Arthritis Osteoarthritis OA Osteoarthritis Most common form of









- Slides: 38
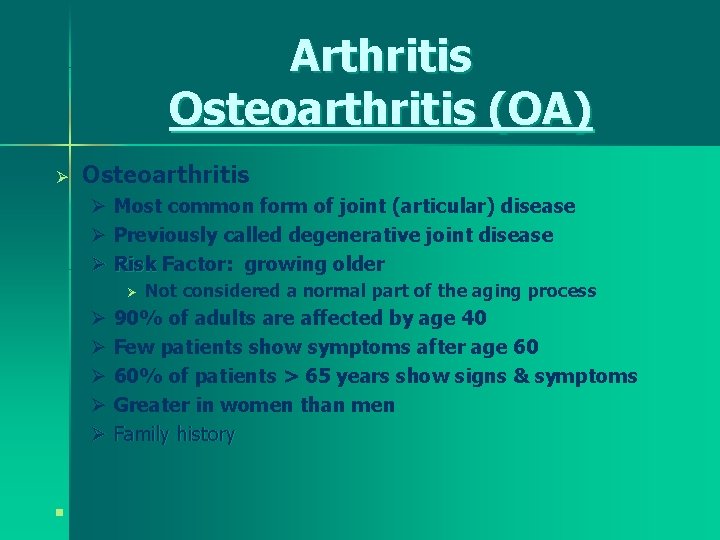
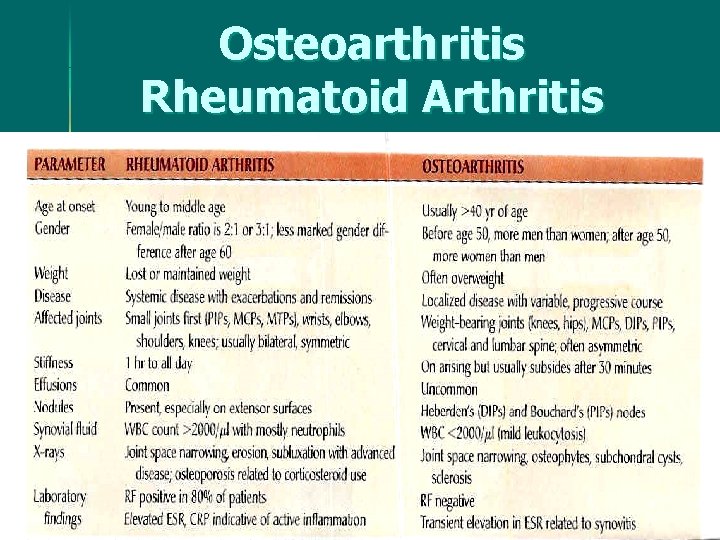
Arthritis Osteoarthritis (OA) Ø Osteoarthritis Ø Most common form of joint (articular) disease Ø Previously called degenerative joint disease Ø Risk Factor: growing older Ø Not considered a normal part of the aging process Ø 90% of adults are affected by age 40 Ø Few patients show symptoms after age 60 Ø 60% of patients > 65 years show signs & symptoms Ø Greater in women than men Ø Family history n
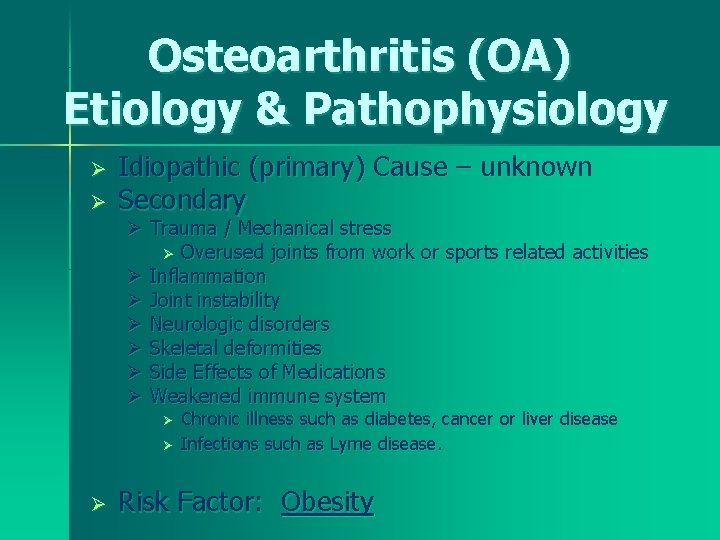
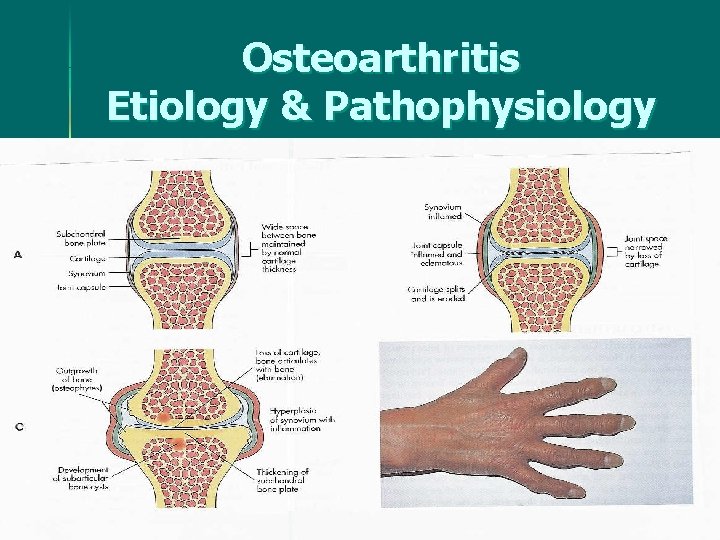
Osteoarthritis (OA) Etiology & Pathophysiology Ø Ø Idiopathic (primary) Cause – unknown Secondary Ø Trauma / Mechanical stress Ø Overused joints from work or sports related activities Ø Inflammation Ø Joint instability Ø Neurologic disorders Ø Skeletal deformities Ø Side Effects of Medications Ø Weakened immune system Ø Ø Ø Chronic illness such as diabetes, cancer or liver disease Infections such as Lyme disease. Risk Factor: Obesity
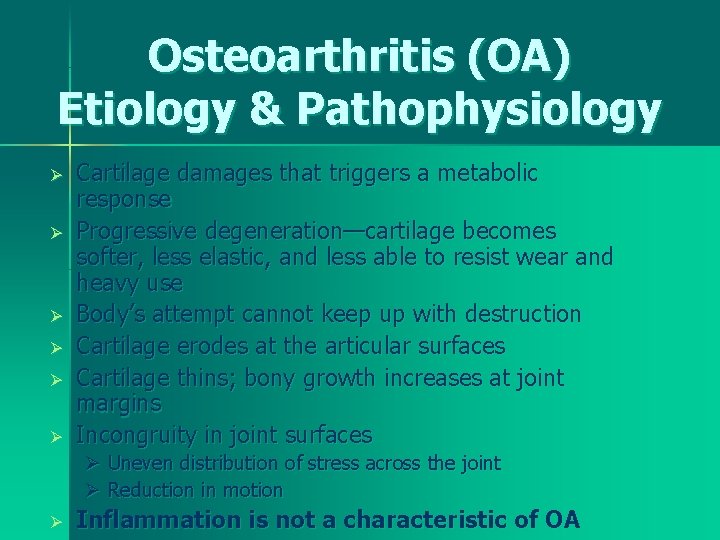
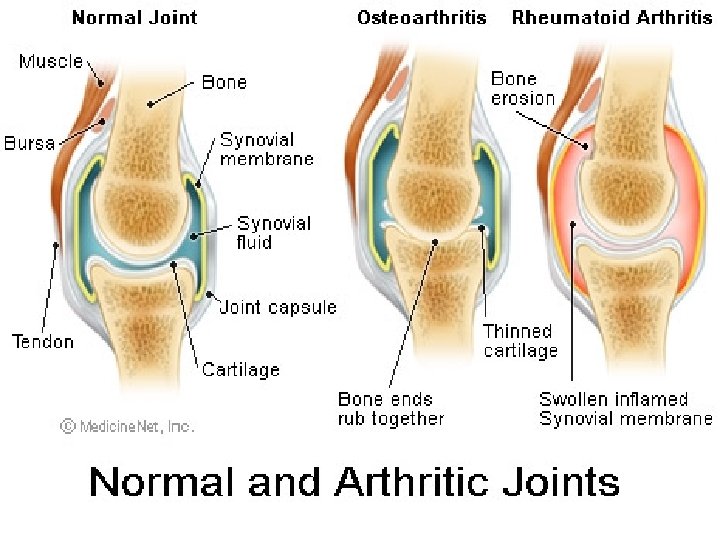
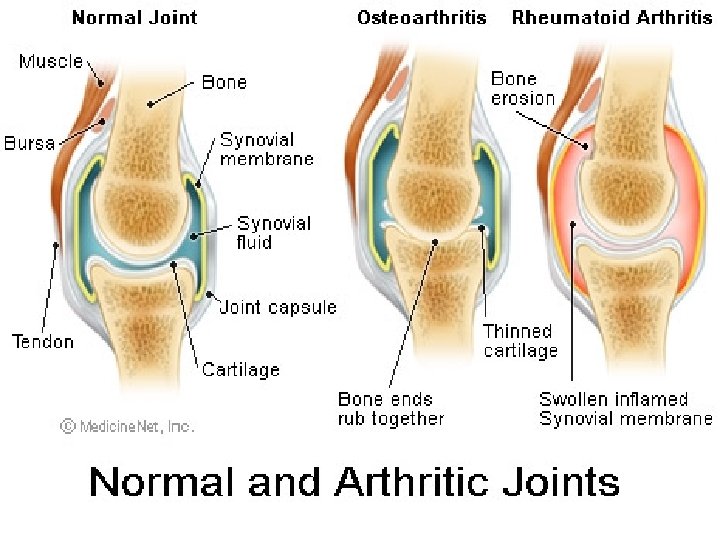
