Aspheric Diffractive Versus Refractive Multifocal IOLs Comparison of
- Slides: 12
Aspheric Diffractive Versus Refractive Multifocal IOLs: Comparison of Visual Prognosis and Patient Satisfaction Eltutar, Kadir; Akcetin, Tulay A. ; Ozcelik, N. Demet Istanbul Education and Research Hospital Department of Ophthalmology The authors state that they have no proprietary interest and they have not received any grants or funds in support of the study.
Purpose: To evaluate the optical and visual performance after bilateral implantation of refractive and aspheric diffractive multifocal intraocular lenses.
Methods: The primary objective of the study was to determine the uncorrected distance, intermediate and near visual acuities after uncomplicated cataract surgery, and bilateral MIOL implantation. 10 patients who had bilateral implantation of the aspheric diffractive MIOL (n=20; + 4. 00 D add), and 10 patients who had bilateral implantation of the refractive MIOL (n=20, + 3. 50 add) were enrolled. Spectacle independency, patient satisfaction and photic phenomena were evaluated. The study was carried out prospectively with a followup period lasting for six months postoperatively.
Methods: Patients had to follow the examination dates on postoperative days 1, 30 and 180. Immersion A-scan biometry was used for axial length measurements with targeted emmetropia using SRK-T formula. Distance visual acuities were achieved by ETDRS chart at 4, 0 meters, intermediate (60. 0 cm) and near (40. 0 cm) visual acuities were evaluated with Jaeger cards.
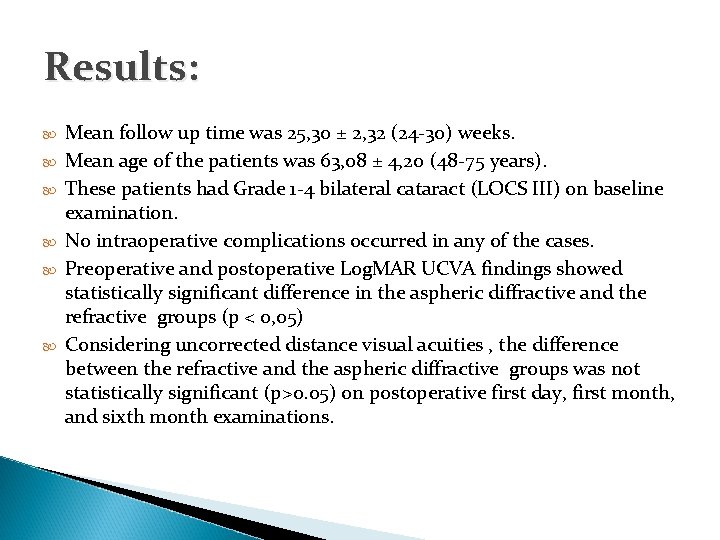
Results: Mean follow up time was 25, 30 ± 2, 32 (24 -30) weeks. Mean age of the patients was 63, 08 ± 4, 20 (48 -75 years). These patients had Grade 1 -4 bilateral cataract (LOCS III) on baseline examination. No intraoperative complications occurred in any of the cases. Preoperative and postoperative Log. MAR UCVA findings showed statistically significant difference in the aspheric diffractive and the refractive groups (p < 0, 05) Considering uncorrected distance visual acuities , the difference between the refractive and the aspheric diffractive groups was not statistically significant (p>0. 05) on postoperative first day, first month, and sixth month examinations.
