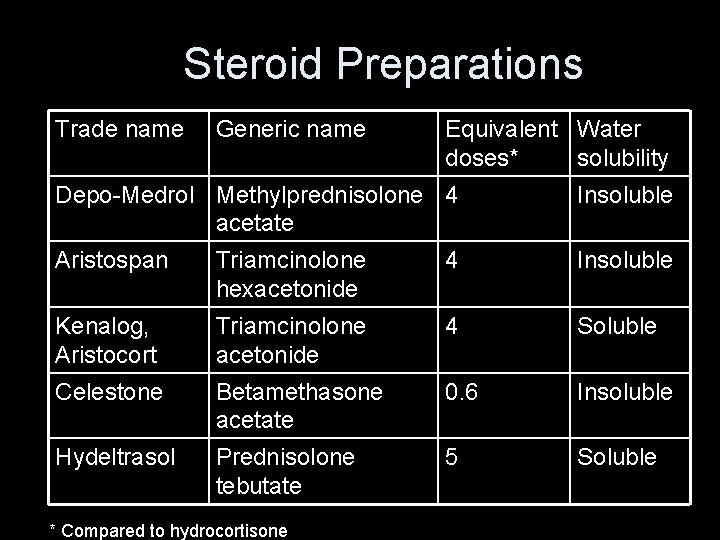
Steroid Preparations Trade name Generic name Equivalent Water doses* solubility Depo-Medrol Methylprednisolone 4 acetate Insoluble Aristospan Triamcinolone hexacetonide 4 Insoluble Kenalog, Aristocort Triamcinolone acetonide 4 Soluble Celestone Betamethasone acetate 0. 6 Insoluble Hydeltrasol Prednisolone tebutate 5 Soluble * Compared to hydrocortisone
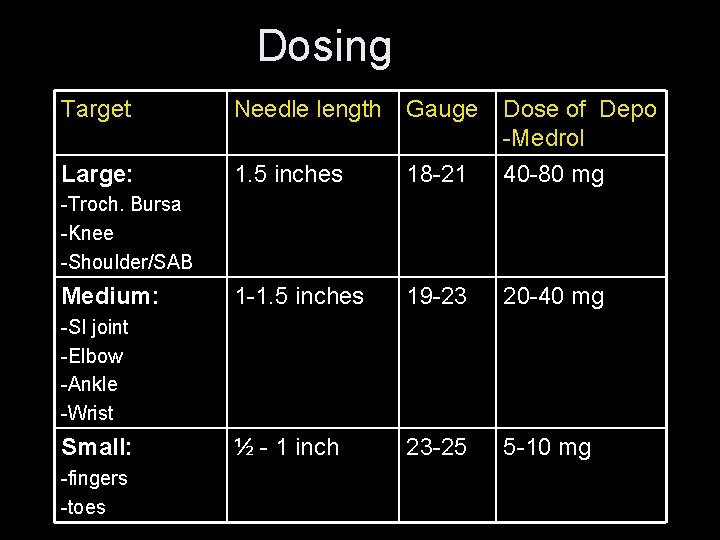
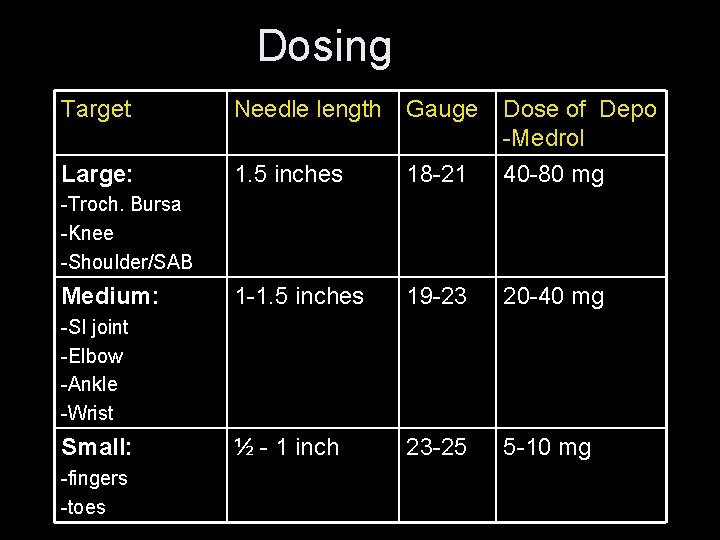
Dosing Target Needle length Gauge Large: 1. 5 inches 18 -21 Dose of Depo -Medrol 40 -80 mg 1 -1. 5 inches 19 -23 20 -40 mg ½ - 1 inch 23 -25 5 -10 mg -Troch. Bursa -Knee -Shoulder/SAB Medium: -SI joint -Elbow -Ankle -Wrist Small: -fingers -toes
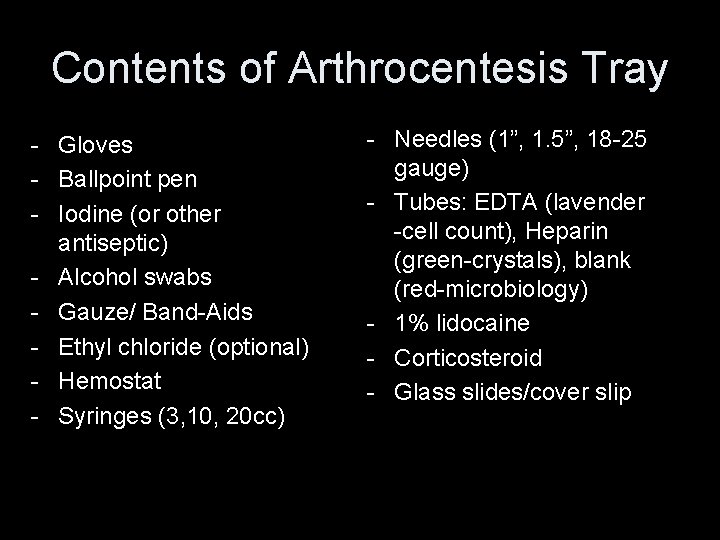
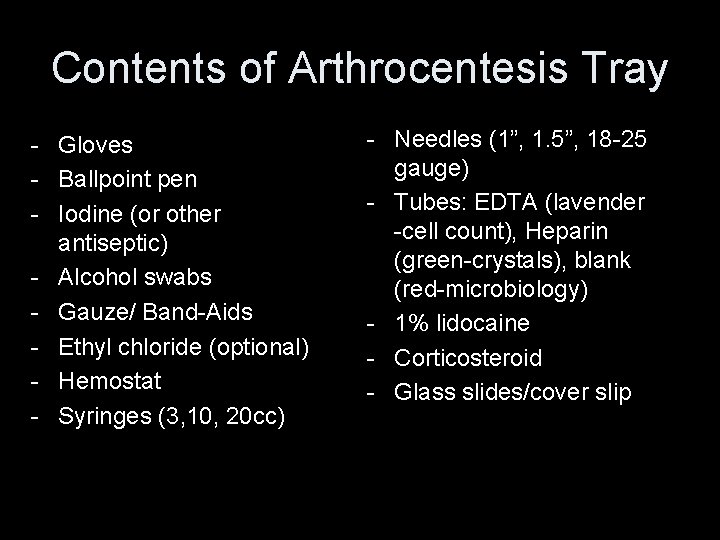
Contents of Arthrocentesis Tray - Gloves - Ballpoint pen - Iodine (or other antiseptic) - Alcohol swabs - Gauze/ Band-Aids - Ethyl chloride (optional) - Hemostat - Syringes (3, 10, 20 cc) - Needles (1”, 1. 5”, 18 -25 gauge) - Tubes: EDTA (lavender -cell count), Heparin (green-crystals), blank (red-microbiology) - 1% lidocaine - Corticosteroid - Glass slides/cover slip
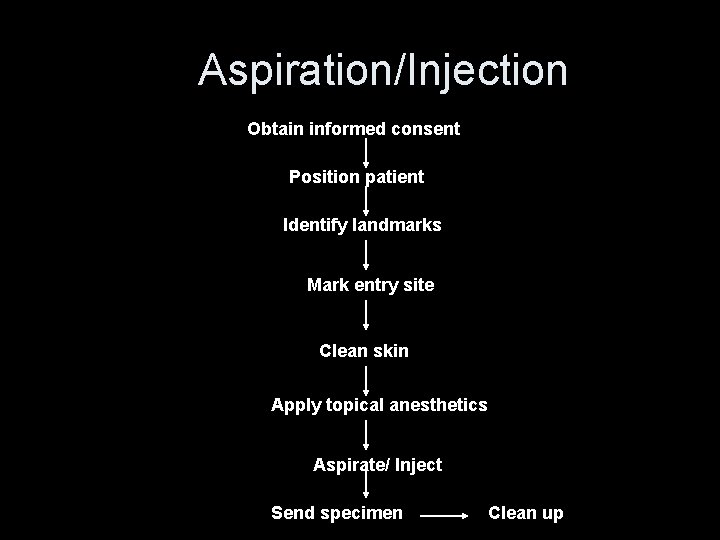
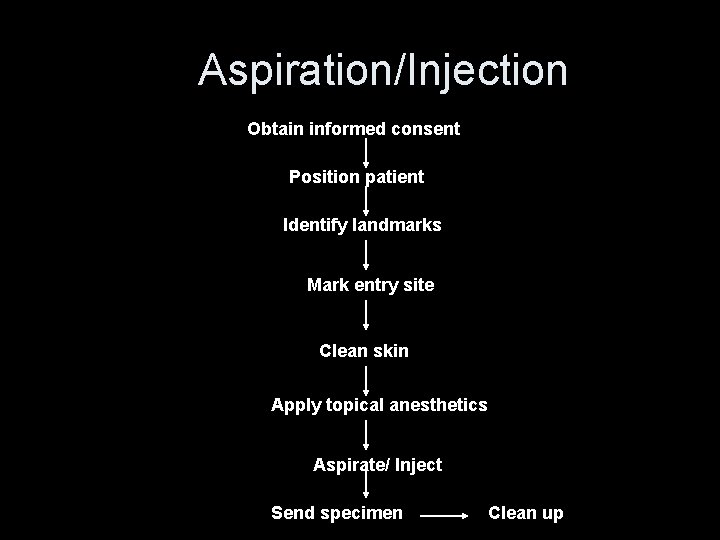
Aspiration/Injection Obtain informed consent Position patient Identify landmarks Mark entry site Clean skin Apply topical anesthetics Aspirate/ Inject Send specimen Clean up
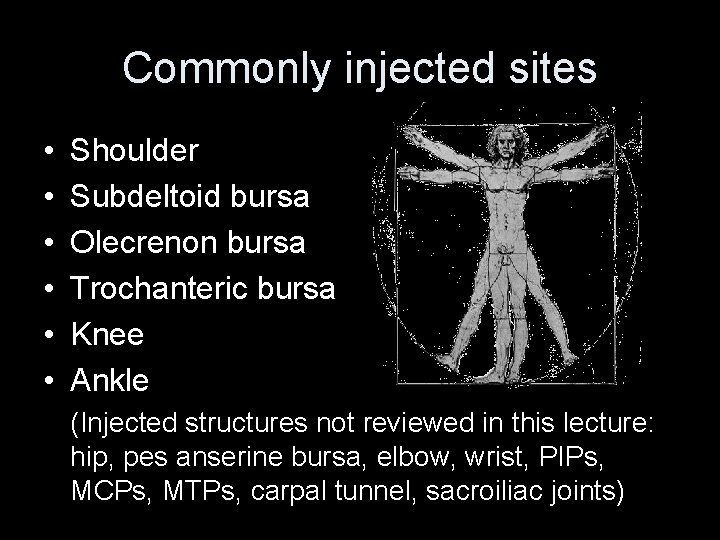
