ARRHYTHMIAS IN ACUTE MYOCARDIAL INFARCTION CCU MANAGEMENT K


- Slides: 61
ARRHYTHMIAS IN ACUTE MYOCARDIAL INFARCTION CCU MANAGEMENT K. U. Natarajan, AIMS Kochi
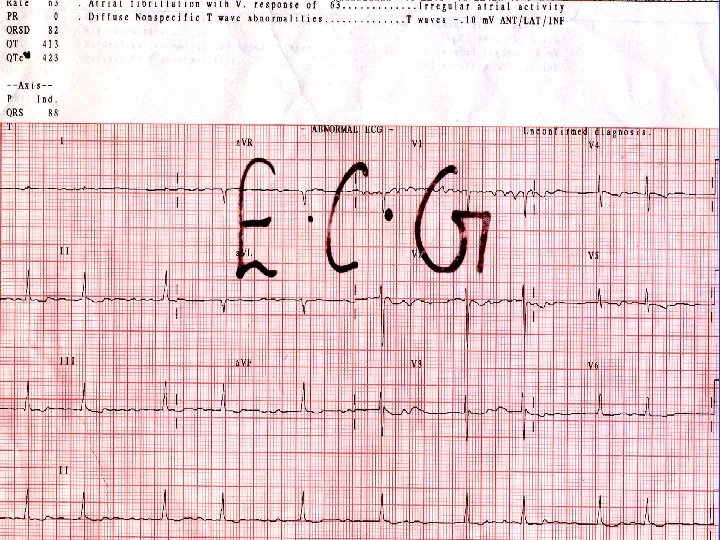
# Most of the time # Treating a cardiac arrhythmia # Is based on SIMPLE & LOGICAL THINKING An example ………
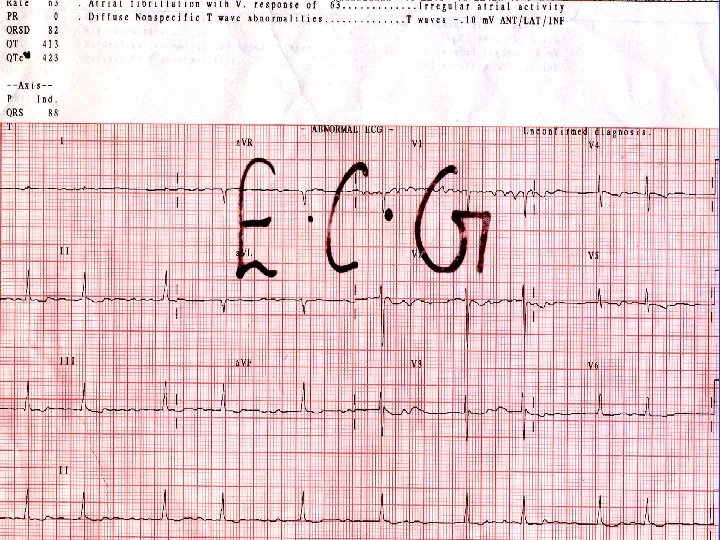
32 year old female RHD , severe MR, AF Underwent MVR
8 th post OP day On Dopamine 7. 5 mcg/Kg/min Dobutamine 7. 5 mcg/Kg/min Adrenaline infusion BP 85/45 Not able to wean off supports – persistent hypotension
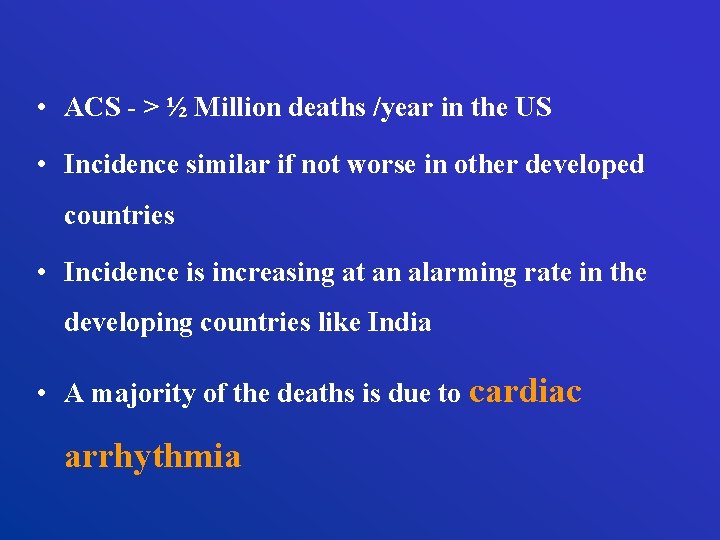
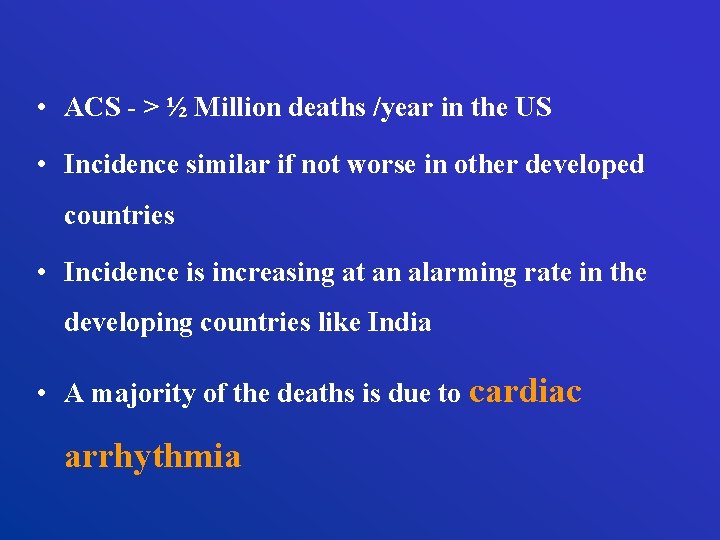
• ACS - > ½ Million deaths /year in the US • Incidence similar if not worse in other developed countries • Incidence