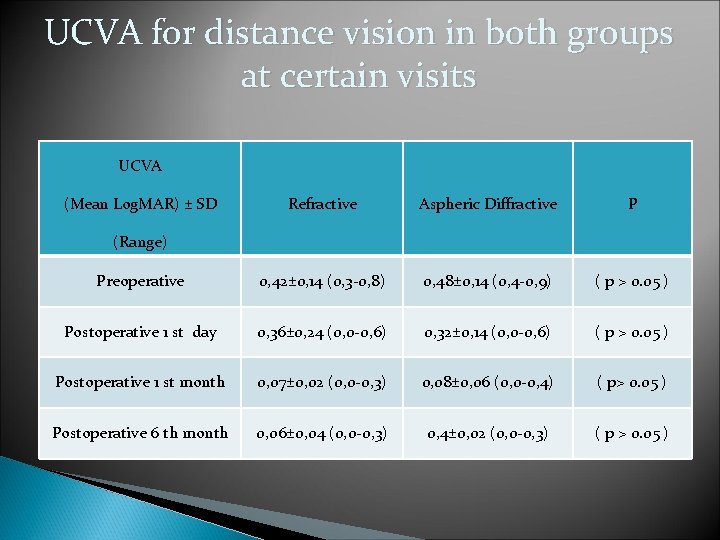
UCVA for distance vision in both groups at certain visits UCVA (Mean Log. MAR) ± SD Refractive Aspheric Diffractive P Preoperative 0, 42± 0, 14 (0, 3 -0, 8) 0, 48± 0, 14 (0, 4 -0, 9) ( p > 0. 05 ) Postoperative 1 st day 0, 36± 0, 24 (0, 0 -0, 6) 0, 32± 0, 14 (0, 0 -0, 6) ( p > 0. 05 ) Postoperative 1 st month 0, 07± 0, 02 (0, 0 -0, 3) 0, 08± 0, 06 (0, 0 -0, 4) ( p> 0. 05 ) Postoperative 6 th month 0, 06± 0, 04 (0, 0 -0, 3) 0, 4± 0, 02 (0, 0 -0, 3) ( p > 0. 05 ) (Range)
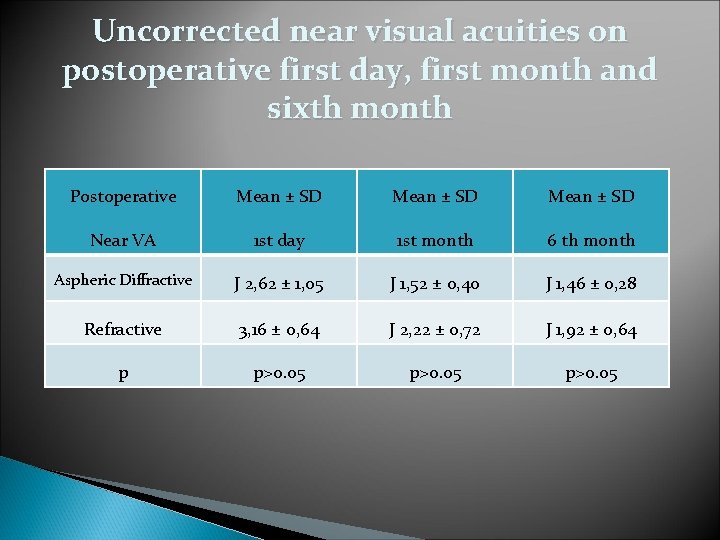
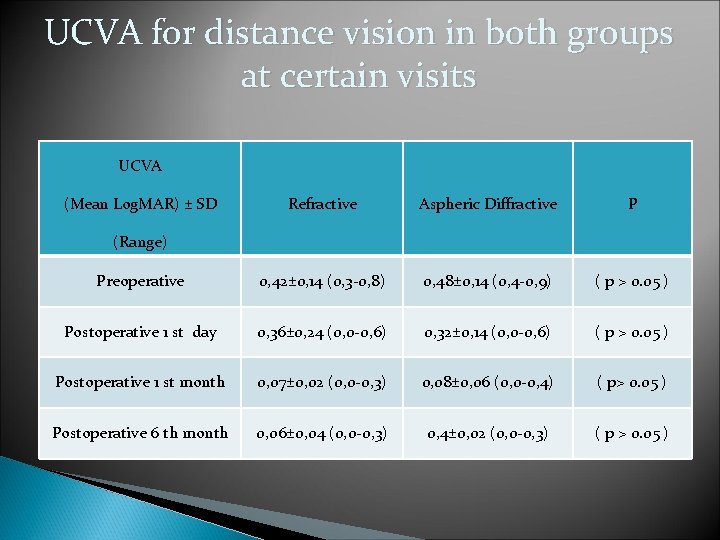
