Aspergillus ABPA Disease spectrum IPA Invasive pulmonary aspergillosis
Aspergillus & ABPA
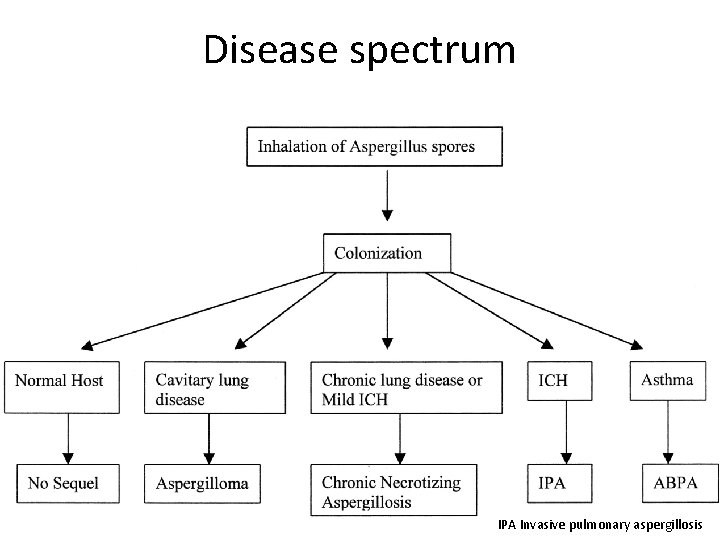
Disease spectrum IPA Invasive pulmonary aspergillosis
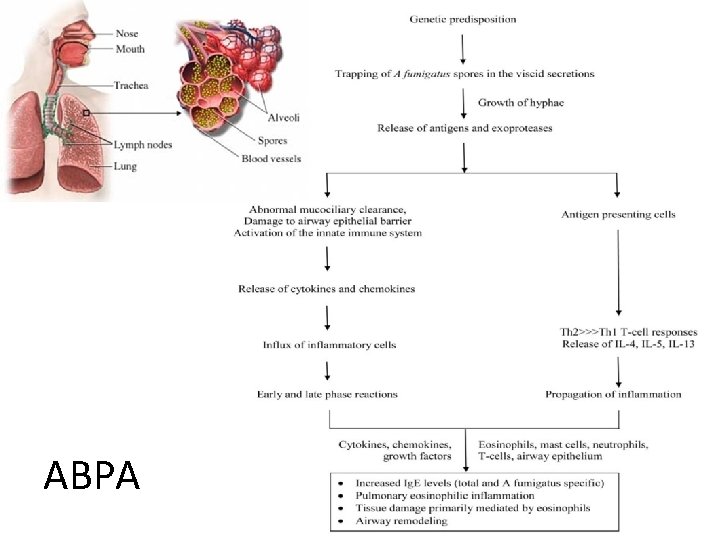
ABPA
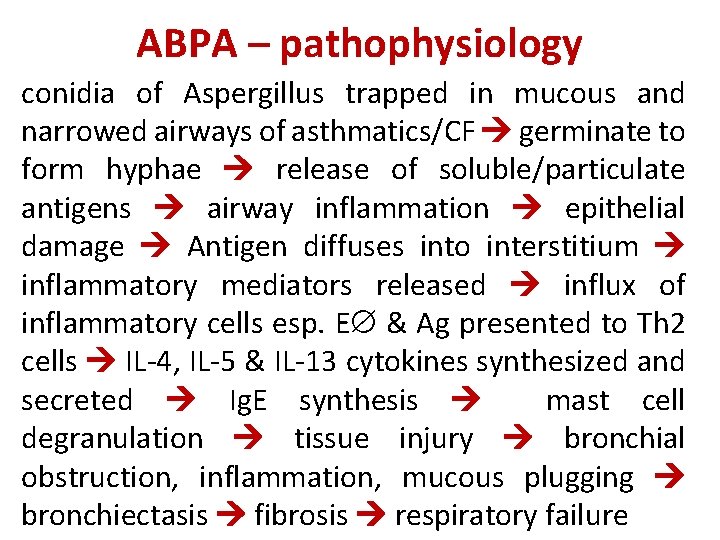
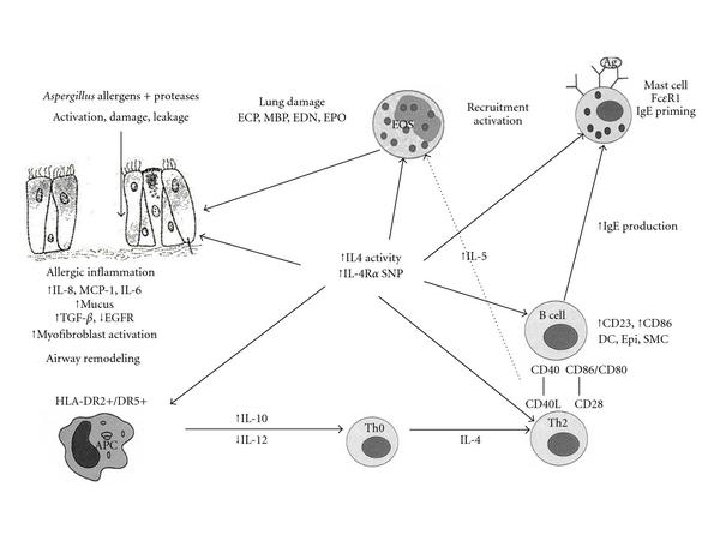
ABPA – pathophysiology conidia of Aspergillus trapped in mucous and narrowed airways of asthmatics/CF germinate to form hyphae release of soluble/particulate antigens airway inflammation epithelial damage Antigen diffuses into interstitium inflammatory mediators released influx of inflammatory cells esp. E & Ag presented to Th 2 cells IL-4, IL-5 & IL-13 cytokines synthesized and secreted Ig. E synthesis mast cell degranulation tissue injury bronchial obstruction, inflammation, mucous plugging bronchiectasis fibrosis respiratory failure
