Artery White blood cells Platelets Red blood cells
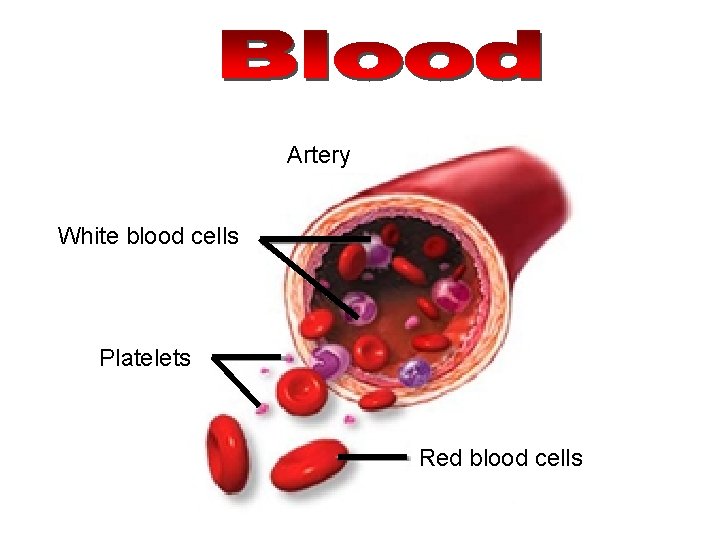
Artery White blood cells Platelets Red blood cells
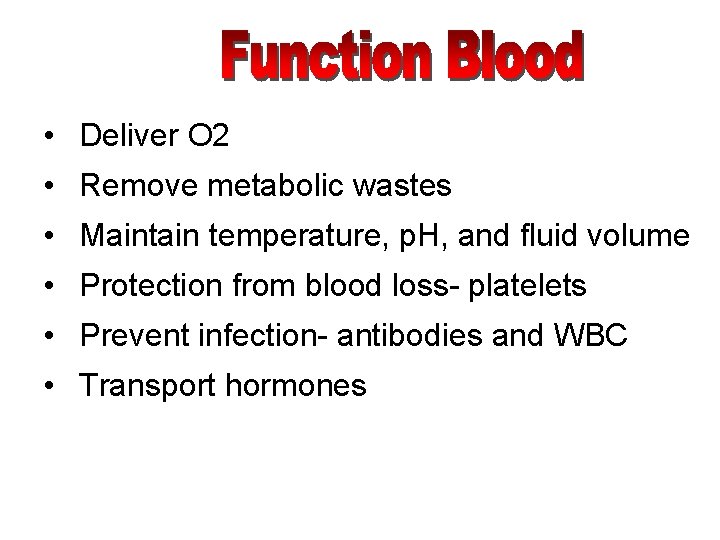
• Deliver O 2 • Remove metabolic wastes • Maintain temperature, p. H, and fluid volume • Protection from blood loss- platelets • Prevent infection- antibodies and WBC • Transport hormones
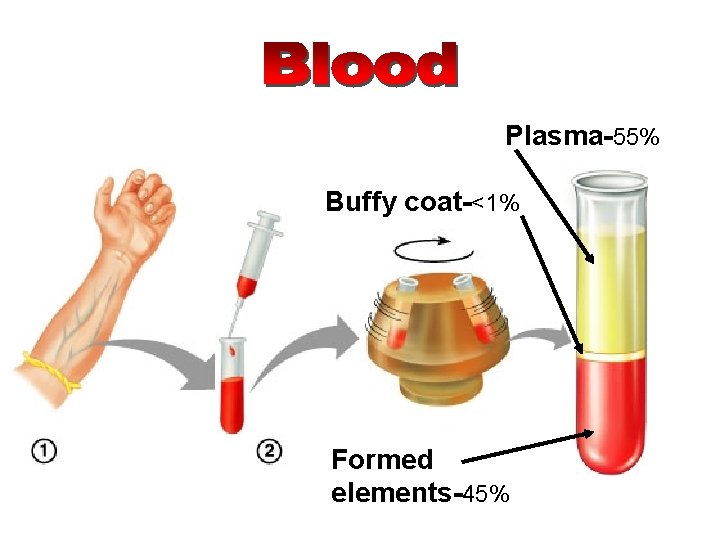
Plasma-55% Buffy coat-<1% Formed elements-45%
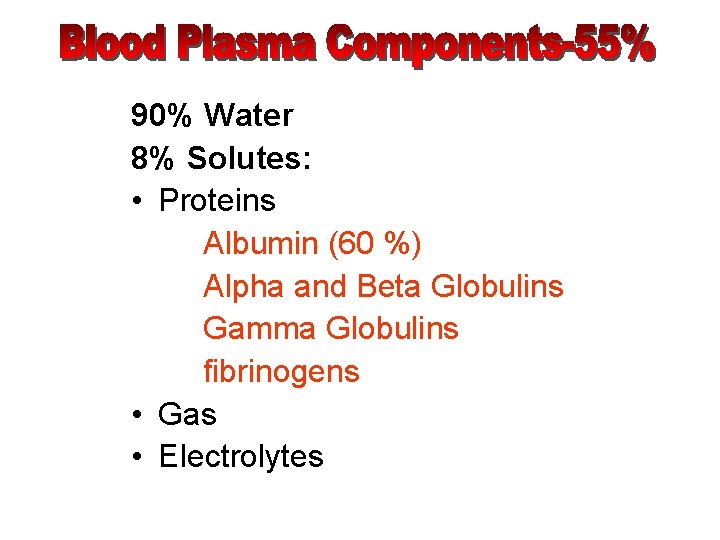
90% Water 8% Solutes: • Proteins Albumin (60 %) Alpha and Beta Globulins Gamma Globulins fibrinogens • Gas • Electrolytes
• Organic Nutrients Carbohydrates Amino Acids Lipids Vitamins • Hormones • Metabolic waste CO 2 Urea
• Leukocytes • Platelets
