ARVO Meeting Fort Lauderdale Florida USA May 2
- Slides: 1
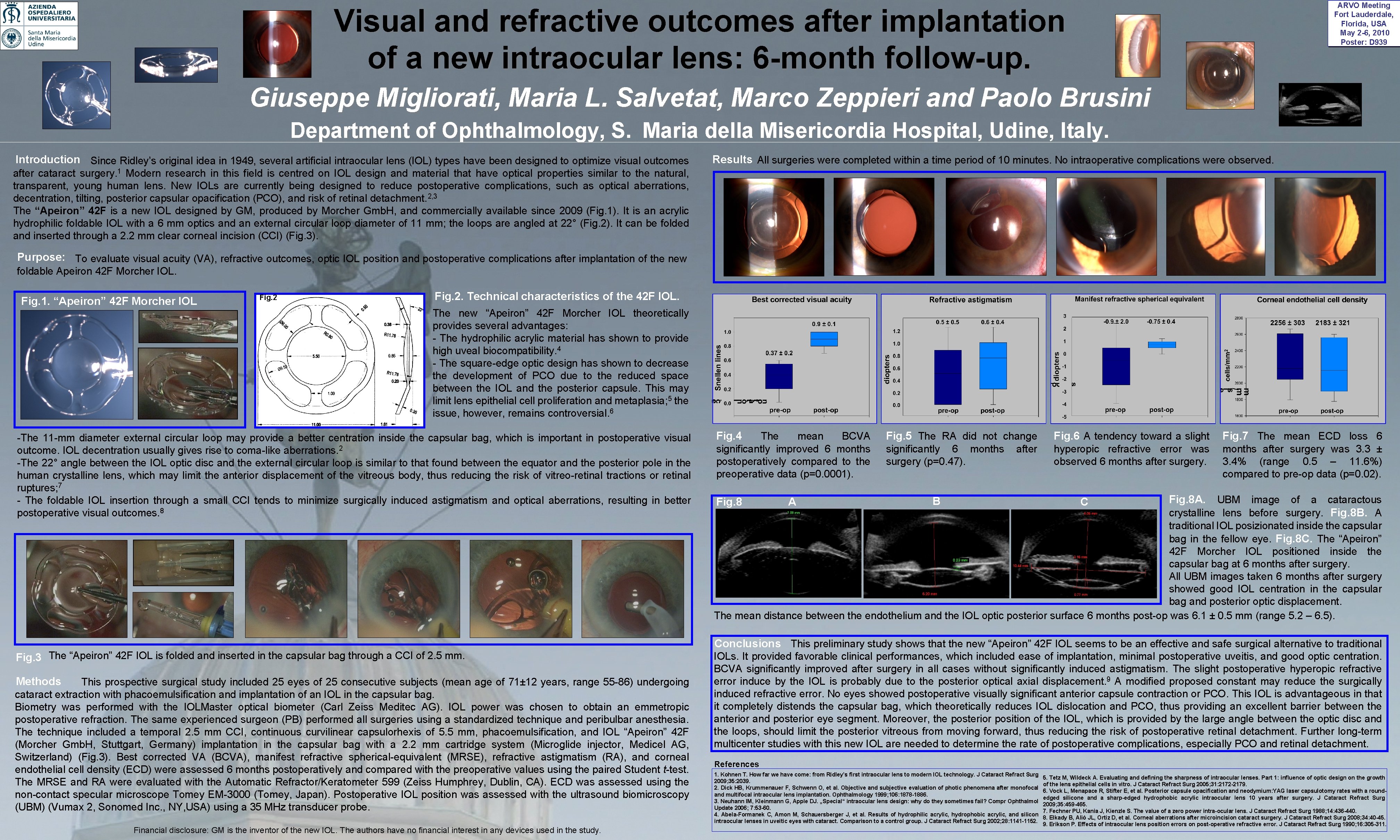
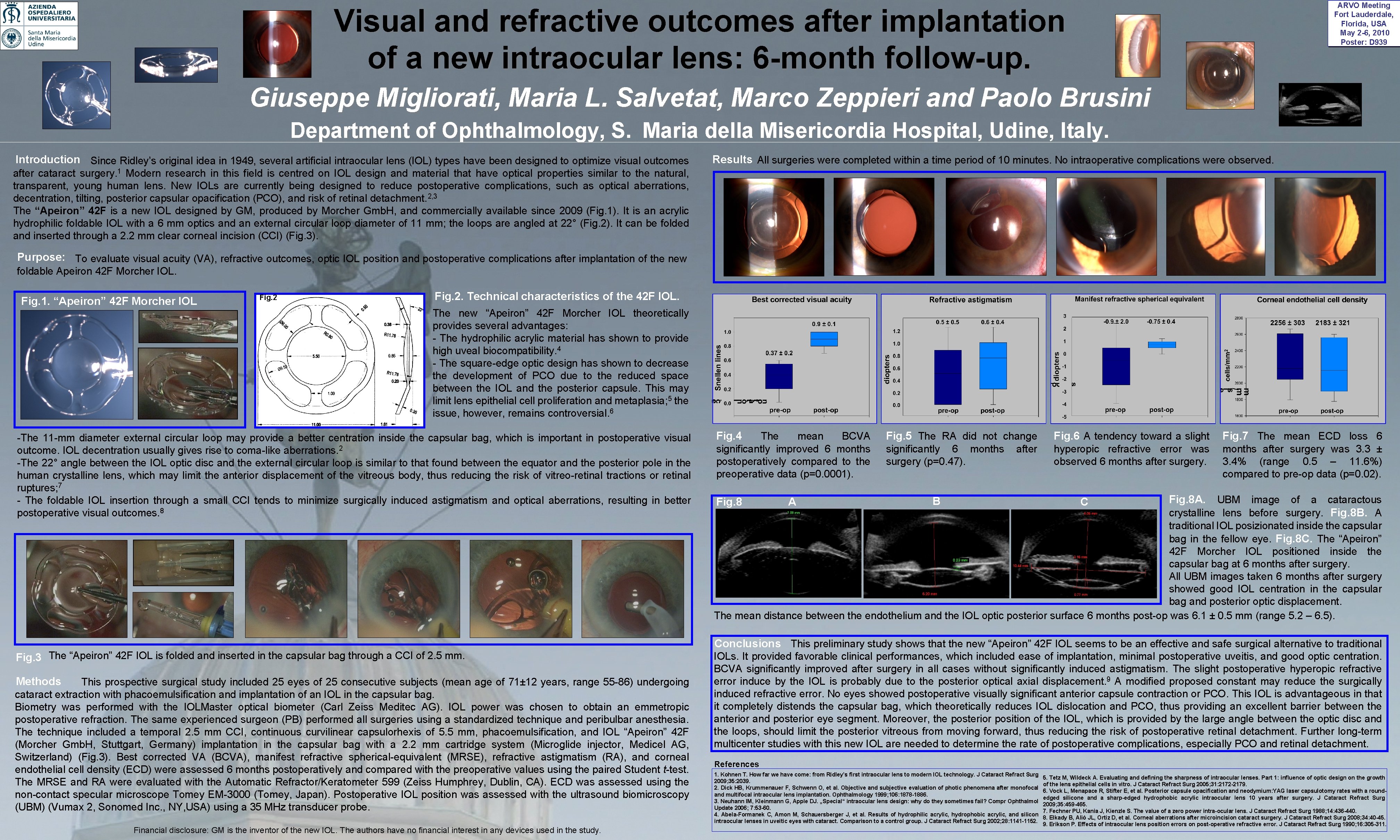
ARVO Meeting Fort Lauderdale, Florida, USA May 2 -6, 2010 Poster: D 939 Visual and refractive outcomes after implantation of a new intraocular lens: 6 -month follow-up. Giuseppe Migliorati, Maria L. Salvetat, Marco Zeppieri and Paolo Brusini Department of Ophthalmology, S. Maria della Misericordia Hospital, Udine, Italy. Introduction Since Ridley’s original idea in 1949, several artificial intraocular lens (IOL) types have been designed to optimize visual outcomes Results All surgeries were completed within a time period of 10 minutes. No intraoperative complications were observed. after cataract surgery. 1 Modern research in this field is centred on IOL design and material that have optical properties similar to the natural, transparent, young human lens. New IOLs are currently being designed to reduce postoperative complications, such as optical aberrations, decentration, tilting, posterior capsular opacification (PCO), and risk of retinal detachment. 2, 3 The “Apeiron” 42 F is a new IOL designed by GM, produced by Morcher Gmb. H, and commercially available since 2009 (Fig. 1). It is an acrylic hydrophilic foldable IOL with a 6 mm optics and an external circular loop diameter of 11 mm; the loops are angled at 22° (Fig. 2). It can be folded and inserted through a 2. 2 mm clear corneal incision (CCI) (Fig. 3). Purpose: To evaluate visual acuity (VA), refractive outcomes, optic IOL position and postoperative complications after implantation of the new foldable Apeiron 42 F Morcher IOL. Fig. 1. “Apeiron” 42 F Morcher IOL Fig. 2. Technical characteristics of the 42 F IOL. The new “Apeiron” 42 F Morcher IOL theoretically provides several advantages: - The hydrophilic acrylic material has shown to provide high uveal biocompatibility. 4 - The square-edge optic design has shown to decrease the development of PCO due to the reduced space between the IOL and the posterior capsule. This may limit lens epithelial cell proliferation and metaplasia; 5 the issue, however, remains controversial. 