ASEPTIC TECHNIQUE Surgical Conscience An inner commitment to

- Slides: 34
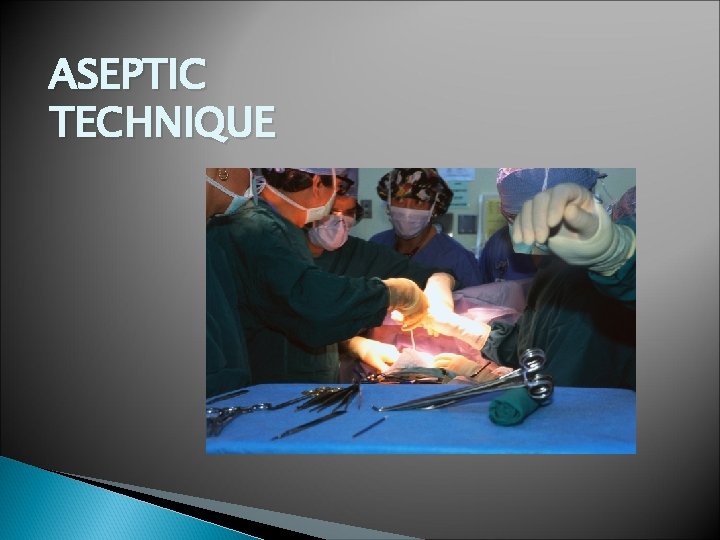
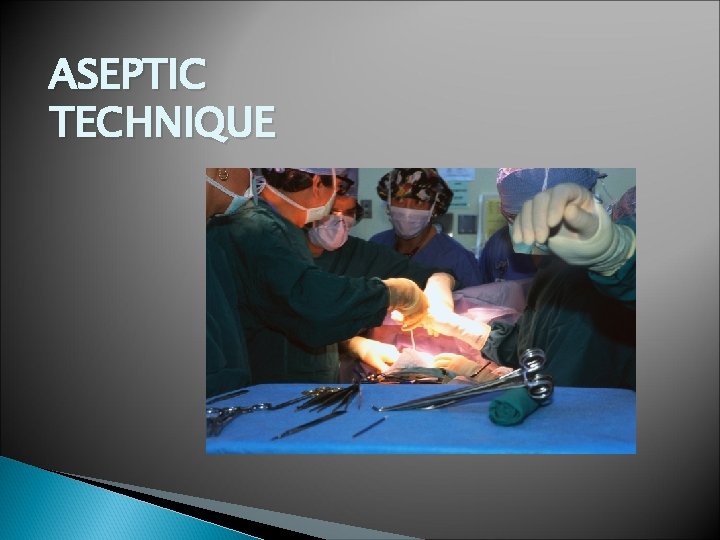
ASEPTIC TECHNIQUE
Surgical Conscience An inner commitment to strictly adhere to aseptic practice, report any break in technique, and correct any violation, whether or not anyone is present and views the incident. A surgical conscious mandates commitment to aseptic practices at all times.
Aseptic Technique Definitions: ◦ Asepsis-is the absence of infectious organisms. ◦ Aseptic Technique-restricts microorganisms in the environment (on equipment, supplies etc) ◦ The goal is to optimize primary wound healing, prevent infection and minimize length of recovery. ◦ Perioperative surgical asepsis is the foundation for infection control efforts in the perioperative setting. Microsoft Clipart
Creating and Maintaining a Sterile Field RN is responsible for: ◦ Understanding infection sources, modes and transmission. ◦ Methods for reducing/eliminating microorganisms. ◦ Knowledge of scrubbing, gowning, gloving, prepping, draping, maintaining a sterile field and operating room sanitation practices.