• Erythrocytes (red blood cells) • Leukocytes (white blood cells) • Platelets (thrombocytes)
Erythrocytes
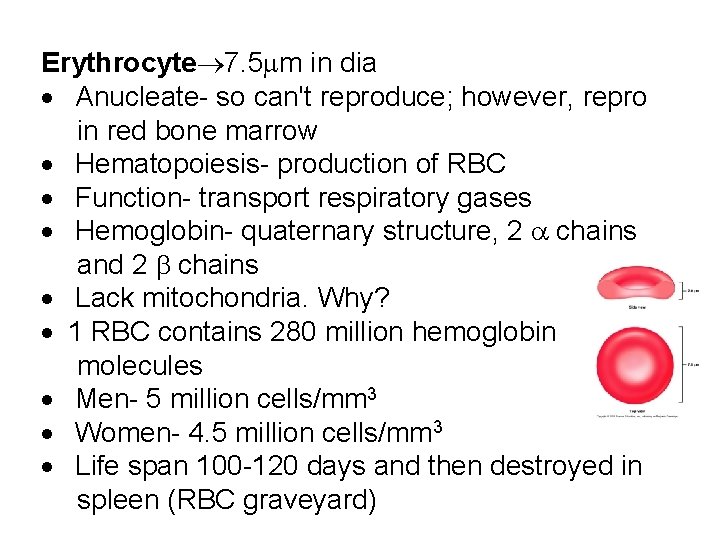
Erythrocyte 7. 5 m in dia · Anucleate- so can't reproduce; however, repro in red bone marrow · Hematopoiesis- production of RBC · Function- transport respiratory gases · Hemoglobin- quaternary structure, 2 chains and 2 chains · Lack mitochondria. Why? · 1 RBC contains 280 million hemoglobin molecules · Men- 5 million cells/mm 3 · Women- 4. 5 million cells/mm 3 · Life span 100 -120 days and then destroyed in spleen (RBC graveyard)
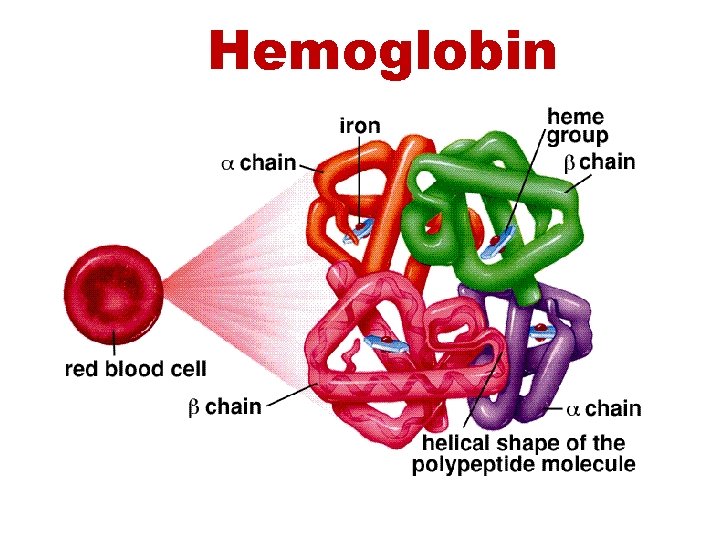
Hemoglobin
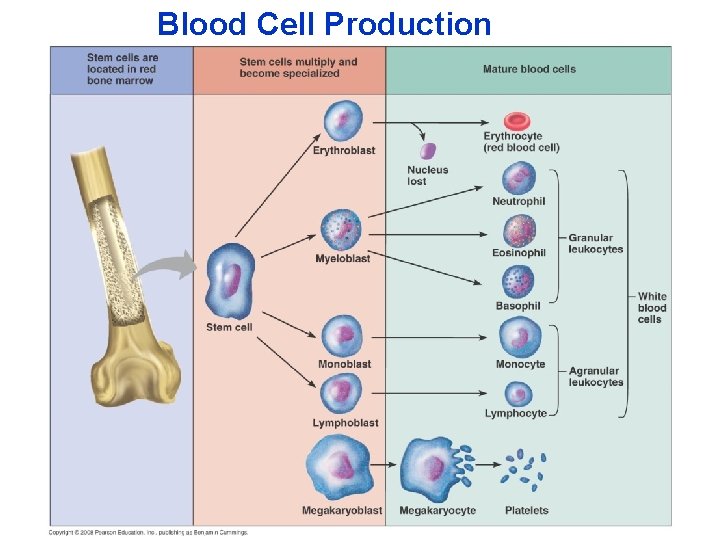
Blood Cell Production
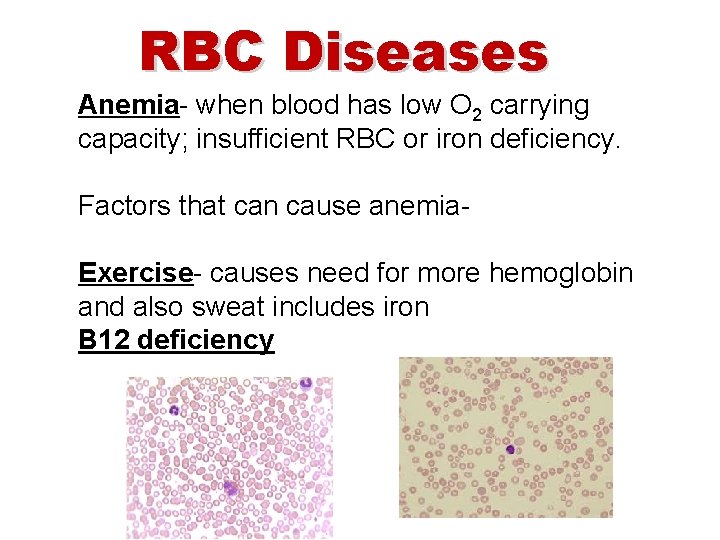