Commonly injected sites • • • Shoulder Subdeltoid bursa Olecrenon bursa Trochanteric bursa Knee Ankle (Injected structures not reviewed in this lecture: hip, pes anserine bursa, elbow, wrist, PIPs, MCPs, MTPs, carpal tunnel, sacroiliac joints)
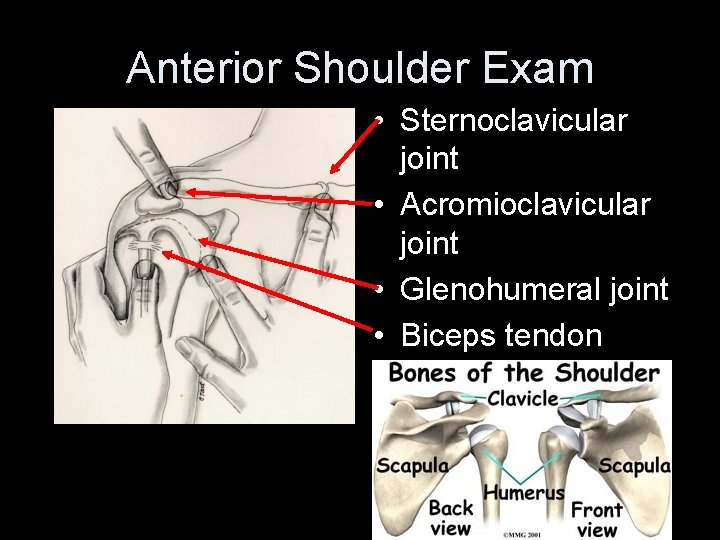
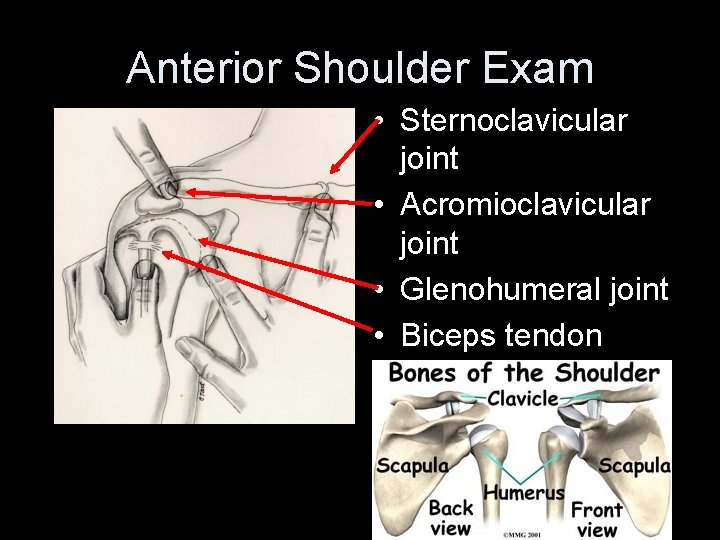
Anterior Shoulder Exam • Sternoclavicular joint • Acromioclavicular joint • Glenohumeral joint • Biceps tendon
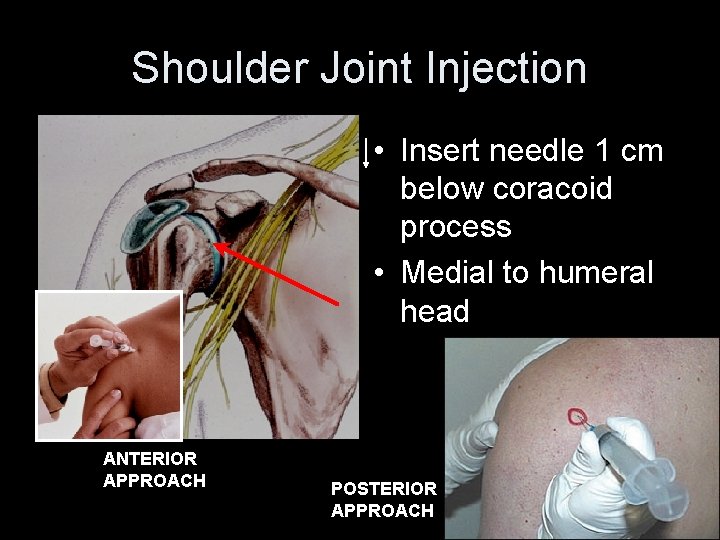
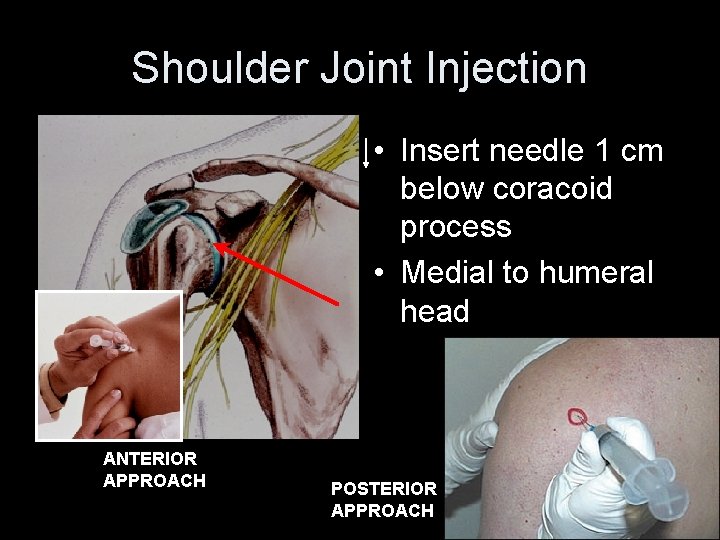
Shoulder Joint Injection • Insert needle 1 cm below coracoid process • Medial to humeral head ANTERIOR APPROACH POSTERIOR APPROACH
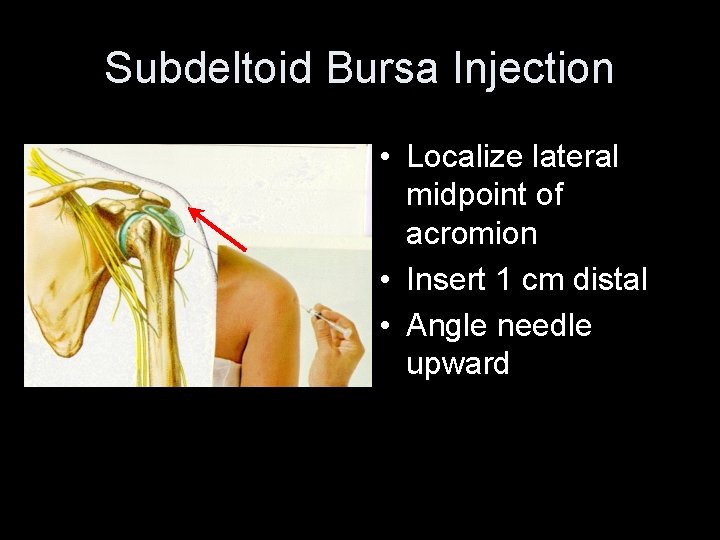
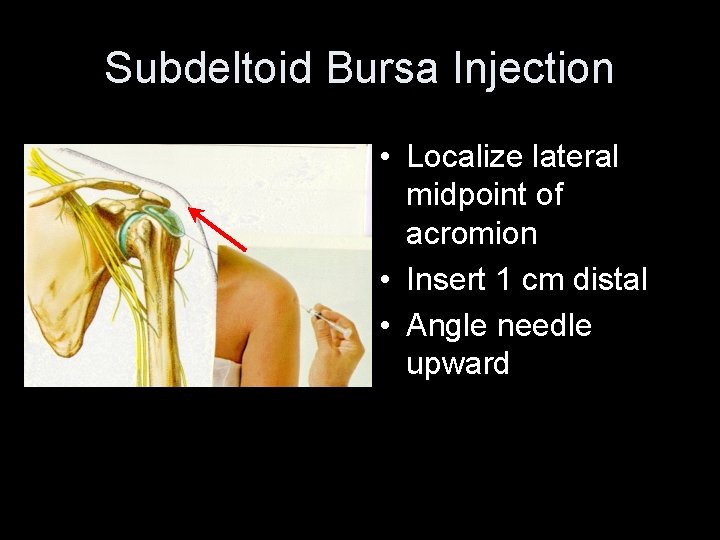
Subdeltoid Bursa Injection • Localize lateral midpoint of acromion • Insert 1 cm distal • Angle needle upward
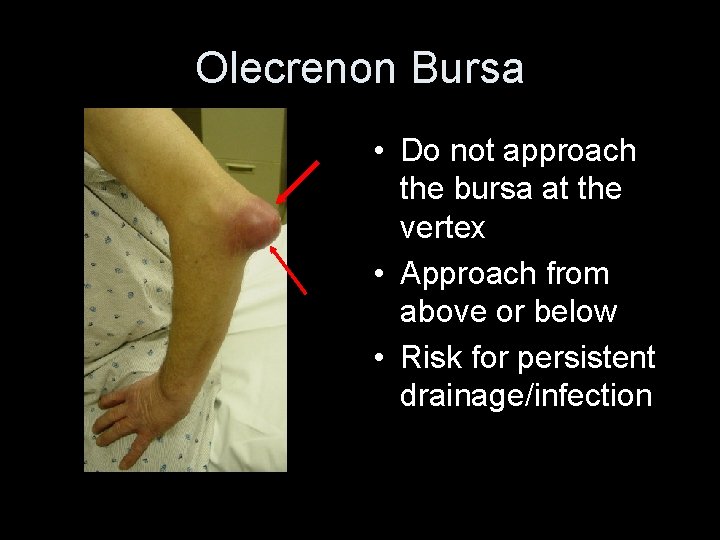
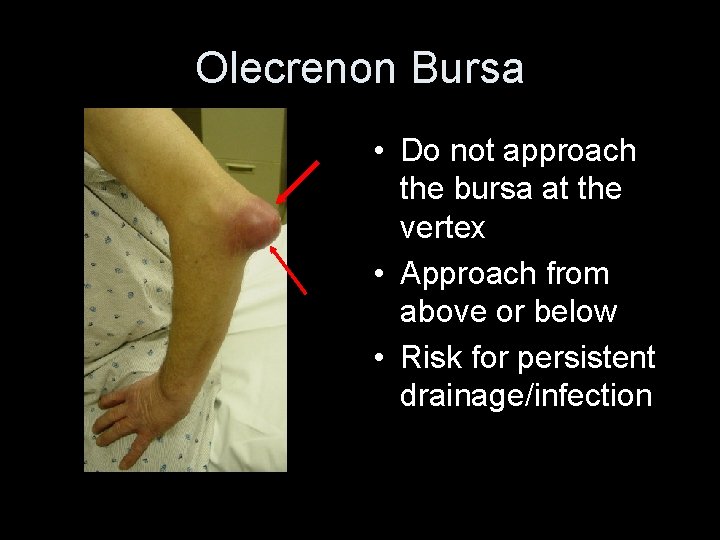
Olecrenon Bursa • Do not approach the bursa at the vertex • Approach from above or below • Risk for persistent drainage/infection
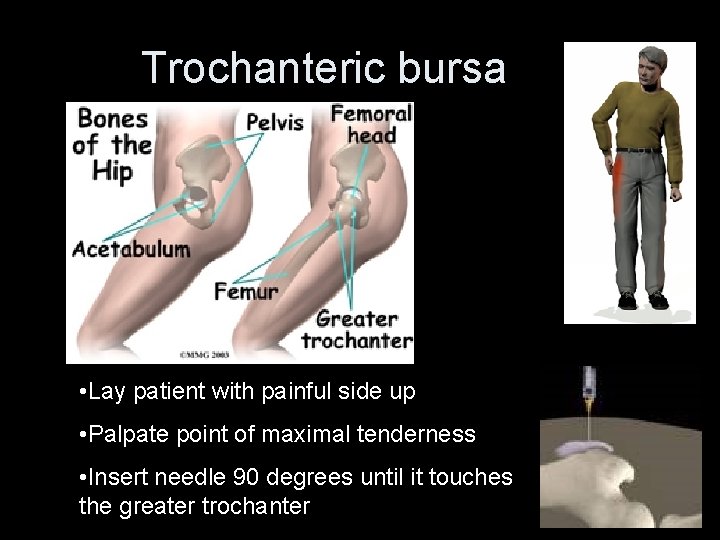
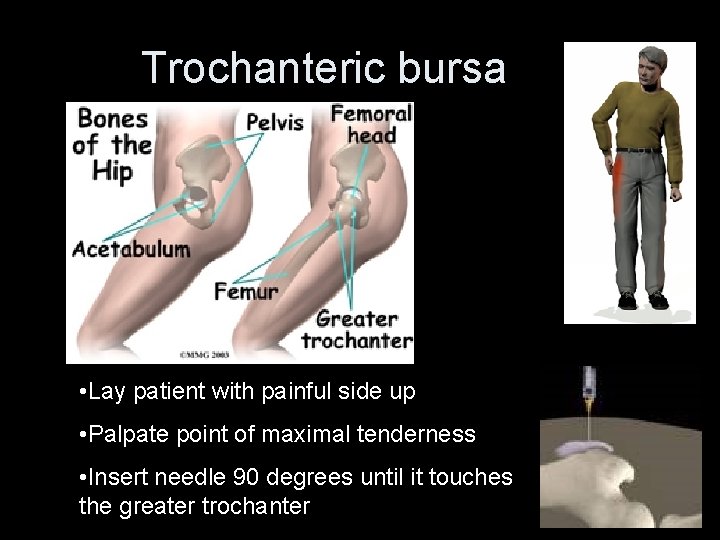
Trochanteric bursa • Lay patient with painful side up • Palpate point of maximal tenderness • Insert needle 90 degrees until it touches the greater trochanter
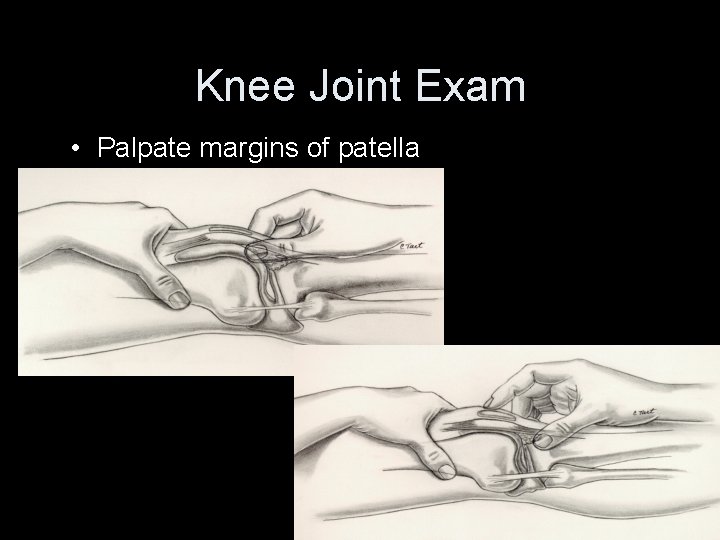
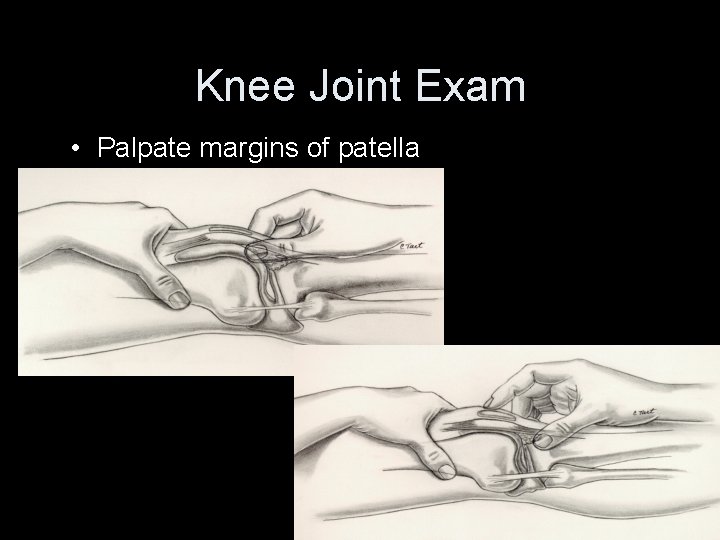
Knee Joint Exam • Palpate margins of patella
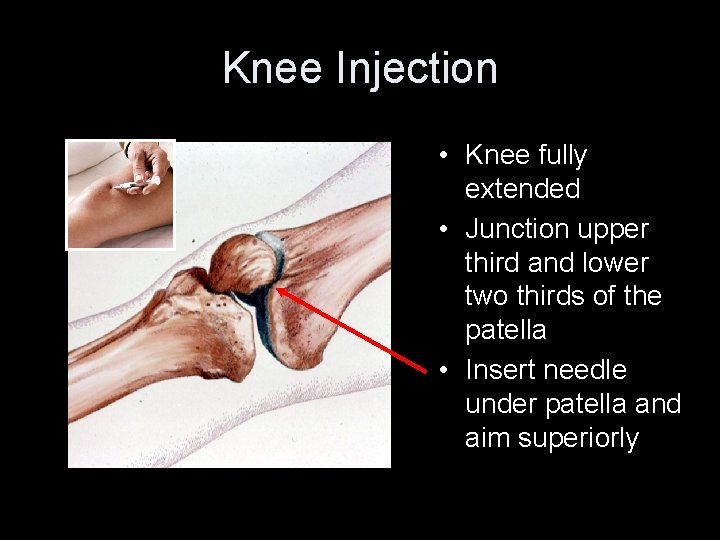
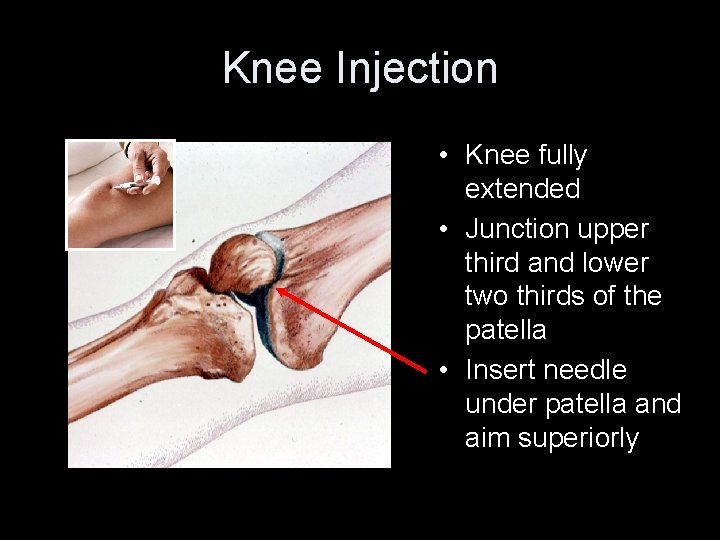
Knee Injection • Knee fully extended • Junction upper third and lower two thirds of the patella • Insert needle under patella and aim superiorly © ACR