Osteoarthritis (OA) Etiology & Pathophysiology Ø Ø Ø Cartilage damages that triggers a metabolic response Progressive degeneration—cartilage becomes softer, less elastic, and less able to resist wear and heavy use Body’s attempt cannot keep up with destruction Cartilage erodes at the articular surfaces Cartilage thins; bony growth increases at joint margins Incongruity in joint surfaces Ø Uneven distribution of stress across the joint Ø Reduction in motion Ø Inflammation is not a characteristic of OA
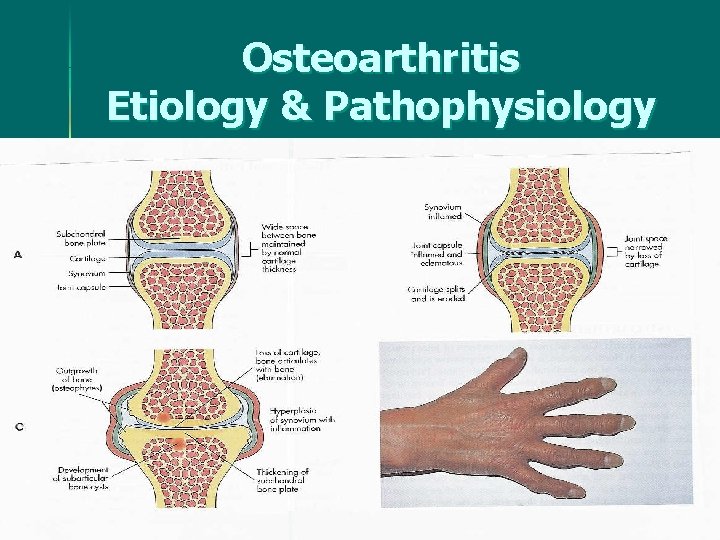
Osteoarthritis Etiology & Pathophysiology
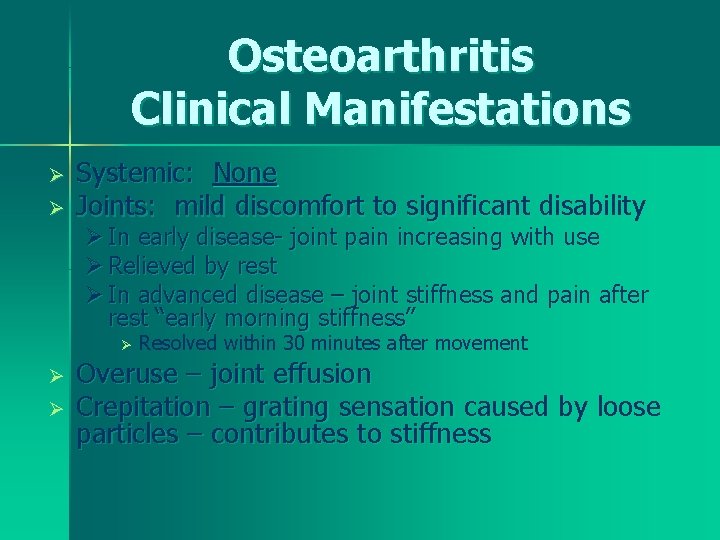
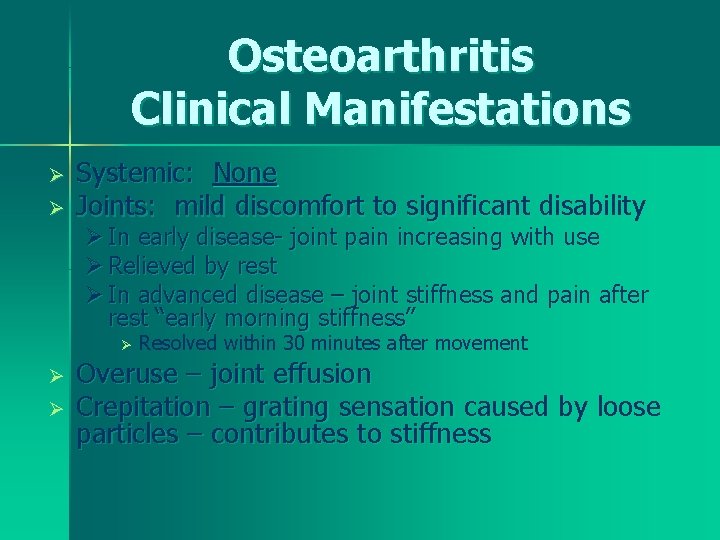
Osteoarthritis Clinical Manifestations Ø Ø Systemic: None Joints: mild discomfort to significant disability Ø In early disease- joint pain increasing with use Ø Relieved by rest Ø In advanced disease – joint stiffness and pain after rest “early morning stiffness” Ø Ø Ø Resolved within 30 minutes after movement Overuse – joint effusion Crepitation – grating sensation caused by loose particles – contributes to stiffness
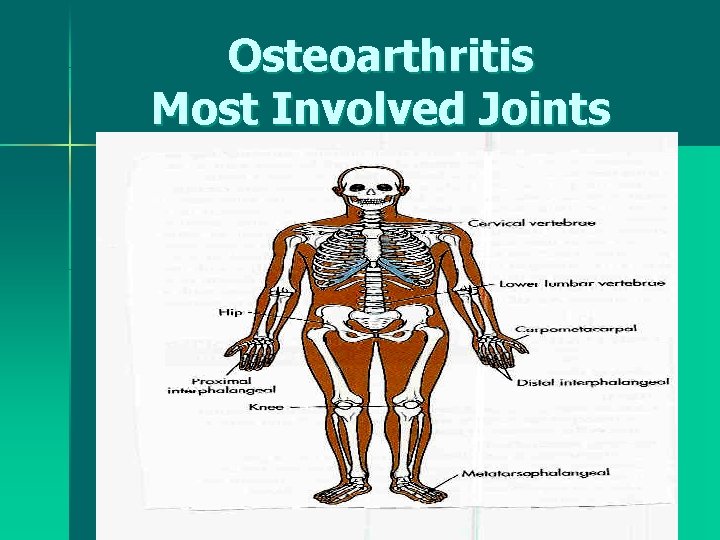
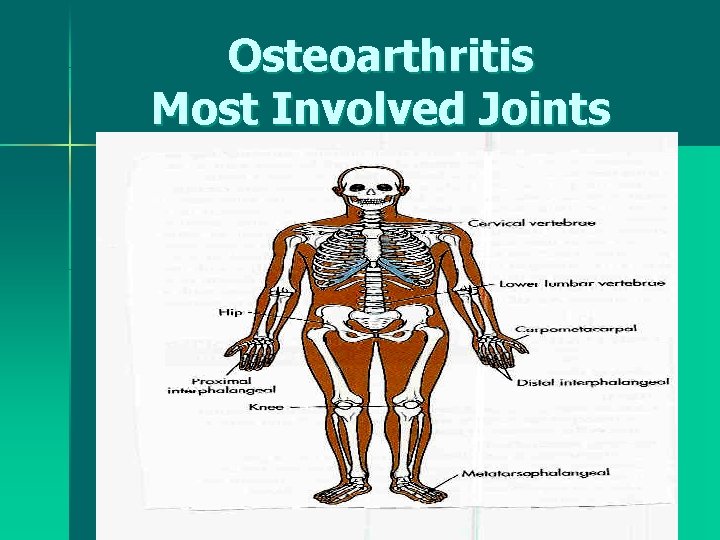
