Ashermans syndrome DICK SCHOOT MD PHD CATHARINA HOSPITAL






- Slides: 19
Asherman’s syndrome DICK SCHOOT MD PHD CATHARINA HOSPITAL EINDHOVEN THE NETHERLANDS
Primaire preventie Secundaire preventie Behandeling adhaesies
cause of adhaesions Curettage Genetic predisposition Placental characteristics
Primaire preventie Chemische abortus inductie Mefigyn cytotec

Primaire preventie door adequate curettage

placental remnants
remnant placental or trophoblastic tissue often leads to infection repeated curettage intrauterine adhaesions (Asherman’s syndrome)
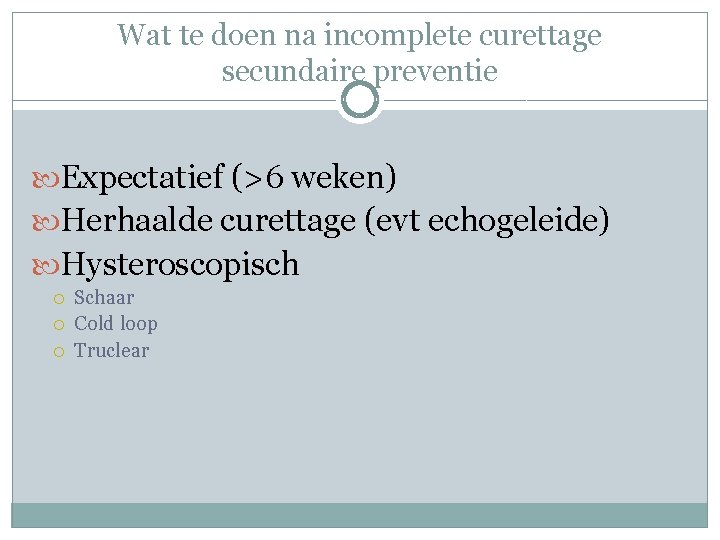
Wat te doen na incomplete curettage secundaire preventie Expectatief (>6 weken) Herhaalde curettage (evt echogeleide) Hysteroscopisch Schaar Cold loop Truclear

prevalence of adhaesions after secondary or repeated curettage 35% Golan 1996 50% Westendorp 1998

patients and procedure n = 55 (Jan 2005 -Jan 2008) mean age 34 (21 -40) previous curettage = 20 (first trimester and puerperal) manual placenta removal = 35 median interval first proc. and morc. 8 wks (2 -40) hysteroscopic morcellation (TRUCLEAR Smith&Nephew) saline distension (max. 120 mm Hg) antibiotic prophylaxis
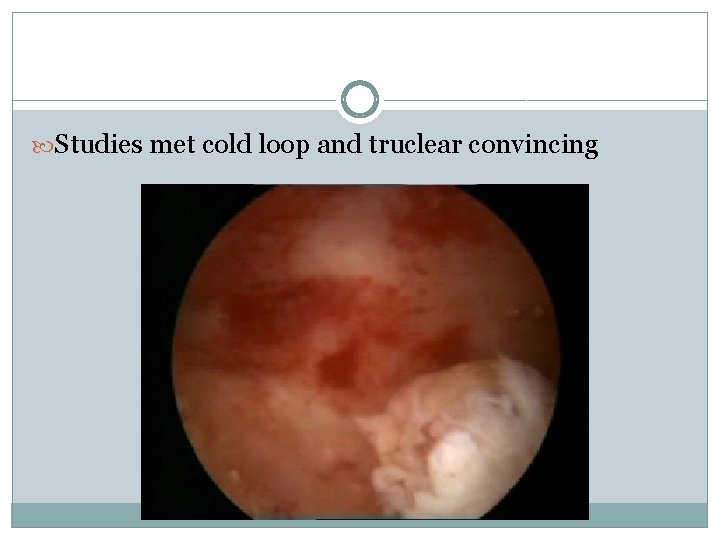
Studies met cold loop and truclear convincing
conclusion the prevalence of intrauterine synechiae is high (35 -50%) after secondary or repeated curettage of placental remnants hysteroscopic morcellation reduces the risk of these synechiae (5. 5%)
If prevention failed: Synechiae