6 -The 11 -mm diameter external circular loop may provide a better centration inside the capsular bag, which is important in postoperative visual outcome. IOL decentration usually gives rise to coma-like aberrations. 2 -The 22° angle between the IOL optic disc and the external circular loop is similar to that found between the equator and the posterior pole in the human crystalline lens, which may limit the anterior displacement of the vitreous body, thus reducing the risk of vitreo-retinal tractions or retinal ruptures; 7 - The foldable IOL insertion through a small CCI tends to minimize surgically induced astigmatism and optical aberrations, resulting in better postoperative visual outcomes. 8 Fig. 4 The mean BCVA significantly improved 6 months postoperatively compared to the preoperative data (p=0. 0001). Fig. 5 The RA did not change Fig. 6 A tendency toward a slight Fig. 7 The mean ECD loss 6 significantly 6 months surgery (p=0. 47). hyperopic refractive error was observed 6 months after surgery was 3. 3 ± 3. 4% (range 0. 5 – 11. 6%) compared to pre-op data (p=0. 02). after Fig. 8 A. UBM image of a cataractous crystalline lens before surgery. Fig. 8 B. A traditional IOL posizionated inside the capsular bag in the fellow eye. Fig. 8 C. The “Apeiron” 42 F Morcher IOL positioned inside the capsular bag at 6 months after surgery. All UBM images taken 6 months after surgery showed good IOL centration in the capsular bag and posterior optic displacement. The mean distance between the endothelium and the IOL optic posterior surface 6 months post-op was 6. 1 ± 0. 5 mm (range 5. 2 – 6. 5). Fig. 8 A B C Conclusions This preliminary study shows that the new “Apeiron” 42 F IOL seems to be an effective and safe surgical alternative to traditional Fig. 3 The “Apeiron” 42 F IOL is folded and inserted in the capsular bag through a CCI of 2. 