RBC Diseases Anemia- when blood has low O 2 carrying capacity; insufficient RBC or iron deficiency. Factors that can cause anemia. Exercise- causes need for more hemoglobin and also sweat includes iron B 12 deficiency
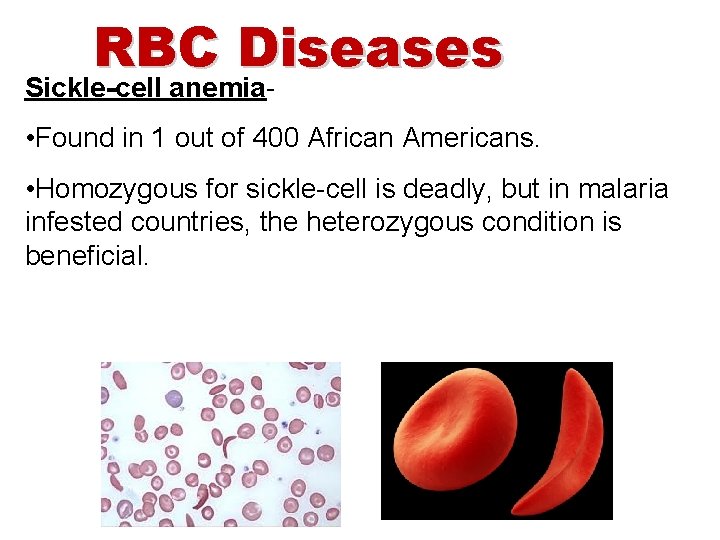
RBC Diseases Sickle-cell anemia- • Found in 1 out of 400 African Americans. • Homozygous for sickle-cell is deadly, but in malaria infested countries, the heterozygous condition is beneficial.
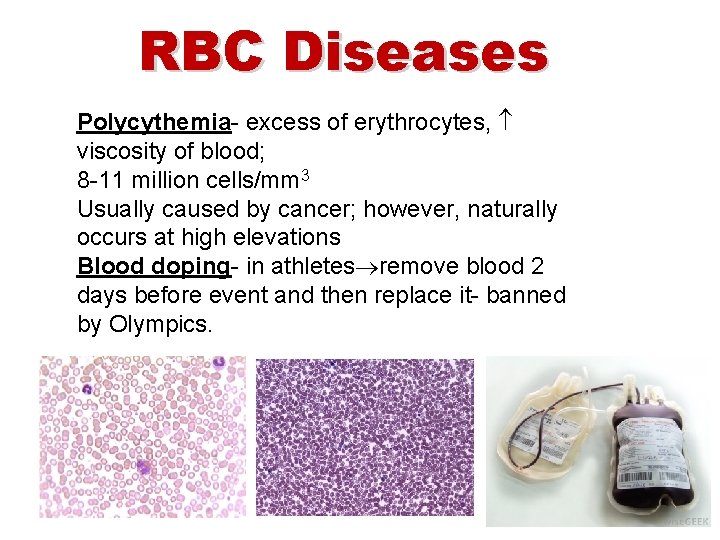
RBC Diseases Polycythemia- excess of erythrocytes, viscosity of blood; 8 -11 million cells/mm 3 Usually caused by cancer; however, naturally occurs at high elevations Blood doping- in athletes remove blood 2 days before event and then replace it- banned by Olympics.