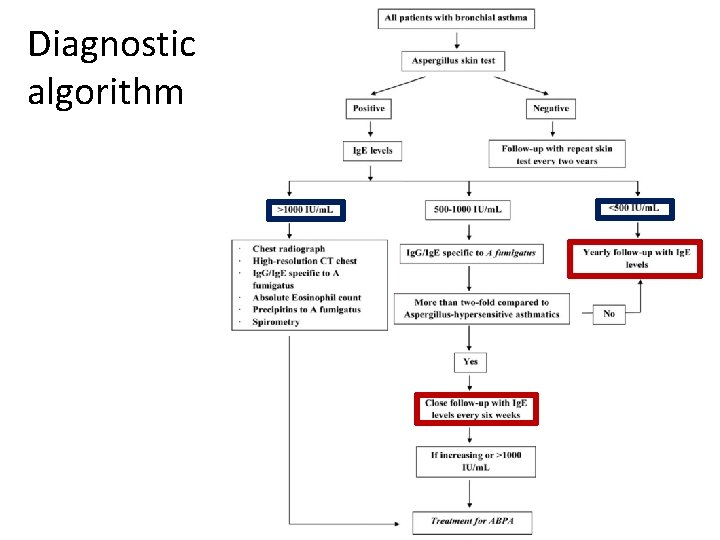
Diagnostic algorithm
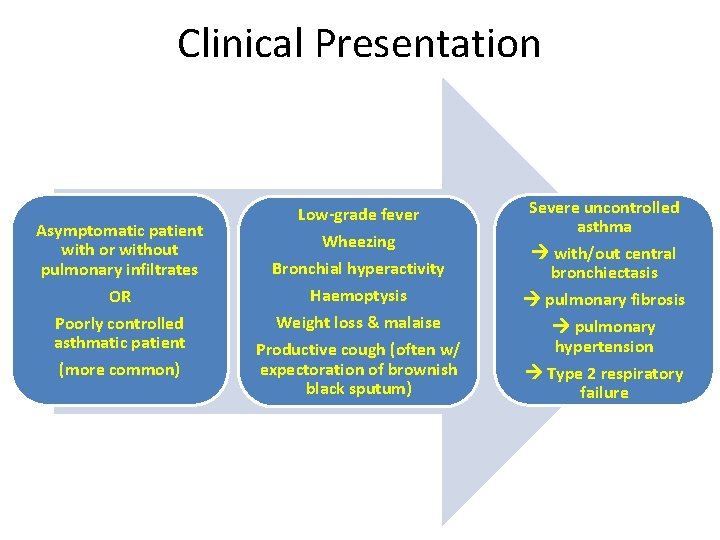
Clinical Presentation Asymptomatic patient with or without pulmonary infiltrates OR Poorly controlled asthmatic patient (more common) Low-grade fever Wheezing Bronchial hyperactivity Haemoptysis Weight loss & malaise Productive cough (often w/ expectoration of brownish black sputum) Severe uncontrolled asthma with/out central bronchiectasis pulmonary fibrosis pulmonary hypertension Type 2 respiratory failure
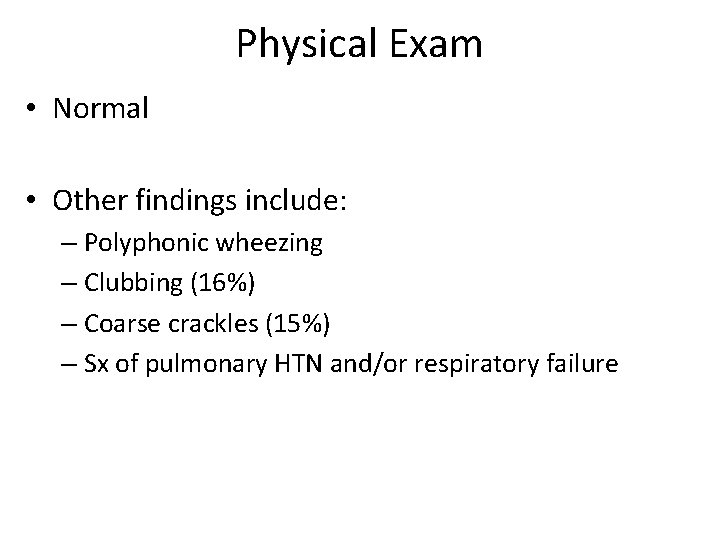
Physical Exam • Normal • Other findings include: – Polyphonic wheezing – Clubbing (16%) – Coarse crackles (15%) – Sx of pulmonary HTN and/or respiratory failure
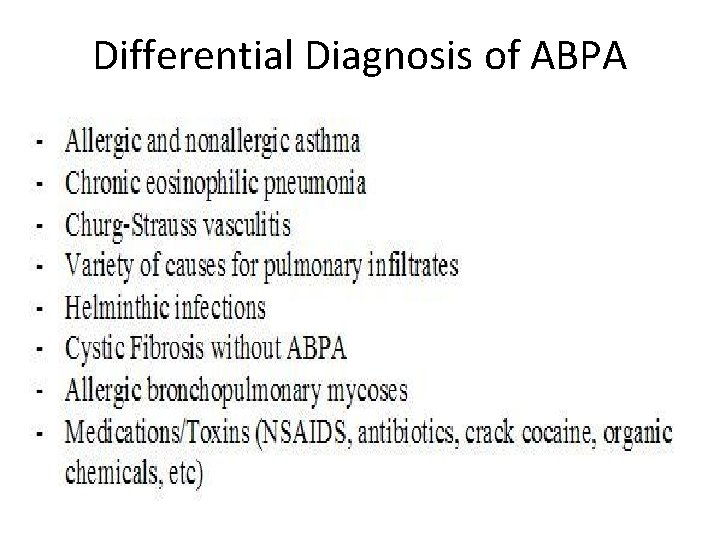
Differential Diagnosis of ABPA
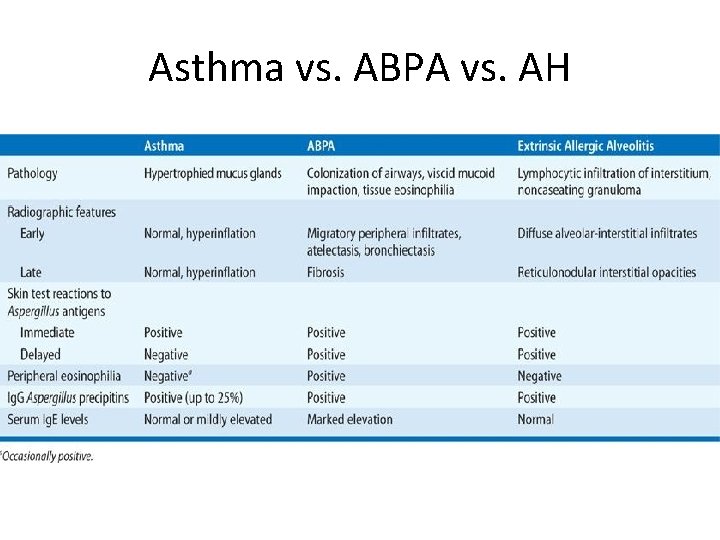