Responsibility All members of the team share responsibility for maintaining and creating a sterile field. Asepsis is dependent on the sterile conscience of the personnel using sterile technique. Perioperative nurse (RN) assumes major responsibility. Continuously monitor the surgical environment for sources of infection: ◦ Endogenous (The patient is the source of infection) ◦ Exogenous (Infections are caused by personnel, environment, and equipment. )
Understanding of infection sources, modes and transmission Endogenous ◦ ◦ ◦ ◦ Skin Length of Surgery Neonate and Geriatric Patients Nutritional Status Impaired Defense Mechanisms Pre-existing Infection Smoking
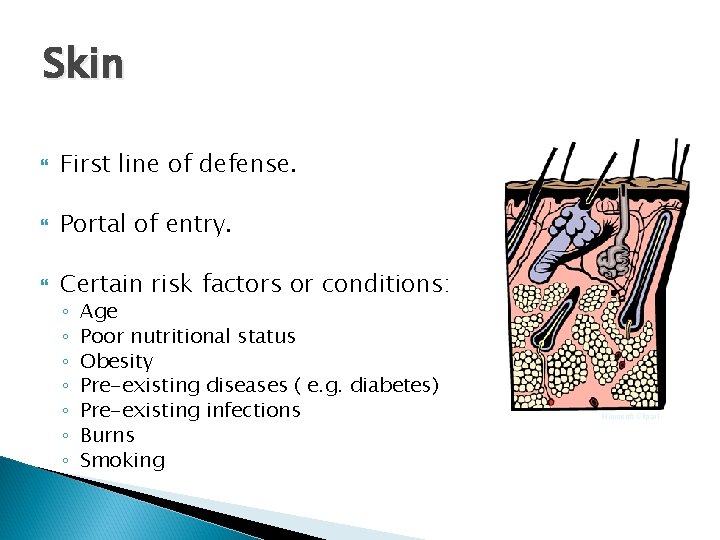
Skin First line of defense. Portal of entry. Certain risk factors or conditions: ◦ ◦ ◦ ◦ Age Poor nutritional status Obesity Pre-existing diseases ( e. g. diabetes) Pre-existing infections Burns Smoking Microsoft Clipart
Length of Stay Type of procedure. Surgical technique. Extended hospital stays. Colonization of the patient if hospitalized prior to surgery, or if patient has had extensive previous stays. Microsoft Clipart
Neonate and Geriatric Patients Neonate: ◦ Increased susceptibility from immature globulin synthesis. ◦ Decreased antibody production. ◦ Weight. Geriatric: ◦ Inadequate circulation (atherosclerosis). ◦ Presence of co-existing disease.
Nutritional Status Drug and alcohol abuse. Unbalanced meals. Decrease in protein intake. Increase in sodium intake. Patients who are diabetic, or on special diets who have not followed the recommended diet regimenare at greater risk because their nutritional status is often inadequate.
Impaired Defense Mechanisms Chemotherapy • Diabetes Radiation Therapy • Cardiac Disease Cancer • Respiratory Disease
Pre-existing Infection Significantly increases risk for infection. Surgery should be postponed if a pre-existing infection is found. Microsoft Clipart
Smoking Decreases delivery of oxygen to tissues. Delays wound healing. Microsoft Clipart
Exogenous Sources of Infection Personnel Environment Equipment Microsoft Clipart
Personnel Major source of microorganisms. Increased number of staff in the room means greater risk for infection. Skin of all persons in the OR. Cells and surface organisms are being shed from skin surfaces. Talking, coughing, and breathing, release microorganisms into the OR environment. Jewelry, artificial nails, cracks in nail polish. When hands with artificial nails were cultured, the number of organisms were increased, especially gram-negative bacteria.

Environment OR Environment—Not Sterile: ◦ Walls ◦ Floors ◦ Lights and Light Tracks ◦ Cabinets ◦ Stationary Equipment
Equipment All supplies, instruments and equipment are potential sources of infection, as these all come in contact with air and OR personnel; therefore, microorganisms can be transferred to these objects when they are touched. Dust particles settle on equipment, instruments, and supplies; particles are deposited on these items and all become sources of infection.