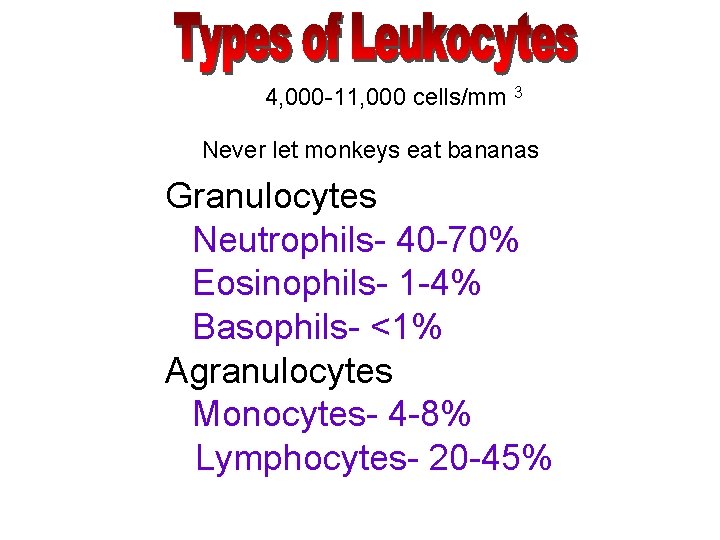
4, 000 -11, 000 cells/mm 3 Never let monkeys eat bananas Granulocytes Neutrophils- 40 -70% Eosinophils- 1 -4% Basophils- <1% Agranulocytes Monocytes- 4 -8% Lymphocytes- 20 -45%
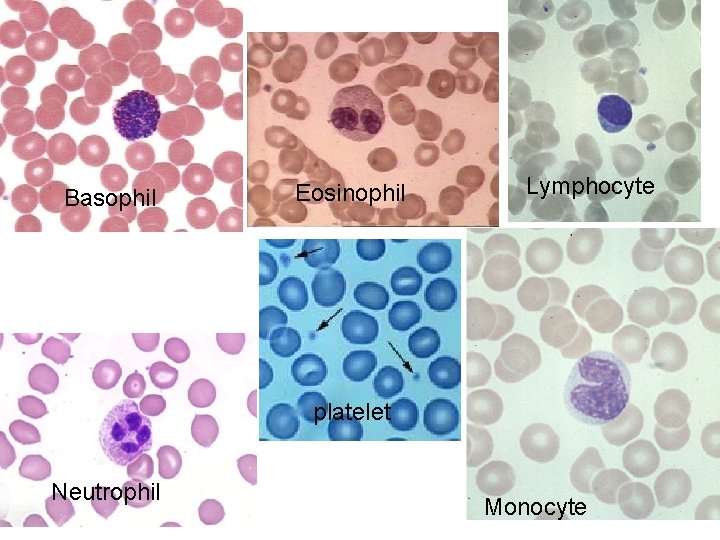
Basophil Eosinophil Lymphocyte platelet Neutrophil Monocyte
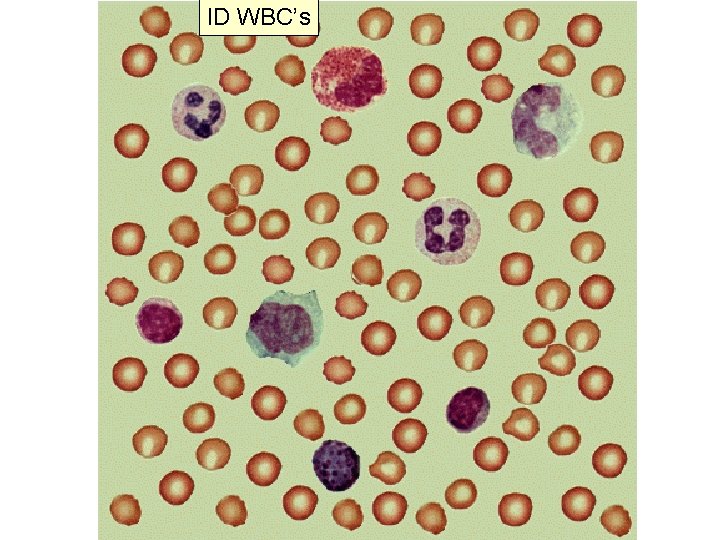
ID WBC’s
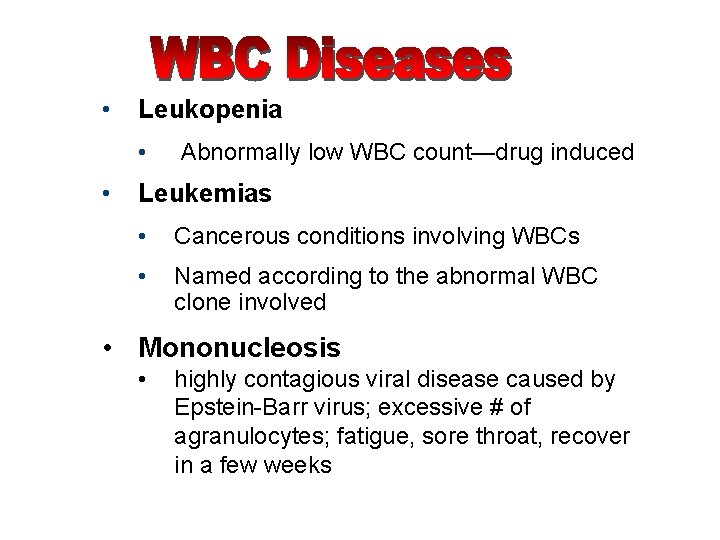
• Leukopenia • • Abnormally low WBC count—drug induced Leukemias • Cancerous conditions involving WBCs • Named according to the abnormal WBC clone involved • Mononucleosis • highly contagious viral disease caused by Epstein-Barr virus; excessive # of agranulocytes; fatigue, sore throat, recover in a few weeks
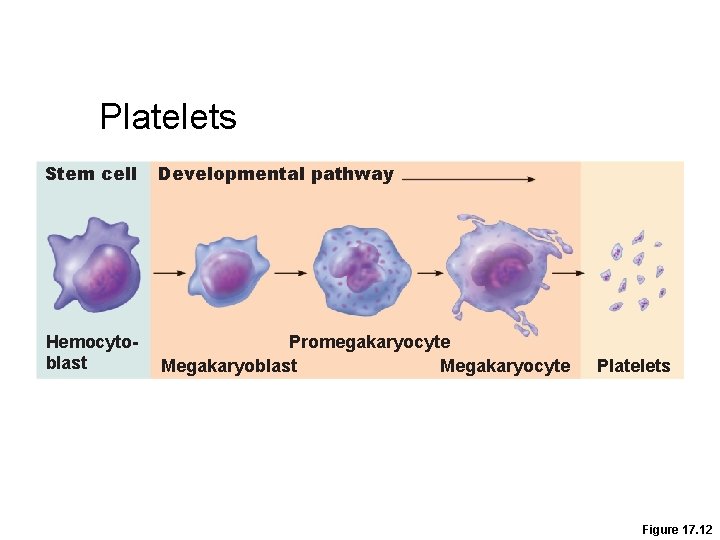
Platelets Stem cell Developmental pathway Hemocytoblast Promegakaryocyte Megakaryoblast Megakaryocyte Platelets Figure 17. 12
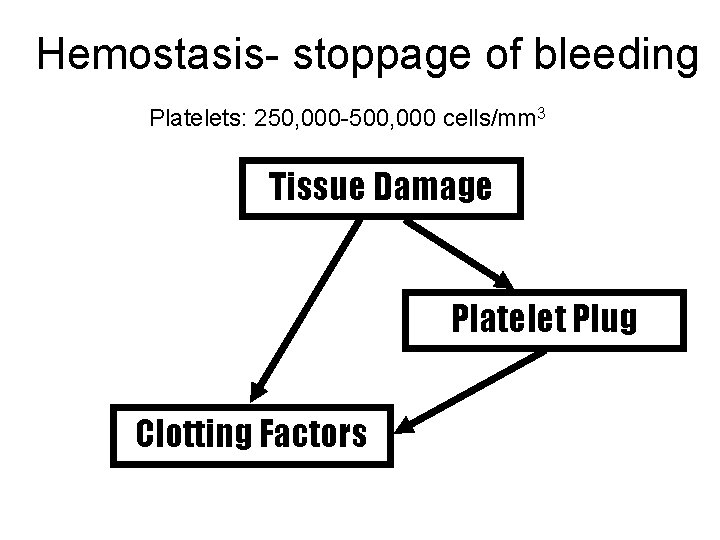