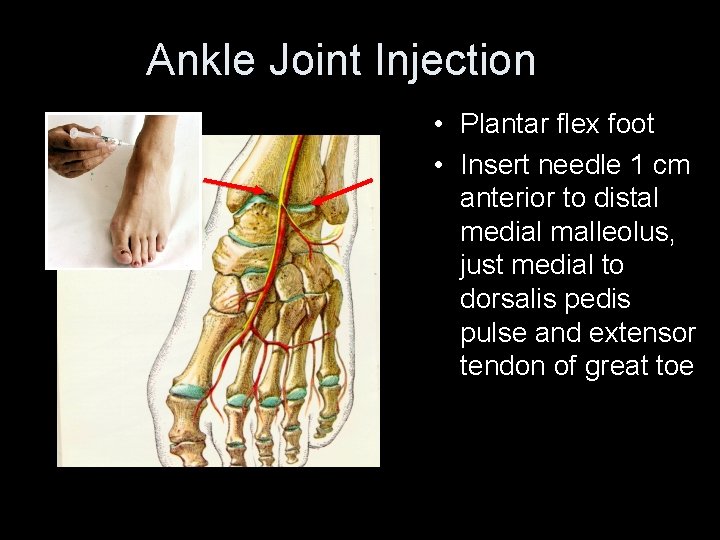
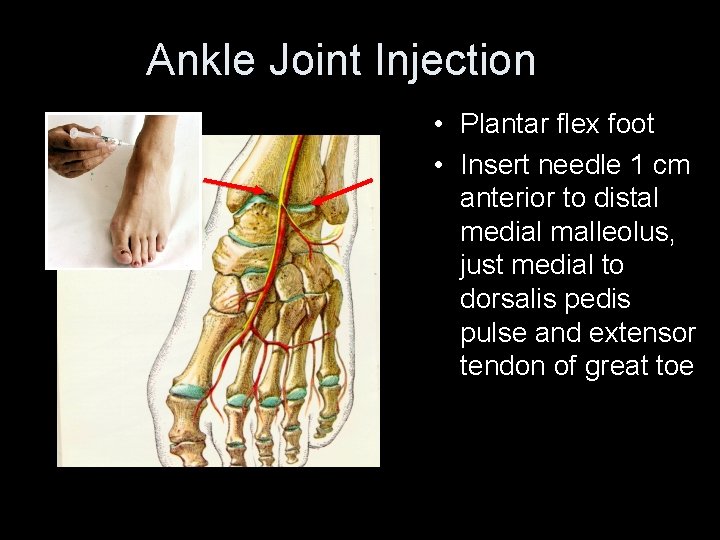
Ankle Joint Injection • Plantar flex foot • Insert needle 1 cm anterior to distal medial malleolus, just medial to dorsalis pedis pulse and extensor tendon of great toe
Synovial Fluid Analysis Document: Site Volume Viscosity Color Clarity
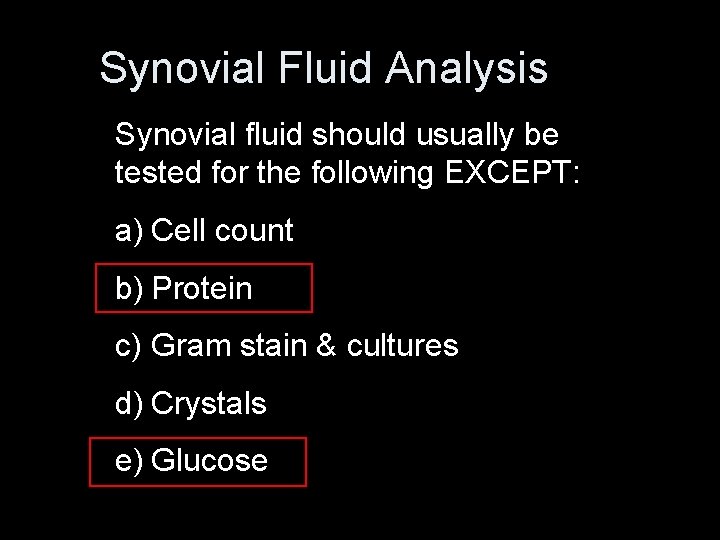
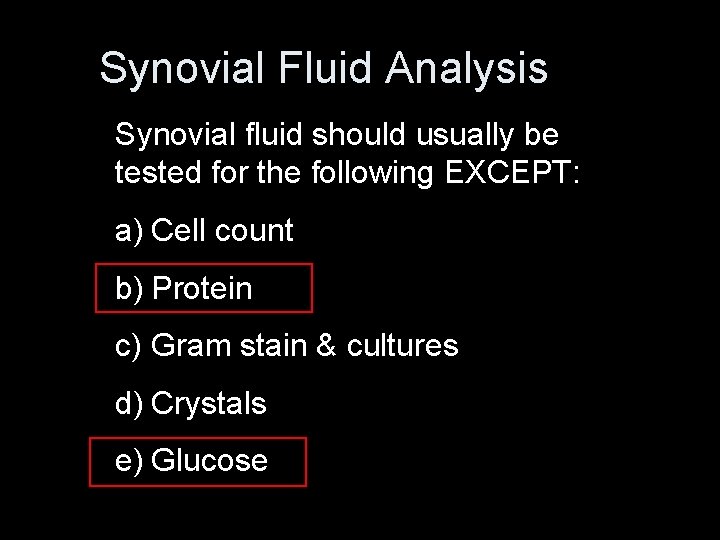
Synovial Fluid Analysis Synovial fluid should usually be tested for the following EXCEPT: a) Cell count b) Protein c) Gram stain & cultures d) Crystals e) Glucose
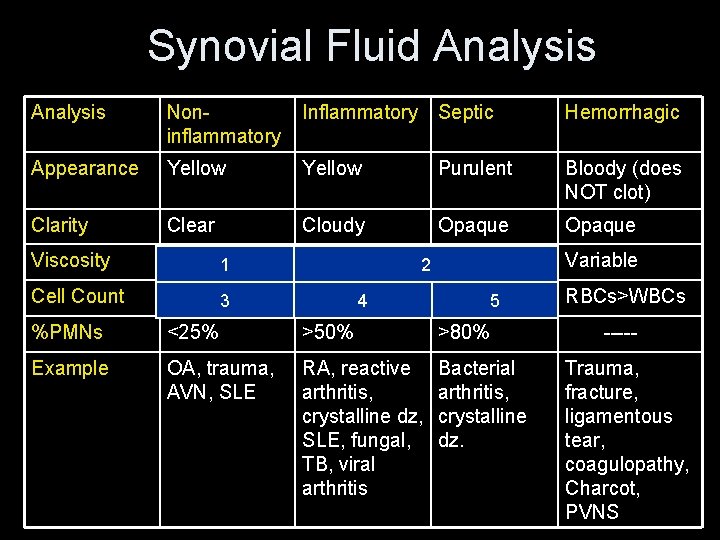
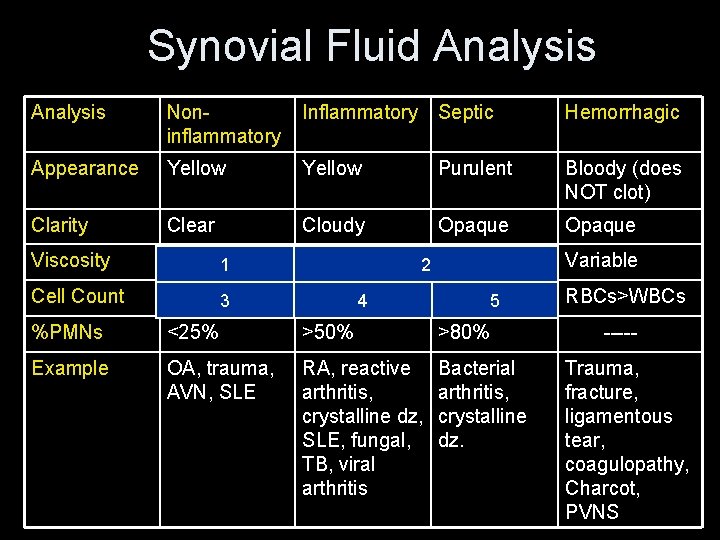
Synovial Fluid Analysis Noninflammatory Inflammatory Septic Hemorrhagic Appearance Yellow Purulent Bloody (does NOT clot) Clarity Clear Cloudy Opaque Viscosity High 1 Decreased 2 Decreased Variable Cell Count 200 -2, 000 3 2, 000 -75, 000 >50, 000 4 5 %PMNs <25% >50% >80% Example OA, trauma, AVN, SLE RA, reactive arthritis, crystalline dz, SLE, fungal, TB, viral arthritis Bacterial arthritis, crystalline dz. RBCs>WBCs ----Trauma, fracture, ligamentous tear, coagulopathy, Charcot, PVNS
nd 2 year resident question: What makes joint fluid viscous? Hyaluronan Intern question: How viscous is normal viscosity? >10 cm string
rd 3 year resident question: What common condition can yield very viscous fluid? hypothyroidism
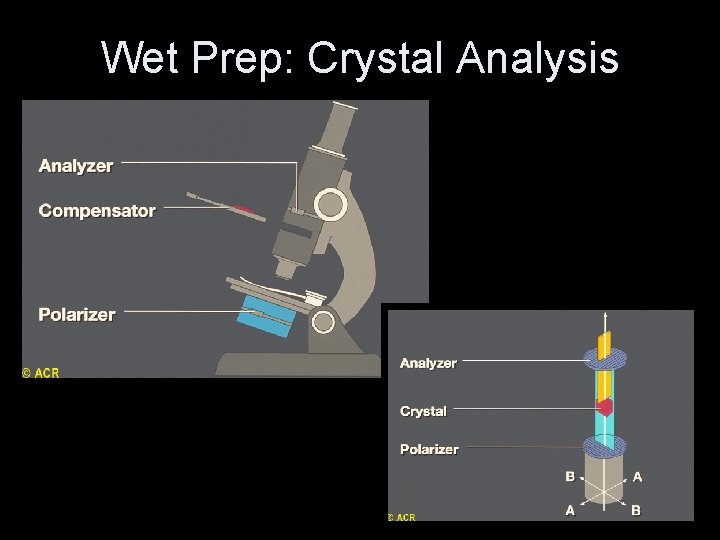
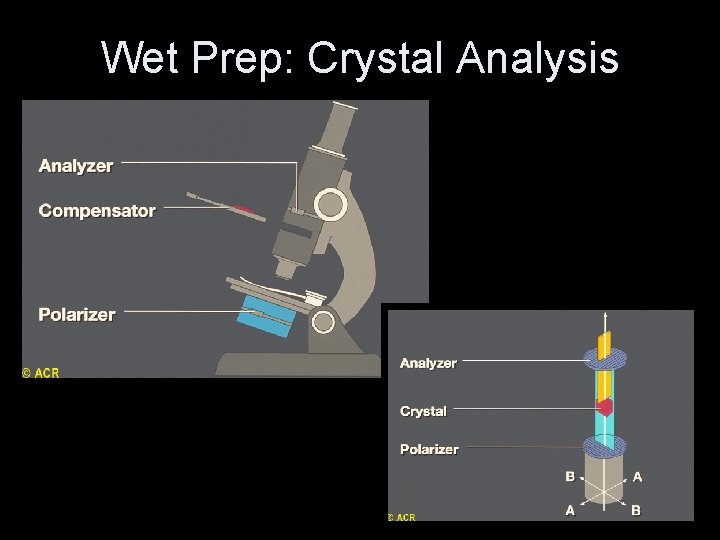
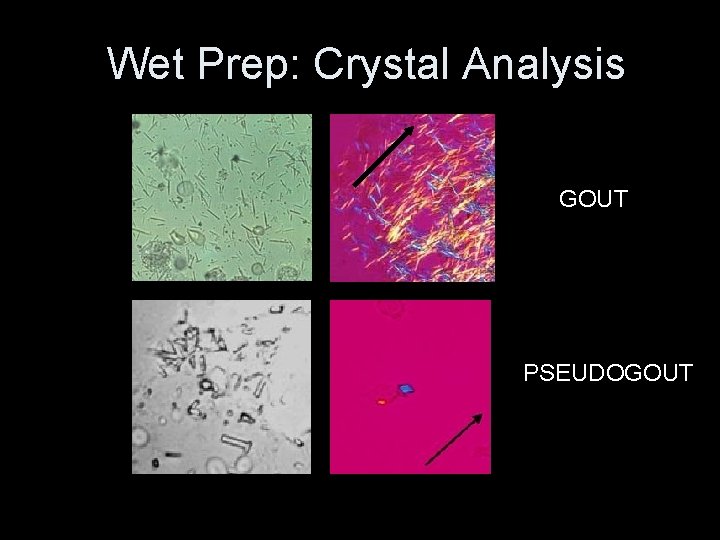
Wet Prep: Crystal Analysis
