Arterial and venous blood pressures Arterial Blood Pressure
Arterial and venous blood pressures
Arterial Blood Pressure (BP) = The lateral pressure force generated by the pumping action of the heart on the wall of aorta & arterial blood vessels per unit area. OR = Pressure inside big arteries (aorta & big vessels). ■ Measured in (mm. Hg), & sometimes in (cm. H 2 O), where 1 mm. Hg = 1. 36 cm. H 2 O. ■ Of 2 components: l l systolic … (= max press reached) diastolic … (= min press reached)
Arterial Blood Pressure (continued) In normal adult 120/80 mm. Hg. ■ Diastolic pressure is more important, because diastolic period is longer than the systolic period in the cardiac cycle. ■ Pulse pressure = Systolic BP – Diastolic BP. ■ Mean arterial pressure = Diastolic BP + 1/3 Pulse press.
Factors affecting ABP: ■ Sex … M > F …due to hormones/ equal at menopause. ■ Age … Elderly > children …due to atherosclerosis. ■ Emotions … due to secretion of adrenaline & noradrenaline. ■ Exercise … due to venous return. ■ Hormones … (e. g. Adrenaline, noradrenaline, thyroid H). ■ Gravity … Lower limbs > upper limbs. ■ Race … Orientals > Westerns … ? dietry factors, or weather. ■ Sleep … due to venous return. ■ Pregnancy … due to metabolism.
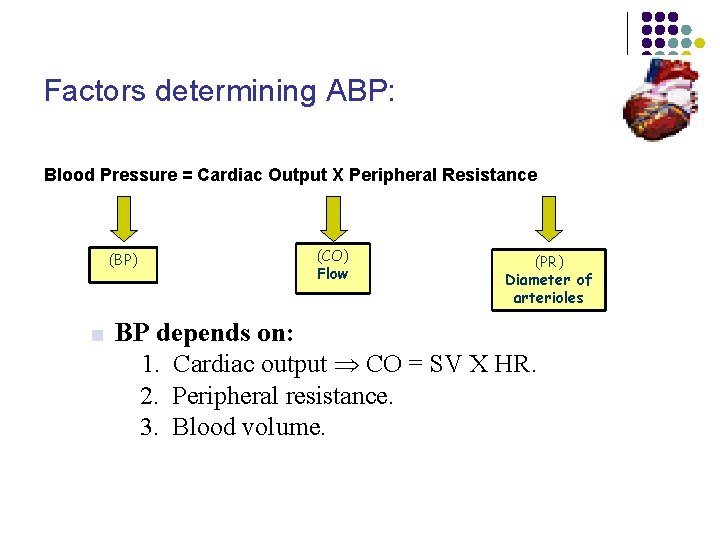
Factors determining ABP: Blood Pressure = Cardiac Output X Peripheral Resistance (CO) Flow (BP) ■ BP depends on: (PR) Diameter of arterioles 1. Cardiac output CO = SV X HR. 2. Peripheral resistance. 3. Blood volume.