Uncorrected near visual acuities on postoperative first day, first month and sixth month Postoperative Mean ± SD Near VA 1 st day 1 st month 6 th month Aspheric Diffractive J 2, 62 ± 1, 05 J 1, 52 ± 0, 40 J 1, 46 ± 0, 28 Refractive 3, 16 ± 0, 64 J 2, 22 ± 0, 72 J 1, 92 ± 0, 64 p p>0. 05
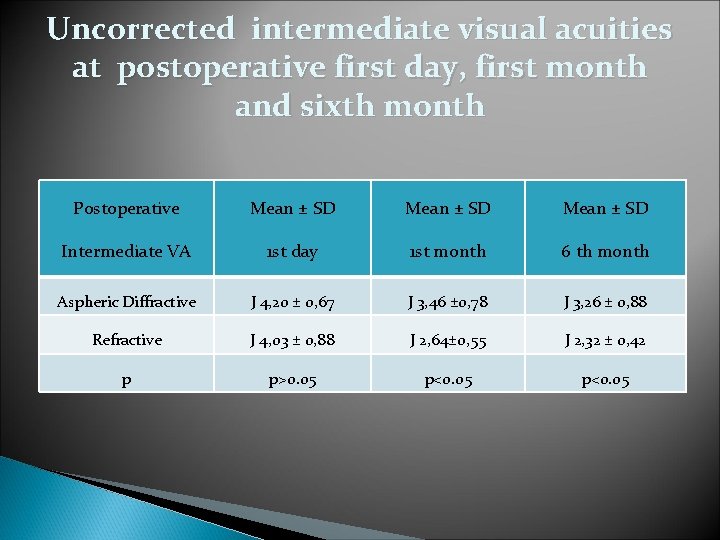
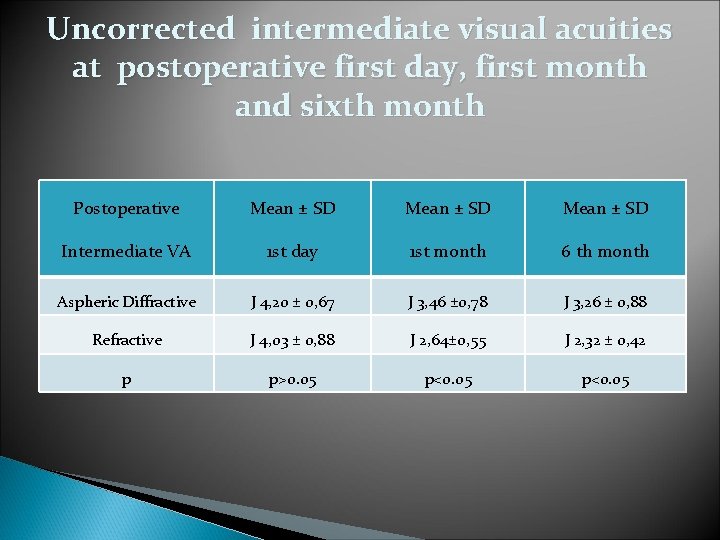
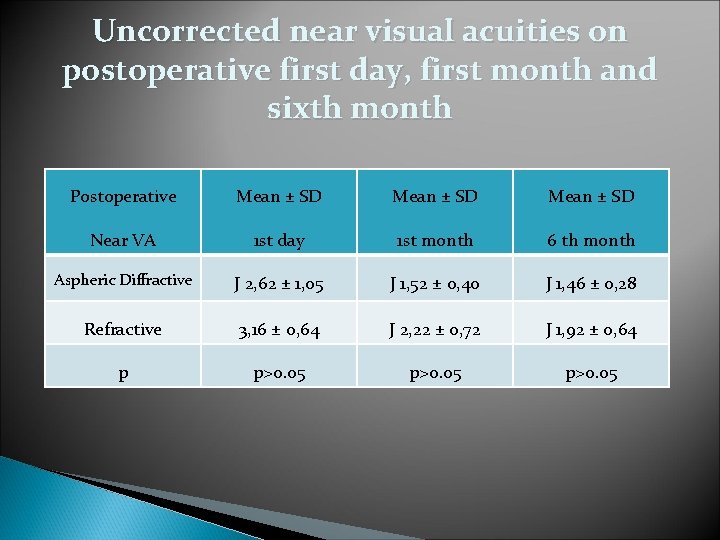
Uncorrected intermediate visual acuities at postoperative first day, first month and sixth month Postoperative Mean ± SD Intermediate VA 1 st day 1 st month 6 th month Aspheric Diffractive