Ascites Done by Dana Othman Investigation Abdominal ultrasonography
Ascites Done by : Dana Othman
Investigation � Abdominal ultrasonography, diagnostic paracentesis, and ascitic fluid cultures are recommended by the British Society of Gastroenterology, the European Association for the Study of the Liver (EASL), and the American Association for the Study of Liver Diseases (AASLD), particularly in the setting of supsected infection. [1 ] � Laparoscopy may be valuable for the diagnosis of otherwise unexplained cases, especially if malignant ascites is suspected. [6] This may be of particular importance in the diagnosis of malignant mesothelioma
Laboratory Studies In patients with new-onset ascites of unknown origin, peritoneal fluid should be sent for cell count, albumin level, culture, total protein, Gram stain, and cytology � Inspection: Most ascitic fluid is transparent and tinged yellow. A minimum of 10, 000 red blood cells/µL is required for ascitic fluid to appear pink, and more than 20, 000 red blood cells/µL will produce distinctly blood-tinged fluid. This may result from either a traumatic tap or malignancy. Bloody fluid from a traumatic tap is heterogeneously bloody, and the fluid will clot. Nontraumatic bloody fluid is homogeneously red and does not clot because the blood has already clotted and lysed. Cloudy ascitic fluid with a purulent consistency indicates infection

� Cell count: Normal ascitic fluid contains fewer than 500 leukocytes/µL and fewer than 250 polymorphonuclear leukocytes (PMNs)/µL. Any inflammatory condition cause an elevated white blood cell count. A PMN count of greater than 250 cells/µL is highly suggestive of bacterial peritonitis. [7] In tuberculous peritonitis and peritoneal carcinomatosis, lymphocytes usually predominate

� SAAG Interpretation The serum ascites albumin gradient (SAAG) is a formula used to assist in determining the etiology of ascites � � The formula is below. � SAAG = serum albumin – ascites albumin
A high gradient (SAAG >1. 1 g/d. L) indicates portal hypertension and suggests a nonperitoneal cause of ascites. � Such conditions may include the following: [1] � � � � Cirrhosis Fulminant hepatic failure Veno-occlusive disease Hepatic vein obstruction (ie, Budd-Chiari syndrome) Congestive heart failure Nephrotic syndrome Protein-losing enteropathy Malnutrition Myxedema Ovarian tumors Pancreatic ascites Biliary ascites Malignancy Trauma � Portal hypertension
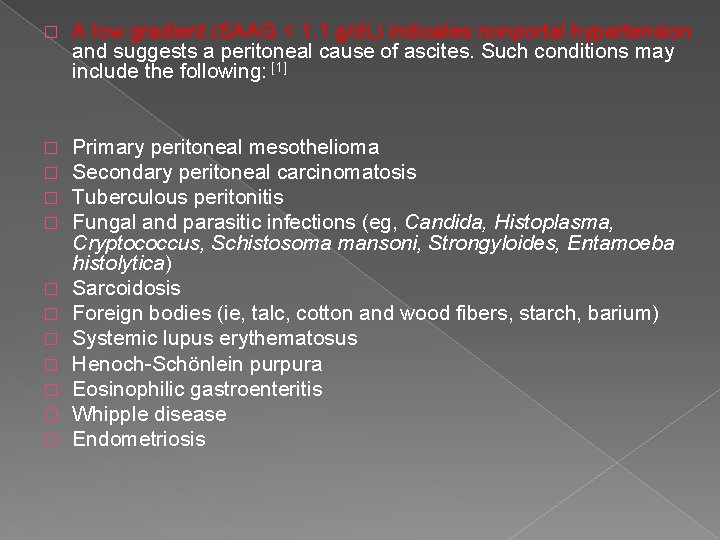
� A low gradient (SAAG < 1. 1 g/d. L) indicates nonportal hypertension and suggests a peritoneal cause of ascites. Such conditions may include the following: [1] � � Primary peritoneal mesothelioma Secondary peritoneal carcinomatosis Tuberculous peritonitis Fungal and parasitic infections (eg, Candida, Histoplasma, Cryptococcus, Schistosoma mansoni, Strongyloides, Entamoeba histolytica) Sarcoidosis Foreign bodies (ie, talc, cotton and wood fibers, starch, barium) Systemic lupus erythematosus Henoch-Schönlein purpura Eosinophilic gastroenteritis Whipple disease Endometriosis � � � �

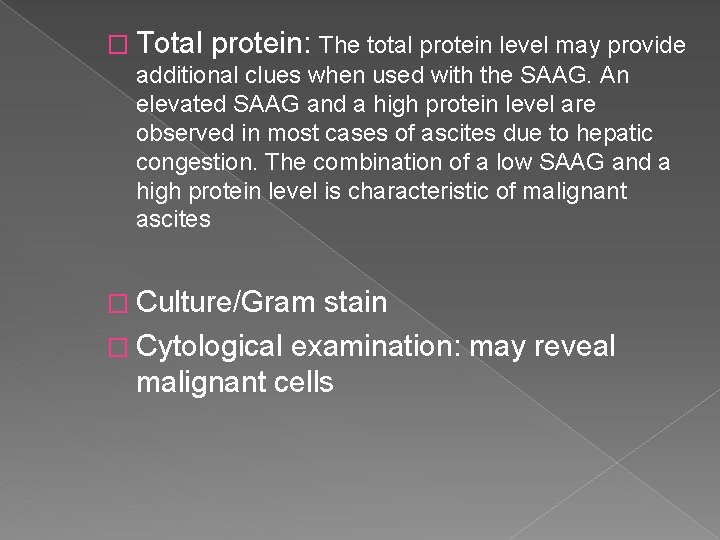
� Total protein: The total protein level may provide additional clues when used with the SAAG. An elevated SAAG and a high protein level are observed in most cases of ascites due to hepatic congestion. The combination of a low SAAG and a high protein level is characteristic of malignant ascites � Culture/Gram stain � Cytological examination: may reveal malignant cells
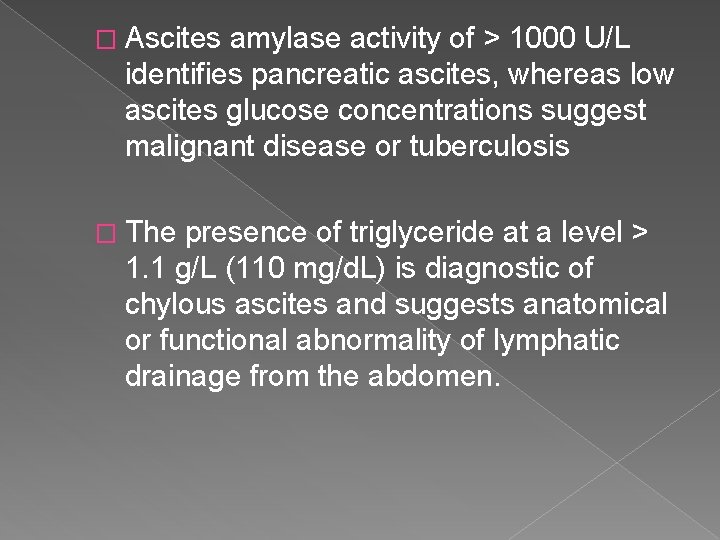
� Ascites amylase activity of > 1000 U/L identifies pancreatic ascites, whereas low ascites glucose concentrations suggest malignant disease or tuberculosis � The presence of triglyceride at a level > 1. 1 g/L (110 mg/d. L) is diagnostic of chylous ascites and suggests anatomical or functional abnormality of lymphatic drainage from the abdomen.

Management Sodium and water restriction Diuretics Paracentesis Transjugular intrahepatic portosystemic stent shunt

Sodium and water restriction � Restriction of dietary sodium intake is essential to achieve negative sodium balance and a few patients can be managed satisfactorily by this alone. Restriction of sodium intake to 100 mmol/24 hrs (‘no added salt diet ) is usually adequate. � Drugs containing relatively large amounts of sodium, and those promoting sodium retention

Medical treatment The goals of pharmacotherapy are to reduce morbidity and to prevent complications in patients with ascites. � Diuretics should be initiated in patients whose ascites does not respond to sodium restriction. A useful regimen is to start with spironolactone at 100 mg/d. The addition of loop diuretics may be necessary in some cases to increase the natriuretic effect. If no response occurs after 4 -5 days, the dosage may be increased stepwise up to spironolactone at 400 mg/d plus furosemide at 160 mg/d �

� Diuretic agents are the mainstay of medical therapy in ascites. � Spironolactone (Aldactone) � For the management of edema resulting from excessive aldosterone excretion. Competes with aldosterone for receptor sites in distal renal tubules, increasing water excretion while retaining potassium and hydrogen ions. The peak effect of Aldactone is approximately 3 d.
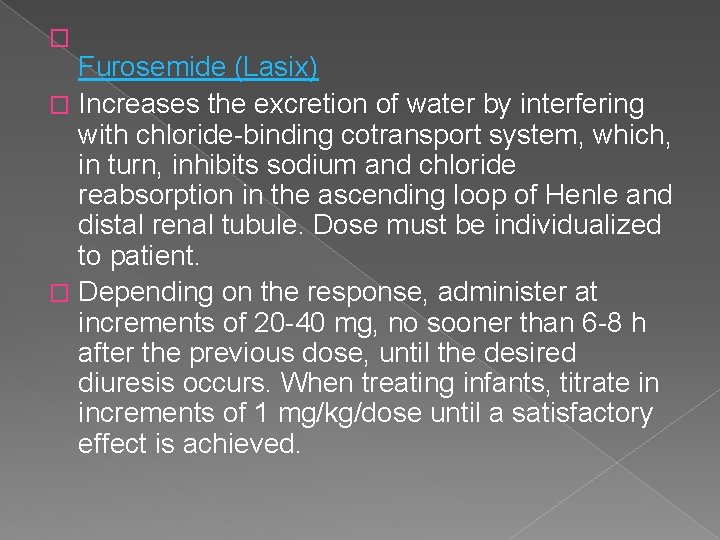
� Furosemide (Lasix) � Increases the excretion of water by interfering with chloride-binding cotransport system, which, in turn, inhibits sodium and chloride reabsorption in the ascending loop of Henle and distal renal tubule. Dose must be individualized to patient. � Depending on the response, administer at increments of 20 -40 mg, no sooner than 6 -8 h after the previous dose, until the desired diuresis occurs. When treating infants, titrate in increments of 1 mg/kg/dose until a satisfactory effect is achieved.
� Amiloride (midamor) � Metolazone (mykrox, zaroxolyn) � Mannitol (osmitrol)