Asthma vs. ABPA vs. AH
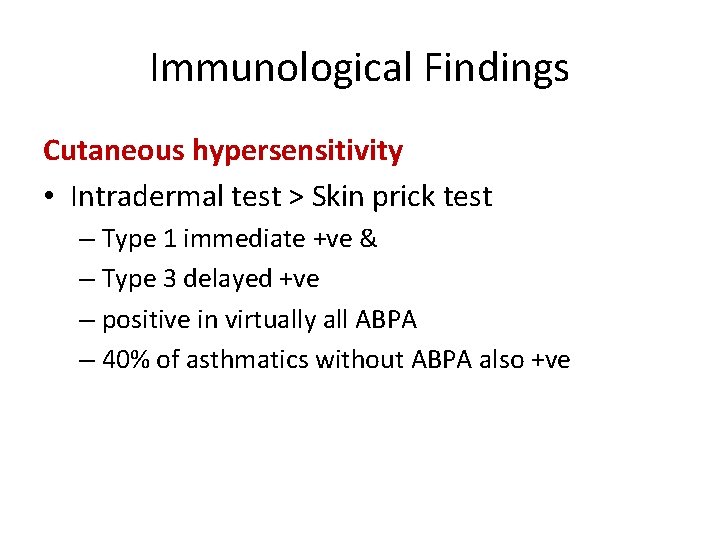
Immunological Findings Cutaneous hypersensitivity • Intradermal test > Skin prick test – Type 1 immediate +ve & – Type 3 delayed +ve – positive in virtually all ABPA – 40% of asthmatics without ABPA also +ve
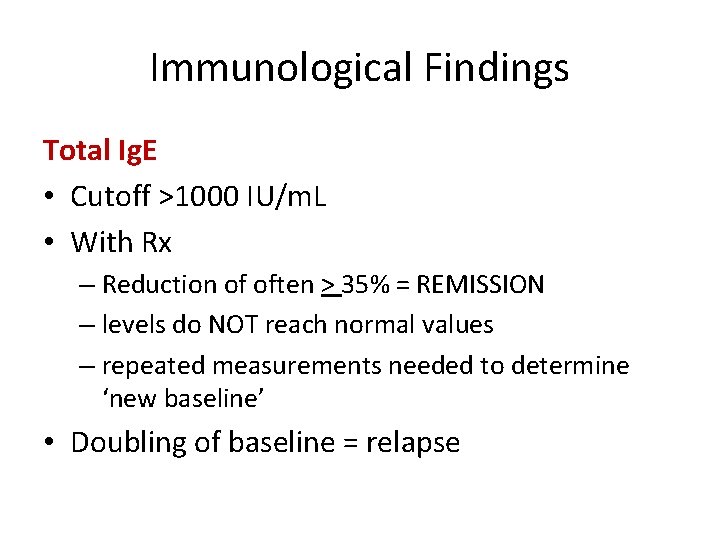
Immunological Findings Total Ig. E • Cutoff >1000 IU/m. L • With Rx – Reduction of often > 35% = REMISSION – levels do NOT reach normal values – repeated measurements needed to determine ‘new baseline’ • Doubling of baseline = relapse
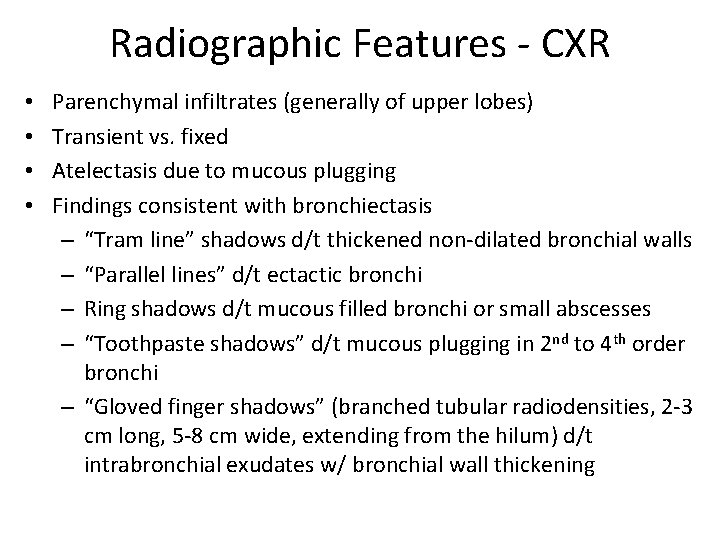
Radiographic Features - CXR • • Parenchymal infiltrates (generally of upper lobes) Transient vs. fixed Atelectasis due to mucous plugging Findings consistent with bronchiectasis – “Tram line” shadows d/t thickened non-dilated bronchial walls – “Parallel lines” d/t ectactic bronchi – Ring shadows d/t mucous filled bronchi or small abscesses – “Toothpaste shadows” d/t mucous plugging in 2 nd to 4 th order bronchi – “Gloved finger shadows” (branched tubular radiodensities, 2 -3 cm long, 5 -8 cm wide, extending from the hilum) d/t intrabronchial exudates w/ bronchial wall thickening
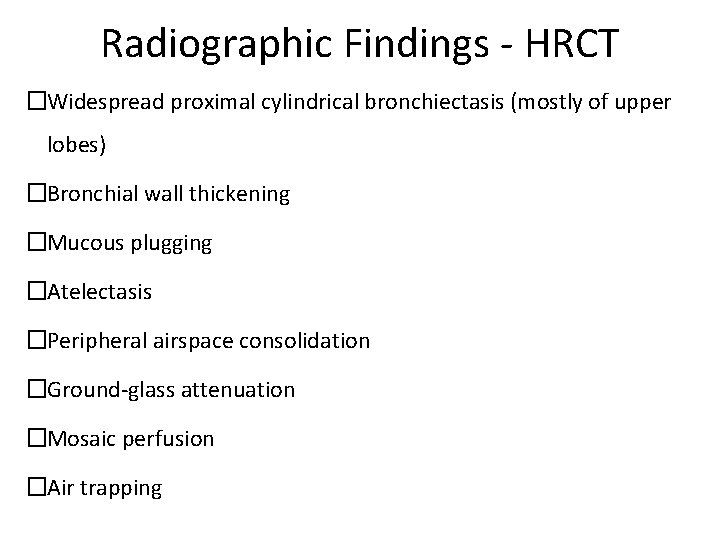
Radiographic Findings - HRCT �Widespread proximal cylindrical bronchiectasis (mostly of upper lobes) �Bronchial wall thickening �Mucous plugging �Atelectasis �Peripheral airspace consolidation �Ground-glass attenuation �Mosaic perfusion �Air trapping
Diagnosis of ABPA
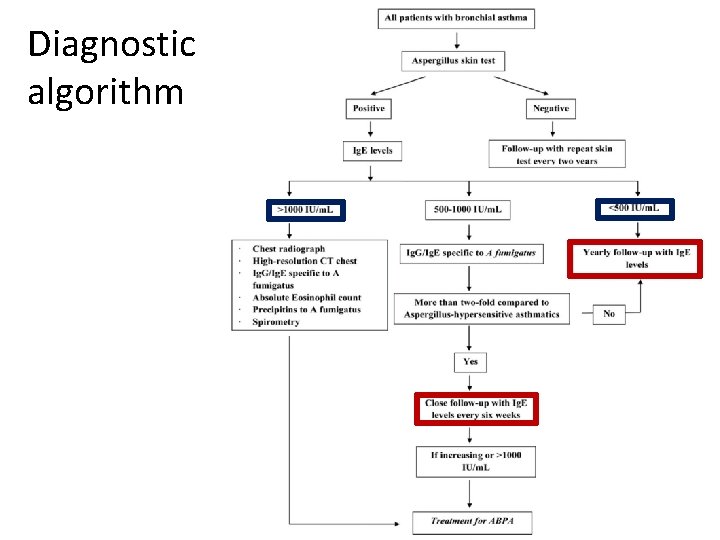
Diagnostic algorithm
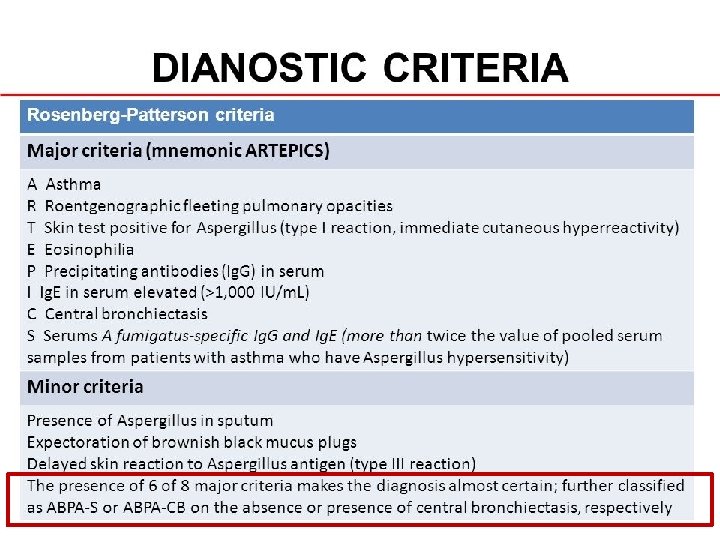
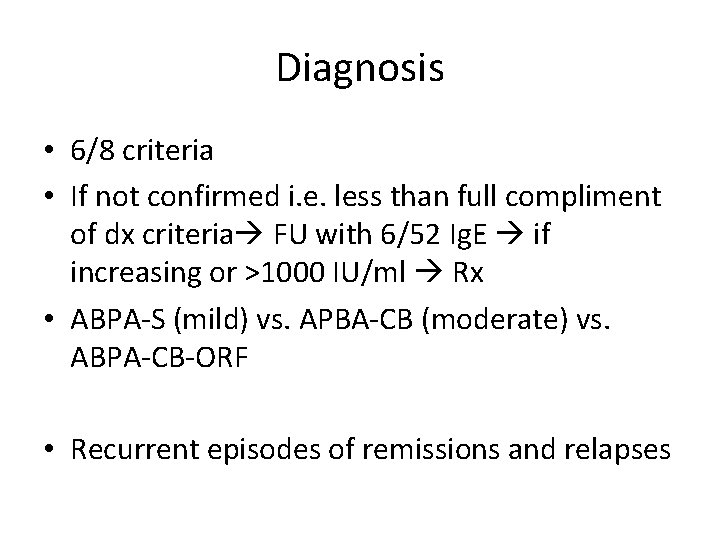