J 4, 20 ± 0, 67 J 3, 46 ± 0, 78 J 3, 26 ± 0, 88 Refractive J 4, 03 ± 0, 88 J 2, 64± 0, 55 J 2, 32 ± 0, 42 p p>0. 05 p<0. 05
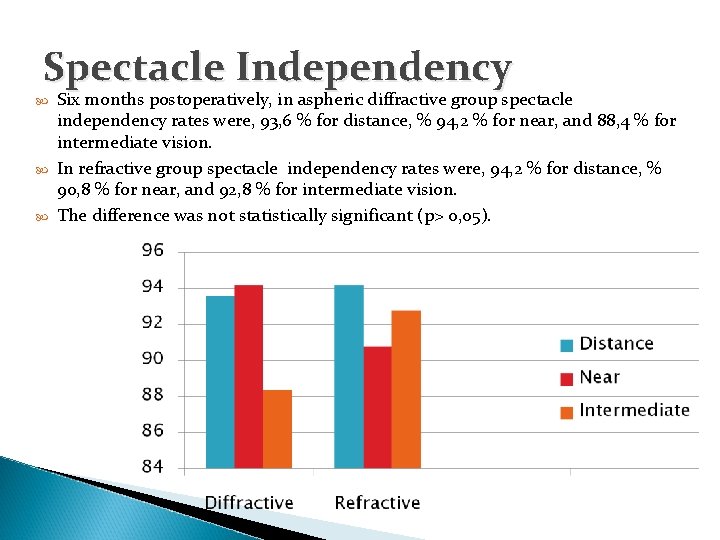
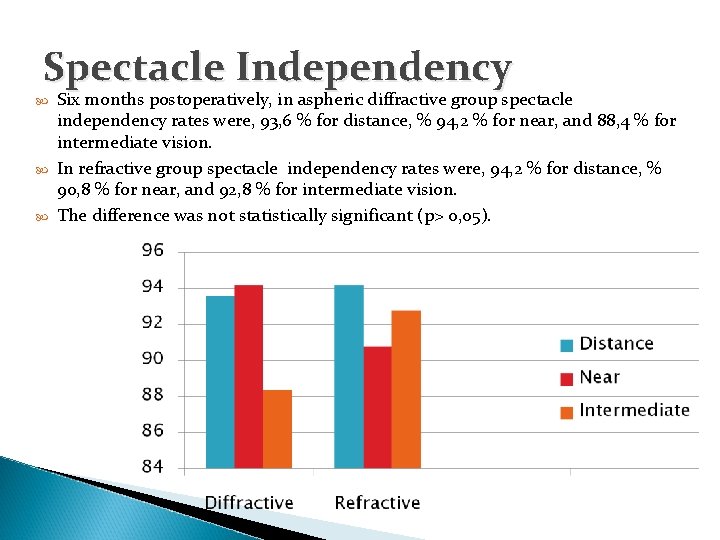
Spectacle Independency Six months postoperatively, in aspheric diffractive group spectacle independency rates were, 93, 6 % for distance, % 94, 2 % for near, and 88, 4 % for intermediate vision. In refractive group spectacle independency rates were, 94, 2 % for distance, % 90, 8 % for near, and 92, 8 % for intermediate vision. The difference was not statistically significant (p> 0, 05).