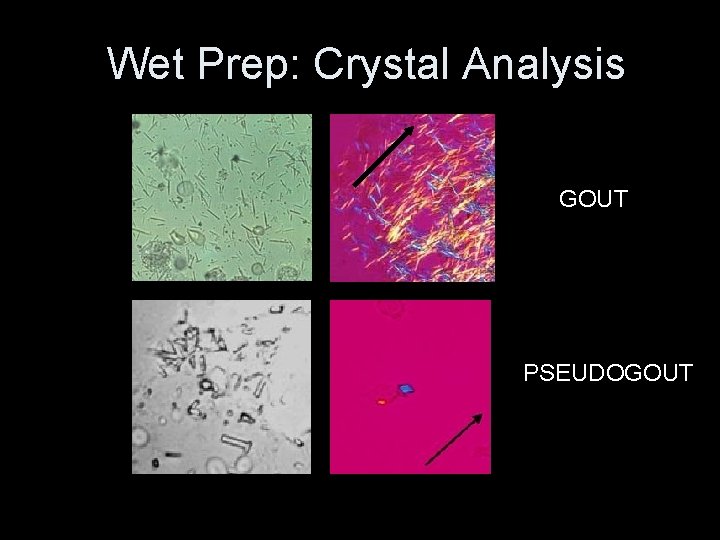
Wet Prep: Crystal Analysis GOUT PSEUDOGOUT
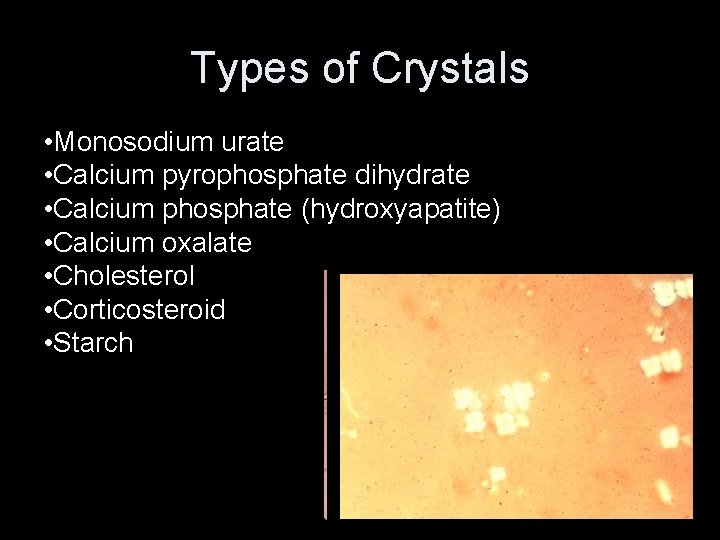
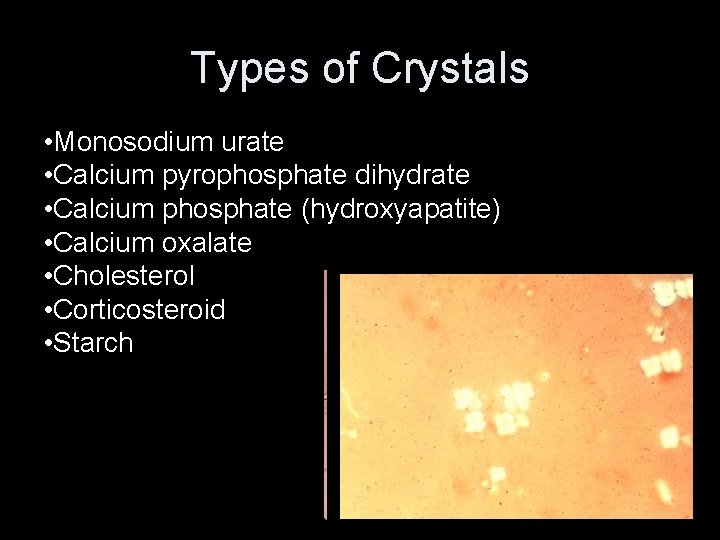
Types of Crystals • Monosodium urate • Calcium pyrophosphate dihydrate • Calcium phosphate (hydroxyapatite) • Calcium oxalate • Cholesterol • Corticosteroid • Starch
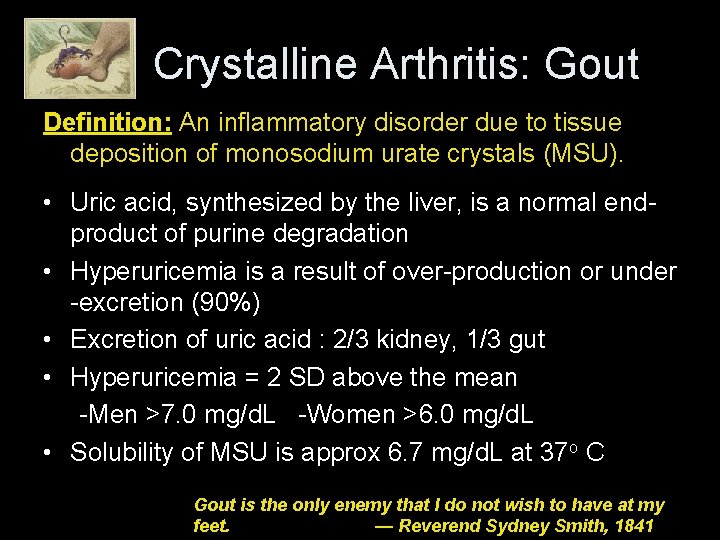
Crystalline Arthritis: Gout Definition: An inflammatory disorder due to tissue deposition of monosodium urate crystals (MSU). • Uric acid, synthesized by the liver, is a normal endproduct of purine degradation • Hyperuricemia is a result of over-production or under -excretion (90%) • Excretion of uric acid : 2/3 kidney, 1/3 gut • Hyperuricemia = 2 SD above the mean -Men >7. 0 mg/d. L -Women >6. 0 mg/d. L • Solubility of MSU is approx 6. 7 mg/d. L at 37 o C Gout is the only enemy that I do not wish to have at my feet. — Reverend Sydney Smith, 1841
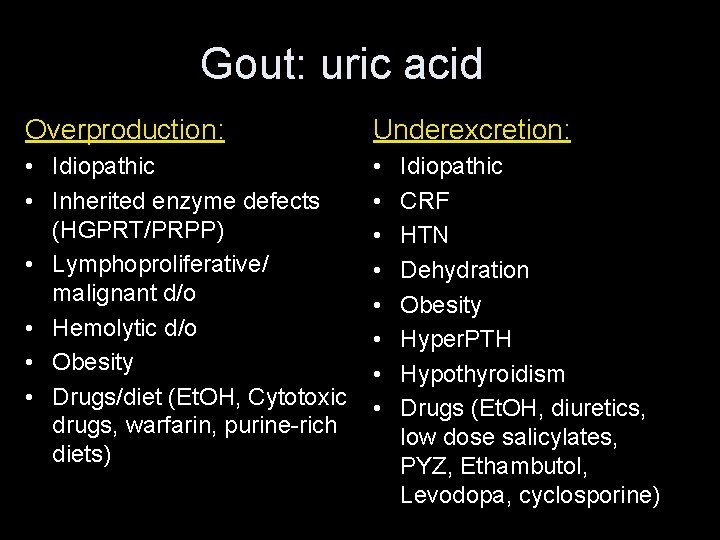
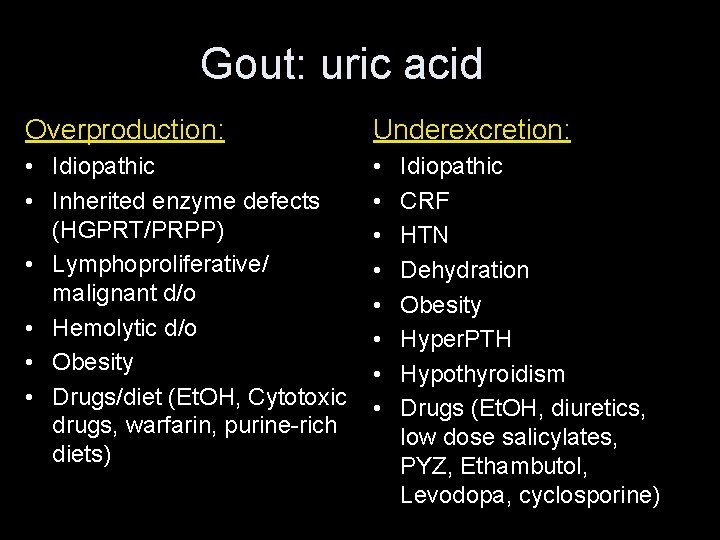
Gout: uric acid Overproduction: Underexcretion: • Idiopathic • Inherited enzyme defects (HGPRT/PRPP) • Lymphoproliferative/ malignant d/o • Hemolytic d/o • Obesity • Drugs/diet (Et. OH, Cytotoxic drugs, warfarin, purine-rich diets) • • Idiopathic CRF HTN Dehydration Obesity Hyper. PTH Hypothyroidism Drugs (Et. OH, diuretics, low dose salicylates, PYZ, Ethambutol, Levodopa, cyclosporine)
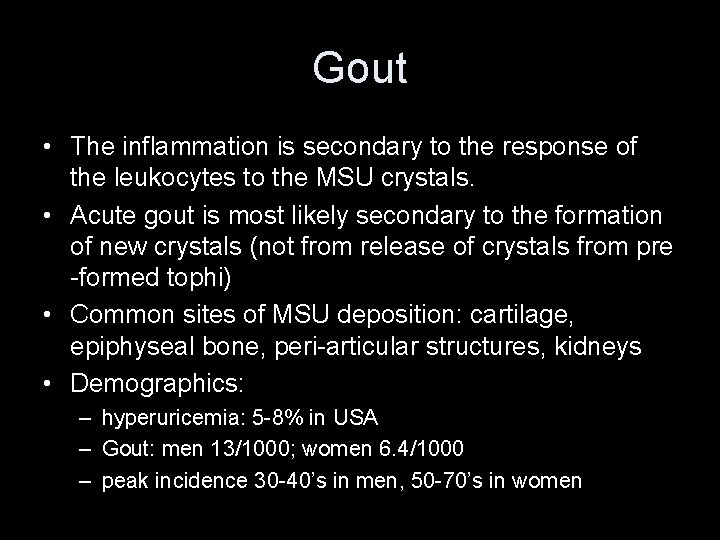