Hemostasis- stoppage of bleeding Platelets: 250, 000 -500, 000 cells/mm 3 Tissue Damage Platelet Plug Clotting Factors
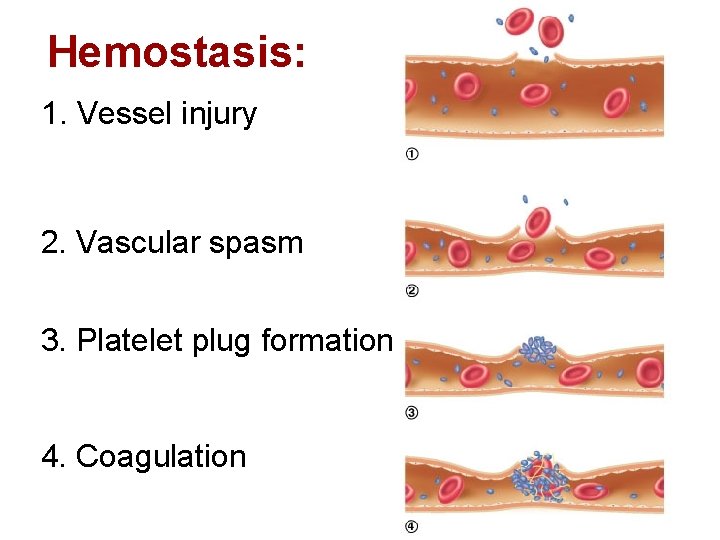
Hemostasis: 1. Vessel injury 2. Vascular spasm 3. Platelet plug formation 4. Coagulation
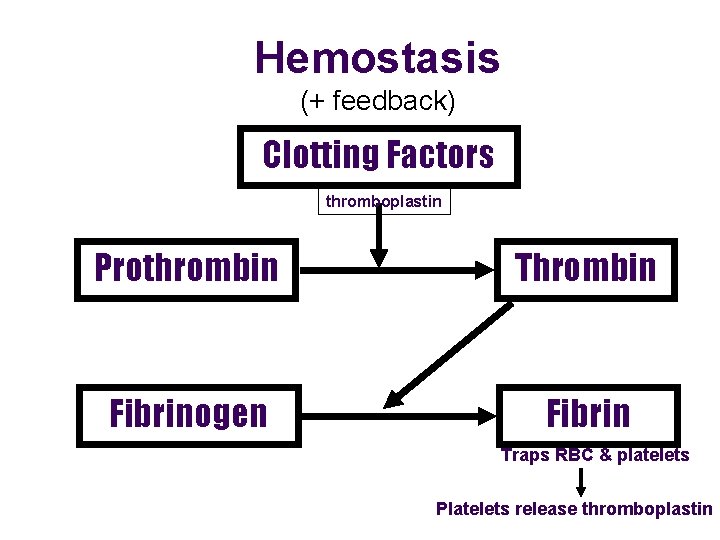
Hemostasis (+ feedback) Clotting Factors thromboplastin Prothrombin Thrombin Fibrinogen Fibrin Traps RBC & platelets Platelets release thromboplastin
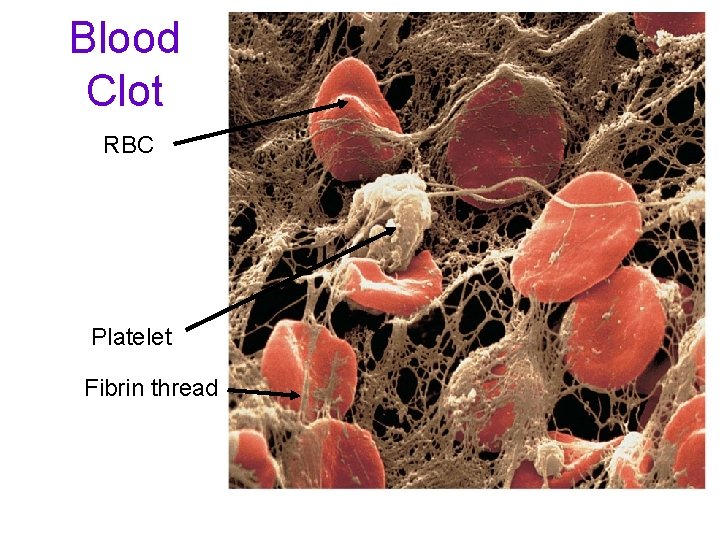
Blood Clot RBC Platelet Fibrin thread
Disorders of Hemostasis • Thromboembolytic disorders: undesirable clot formation • Bleeding disorders: abnormalities that prevent normal clot formation
Thromboembolytic Conditions • Thrombus: clot that develops and persists in an unbroken blood vessel – May block circulation, leading to tissue death • Embolus: a thrombus freely floating in the blood stream – Pulmonary emboli impair the ability of the body to obtain oxygen – Cerebral emboli can cause strokes