is increasing at an alarming rate in the developing countries like India • A majority of the deaths is due to cardiac arrhythmia
The CCU • An innovation to improve survival following AMI • Advances in detection & treatment of arrhythmias introduced in 1950 s • Set the stage for invention of the CCU concept in early 1960 s
The CCU • New technologies gave us the power to treat life threatening arrhythmias • “Monitor”, “Defibrillator” & “Pacemaker”
A tribute to the masters… • Middle of the 20 th century • Several teams of researchers • Electrical Engineers Cardiologists Physiologists Surgeons Made discoveries & inventions that lead to the introduction of defibrillator & pacemaker
A tribute to the masters… • 1947 – Claude Beck – Heart surgeon – 1 st human resuscitation using defibrillator • Delivered the shock directly to the heart after opening the chest • 1956 – Paul Zoll – cardiologist from Boston • Successful delivery of shock through the chest wall
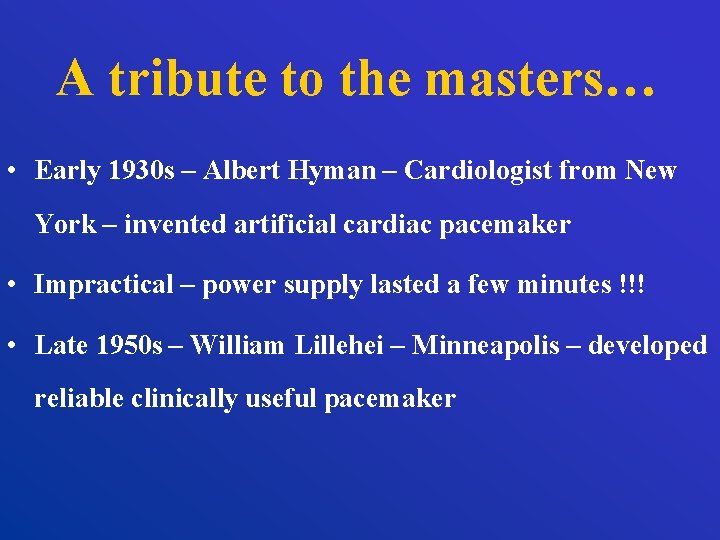
A tribute to the masters… • Early 1930 s – Albert Hyman – Cardiologist from New York – invented artificial cardiac pacemaker • Impractical – power supply lasted a few minutes !!! • Late 1950 s – William Lillehei – Minneapolis – developed reliable clinically useful pacemaker
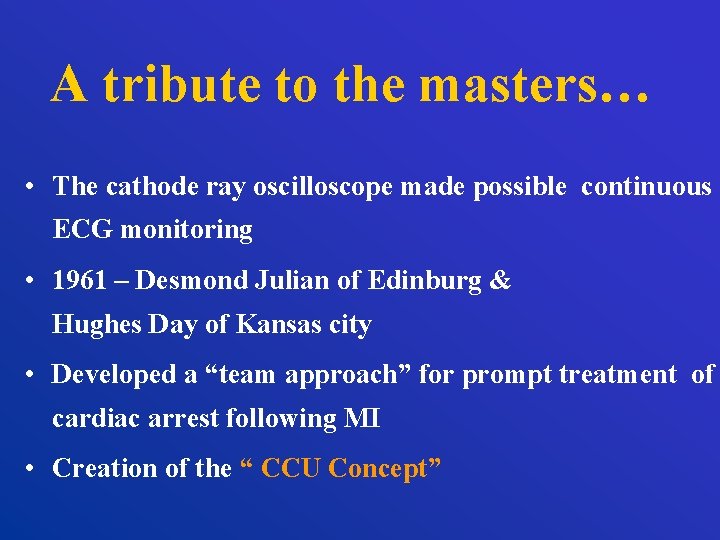
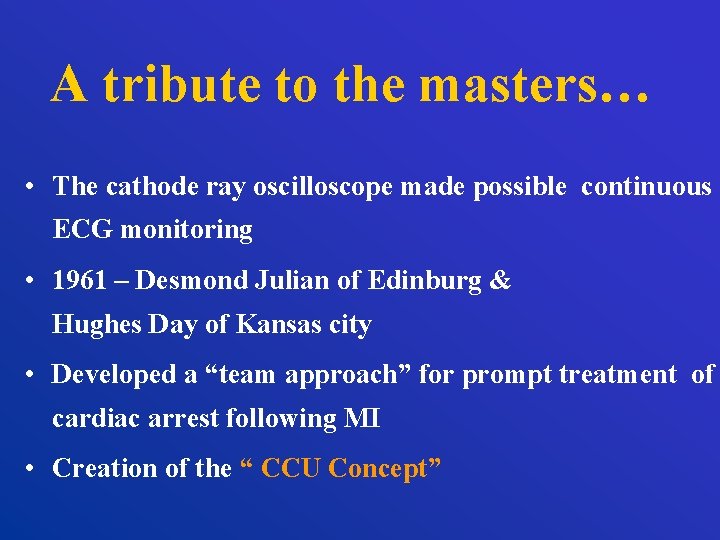
A tribute to the masters… • The cathode ray oscilloscope made possible continuous ECG monitoring • 1961 – Desmond Julian of Edinburg & Hughes Day of