Standard and Transmission-Based Precautions Used to protect worker exposure. PPE (Personal Protective Equipment). Transmission-based Precautions: ◦ Airborne-TB, varicella, and rubeola that are transmitted via the air. ◦ Droplet-influenza, and mumps are transmitted through droplets. ◦ Contact Precautions-pathogens that are transmitted through direct or indirect contact. ◦-
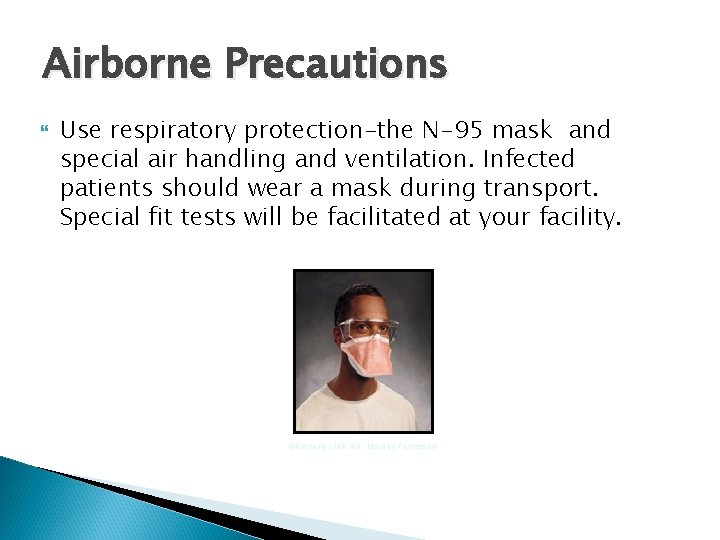
Airborne Precautions Use respiratory protection-the N-95 mask and special air handling and ventilation. Infected patients should wear a mask during transport. Special fit tests will be facilitated at your facility. ©Kimberly Clark Inc. , Used by Permission
Droplet Precautions Wear a mask if within three feet of the infected patient. Position other patients at least three feet from the infected patients. Infected patients should wear a mask during transport.
Contact Precautions Use gloves and gowns. Clean and disinfect patient equipment with facilityappropriate disinfecting agent. Microsoft Clipart
Universal Precautions Designed by CDC in 1987. Precautions taken to prevent transmission of HIV, Hepatitis B (HBV) and other blood borne pathogens. Incorporated into the Standard and Transmission. Based Precautions (OR Personnel tend to be more familiar with the term Universal Precautions). All patients are treated the same, as if they are potentially infected. Standard basic precautions are used on everyone.
AORN Recommended Practices for Standard and Transmission-Based Precautions in the Perioperative Practice Setting Recommended Practice I: ◦ “Standard precautions to prevent pathogen transmission should be used during all invasive procedures. ”
AORN Recommended Practices Recommended Practice II: ◦ “Standard precautions should include use of protective barriers and prompt and frequent hand washing to reduce the risk of exposure to potentially infectious materials. ”
AORN Recommended Practices Recommended Practice IV: ◦ “Personnel should handle specimens as potentially infectious material. ” Recommended Practice V: ◦ “Work practices should be designed to minimize risk of occupational exposure to bloodborne and other potentially infectious pathogens. ”
AORN Recommended Practices Recommended Practice VI: ◦ “Personnel who have exudative lesions or weeping dermatitis should refrain from providing direct patient care or handling medical devices used in performing invasive procedures. ” Recommended Practice VII: ◦ “Personnel who participate in invasive procedures are encouraged to voluntarily know if HIV & HBV status to the appropriate facility authority. ”
AORN Recommended Practices Recommended Practice VIII: ◦ Guidelines of the Centers for Disease Control Advisory Committee on Immunization Practices regarding HBV immunization should be followed. Recommended Practice IX: ◦ Transmission-based precautions should be used in addition to standard precautions for patient who are known or suspected to be infected with epidemiologically important and highly transmissible pathogens. Types of transmissionbased precautions include airborne, droplet and contact precautions.
AORN Recommended Practices Recommended Practice X: ◦ Policies and procedures that address occupational exposure to blood and body fluids and epidemiologically important microorganisms should be written, reviewed periodically, and readily available within the practice setting.