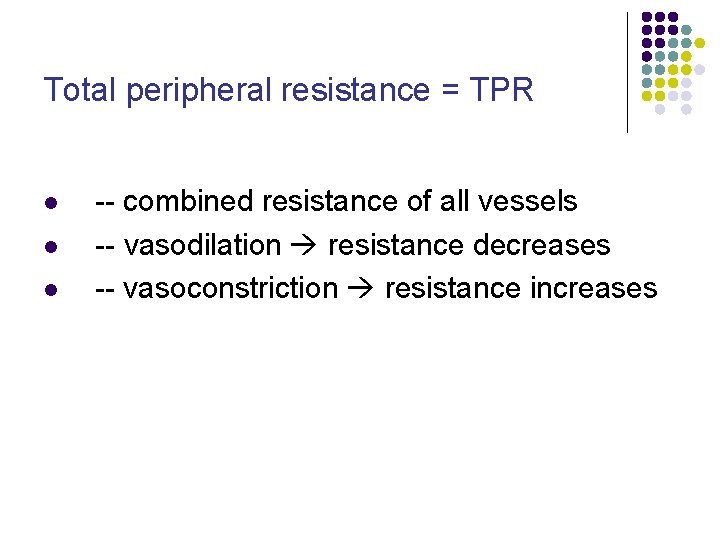
Total peripheral resistance = TPR l l l -- combined resistance of all vessels -- vasodilation resistance decreases -- vasoconstriction resistance increases
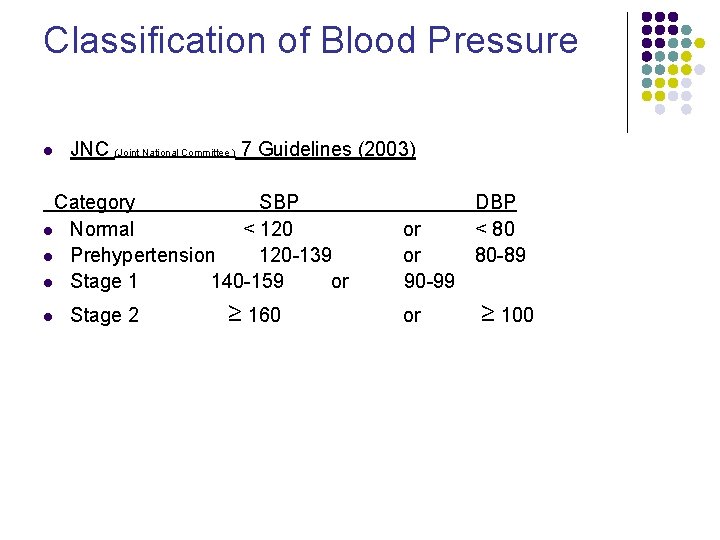
Classification of Blood Pressure l JNC (Joint National Committee ) 7 Guidelines (2003) Category SBP l Normal < 120 l Prehypertension 120 -139 l Stage 1 140 -159 or l Stage 2 ≥ 160 or or 90 -99 or DBP < 80 80 -89 ≥ 100
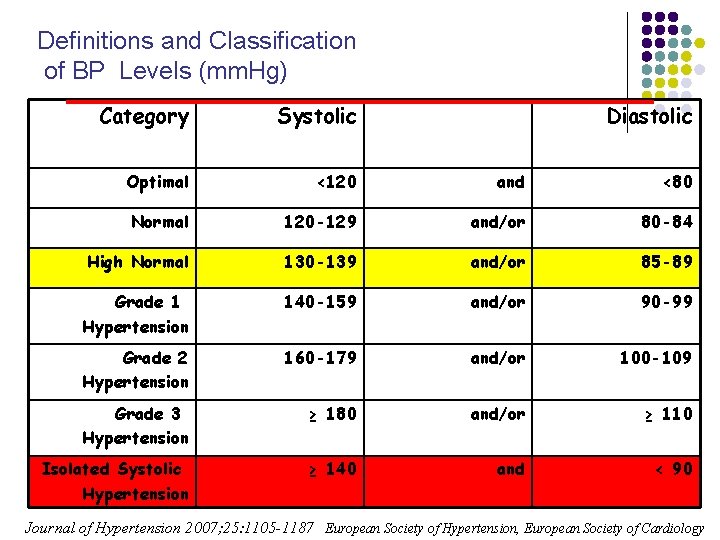
Definitions and Classification of BP Levels (mm. Hg) Category Systolic Diastolic Optimal <120 and <80 Normal 120 -129 and/or 80 -84 High Normal 130 -139 and/or 85 -89 Grade 1 Hypertension 140 -159 and/or 90 -99 Grade 2 Hypertension 160 -179 and/or 100 -109 Grade 3 Hypertension ≥ 180 and/or ≥ 110 Isolated Systolic Hypertension ≥ 140 and < 90 Journal of Hypertension 2007; 25: 1105 -1187 European Society of Hypertension, European Society of Cardiology
l Hypertension with no known cause (primary, formerly, essential hypertension) is most common. l Hypertension with an identified cause (secondary hypertension) is usually due to a renal disorder. l Usually, no symptoms develop unless hypertension is severe or long-standing.