cause of adhaesions in most cases only a single uncomplicated pregnancy related intra-uterine procedure first trimester curettage puerperal curettage manual placenta removal always pregnancy related never spontaneous difficult to mimmick in ‘disfunctional bleeders’
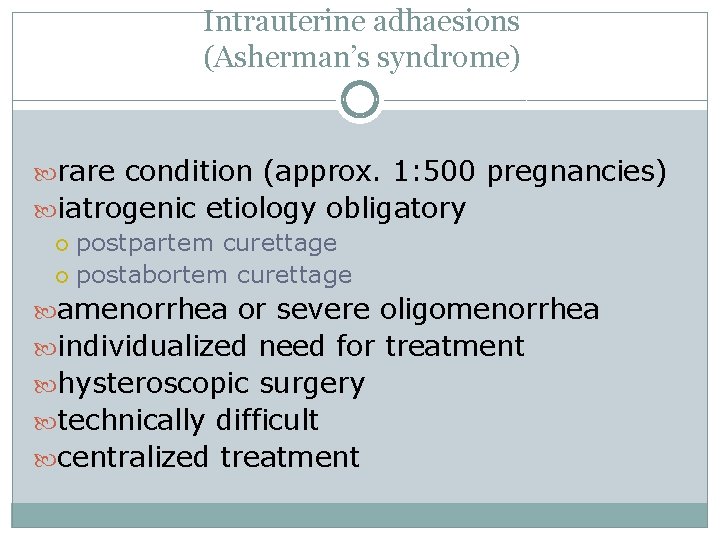
Intrauterine adhaesions (Asherman’s syndrome) rare condition (approx. 1: 500 pregnancies) iatrogenic etiology obligatory postpartem curettage postabortem curettage amenorrhea or severe oligomenorrhea individualized need for treatment hysteroscopic surgery technically difficult centralized treatment
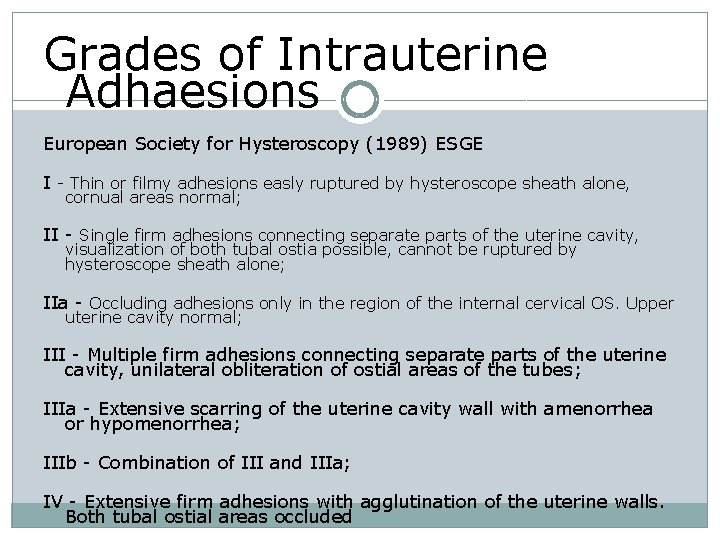
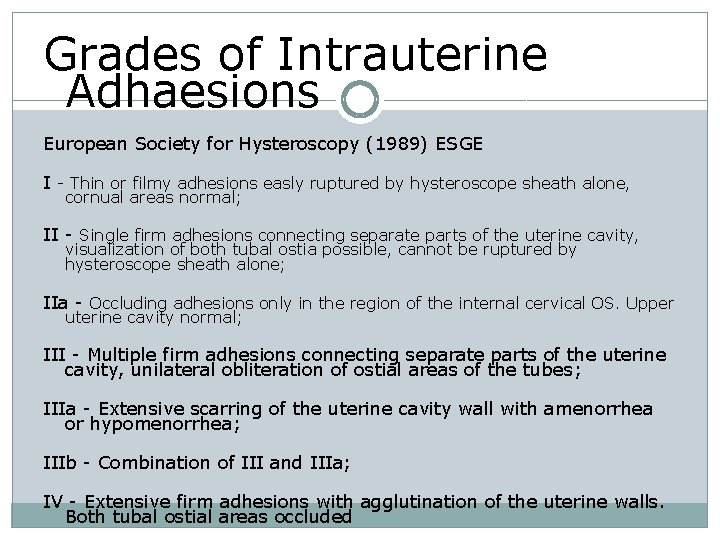
Grades of Intrauterine Adhaesions European Society for Hysteroscopy (1989) ESGE I - Thin or filmy adhesions easly ruptured by hysteroscope sheath alone, cornual areas normal; II - Single firm adhesions connecting separate parts of the uterine cavity, visualization of both tubal ostia possible, cannot be ruptured by hysteroscope sheath alone; IIa - Occluding adhesions only in the region of