Gout • The inflammation is secondary to the response of the leukocytes to the MSU crystals. • Acute gout is most likely secondary to the formation of new crystals (not from release of crystals from pre -formed tophi) • Common sites of MSU deposition: cartilage, epiphyseal bone, peri-articular structures, kidneys • Demographics: – hyperuricemia: 5 -8% in USA – Gout: men 13/1000; women 6. 4/1000 – peak incidence 30 -40’s in men, 50 -70’s in women
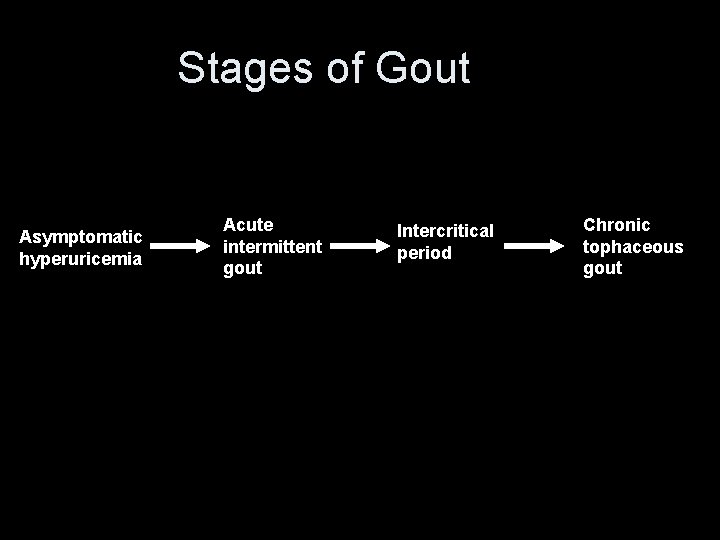
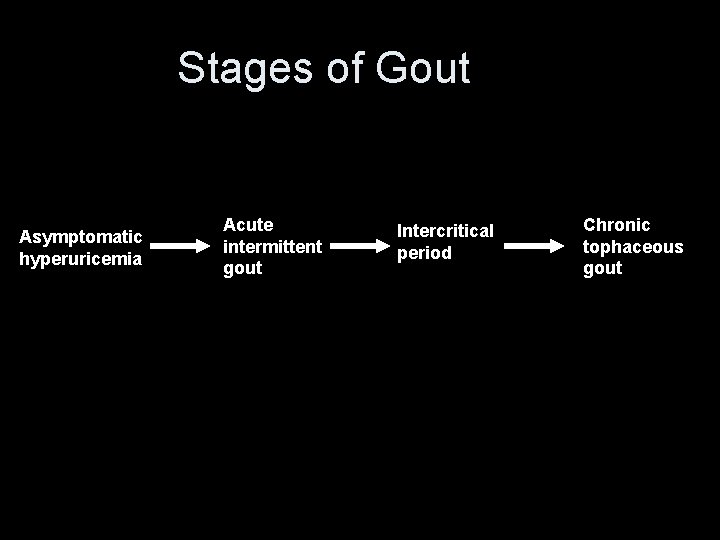
Stages of Gout Asymptomatic hyperuricemia Acute intermittent gout Intercritical period Chronic tophaceous gout
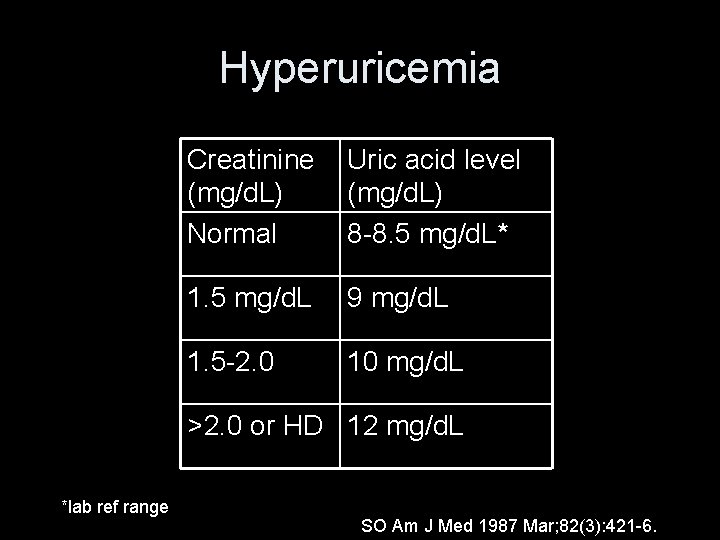
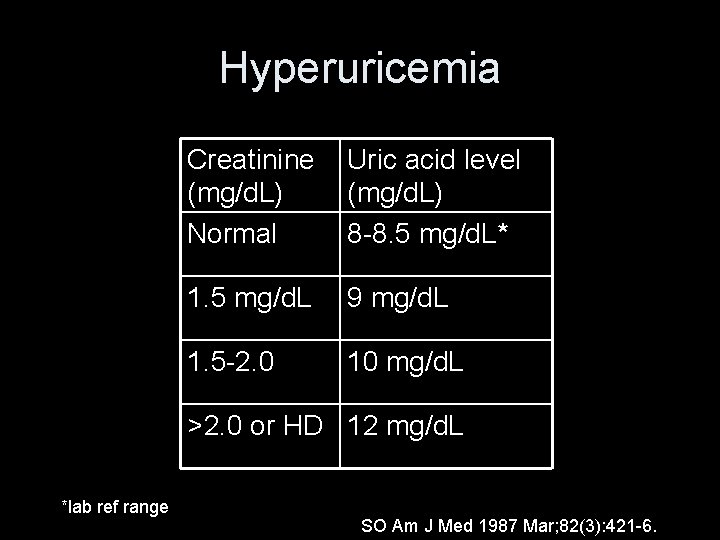
Hyperuricemia Creatinine (mg/d. L) Normal Uric acid level (mg/d. L) 8 -8. 5 mg/d. L* 1. 5 mg/d. L 9 mg/d. L 1. 5 -2. 0 10 mg/d. L >2. 0 or HD 12 mg/d. L *lab ref range SO Am J Med 1987 Mar; 82(3): 421 -6.
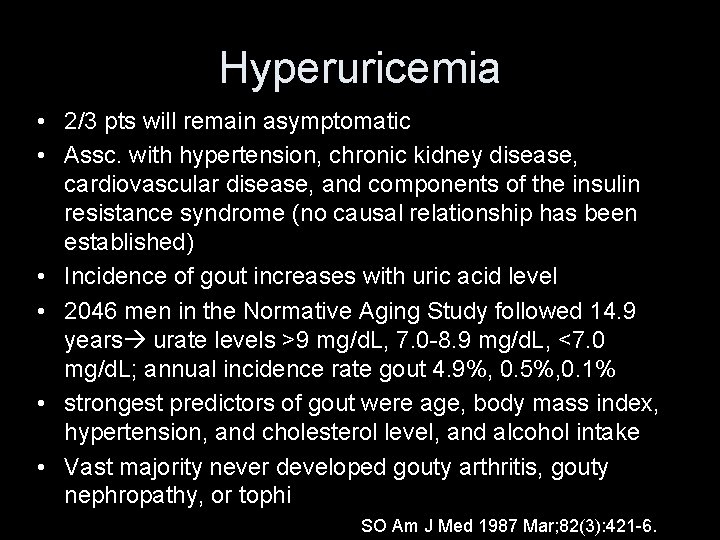
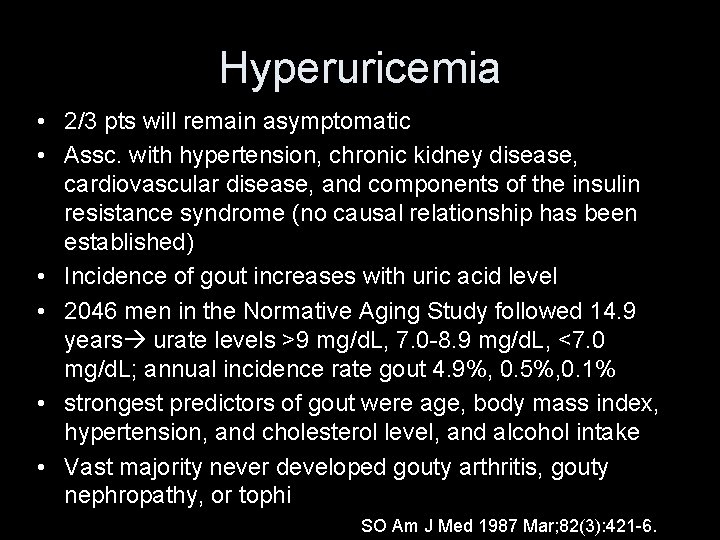
Hyperuricemia • 2/3 pts will remain asymptomatic • Assc. with hypertension, chronic kidney disease, cardiovascular disease, and components of the insulin resistance syndrome (no causal relationship has been established) • Incidence of gout increases with uric acid level • 2046 men in the Normative Aging Study followed 14. 9 years urate levels >9 mg/d. L, 7. 0 -8. 9 mg/d. L, <7. 0 mg/d. L; annual incidence rate gout 4. 9%, 0. 5%, 0. 1% • strongest predictors of gout were age, body mass index, hypertension, and cholesterol level, and alcohol intake • Vast majority never developed gouty arthritis, gouty nephropathy, or tophi SO Am J Med 1987 Mar; 82(3): 421 -6.