Event Related Sterility Actual shelf life of a sterile item is event-related not time-related. Events that render an item un-sterile. Proper packaging, handling and storage can prevent contamination. Before a package is opened, it must be visually inspected to determine if sterility appears to have been maintained. A pinhole, stain, or tear are obvious indicators that the item has been contaminated. Always check the expiration date before opening supplies on to a sterile field.
AORN Recommended Practice for Selection and Use of Packaging Systems Recommended Practice VIII: ◦ “According to AORN Recommended Practices for sterilization in practice settings, shelf life of a sterile packaged item is event-related. ”
Aseptic Practice and Prevention of Infection Surgical incision creates an opportunity for microorganisms to enter the body, resulting in infection. For all patients undergoing surgery, a common nursing diagnosis is: “Potential for high risk of surgical site infection. ”
Signs and Symptoms of Infection Fever Induration Cellulitis Erythema (redness) Purulent Drainage Abscess Dehiscence
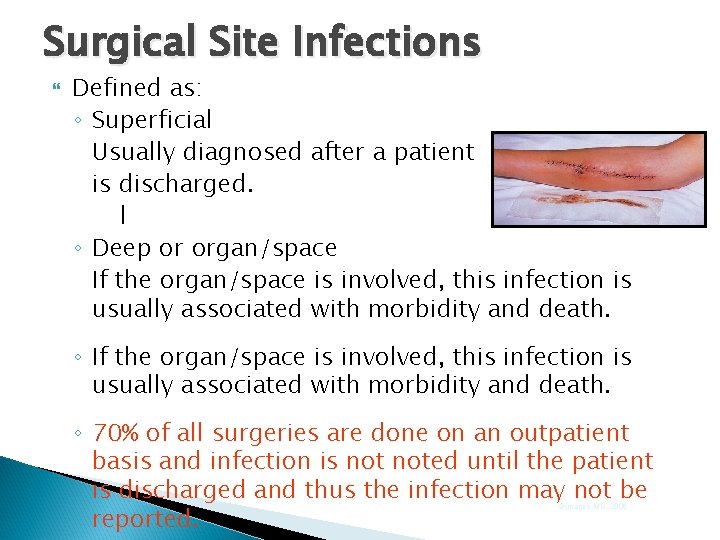
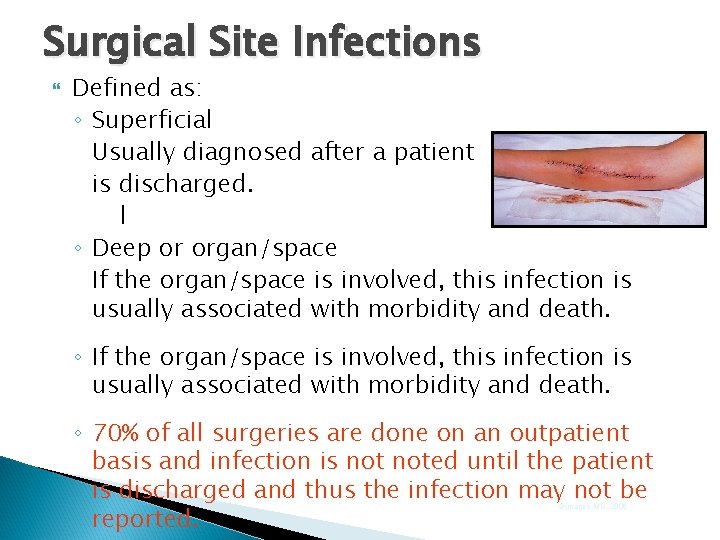
Surgical Site Infections Defined as: ◦ Superficial Usually diagnosed after a patient is discharged. l ◦ Deep or organ/space If the organ/space is involved, this infection is usually associated with morbidity and death. ◦ If the organ/space is involved, this infection is usually associated with morbidity and death. ◦ 70% of all surgeries are done on an outpatient basis and infection is noted until the patient is discharged and thus the infection may not be reported. ©images. MD, 2006
In Conclusion… Aseptic technique is used to prevent infection and contamination of sterile supplies. Asepsis is dependent on the sterile conscience of the personnel using sterile technique. Microsoft Clipart