the internal cervical OS. Upper uterine cavity normal; III - Multiple firm adhesions connecting separate parts of the uterine cavity, unilateral obliteration of ostial areas of the tubes; IIIa - Extensive scarring of the uterine cavity wall with amenorrhea or hypomenorrhea; IIIb - Combination of III and IIIa; IV - Extensive firm adhesions with agglutination of the uterine walls. Both tubal ostial areas occluded
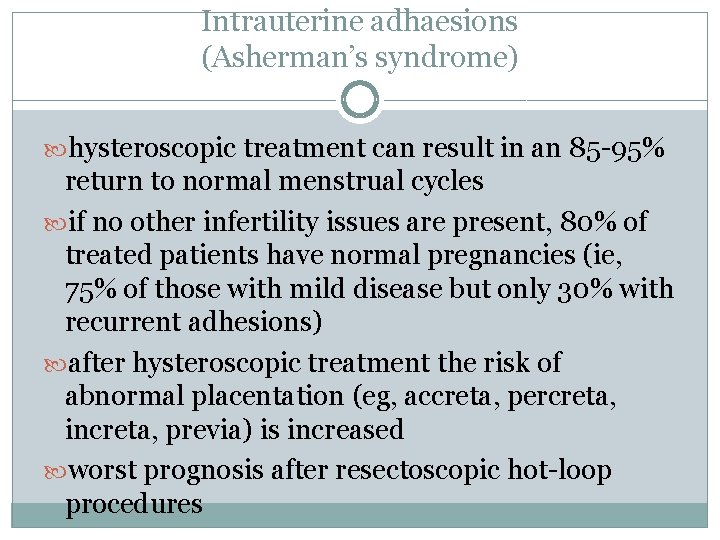
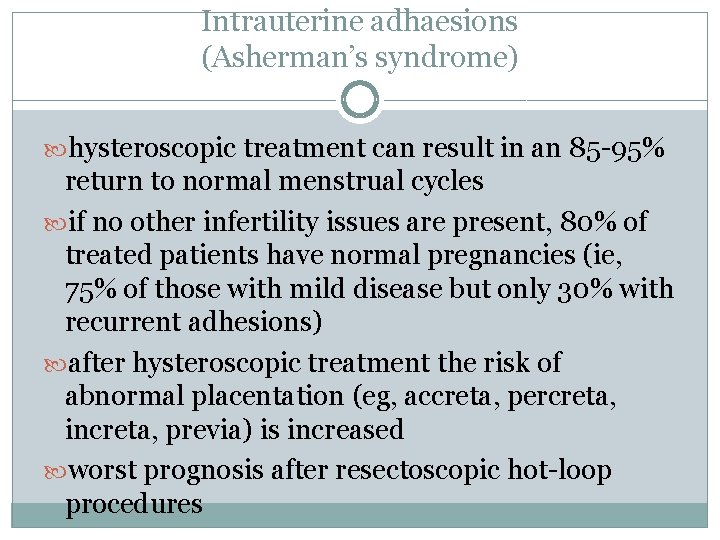
Intrauterine adhaesions (Asherman’s syndrome) hysteroscopic treatment can result in an 85 -95% return to normal menstrual cycles if no other infertility issues are present, 80% of treated patients have normal pregnancies (ie, 75% of those with mild disease but only 30% with recurrent adhesions) after hysteroscopic treatment the risk of abnormal placentation (eg, accreta, percreta, increta, previa) is increased worst prognosis after resectoscopic hot-loop procedures
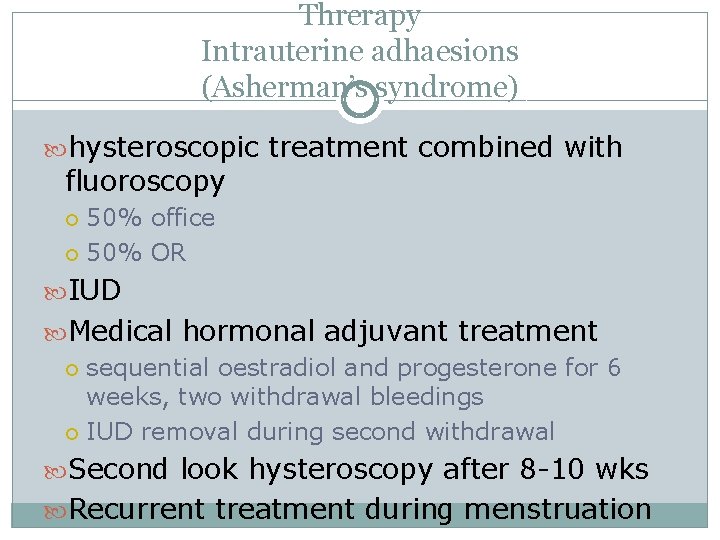
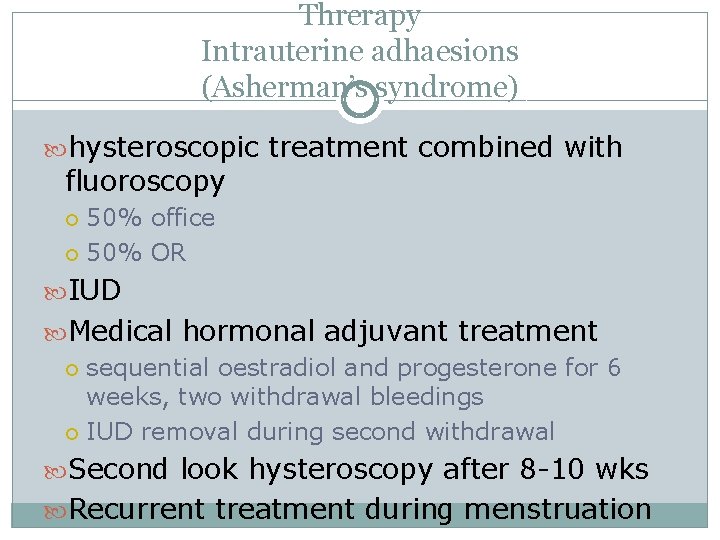
Threrapy Intrauterine adhaesions (Asherman’s syndrome) hysteroscopic treatment combined with fluoroscopy 50% office 50% OR IUD Medical hormonal adjuvant treatment sequential oestradiol and progesterone for 6 weeks, two withdrawal bleedings IUD removal during second withdrawal Second look hysteroscopy after 8 -10 wks Recurrent treatment during menstruation

 Robert stevenson director
Robert stevenson director Catharina glaas
Catharina glaas Catharina glaas
Catharina glaas Catharina glaas
Catharina glaas Catharina jerratsch
Catharina jerratsch Jorden i genomskärning
Jorden i genomskärning Jan vermeer catharina bolnes
Jan vermeer catharina bolnes Catharina glaas
Catharina glaas Jmp
Jmp Define hospital
Define hospital Jpsm courses
Jpsm courses Ing marek pavlik phd
Ing marek pavlik phd Maura l. gillison, md, phd
Maura l. gillison, md, phd Department of anthropology
Department of anthropology Van deemter pronunciation
Van deemter pronunciation Ted lai md
Ted lai md Simba cheated acronym
Simba cheated acronym Name of ph
Name of ph Lisa brenner phd
Lisa brenner phd Craig watson md phd
Craig watson md phd