Osteoarthritis Most Involved Joints

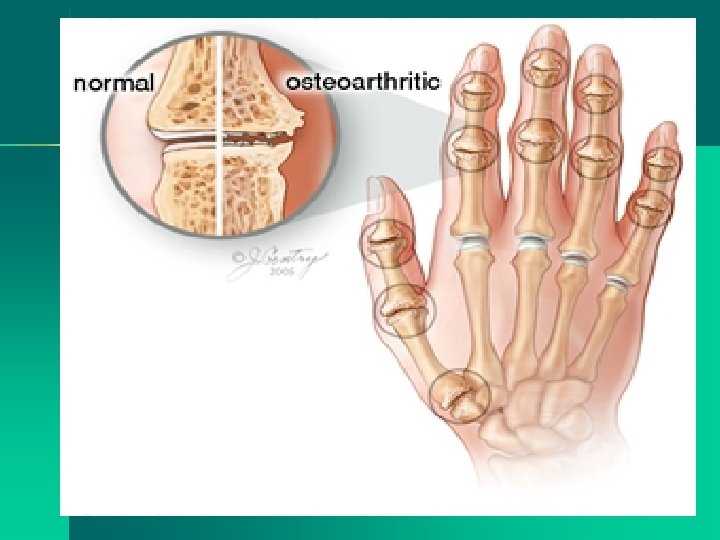
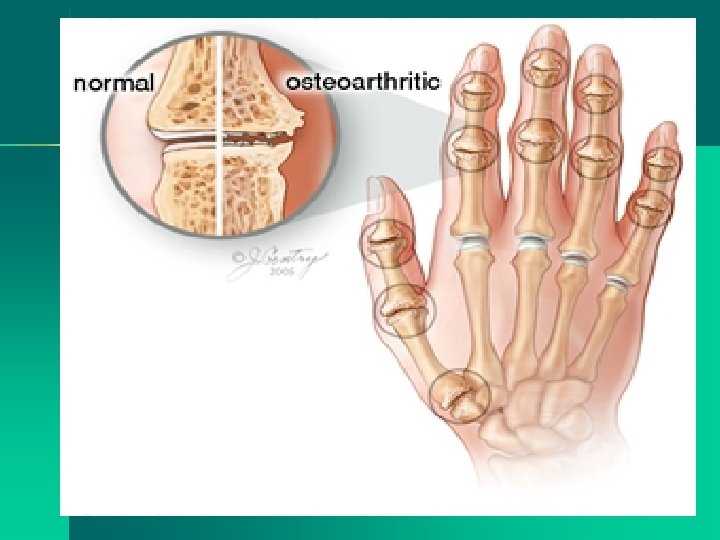
Osteoarthritis Etiology & Pathophysiology Affects joints asymmetrically Ø Most commonly involved joints: Ø ØDistal interphalangeal (DIP) ØProximal interphalangeal (PIP) ØCarpometacarpal joint of the thumb ØWeight-bearing joints (hips, knees) ØMetatarsophalangeal (MTP) joint of the foot ØCervical and lumbar vertebrae
Osteoarthritis Etiology & Pathophysiology Ø Deformity ØSpecific to the involved joint Ø Herberden’s nodes – DIP joints Ø Bouchard’s nodes – PIP joints Ø Both are red, edematous, tender-painful Ø Do not usually cause loss of function
Osteoarthritis Diagnostic Studies Bone Scan Ø CT Ø MRI Ø General x-ray Ø Radiologic changes do not correlate with the degree of disease

Osteoarthritis Treatment Goals Ø No cure Ø Focus: ØManaging pain ØPreventing disability ØMaintaining and improving joint function

Osteoarthritis Treatment Goals Ø Rest and Joint Protection ØBalance of rest and activity ØAssistive devices Ø Heat and Cold Applications ØHot packs, whirlpools, ultrasound, paraffin wax baths, pool therapy Ø Nutritional Therapy & Exercise ØWeight reduction – Goal: decrease load on the joints & increase joint mobilization