Diagnosis • 6/8 criteria • If not confirmed i. e. less than full compliment of dx criteria FU with 6/52 Ig. E if increasing or >1000 IU/ml Rx • ABPA-S (mild) vs. APBA-CB (moderate) vs. ABPA-CB-ORF • Recurrent episodes of remissions and relapses
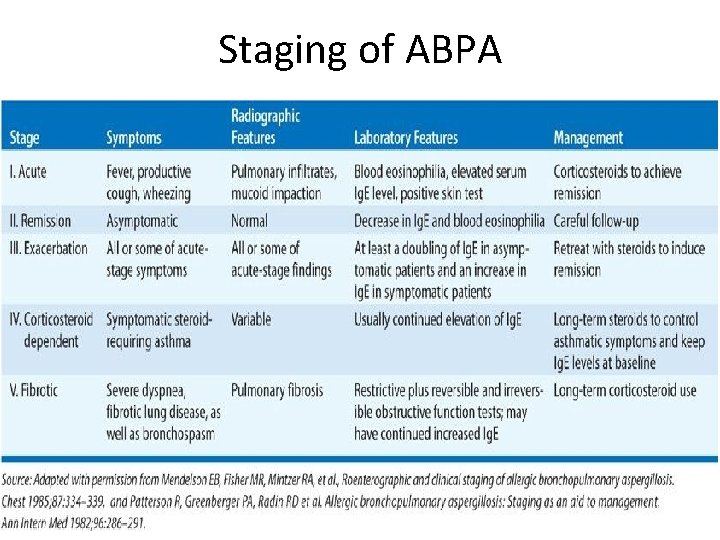
Staging of ABPA
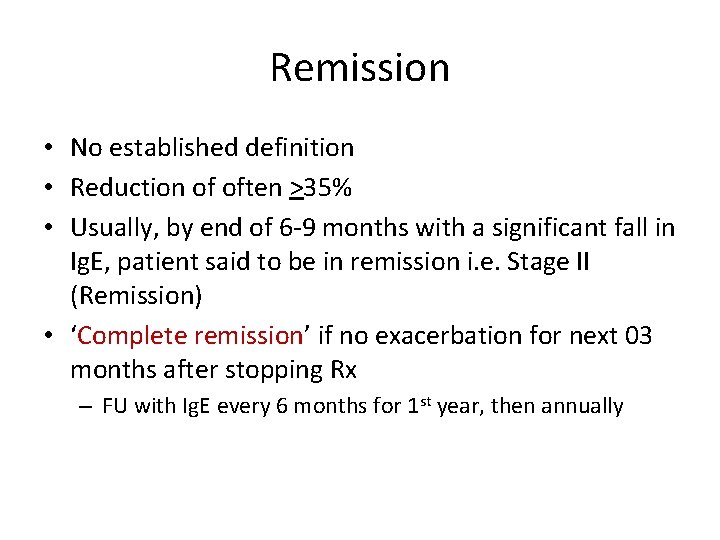
Remission • No established definition • Reduction of often >35% • Usually, by end of 6 -9 months with a significant fall in Ig. E, patient said to be in remission i. e. Stage II (Remission) • ‘Complete remission’ if no exacerbation for next 03 months after stopping Rx – FU with Ig. E every 6 months for 1 st year, then annually
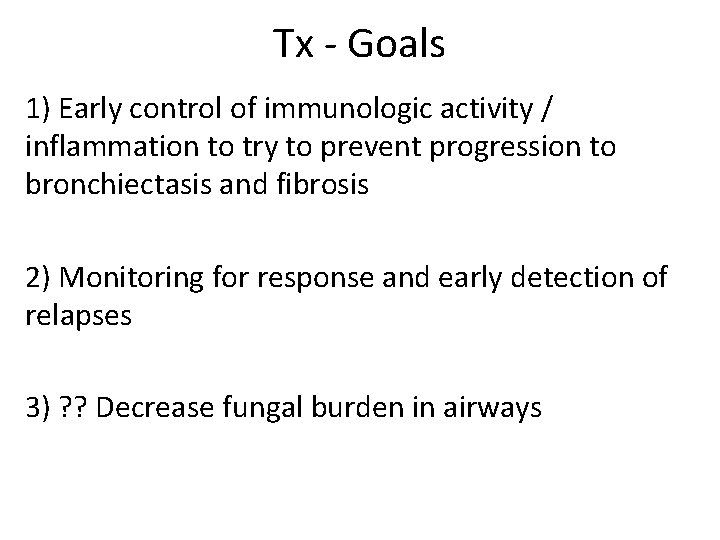
Tx - Goals 1) Early control of immunologic activity / inflammation to try to prevent progression to bronchiectasis and fibrosis 2) Monitoring for response and early detection of relapses 3) ? ? Decrease fungal burden in airways