Kansas city • Developed a “team approach” for prompt treatment of cardiac arrest following MI • Creation of the “ CCU Concept”
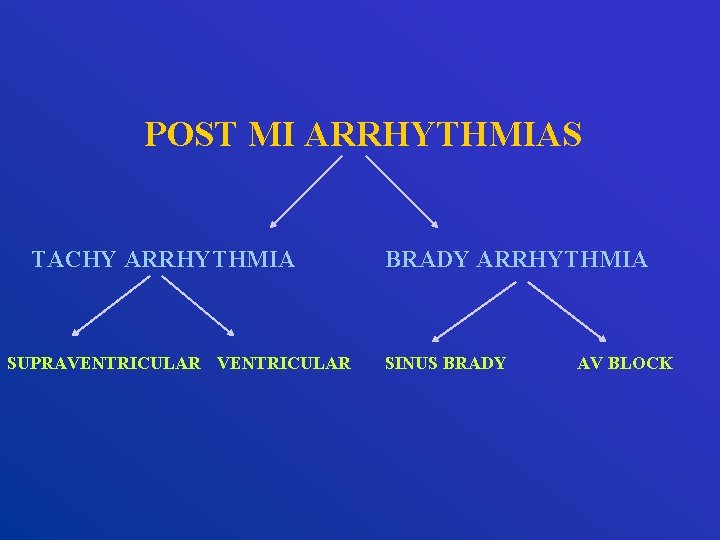
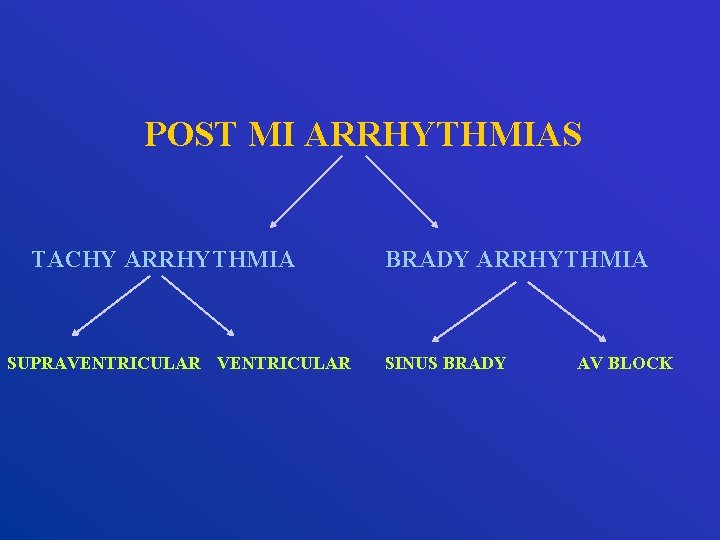
POST MI ARRHYTHMIAS TACHY ARRHYTHMIA SUPRAVENTRICULAR BRADY ARRHYTHMIA SINUS BRADY AV BLOCK
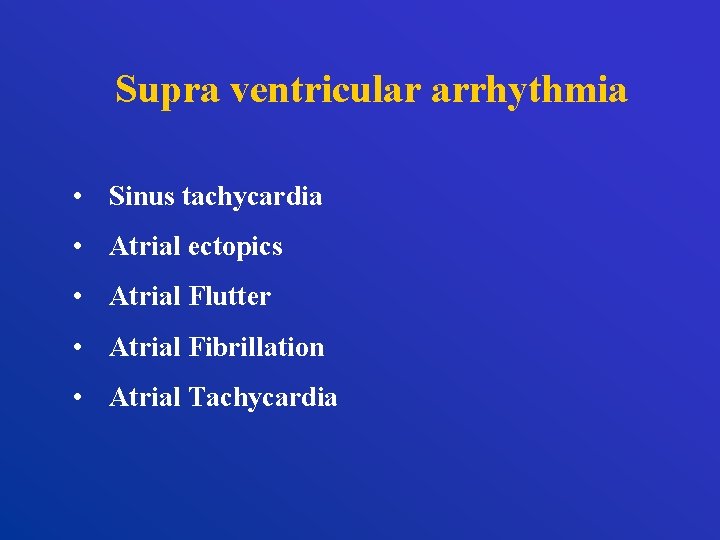
Supra ventricular arrhythmia • Sinus tachycardia • Atrial ectopics • Atrial Flutter • Atrial Fibrillation • Atrial Tachycardia
Ventricular arrhythmias • Ventricular ectopics • AIVR • Ventricular tachycardia NSVT / Monomorphic / polymorphic • Ventricular Fibrillation
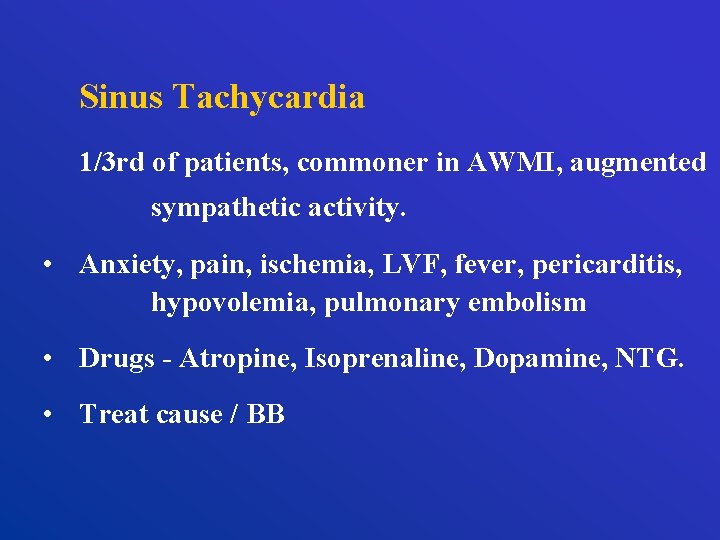