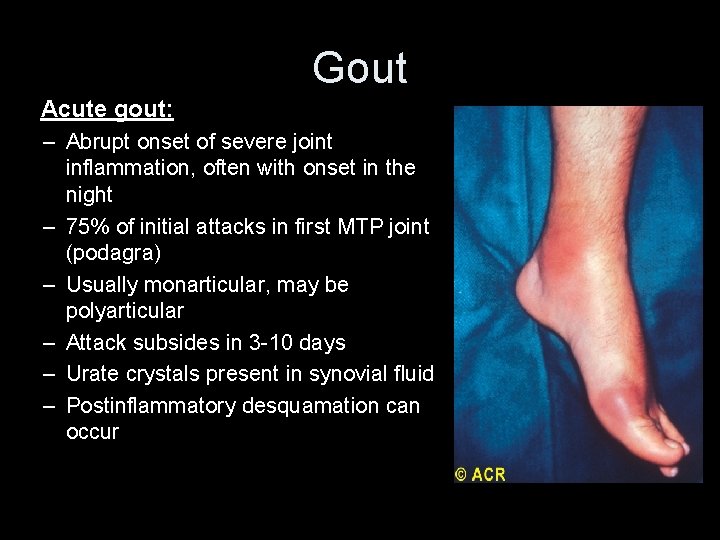
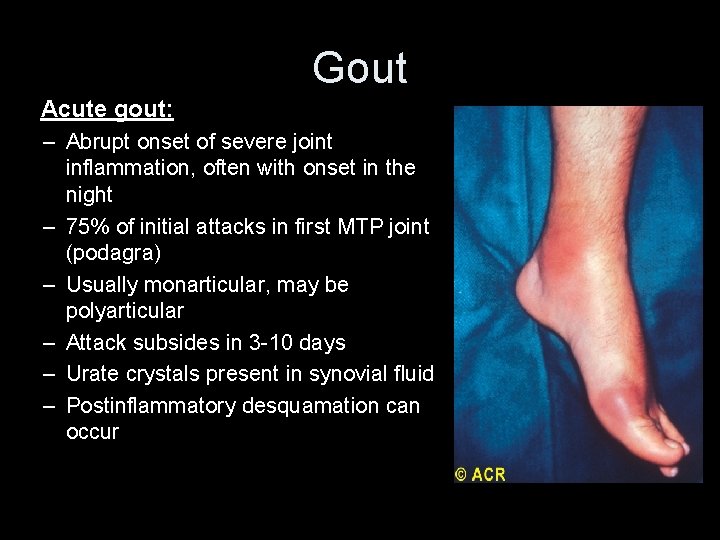
Gout Acute gout: – Abrupt onset of severe joint inflammation, often with onset in the night – 75% of initial attacks in first MTP joint (podagra) – Usually monarticular, may be polyarticular – Attack subsides in 3 -10 days – Urate crystals present in synovial fluid – Postinflammatory desquamation can occur
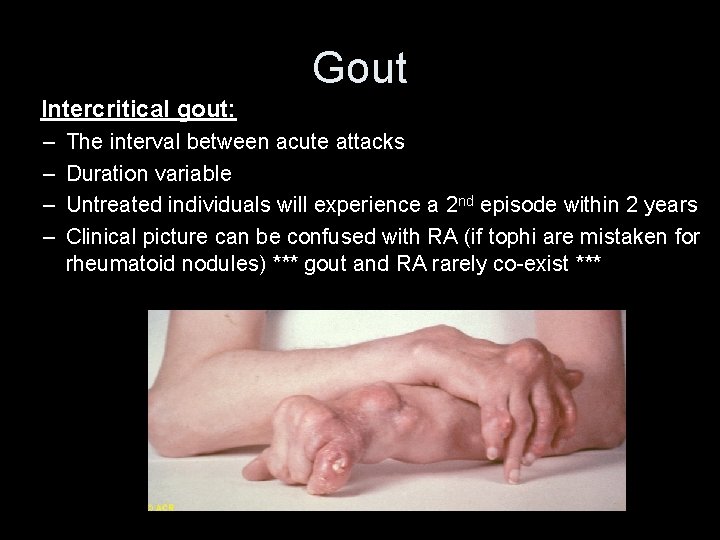
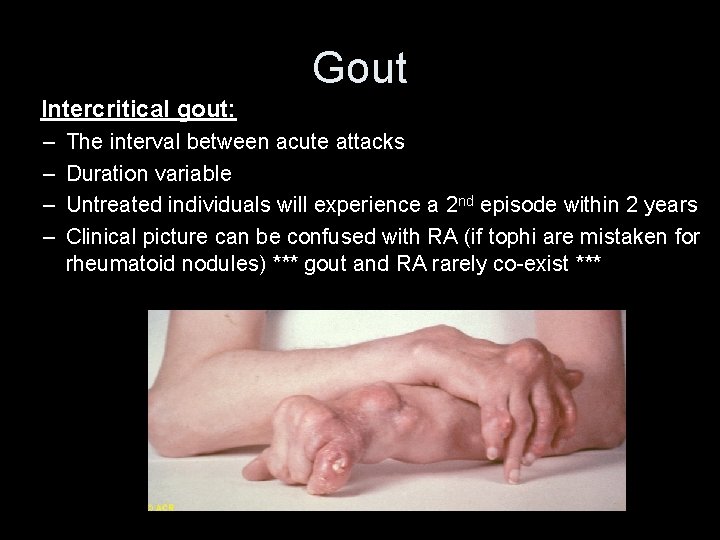
Gout Intercritical gout: – – The interval between acute attacks Duration variable Untreated individuals will experience a 2 nd episode within 2 years Clinical picture can be confused with RA (if tophi are mistaken for rheumatoid nodules) *** gout and RA rarely co-exist ***
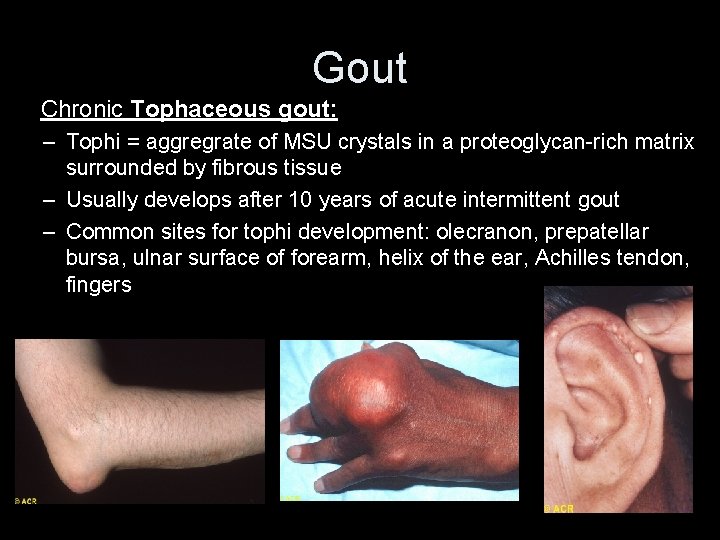
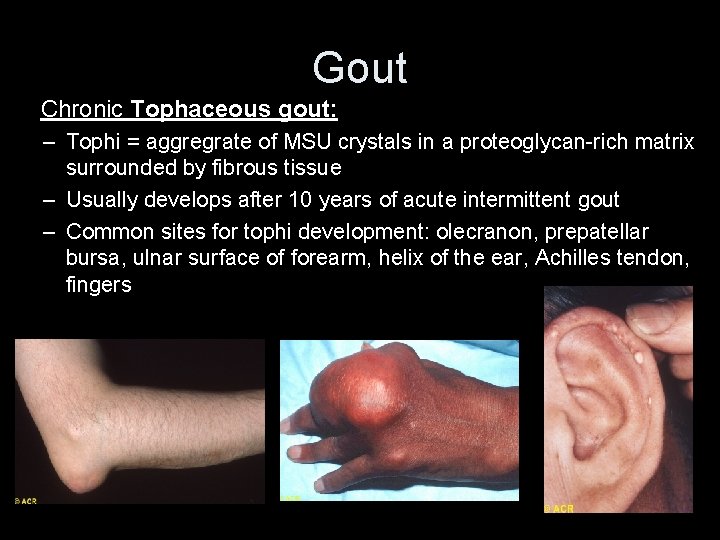
Gout Chronic Tophaceous gout: – Tophi = aggregrate of MSU crystals in a proteoglycan-rich matrix surrounded by fibrous tissue – Usually develops after 10 years of acute intermittent gout – Common sites for tophi development: olecranon, prepatellar bursa, ulnar surface of forearm, helix of the ear, Achilles tendon, fingers
Gout • Diagnostic Tests: – During an attack, labs may show: elevated ESR/CRP, uric acid, leukocytosis, thrombocytosis – Joint fluid: WBC >2000 with >75% NO, intracellular crystal needle-shaped, neg. birefringent 5 -25 um – Always send fluid for cultures as septic arthritis may coexist with gout – Serum Cr and 24 hour urine for uric acid useful to assess risk for renal stones and for planning therapy • Urinary levels are normal below 750 mg/ 24 h; > 1100 mg/dl increase risk for nephrolithiasis by 50%
Intern question: A 40 y. o obese male patient presents acutely with 1 st MTP joint swelling, redness and pain. He cannot put a sheet over his foot. You evaluated him and thought it looked like podagra, but on labs his uric acid level is 3. 1 mg/d. L. Does he have gout? Yes. 40% of patients will have a normal uric acid level during an acute attack.
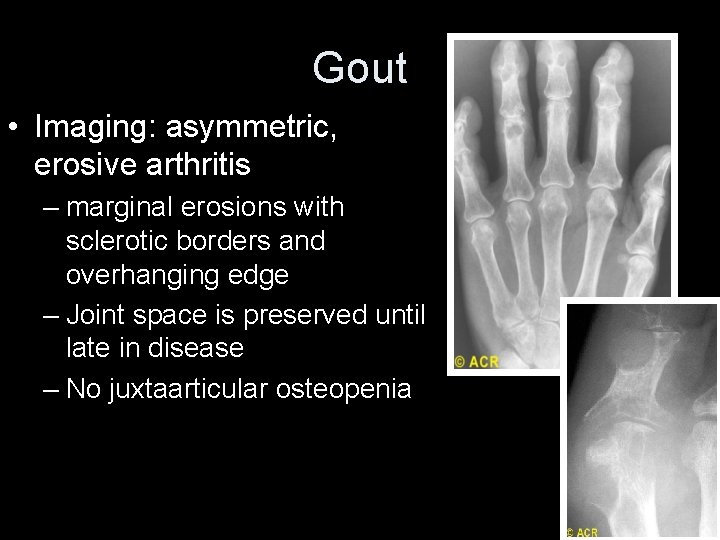
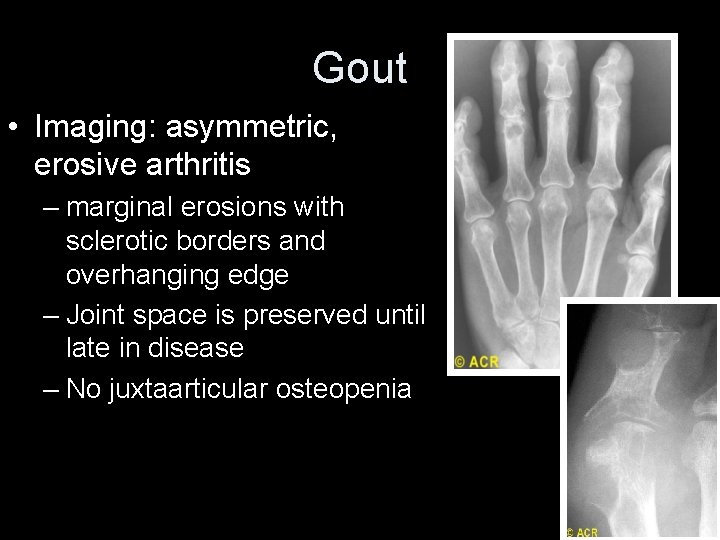
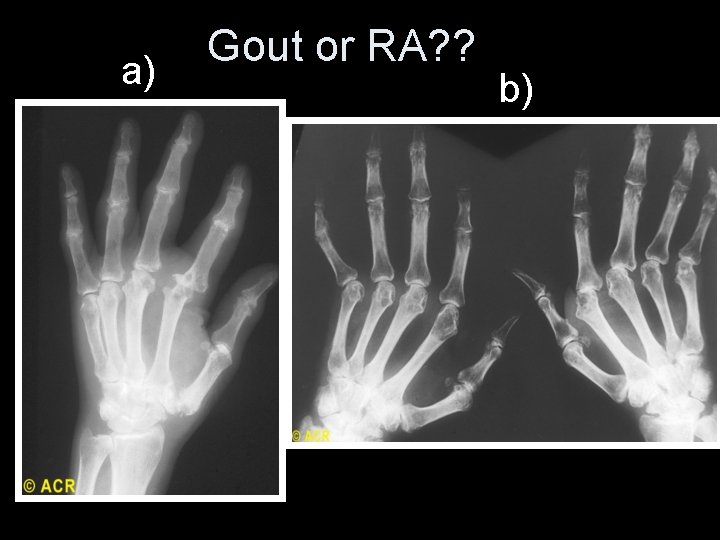
Gout • Imaging: asymmetric, erosive arthritis – marginal erosions with sclerotic borders and overhanging edge – Joint space is preserved until late in disease – No juxtaarticular osteopenia
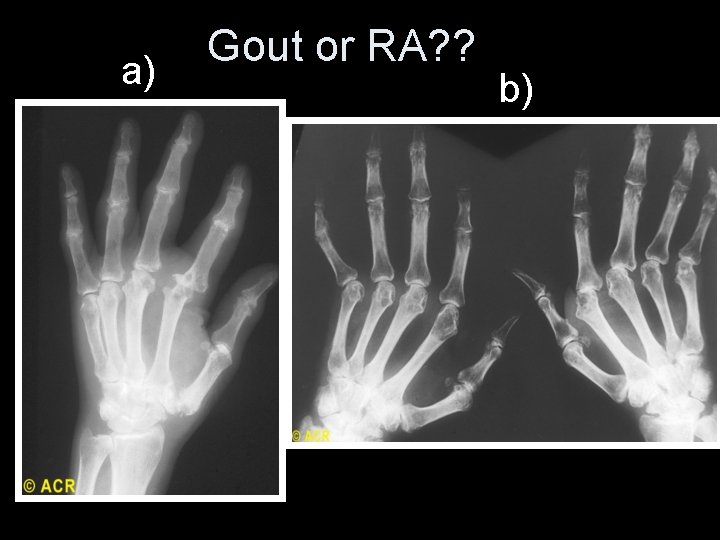
a) Gout or RA? ? b)
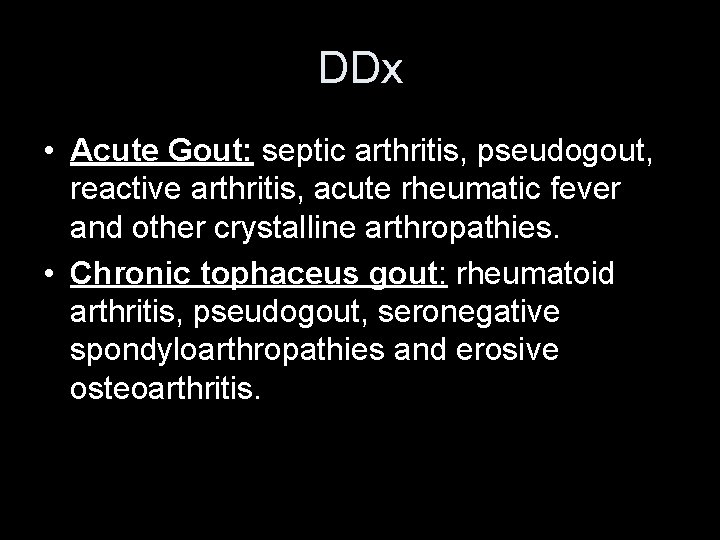
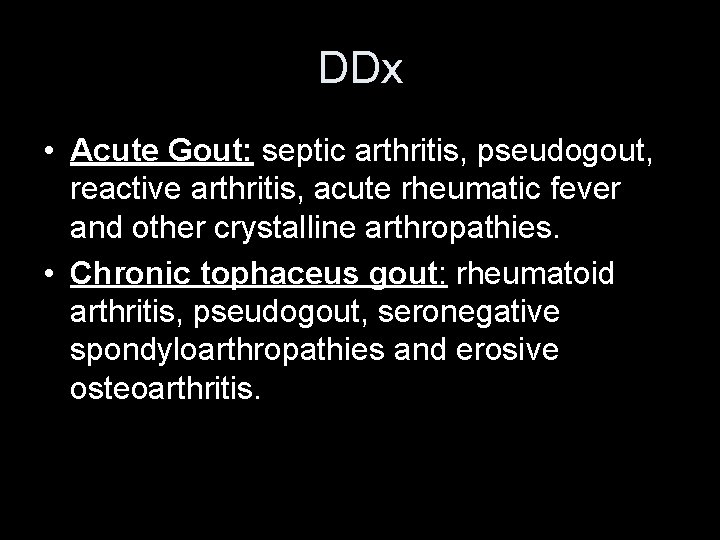
DDx • Acute Gout: septic arthritis, pseudogout, reactive arthritis, acute rheumatic fever and other crystalline arthropathies. • Chronic tophaceus gout: rheumatoid arthritis, pseudogout, seronegative spondyloarthropathies and erosive osteoarthritis.