Osteoarthritis - Tx Goals Ø Drug Therapy Ø Tylenol – up to 1000 mg q 6 h Ø Aspirin Ø Nonsteroidal anti-inflammatory drugs Motrin (OTC) 200 mg qid++ Ø Traditional NSAID – decrease platelet aggregation – prolong bleeding time Ø Newer generation – Cox inhibitors (cyclooxygenase) e. g. , Celebrex Ø Intraarticular injections—knees; shoulder Ø Intraforamenal-intervertebral Injections – vertebral Ø Corticosteroids – decrease local inflammation & effusion Ø Hyaluronic Acid – increased production of synovial fluid – Hyalgan, Synvisc Ø

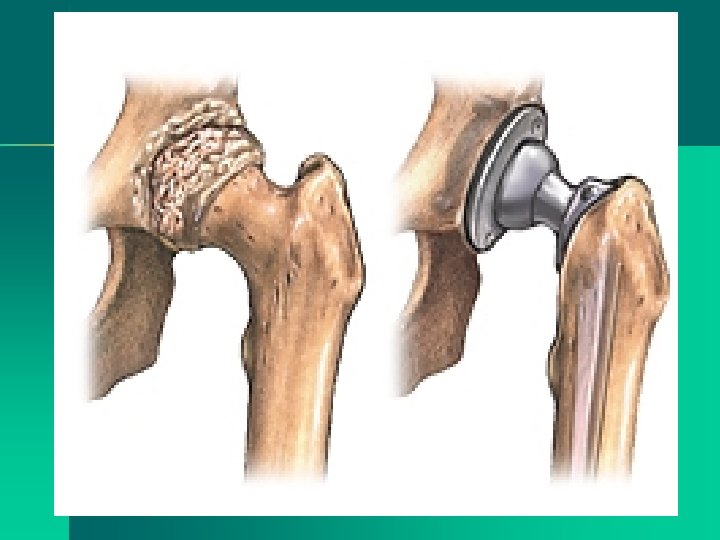
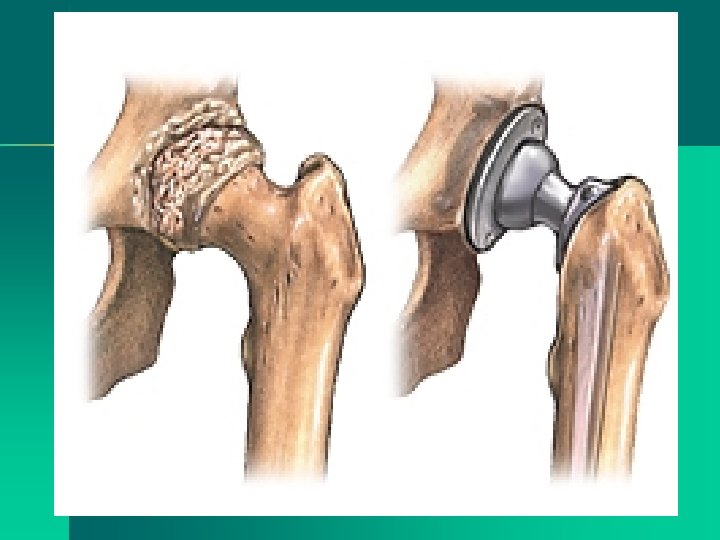
Osteoarthritis Treatment Goals Ø Surgical Treatment ØJoint Replacement Ø Hip, Knee, Shoulder ØSpinal Surgery – Ø Diskectomy /spinal fusion

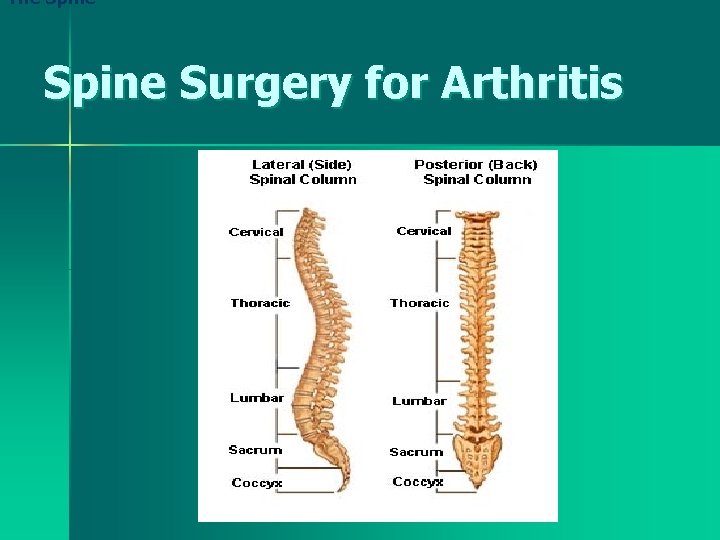
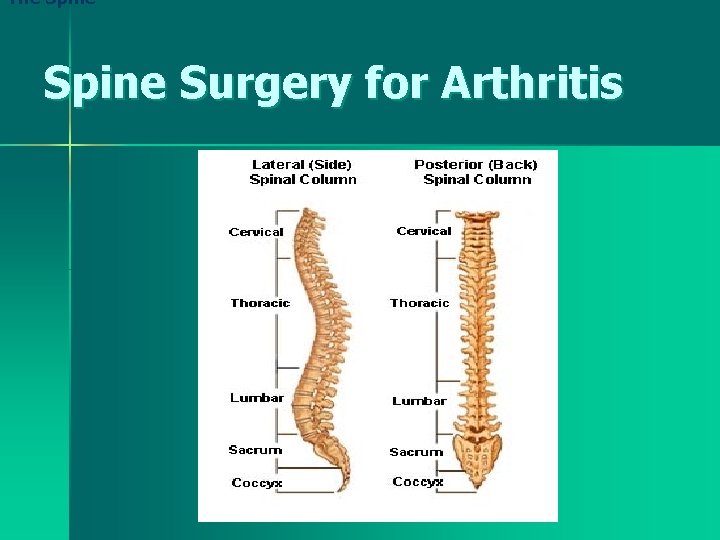
The Spine Surgery for Arthritis
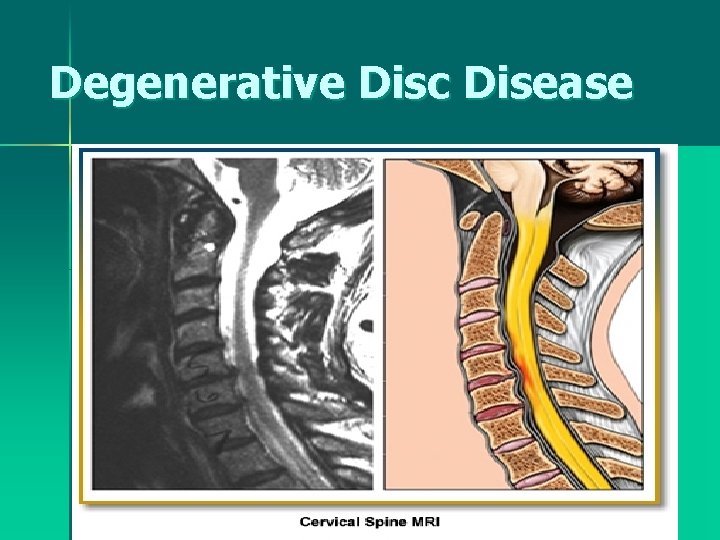
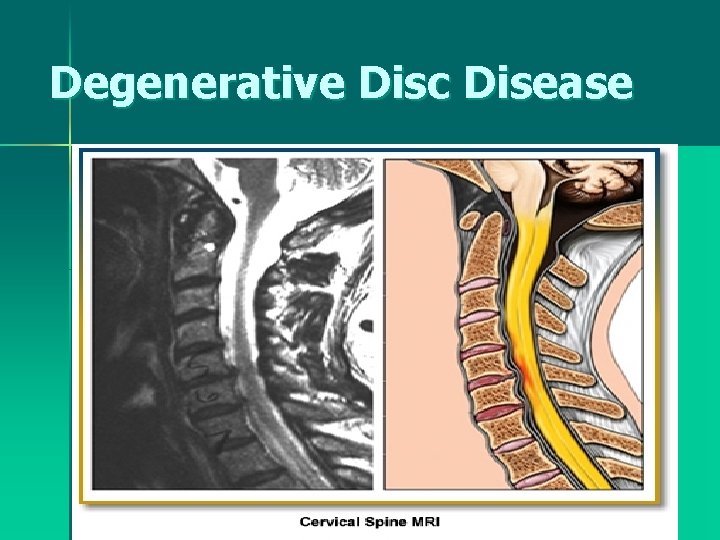
Degenerative Disc Disease
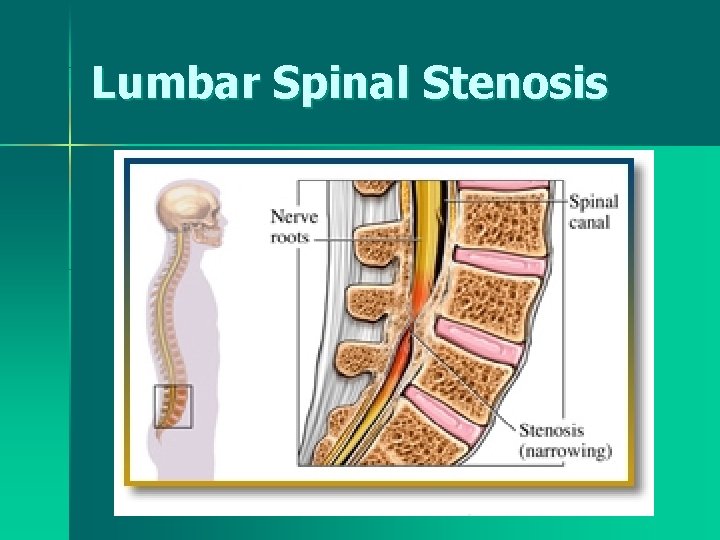
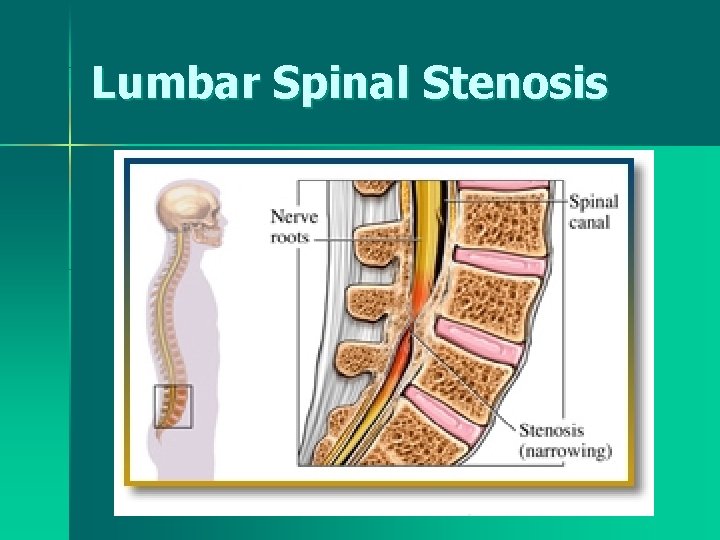
Lumbar Spinal Stenosis