Thromboembolytic Conditions • Prevented by – Aspirin • Antiprostaglandin that inhibits thromboxane A 2 – Heparin • Anticoagulant used clinically for pre- and postoperative cardiac care
Thrombocytosis- too many platelets due to inflammation, infection or cancer Thrombocytopenia- too few platelets • causes spontaneous bleeding • due to suppression or destruction of bone marrow (e. g. , malignancy, radiation) – Platelet count <50, 000/mm 3 is diagnostic – Treated with transfusion of concentrated platelets
• Impaired liver function – Inability to synthesize procoagulants – Causes include vitamin K deficiency, hepatitis, and cirrhosis – Liver disease can also prevent the liver from producing bile, impairing fat and vitamin K absorption
• Hemophilias include several similar hereditary bleeding disorders • Symptoms include prolonged bleeding, especially into joint cavities • Treated with plasma transfusions and injection of missing factors
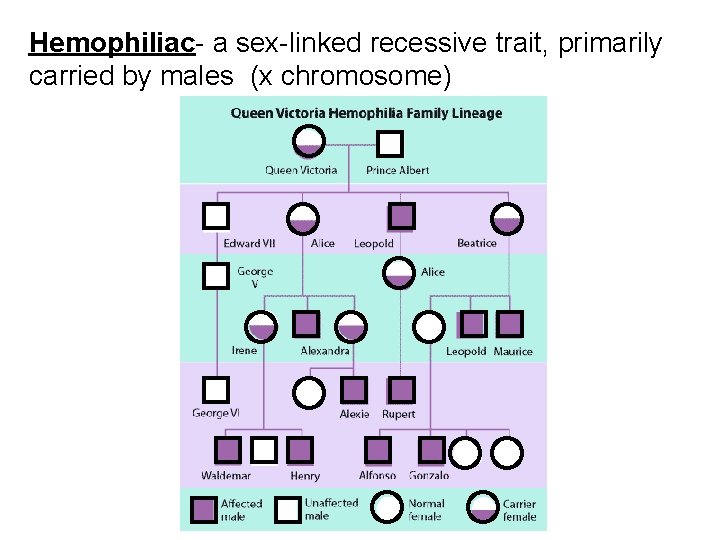
Hemophiliac- a sex-linked recessive trait, primarily carried by males (x chromosome)