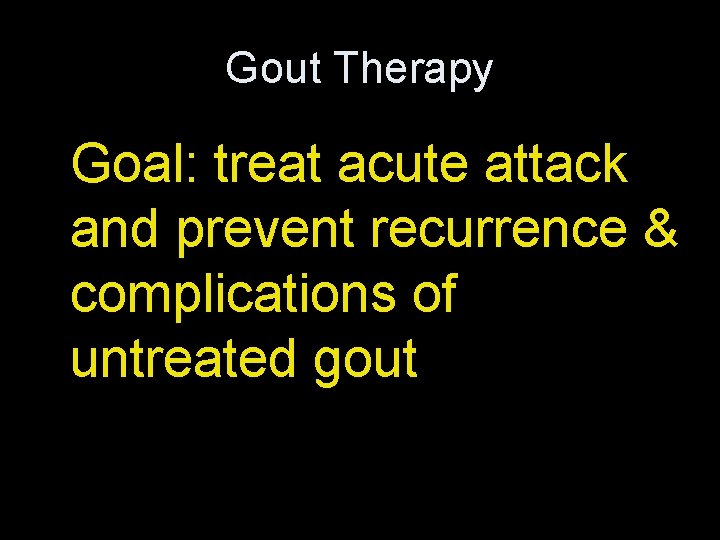
Gout Therapy Goal: treat acute attack and prevent recurrence & complications of untreated gout
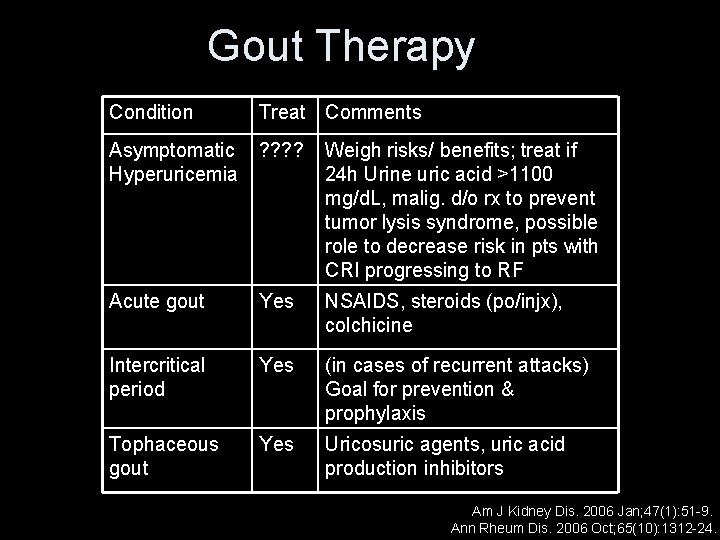
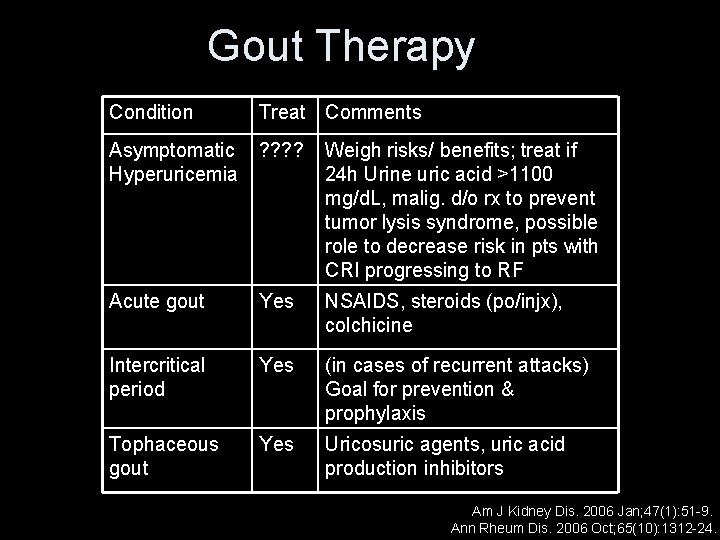
Gout Therapy Condition Treat Comments Asymptomatic Hyperuricemia ? ? Weigh risks/ benefits; treat if 24 h Urine uric acid >1100 mg/d. L, malig. d/o rx to prevent tumor lysis syndrome, possible role to decrease risk in pts with CRI progressing to RF Acute gout Yes NSAIDS, steroids (po/injx), colchicine Intercritical period Yes (in cases of recurrent attacks) Goal for prevention & prophylaxis Tophaceous gout Yes Uricosuric agents, uric acid production inhibitors Am J Kidney Dis. 2006 Jan; 47(1): 51 -9. Ann Rheum Dis. 2006 Oct; 65(10): 1312 -24.
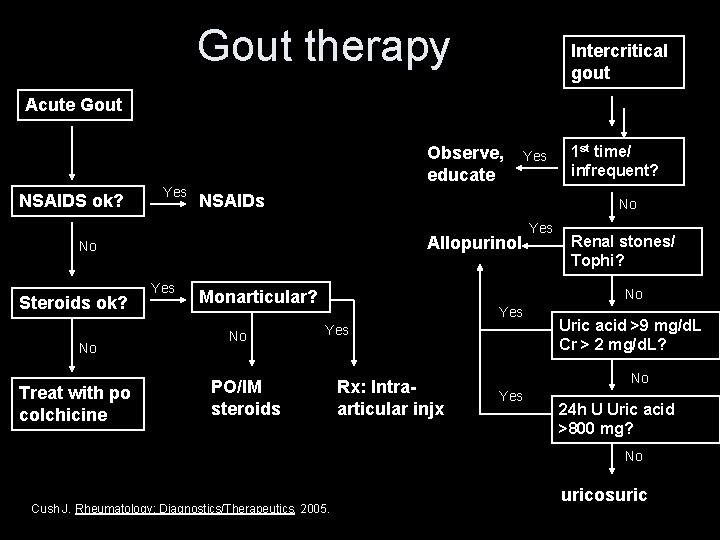
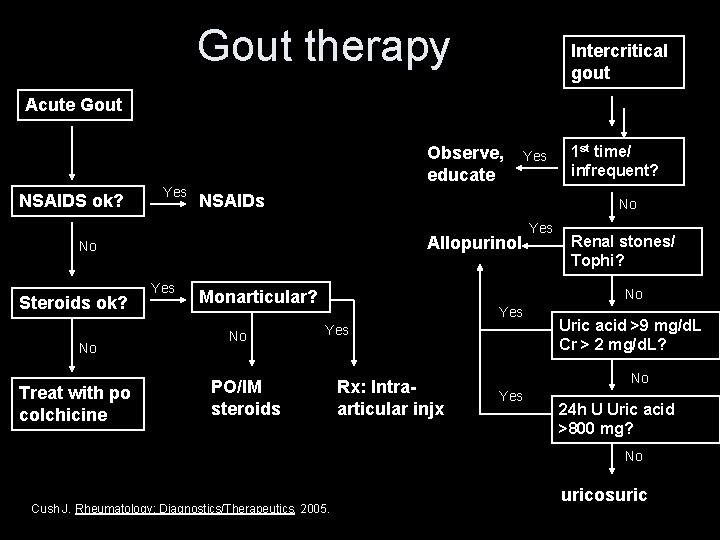
Gout therapy Intercritical gout Acute Gout Observe, educate NSAIDS ok? Yes NSAIDs Allopurinol No Treat with po colchicine Yes Renal stones/ Tophi? No Monarticular? No 1 st time/ infrequent? No No Steroids ok? Yes Yes PO/IM steroids Rx: Intraarticular injx Uric acid >9 mg/d. L Cr > 2 mg/d. L? No Yes 24 h U Uric acid >800 mg? No Cush J. Rheumatology: Diagnostics/Therapeutics, 2005. uricosuric
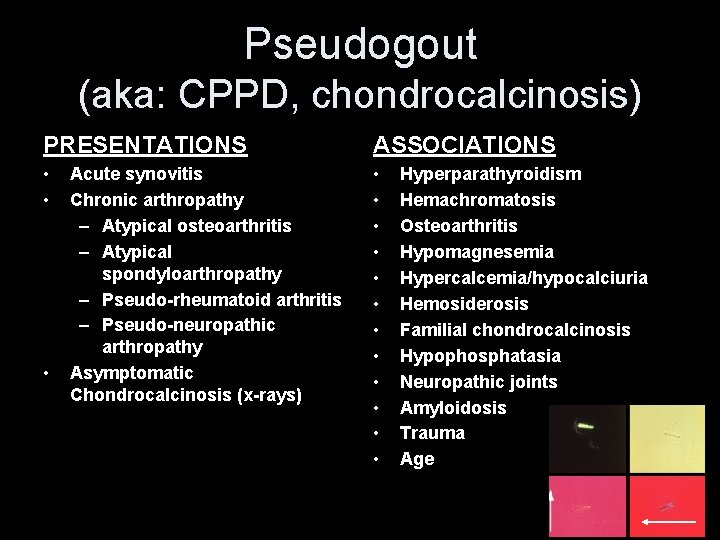
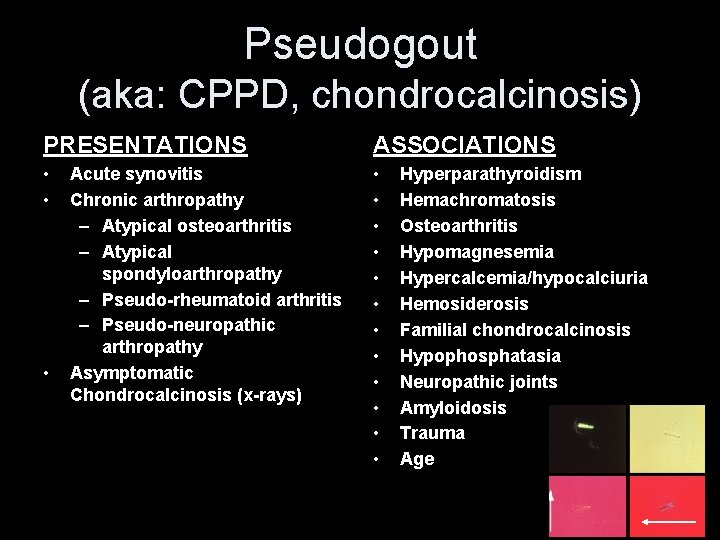
Pseudogout (aka: CPPD, chondrocalcinosis) PRESENTATIONS ASSOCIATIONS • • • • Acute synovitis Chronic arthropathy – Atypical osteoarthritis – Atypical spondyloarthropathy – Pseudo-rheumatoid arthritis – Pseudo-neuropathic arthropathy Asymptomatic Chondrocalcinosis (x-rays) Hyperparathyroidism Hemachromatosis Osteoarthritis Hypomagnesemia Hypercalcemia/hypocalciuria Hemosiderosis Familial chondrocalcinosis Hypophosphatasia Neuropathic joints Amyloidosis Trauma Age
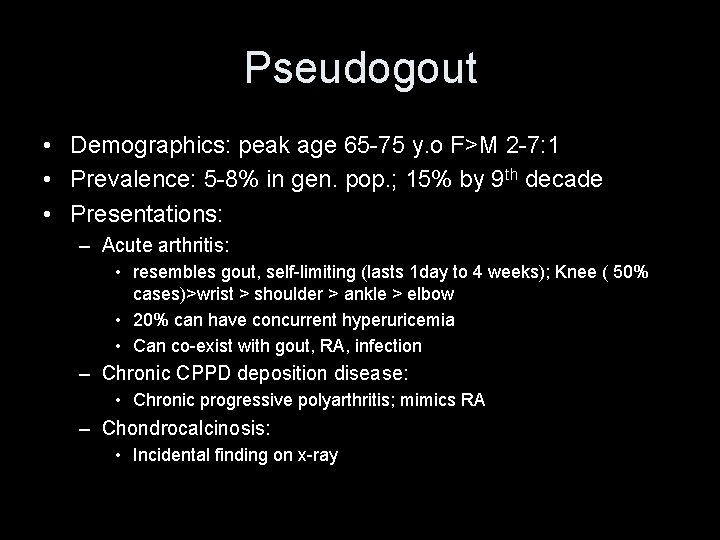
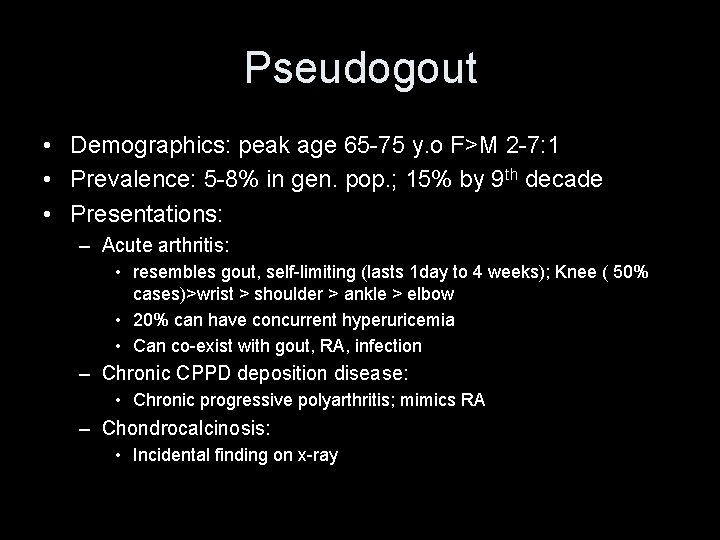