Osteoarthritis Nursing Diagnoses Acute & Chronic Pain r/t physical activity Ø Disturbed sleeping pattern Ø Impaired physical mobility Ø Self-care deficits r/t joint deformity & pain Ø Imbalanced nutrition Ø Chronic low self-esteem r/t changing physical appearance Ø

Osteoarthritis Nursing Management Goals Ø Maintain or improve joint function through balance of rest and activity Ø Joint protection measures to improve activity tolerance Ø Maintain independence and self-care Ø Use drug therapy safely to manage pain without side effects Ø REHABILITATION
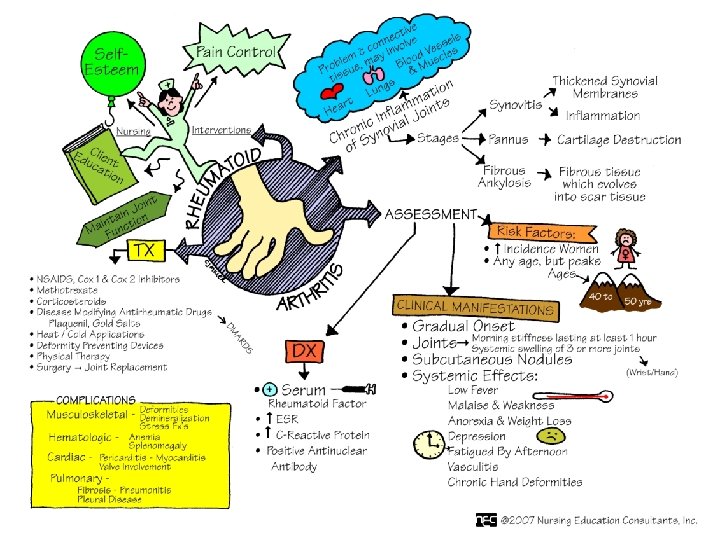
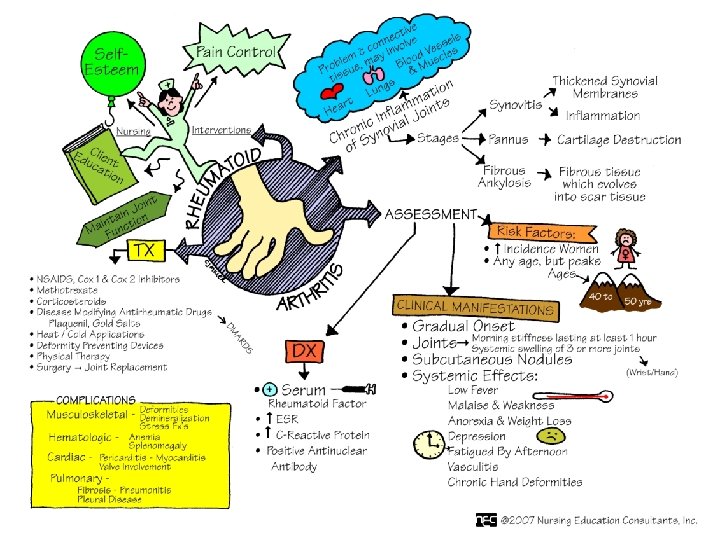
Rheumatoid Arthritis (RA) Ø Chronic, systemic disease Ø Inflammation of connective tissue in the diarthrodial (synovial) joint Ø Periods of remissions & exacerbation Ø Extraarticular manifestations
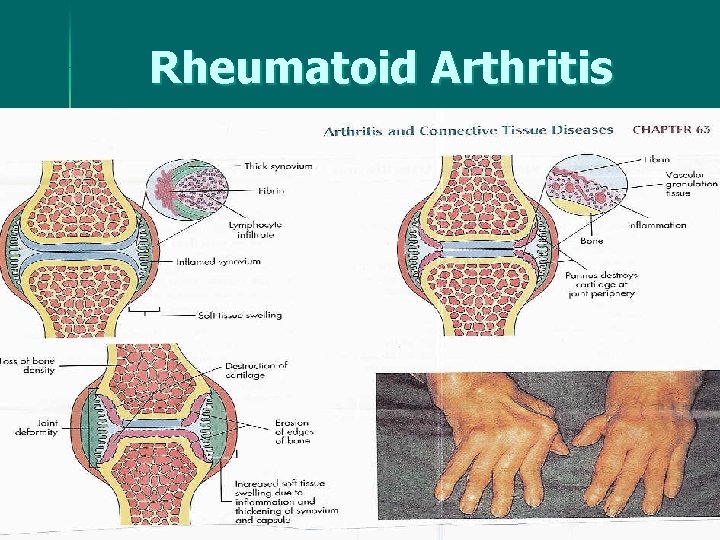
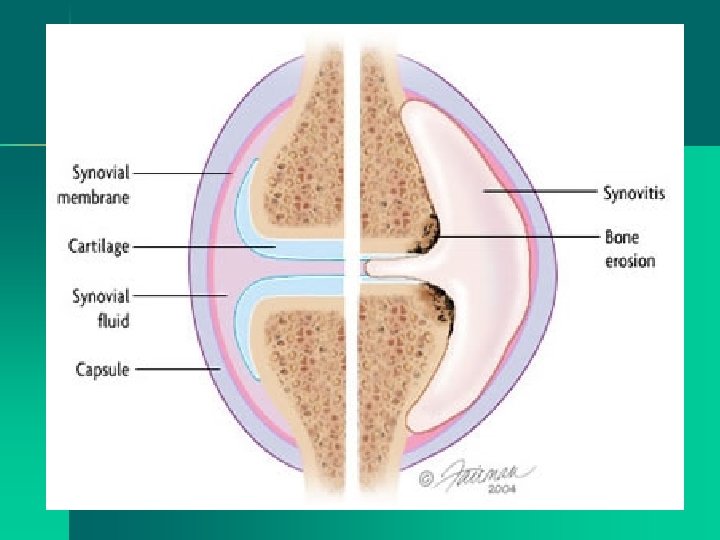
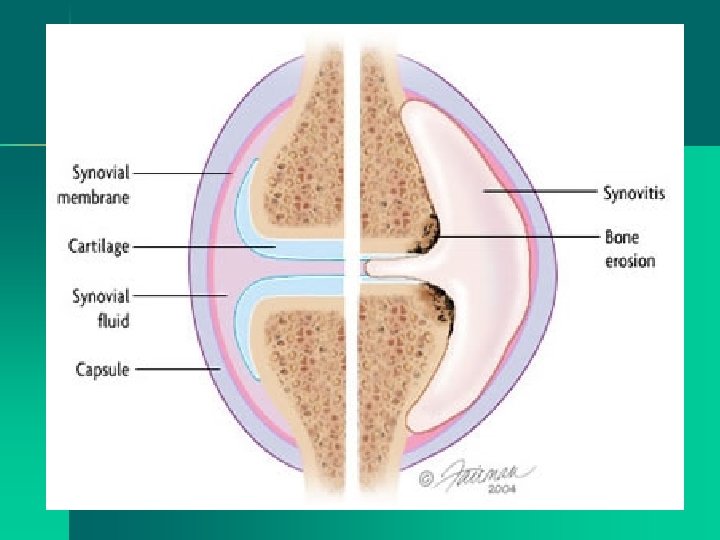
Rheumatoid Arthritis (RA) Etiology & Pathophysiology Ø Ø Cause – unknown Autoimmune – most widely accepted theory Ø Antigen/abnormal Immunoglobulin G (Ig. G) Ø Presence of autoantibodies – rheumatoid factor Ø Ig. G + rheumatoid factor form deposits on synovial membranes & articular cartilage Inflammation results – pannus (granulation tissue at the joint margins) – articular cartilage destruction Ø Genetic – predisposition/familial occurrence of “human leukocyte antigen (HLA) in white RA patients Ø