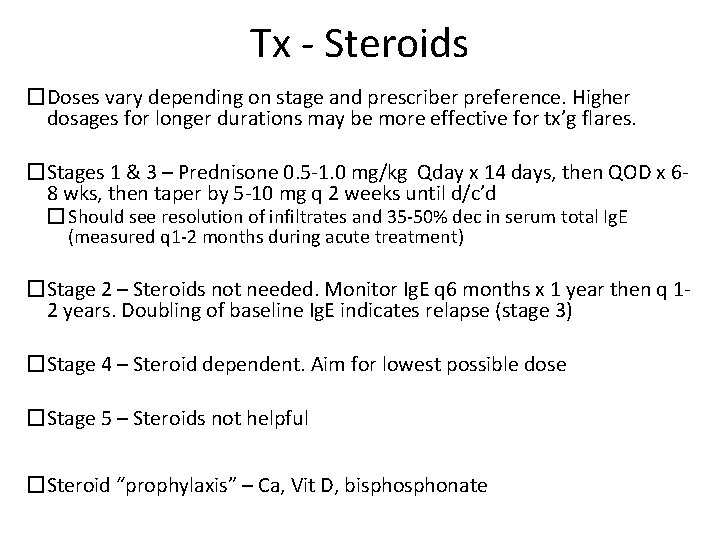
Tx - Steroids �Doses vary depending on stage and prescriber preference. Higher dosages for longer durations may be more effective for tx’g flares. �Stages 1 & 3 – Prednisone 0. 5 -1. 0 mg/kg Qday x 14 days, then QOD x 68 wks, then taper by 5 -10 mg q 2 weeks until d/c’d � Should see resolution of infiltrates and 35 -50% dec in serum total Ig. E (measured q 1 -2 months during acute treatment) �Stage 2 – Steroids not needed. Monitor Ig. E q 6 months x 1 year then q 12 years. Doubling of baseline Ig. E indicates relapse (stage 3) �Stage 4 – Steroid dependent. Aim for lowest possible dose �Stage 5 – Steroids not helpful �Steroid “prophylaxis” – Ca, Vit D, bisphonate
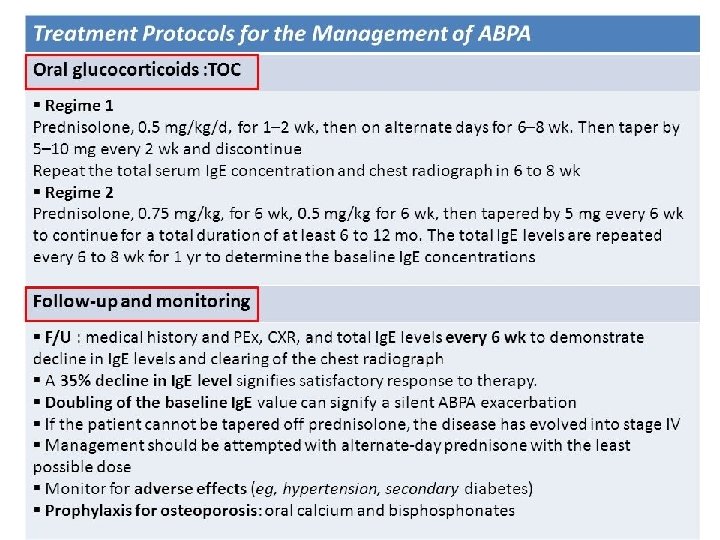
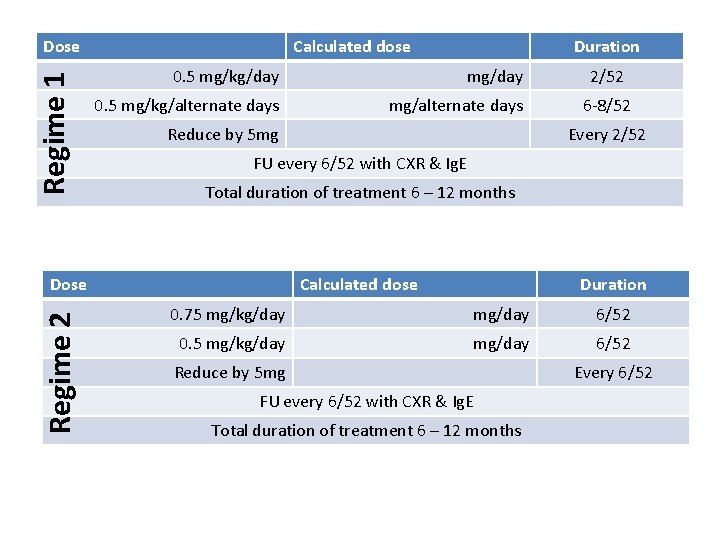