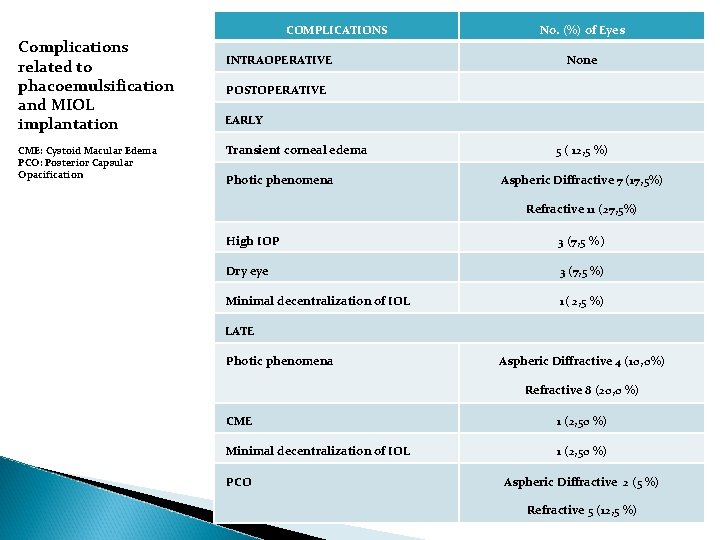
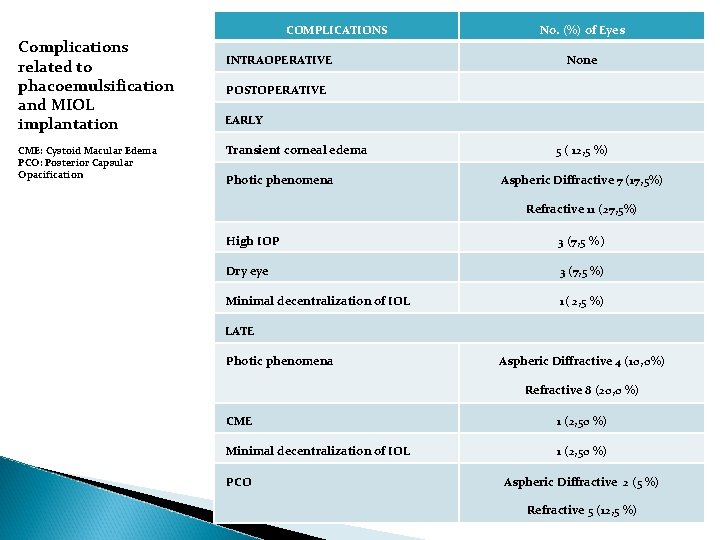
COMPLICATIONS Complications related to phacoemulsification and MIOL implantation CME: Cystoid Macular Edema PCO: Posterior Capsular Opacification INTRAOPERATIVE No. (%) of Eyes None POSTOPERATIVE EARLY Transient corneal edema Photic phenomena 5 ( 12, 5 %) Aspheric Diffractive 7 (17, 5%) Refractive 11 (27, 5%) High IOP 3 (7, 5 % ) Dry eye 3 (7, 5 %) Minimal decentralization of IOL 1( 2, 5 %) LATE Photic phenomena Aspheric Diffractive 4 (10, 0%) Refractive 8 (20, 0 %) CME 1 (2, 50 %) Minimal decentralization of IOL 1 (2, 50 %) PCO Aspheric Diffractive 2 (5 %) Refractive 5 (12, 5 %)
Conclusions: • • Our results show that; bilateral implantation of MIOLs with the same optic designs provides efficient distance vision. There is no superiority between the two groups considering uncorrected distance visual acuities. The mean uncorrected near visual acuity was better in the aspheric diffractive group. The mean uncorrected intermediate visual acuity was better in the refractive group. Photic phenomena was tolerable in both groups. Though not statistically significant, photic phenomena related disturbances were relatively less detected in the aspheric diffractive group at all visits.
Conclusions: For refractive MIOLs, if poorly tolerated by the patient, photic phenomena may even lead to the extraction of MIOLs. Especially in dim light conditions some patients may need presbyopic correction by spectacles, and patients must be warned about not driving for long hours at night. For aspheric diffractive MIOLs with + 4. 00 D add, near vision was highly satisfactory in both bright and dim light conditions. Some patients may need spectacles for intermediate vision, which might also be resolved by preoperative targeted myopia by biometry, or preferring diffractive miols with lower presbyopic addition.