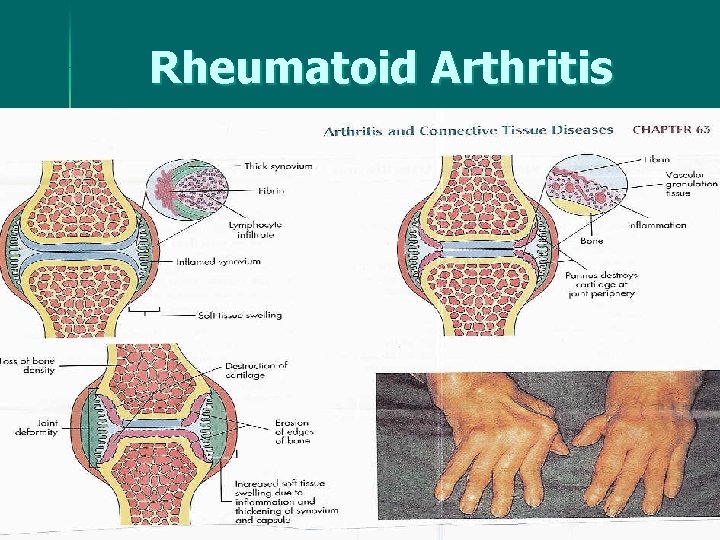
Rheumatoid Arthritis
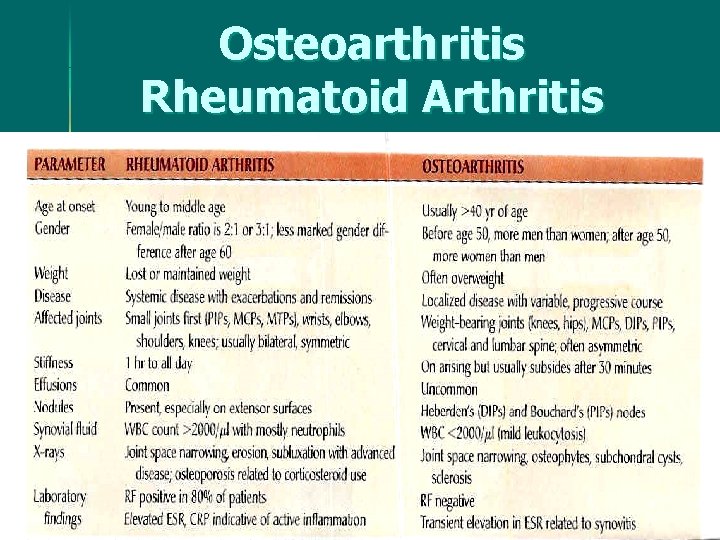
Osteoarthritis Rheumatoid Arthritis
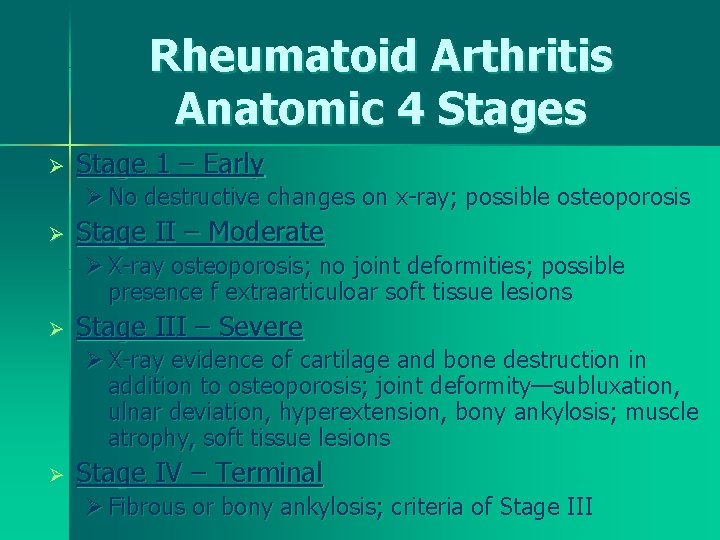
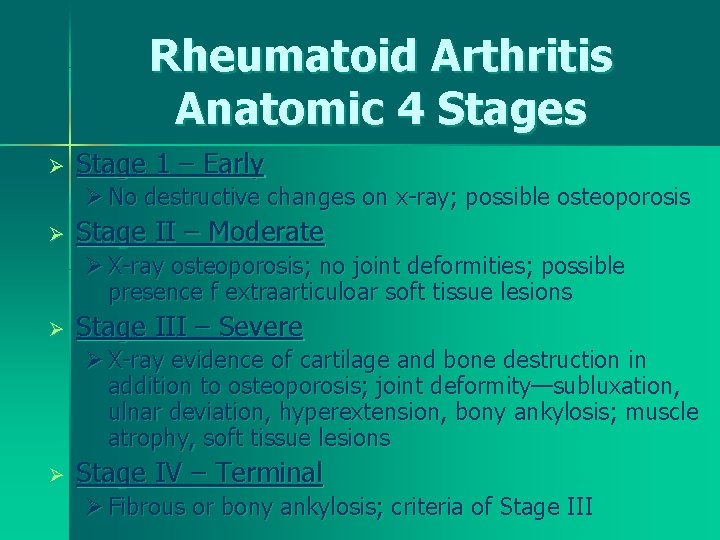
Rheumatoid Arthritis Anatomic 4 Stages Ø Stage 1 – Early Ø No destructive changes on x-ray; possible osteoporosis Ø Stage II – Moderate Ø X-ray osteoporosis; no joint deformities; possible presence f extraarticuloar soft tissue lesions Ø Stage III – Severe Ø X-ray evidence of cartilage and bone destruction in addition to osteoporosis; joint deformity—subluxation, ulnar deviation, hyperextension, bony ankylosis; muscle atrophy, soft tissue lesions Ø Stage IV – Terminal Ø Fibrous or bony ankylosis; criteria of Stage III

Rheumatoid Arthritis Clinical Manifestations Insidious – fatigue, anorexia, weight loss, generalized stiffness Ø Joints Ø ØStiffness becomes localized—pain, edema, limited motion, inflammation, joints warm to touch, fingers—spindle shaped Ø“Morning Stiffness” – 60+ mins to several hours depending on disease progression