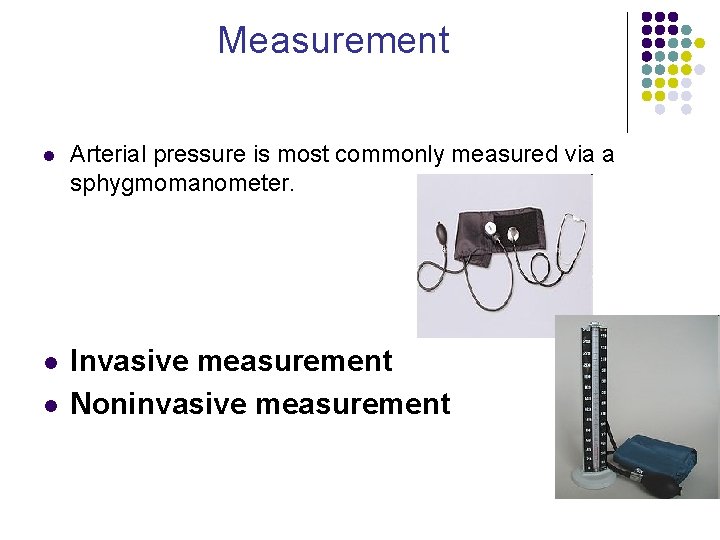
Measurement l Arterial pressure is most commonly measured via a sphygmomanometer. l Invasive measurement Noninvasive measurement l
Invasive measurement l Arterial blood pressure (BP) is most accurately measured invasively through an arterial line. l Invasive arterial pressure measurement with intravascular cannulae involves direct measurement of arterial pressure by placing a cannula needle in an artery (usually radial , femoral , dorsalis pedis or brachial)
Noninvasive measurement l l Palpation method Auscultatory method
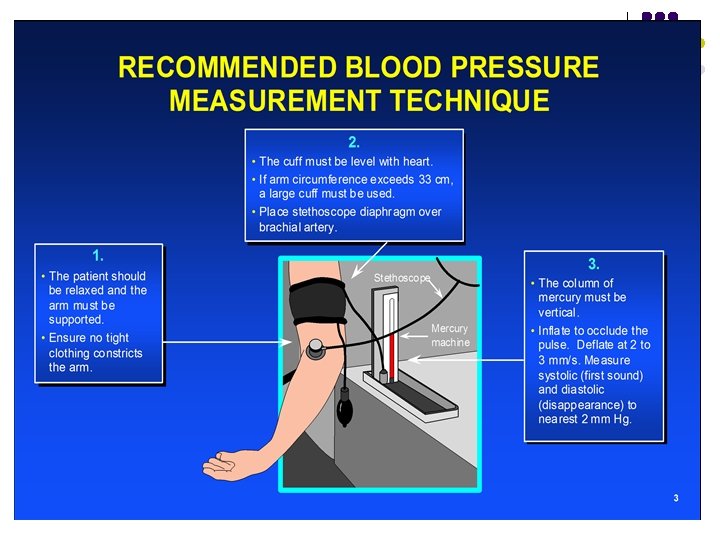
l l l Is your patient ready? If your patient has finished a cigarette or an alcoholic beverage within the last 15 minutes the readings will be altered. If they haven’t sat quietly for at least 5 minutes or are talking during the procedure, the readings will be altered. Systolic and diastolic BP's in hypertensive and normotensive patients increase with talking And if you have placed the cuff over a shirt sleeve the readings will not be reliable.
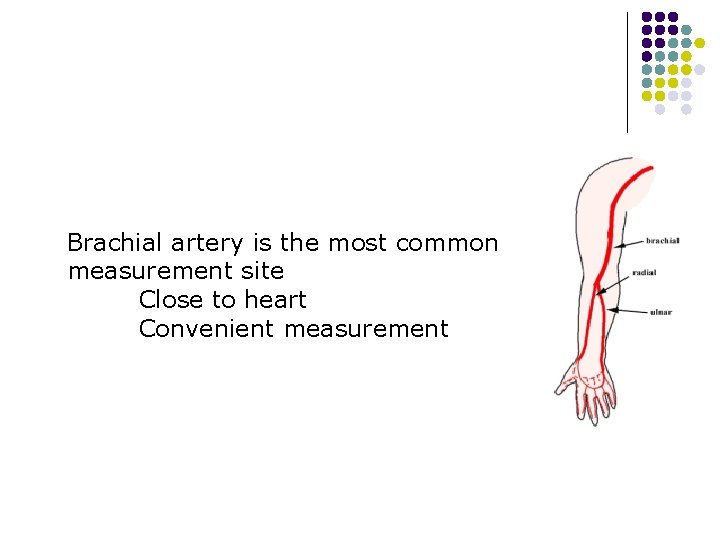
Brachial artery is the most common measurement site Close to heart Convenient measurement
1. Use appropriate size BP cuff l l Is the cuff you are using sized for the patient? A cuff too large can cause reading to be lower than actual and a cuff too small can cause reading to be higher than actual. Cuff sizes are: Small Adult 17 -25 cm/Standard Adult 2333 cm/Large Adult 31 -40 cm/Thigh 38 -50 cm.