Regime 1 Dose Calculated dose 0. 5 mg/kg/day mg/day 0. 5 mg/kg/alternate days mg/alternate days Reduce by 5 mg 2/52 6 -8/52 Every 2/52 FU every 6/52 with CXR & Ig. E Total duration of treatment 6 – 12 months Dose Regime 2 Duration Calculated dose Duration 0. 75 mg/kg/day mg/day 6/52 0. 5 mg/kg/day mg/day 6/52 Reduce by 5 mg FU every 6/52 with CXR & Ig. E Total duration of treatment 6 – 12 months Every 6/52
Total Ig. E levels Date Description Load IU/ml IU/ml IU/ml
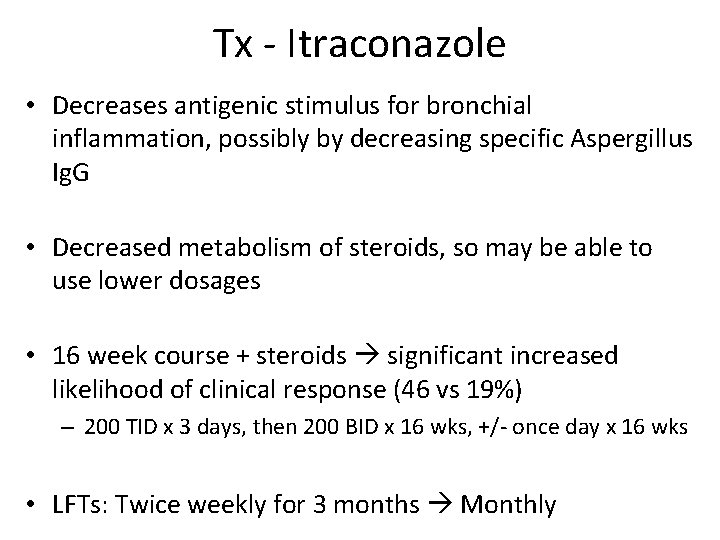
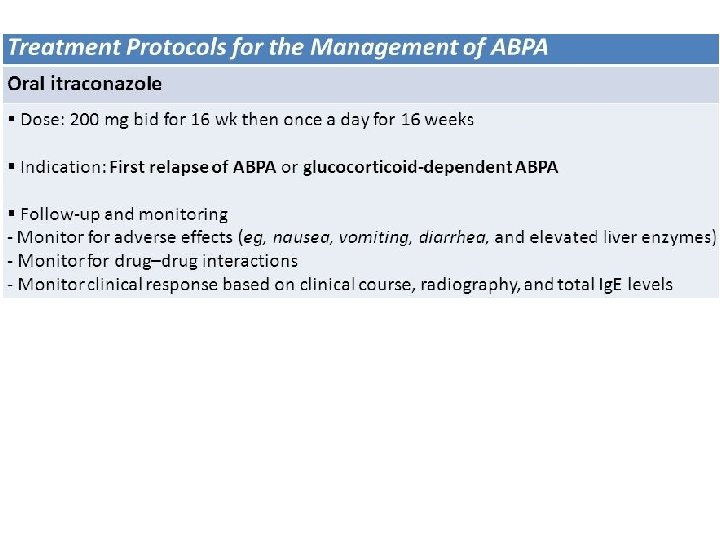
Tx - Itraconazole • Decreases antigenic stimulus for bronchial inflammation, possibly by decreasing specific Aspergillus Ig. G • Decreased metabolism of steroids, so may be able to use lower dosages • 16 week course + steroids significant increased likelihood of clinical response (46 vs 19%) – 200 TID x 3 days, then 200 BID x 16 wks, +/- once day x 16 wks • LFTs: Twice weekly for 3 months Monthly
Miscellaneous
SAM The presence of concomitant allergic fungal sinusitis (AFS) and allergic bronchopulmonary mycosis in the same patient represents an expression of the same process of fungal hypersensitivity in the upper and lower airways. SAM syndrome: an acronym for sinobronchial allergic mycosis
Diagnostic Criteria • • chronic sinusitis involving multiple sinuses asthma total serum Ig. E levels are usually elevated as well immediate cutaneous reactivity to fungal allergens peripheral eosinophilia radiographic evidence of bronchiectasis. variety of chest radiographic abnormalities may occur: ranging from mass lesions to diffuse pulmonary infiltrates and even normal findings on chest radiographs.
- Slides: 30