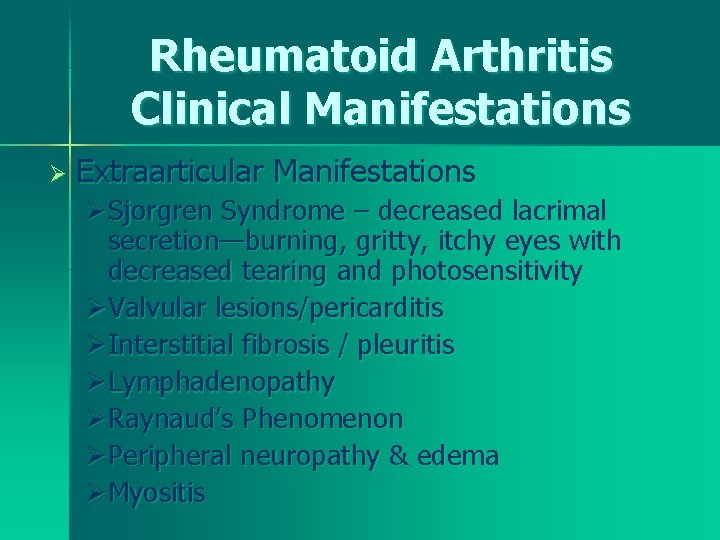
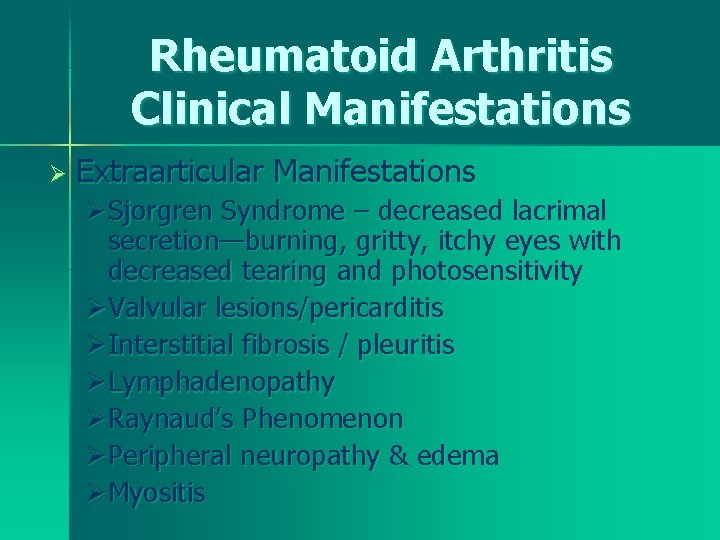
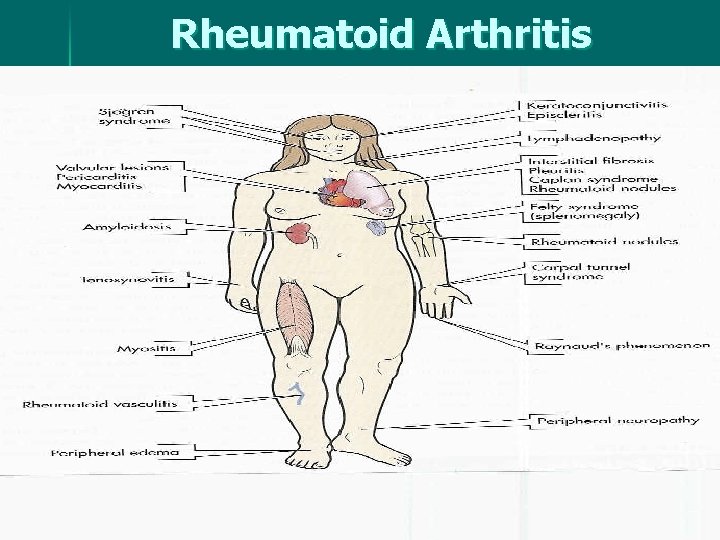
Rheumatoid Arthritis Clinical Manifestations Ø Extraarticular Manifestations ØSjorgren Syndrome – decreased lacrimal secretion—burning, gritty, itchy eyes with decreased tearing and photosensitivity ØValvular lesions/pericarditis ØInterstitial fibrosis / pleuritis ØLymphadenopathy ØRaynaud’s Phenomenon ØPeripheral neuropathy & edema ØMyositis
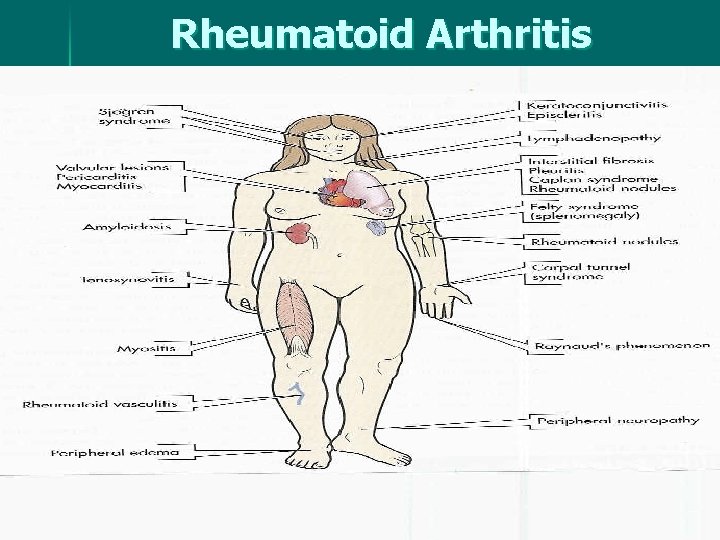
Rheumatoid Arthritis Clinical Manifestations
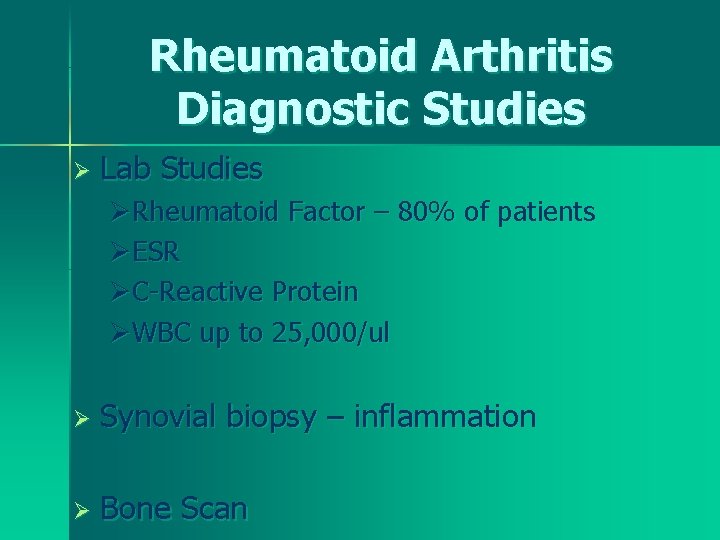
Rheumatoid Arthritis Diagnostic Studies Ø Lab Studies ØRheumatoid Factor – 80% of patients ØESR ØC-Reactive Protein ØWBC up to 25, 000/ul Ø Synovial biopsy – inflammation Ø Bone Scan

Rheumatoid Arthritis Treatment Goals Ø Drug Therapy ØNSAIDs ØDisease-modifying antirheumatic drugs (DMARDS) - Anti-inflammatory action Ø Mild Disease – Plaquenil (antimalarial drug) Ø Moderate – Severe Disease -- Methotrexate Ø Severe Disease - Gold Therapy (weekly injections x 5 months) Ø Corticosteroid Ø Nutrition Therapy – balanced diet
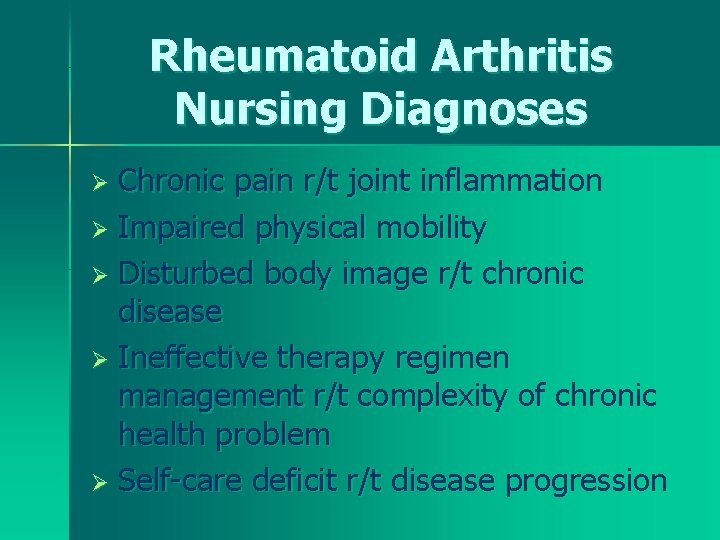