Type A Type B Type AB Type O
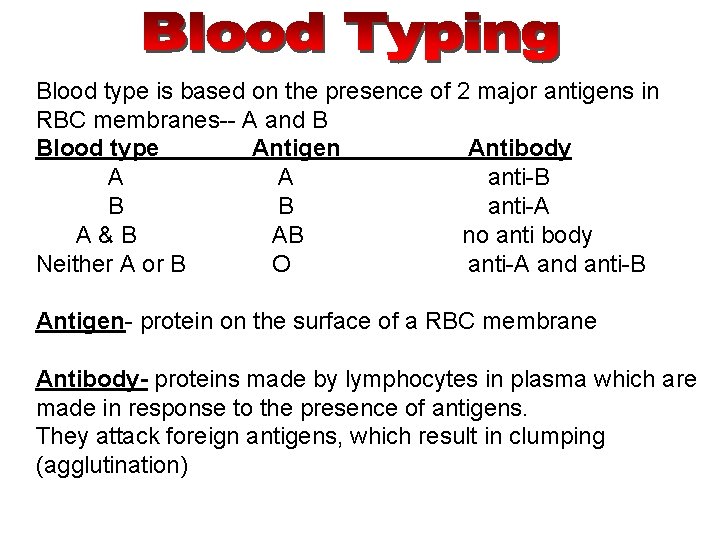
Blood type is based on the presence of 2 major antigens in RBC membranes-- A and B Blood type Antigen Antibody A A anti-B B B anti-A A&B AB no anti body Neither A or B O anti-A and anti-B Antigen- protein on the surface of a RBC membrane Antibody- proteins made by lymphocytes in plasma which are made in response to the presence of antigens. They attack foreign antigens, which result in clumping (agglutination)
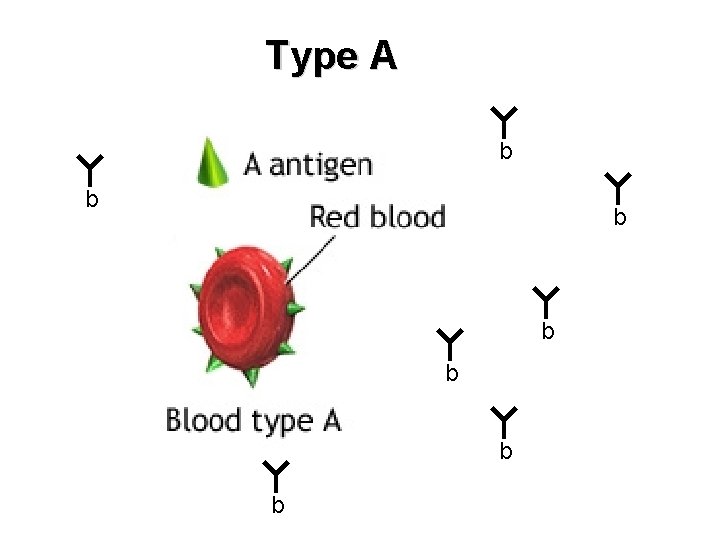
Type A b b b b
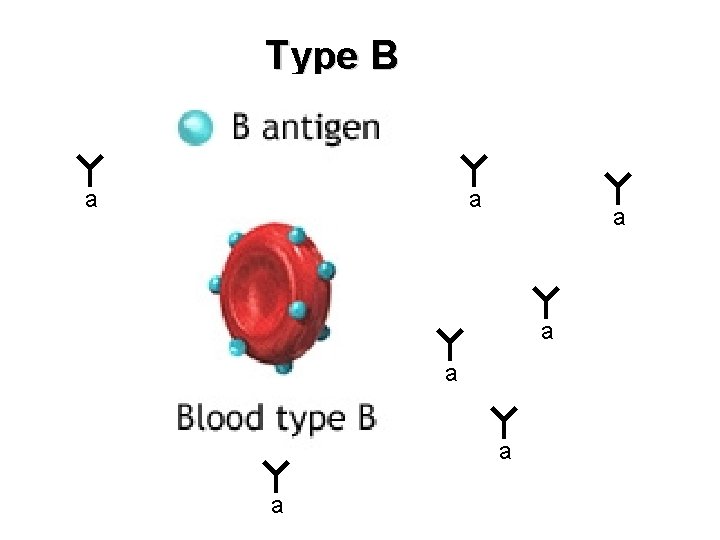
Type B a a a a
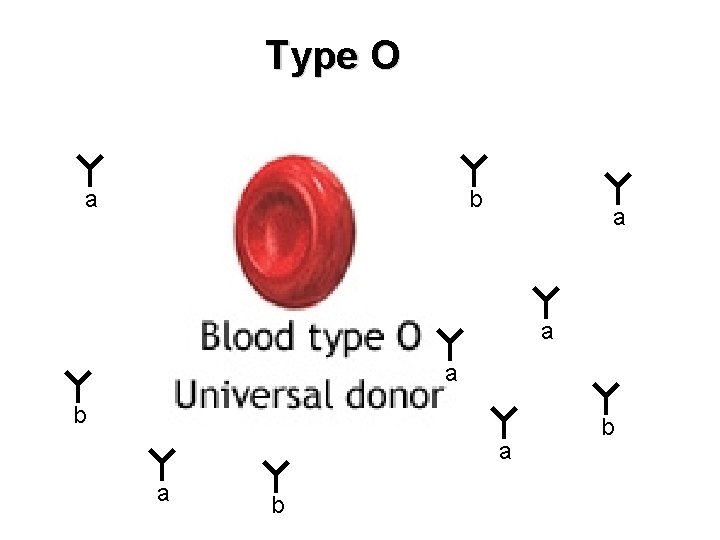
Type O a b a a b b
Type AB
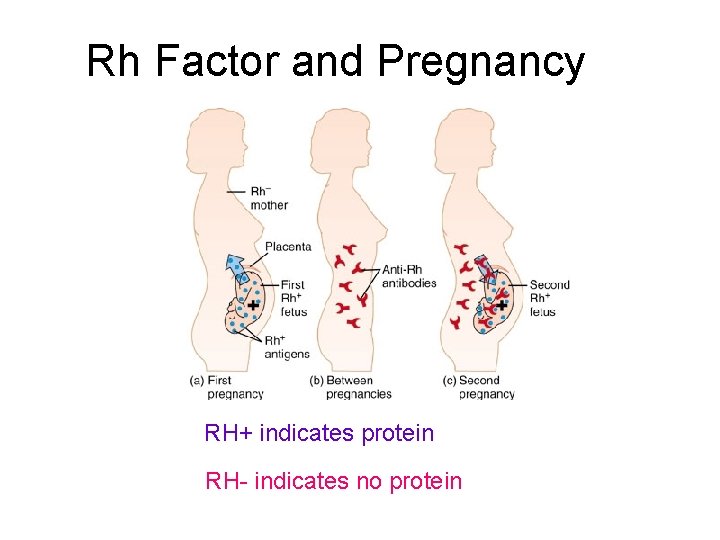
Rh Factor and Pregnancy RH+ indicates protein RH- indicates no protein
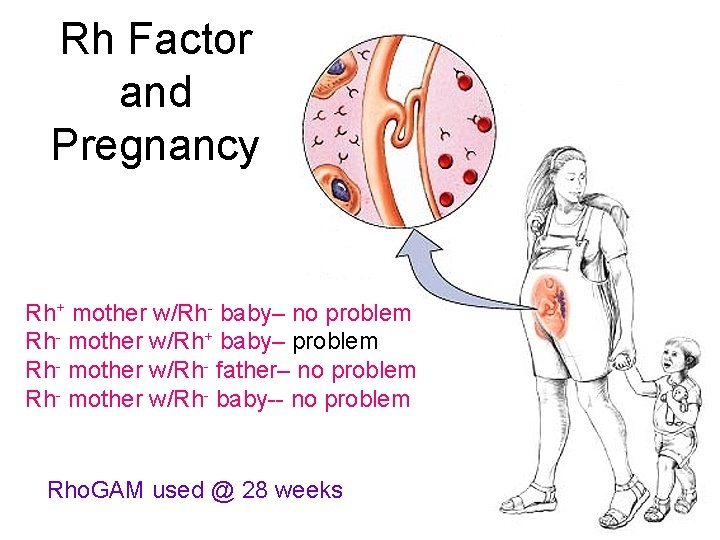
Rh Factor and Pregnancy Rh+ mother w/Rh- baby– no problem Rh- mother w/Rh+ baby– problem Rh- mother w/Rh- father– no problem Rh- mother w/Rh- baby-- no problem Rho. GAM used @ 28 weeks