l 2. Position patient Patient should be seated with back and arms supported, feet on floor, and legs uncrossed with upper arm at heart level
3. Measure baseline BP bilaterally
l l Cuff applied 1 inch above crease at elbow Locate brachial artery Palpate radial pulse Inflate cuff until pulse disappears
Palpation method l l l The blood pressure can be measured in noisy environment Only the systolic pressure can be measured (not DP) The technique does not give accurate results for infants and hypotensive patients
Auscultatory method l l l Pulse waves that propagate through the brachial artery, generate Korotkoff sounds. There are 5 distinct phases in the Korotkoff sounds, which define SP and DP The Korotkoff sounds are ausculted with a stethoscope
Korotkoff sounds l First Phase l l Second Phase l l A clear tapping sound; onset of the sound for two consecutive beats is considered systolic The tapping sound followed by a murmur Third Phase l A loud crisp tapping sound
l Fourth Phase l l Abrupt, distinct muffling of sound, gradually decreasing in intensity Fifth Phase l The disappearance of sound, is considered diastolic blood pressure- two points below the last sound heard
Venous Pressure
Venous Pressure l Venous Pressure generally refers to the average pressure within venous compartment of circulation l Blood from all the systemic veins flows into the right atrium of the heart, therefore the pressure in the Rt atrium called Central Venous pressure
How to measure the CVP ? ? v Direct: by catheter introduced into large thoracic veins v Indirect: pressure Is estimated from Jugular venous