Rheumatoid Arthritis Nursing Diagnoses Chronic pain r/t joint inflammation Ø Impaired physical mobility Ø Disturbed body image r/t chronic disease Ø Ineffective therapy regimen management r/t complexity of chronic health problem Ø Self-care deficit r/t disease progression Ø

Rheumatoid Arthritis Nursing Management Goals Satisfactory pain relief Ø Minimal loss of functional ability of affected joints Ø Patient participation in planning and carrying out therapeutic regimen Ø Positive-self image Ø Self-care to the maximum capability Ø
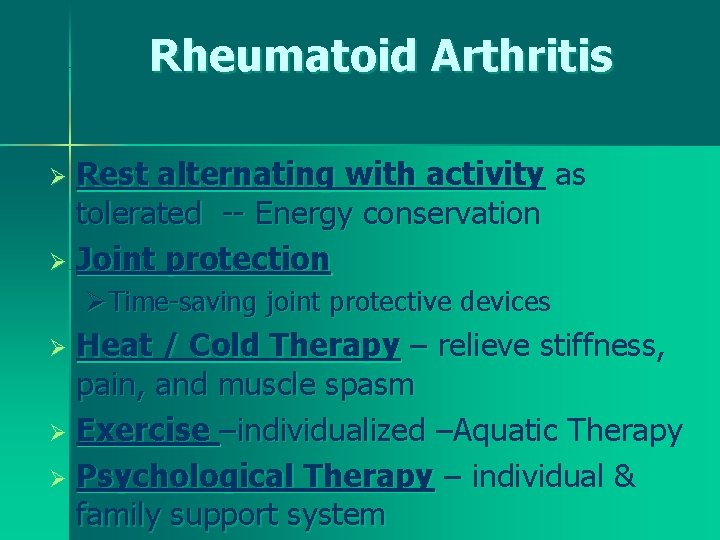
Rheumatoid Arthritis Rest alternating with activity as tolerated -- Energy conservation Ø Joint protection Ø ØTime-saving joint protective devices Heat / Cold Therapy – relieve stiffness, pain, and muscle spasm Ø Exercise –individualized –Aquatic Therapy Ø Psychological Therapy – individual & family support system Ø
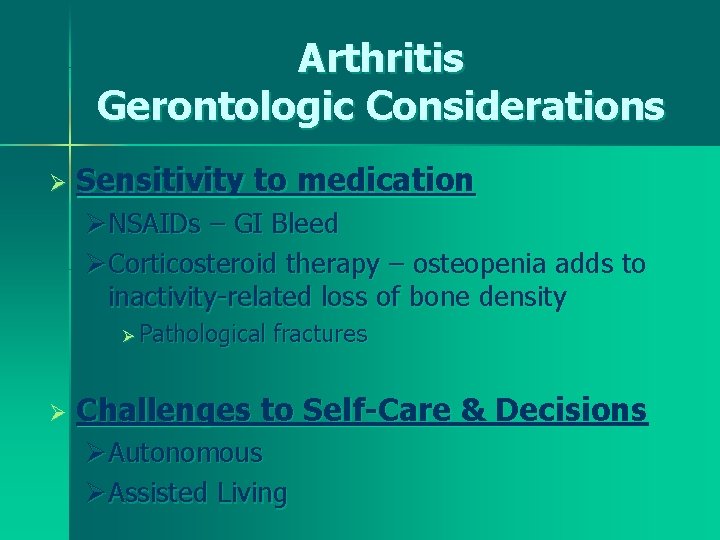
Arthritis Gerontologic Considerations Ø Sensitivity to medication ØNSAIDs – GI Bleed ØCorticosteroid therapy – osteopenia adds to inactivity-related loss of bone density Ø Pathological Ø fractures Challenges to Self-Care & Decisions ØAutonomous ØAssisted Living