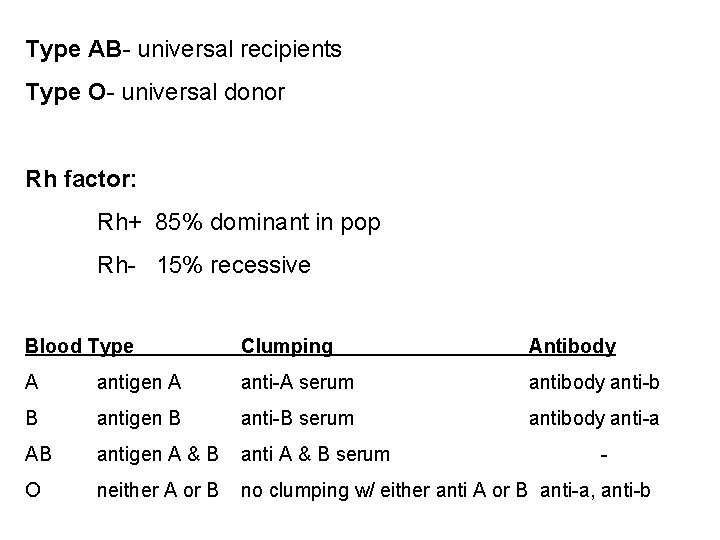
Type AB- universal recipients Type O- universal donor Rh factor: Rh+ 85% dominant in pop Rh- 15% recessive Blood Type Clumping Antibody A antigen A anti-A serum antibody anti-b B antigen B anti-B serum antibody anti-a AB antigen A & B anti A & B serum O neither A or B no clumping w/ either anti A or B anti-a, anti-b -
Blood Type & Rh How Many Have It O O A A B B AB AB 1 person in 3 1 person in 15 1 person in 3 1 person in 16 1 person in 12 1 person in 67 1 person in 29 1 person in 167 Rh Positive Rh Negative Frequency 37. 4% 6. 6% 35. 7% 6. 3% 8. 5% 1. 5% 3. 4%. 6%
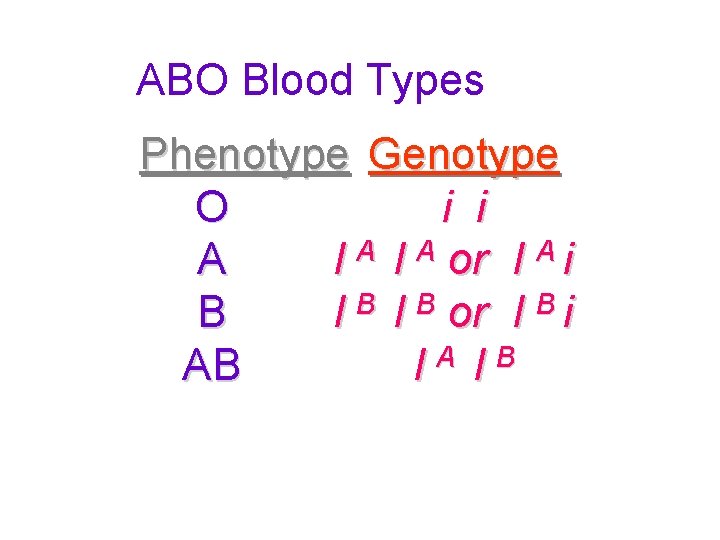
ABO Blood Types Phenotype Genotype O i i A I A or I A i B I B or I B i AB IA IB
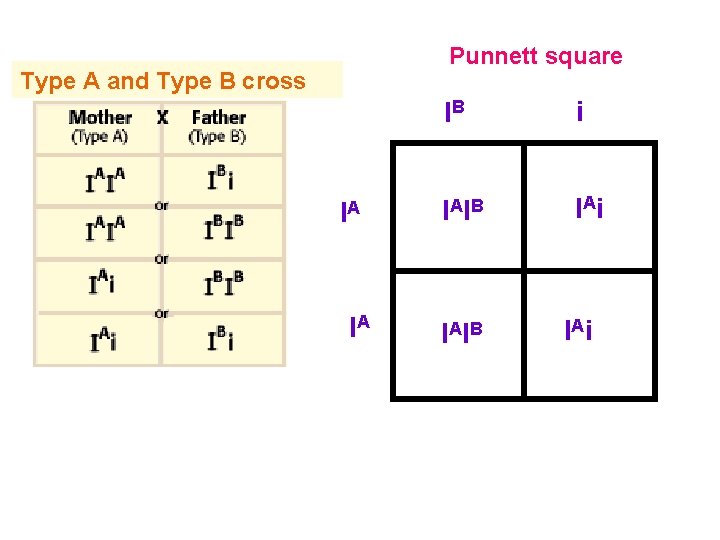
Punnett square Type A and Type B cross IA IA IB i I AI B I Ai
Bozeman Video - Blood Types http: //www. youtube. com/watch? v=K XTF 7 Wehg. M 8
- Slides: 44