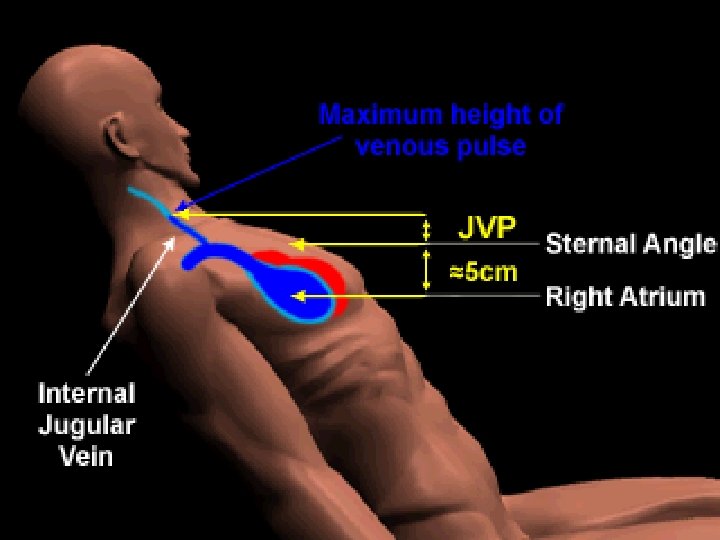
Jugular Venous Pulse (JVP) There is no valves between the Rt atrium and the Internal Jugular Vein. So the degree of distension of this vein is dictated by the Rt atrium pressure. l Pressure changes transmitted from right atrium l The right internal jugular is the best neck vein to inspect l Provides information about hemodynamic changes in right atrium & ventricle l
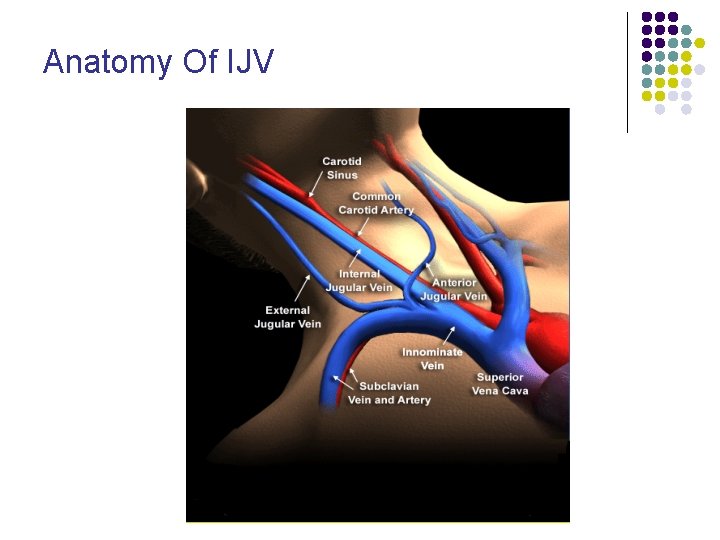
Anatomy Of IJV
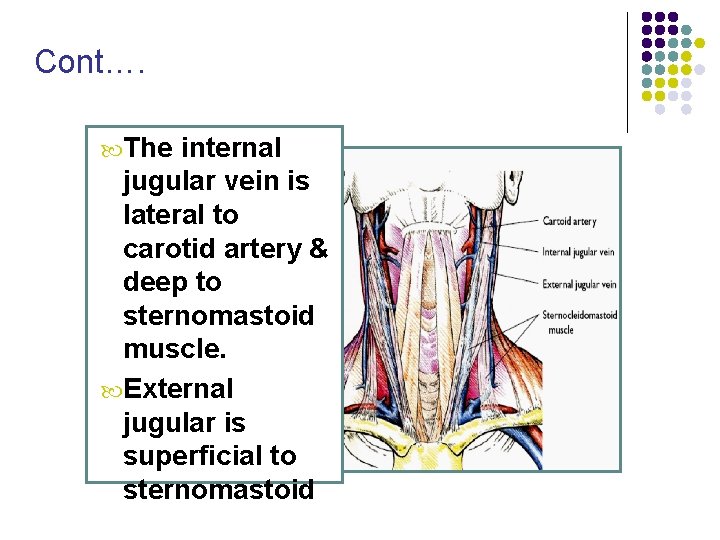
Cont…. The internal jugular vein is lateral to carotid artery & deep to sternomastoid muscle. External jugular is superficial to sternomastoid
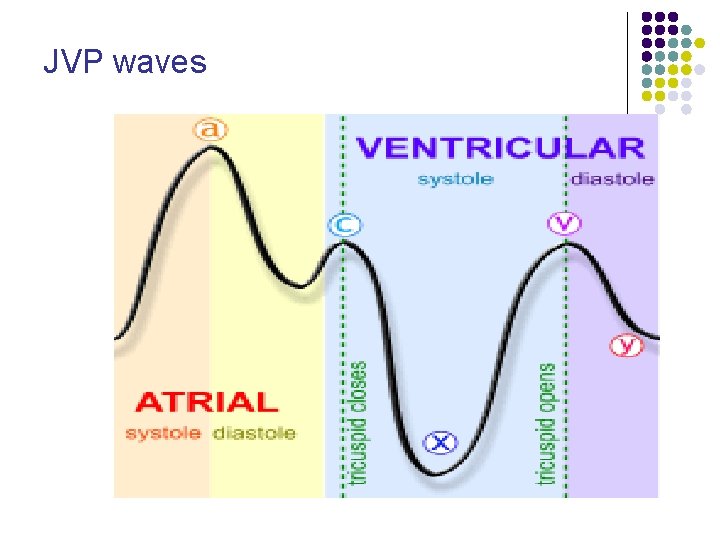
JVP waves
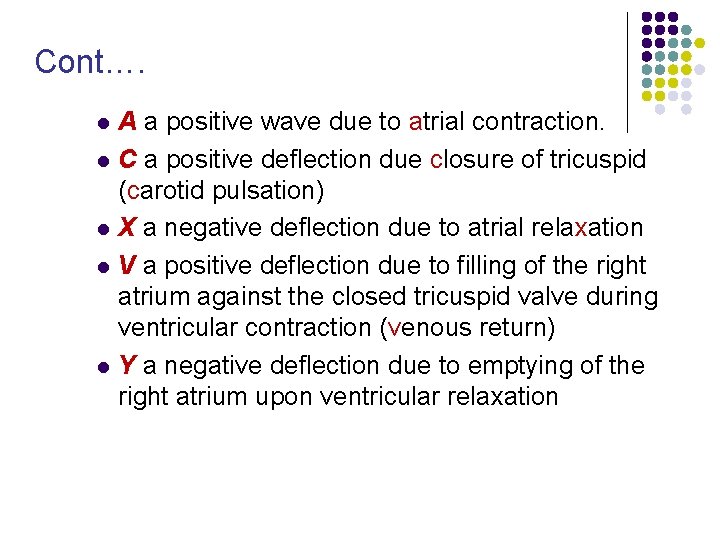
Cont…. l l l A a positive wave due to atrial contraction. C a positive deflection due closure of tricuspid (carotid pulsation) X a negative deflection due to atrial relaxation V a positive deflection due to filling of the right atrium against the closed tricuspid valve during ventricular contraction (venous return) Y a negative deflection due to emptying of the right atrium upon ventricular relaxation
Abnormalities of wave l Prominent ‘a’ wave : Right atrial and right ventricular hypertrophy (due to P. HTN or P. stenosis) Tricuspid stenosis. l Cannon wave: Large ‘a’ wave produce when Rt atrium contract against closed tricuspid valve. This seen in complete heart block
Cont… l Kussmaul sign: A paradoxical rise of JVP on inspiration. Causes: Constrictive pericarditis Cardiac tamponade Sever Rt ventricular failure