Paracentesis � First-line treatment of refractory ascites is large-volume paracentesis. � Paracentesis can be used as an initial therapy or when other treatments fail
Transjugular intrahepatic portosystemic stent shunt Transjugular Intrahepatic Portosystemic Shunt or TIPS is a procedure that uses imaging guidance to connect the portal vein to the hepatic vein in the liver. A small metal device called a stent is placed to keep the connection open and allow it to bring blood draining from the bowel back to the heart while avoiding the liver. TIPS may successfully reduce internal bleeding in the stomach and esophagus in patients with cirrhosis.

Transjugular intrahepatic portosystemic stent shunt � transjugular intrahepatic portosystemic stent shunt can relieve resistant ascites but does not prolong life; � can be used in patients awaiting liver transplantation or in those with reasonable liver function, but can aggravate encephalopathy in those with poor function.
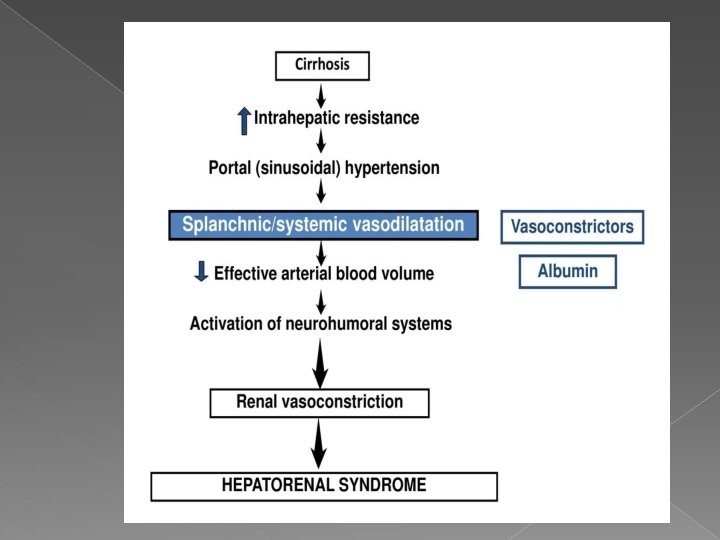
Complications Renal failure: It can be pre-renal due to vasodilatation from sepsis and/or diuretic therapy, or due to hepatorenal syndrome. � Hepatorenal syndrome � This occurs in 10% of patients with advanced cirrhosi complicated by ascites. � There are two clinical types; both are mediated by renal vasoconstriction due to under-filling of the arterial circulation �
Type 1 hepatorenal syndrome Type 1 HRS is characterized by rapidly progressive kidney failure, with a doubling of serum creatinine to a level greater than (2. 5 mg/dl). The prognosis of individuals with type 1 HRS is particularly grim, with a mortality rate exceeding 50% after one month. Patients with type 1 HRS are usually ill, may have low blood pressure , and may require therapy with drugs to improve the strength of heart muscle contraction (inotropes) or other drugs to maintain blood pressure (vasopressors). Unlike type II, in type I hepatorenal syndrome the renal failure improves with treatment and stabilizes. Vasoconstrictors and volume expanders are the mainstay of treatment

Type 2 hepatorenal syndrome In contrast, type 2 HRS is slower in onset and progression, and is not associated with an inciting event. It is defined by an increase in serum creatinine (1. 5 mg/d. L) Type 2 HRS is thought to be part of a spectrum of illness associated with increased pressures in the portal vein circulation, which begins with the development of fluid in the abdomen (ascites). The spectrum continues with diuretic-resistant ascites, where the kidneys are unable to excrete sufficient sodium to clear the fluid even with the use of diuretic medications. Most individuals with type 2 HRS have diureticresistant ascites before they develop deterioration in kidney function.

� Type 1 hepatorenal syndrome This is characterised by progressive oliguria, a rapid rise of the serum creatinine and a very poor prognosis � Type 2 hepatorenal syndrome This usually occurs in patients with refractory ascites, is characterised by a moderate and stable increase in serum creatinine, and has a better prognosis. � Spontaneous bacterial peritonitis

Prognosis Only 10– 20% of patients survive for 5 years from the first appearance of ascites due to cirrhosis. � and is best in those with well-maintained liver function and a good response to therapy. � The prognosis is also better when a treatable cause for the underlying cirrhosis is present or when a precipitating cause for ascites, such as excess salt intake, is found. �
reference � Davidson’s Principles and practice of medicine (2018, Elsevier) � Medscape
- Slides: 28