5 mm. Methods This prospective surgical study included 25 eyes of 25 consecutive subjects (mean age of 71± 12 years, range 55 -86) undergoing cataract extraction with phacoemulsification and implantation of an IOL in the capsular bag. Biometry was performed with the IOLMaster optical biometer (Carl Zeiss Meditec AG). IOL power was chosen to obtain an emmetropic postoperative refraction. The same experienced surgeon (PB) performed all surgeries using a standardized technique and peribulbar anesthesia. The technique included a temporal 2. 5 mm CCI, continuous curvilinear capsulorhexis of 5. 5 mm, phacoemulsification, and IOL “Apeiron” 42 F (Morcher Gmb. H, Stuttgart, Germany) implantation in the capsular bag with a 2. 2 mm cartridge system (Microglide injector, Medicel AG, Switzerland) (Fig. 3). Best corrected VA (BCVA), manifest refractive spherical-equivalent (MRSE), refractive astigmatism (RA), and corneal endothelial cell density (ECD) were assessed 6 months postoperatively and compared with the preoperative values using the paired Student t-test. The MRSE and RA were evaluated with the Automatic Refractor/Keratometer 599 (Zeiss Humphrey, Dublin, CA). ECD was assessed using the non-contact specular microscope Tomey EM-3000 (Tomey, Japan). Postoperative IOL position was assessed with the ultrasound biomicroscopy (UBM) (Vumax 2, Sonomed Inc. , NY, USA) using a 35 MHz transducer probe. Financial disclosure: GM is the inventor of the new IOL. The authors have no financial interest in any devices used in the study. IOLs. It provided favorable clinical performances, which included ease of implantation, minimal postoperative uveitis, and good optic centration. BCVA significantly improved after surgery in all cases without significantly induced astigmatism. The slight postoperative hyperopic refractive error induce by the IOL is probably due to the posterior optical axial displacement. 9 A modified proposed constant may reduce the surgically induced refractive error. No eyes showed postoperative visually significant anterior capsule contraction or PCO. This IOL is advantageous in that it completely distends the capsular bag, which theoretically reduces IOL dislocation and PCO, thus providing an