Pseudogout • Demographics: peak age 65 -75 y. o F>M 2 -7: 1 • Prevalence: 5 -8% in gen. pop. ; 15% by 9 th decade • Presentations: – Acute arthritis: • resembles gout, self-limiting (lasts 1 day to 4 weeks); Knee ( 50% cases)>wrist > shoulder > ankle > elbow • 20% can have concurrent hyperuricemia • Can co-exist with gout, RA, infection – Chronic CPPD deposition disease: • Chronic progressive polyarthritis; mimics RA – Chondrocalcinosis: • Incidental finding on x-ray
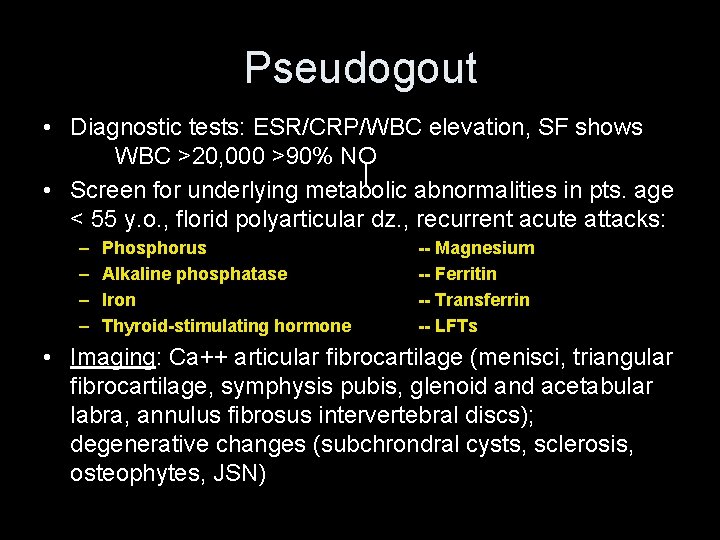
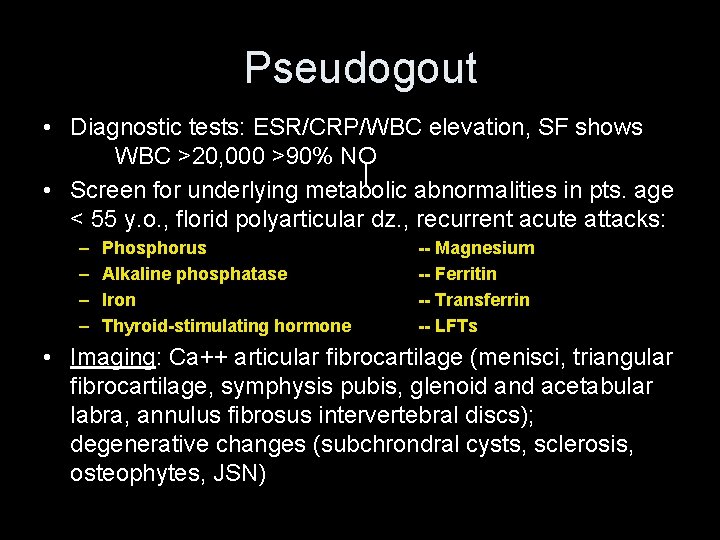
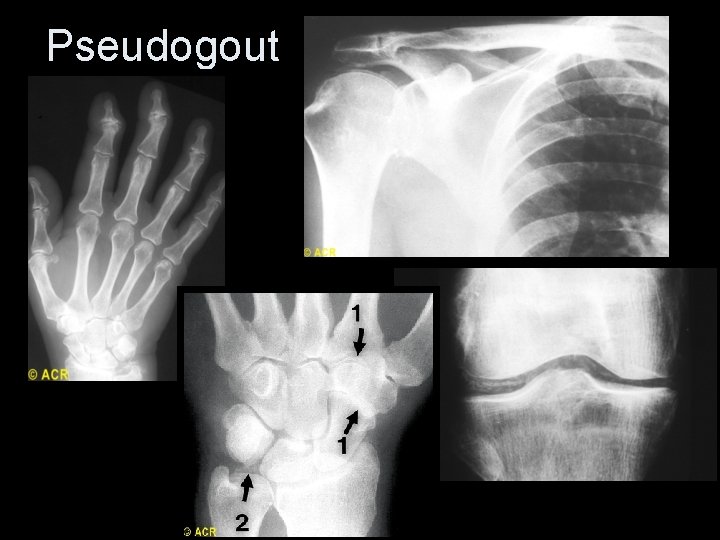
Pseudogout • Diagnostic tests: ESR/CRP/WBC elevation, SF shows WBC >20, 000 >90% NO • Screen for underlying metabolic abnormalities in pts. age < 55 y. o. , florid polyarticular dz. , recurrent acute attacks: – – Phosphorus Alkaline phosphatase Iron Thyroid-stimulating hormone -- Magnesium -- Ferritin -- Transferrin -- LFTs • Imaging: Ca++ articular fibrocartilage (menisci, triangular fibrocartilage, symphysis pubis, glenoid and acetabular labra, annulus fibrosus intervertebral discs); degenerative changes (subchrondral cysts, sclerosis, osteophytes, JSN)
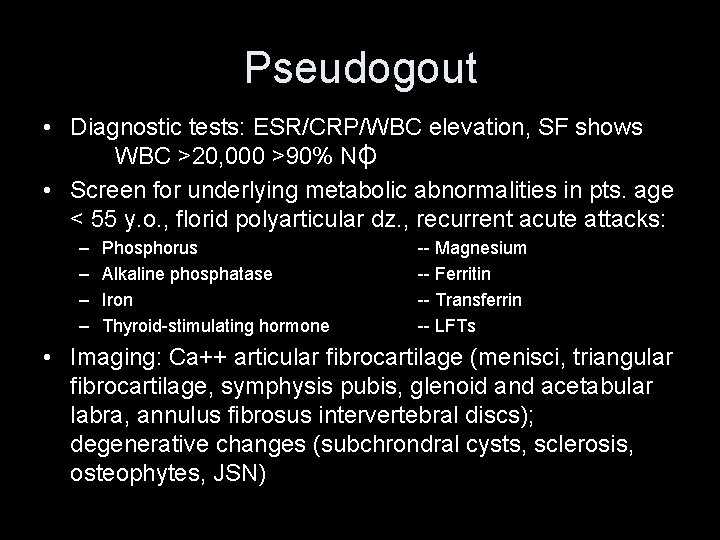
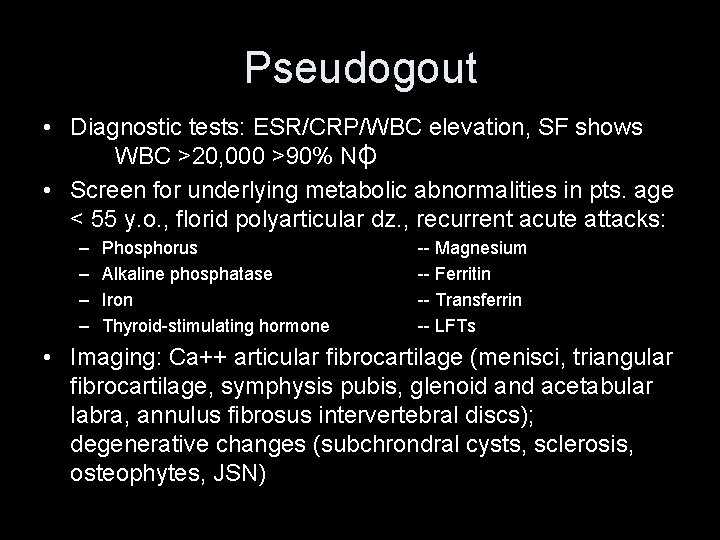
Pseudogout • Diagnostic tests: ESR/CRP/WBC elevation, SF shows WBC >20, 000 >90% NO • Screen for underlying metabolic abnormalities in pts. age < 55 y. o. , florid polyarticular dz. , recurrent acute attacks: – – Phosphorus Alkaline phosphatase Iron Thyroid-stimulating hormone -- Magnesium -- Ferritin -- Transferrin -- LFTs • Imaging: Ca++ articular fibrocartilage (menisci, triangular fibrocartilage, symphysis pubis, glenoid and acetabular labra, annulus fibrosus intervertebral discs); degenerative changes (subchrondral cysts, sclerosis, osteophytes, JSN)
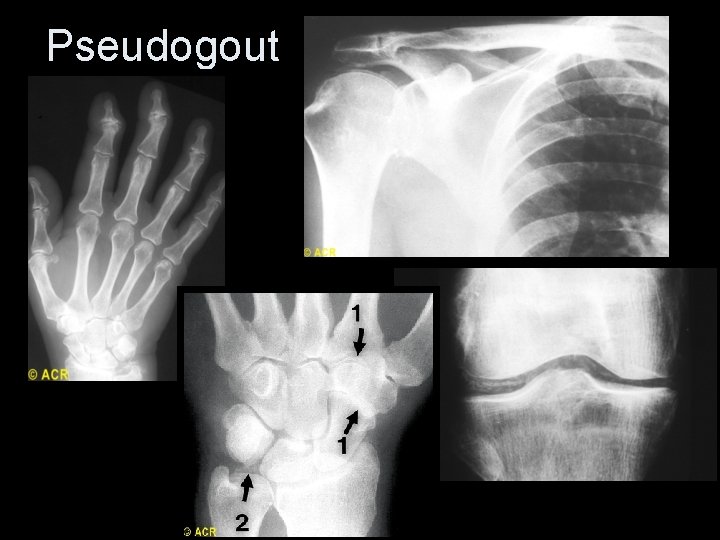
Pseudogout
Pseudogout Rx • • • Steroid injection NSAIDs Colchicine (in acute Rx and for prophylaxis) PO steroids (no controlled trials) Identify and treat underlying metabolic disorder
Conclusions • • Most joints can be aspirated and injected Always obtain informed consent Use good techniques Gout and pseudogout are common causes of inflammatory arthritis, but can easily be treated.

Review Video