Difference between arterial and venous pulsation in neck l Change in posture ? l Change in respiration ? l Abdomino-jugular reflux ? l Pulsation pattern ? l Palpation ? l Occlusion ?
How measure JVP ? LOOK v CONFIRM v. MEASURE v
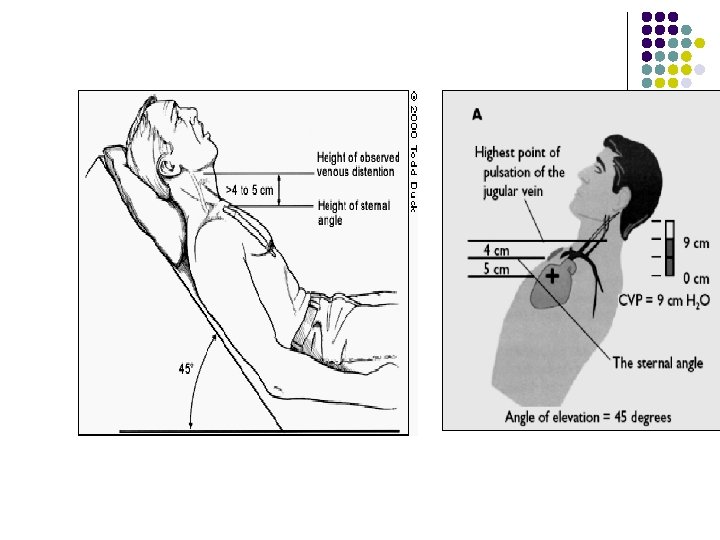
Method l Position 45 degree l Rest the pt head on pillow to ensure neck muscle relax, and slightly tilted toward the left side. l look acorss the neck from the Rt side of the pt. l Identify the Jugular vein l Confirm the pulse.
Cont. . l Identify the upper limit of venous pulsation l JVP is measured by two pencils method l Place one pencil at sternal angle vertical to ground & other pencil at upper limit of venous pulsation horizontal to the ground l Measure length of the verticbal pencil in cm btw the sternal angle & where it is crossed by the horizontal pencil. l Normal JVP up to 3 cm
Causes of raised JVP Right heart failure Constrictive pericarditis Superior vena cava obstruction Pericardial effusion Cardiac tamponade Tricuspid valve disease
Cardiac tamponade l l l Cardiac tamponade: the accumulation of fluid in the pericardium in an amount sufficient to cause serious obstruction to the inflow of blood to ventricle results in cardiac tamponade. The three principal features of tamponade are: 1. elevation of intracardiac pressures 2. limitation of ventricular fillng 3. reduction of cardiac output
Beck triad: 1. increased jugular venous pressure 2. hypotension 3. diminished heart sounds
Thank you
- Slides: 45