excellent barrier between the anterior and posterior eye segment. Moreover, the posterior position of the IOL, which is provided by the large angle between the optic disc and the loops, should limit the posterior vitreous from moving forward, thus reducing the risk of postoperative retinal detachment. Further long-term multicenter studies with this new IOL are needed to determine the rate of postoperative complications, especially PCO and retinal detachment. References 1. Kohnen T. How far we have come: from Ridley’s first intraocular lens to modern IOL technology. J Cataract Refract Surg 2009; 35: 2039. 2. Dick HB, Krummenauer F, Schwenn O, et al. Objective and subjective evaluation of photic phenomena after monofocal and multifocal intraocular lens implantation. Ophthalmology 1999; 106: 1878 -1886. 3. Neuhann IM, Kleinmann G, Apple DJ. „Special“ intraocular lens design: why do they sometimes fail? Compr Ophthalmol Update 2006; 7: 53 -60. 4. Abela-Formanek C, Amon M, Schauersberger J, et al. Results of hydrophilic acrylic, hydrophobic acrylic, and silicon intraocular lenses in uveitic eyes with cataract. Comparison to a control group. J Cataract Refract Surg 2002; 28: 1141 -1152. 5. Tetz M, Wildeck A. Evaluating and defining the sharpness of intraocular lenses. Part 1: influence of optic design on the growth of the lens epithelial cells in vitro. J Cataract Refract Surg 2005; 31: 2172 -2179. 6. Vock L, Menapace R, Stifter E, et al. Posterior capsule opacification and neodymium: YAG laser capsulotomy rates with a roundedged silicone and a sharp-edged hydrophobic acrylic intraocular lens 10 years after surgery. J Cataract Refract Surg 2009; 35: 459 -465. 7. Fechner PU, Kania J, Kienzle S. The value of a zero power intra-ocular lens. J Cataract Refract Surg 1988; 14: 436 -440. 8. Elkady B, Aliò JL, Ortiz D, et al. Corneal aberrations after microincision cataract surgery. J Cataract Refract Surg 2008; 34: 40 -45. 9. Erikson P. Effects of intraocular lens position errors on post-operative refractive error. J Cataract Refract Surg 1990; 16: 305 -311.