Sinus Tachycardia 1/3 rd of patients, commoner in AWMI, augmented sympathetic activity. • Anxiety, pain, ischemia, LVF, fever, pericarditis, hypovolemia, pulmonary embolism • Drugs - Atropine, Isoprenaline, Dopamine, NTG. • Treat cause / BB

Atrial Premature Beats No treatment required
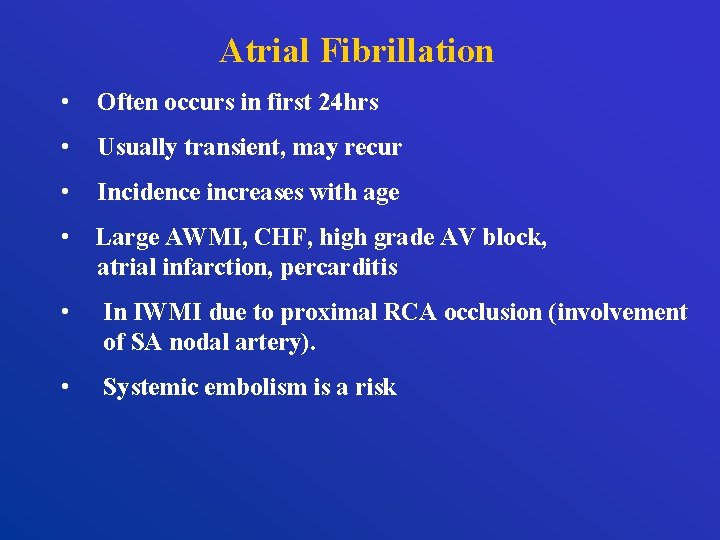
Atrial Fibrillation • Often occurs in first 24 hrs • Usually transient, may recur • Incidence increases with age • Large AWMI, CHF, high grade AV block, atrial infarction, percarditis • In IWMI due to proximal RCA occlusion (involvement of SA nodal artery). • Systemic embolism is a risk
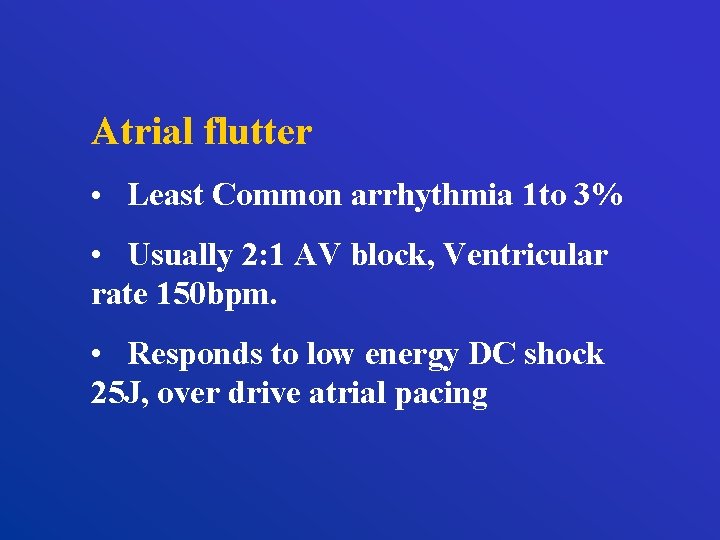
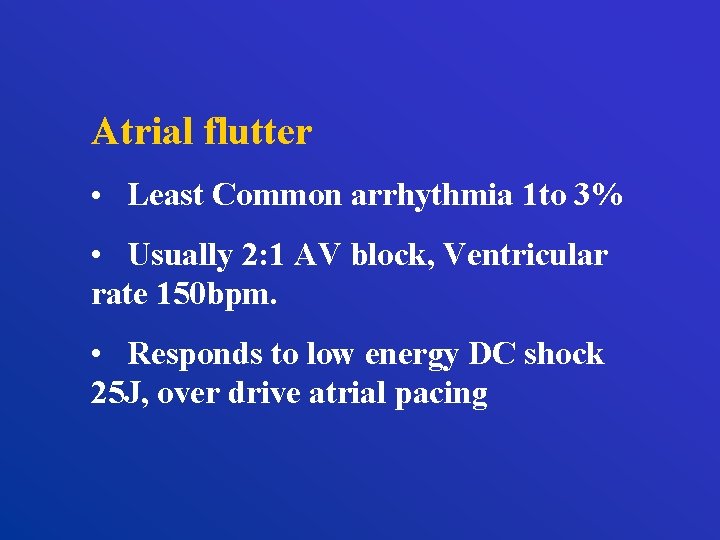
Atrial flutter • Least Common arrhythmia 1 to 3% • Usually 2: 1 AV block, Ventricular rate 150 bpm. • Responds to low energy DC shock 25 J, over drive atrial pacing
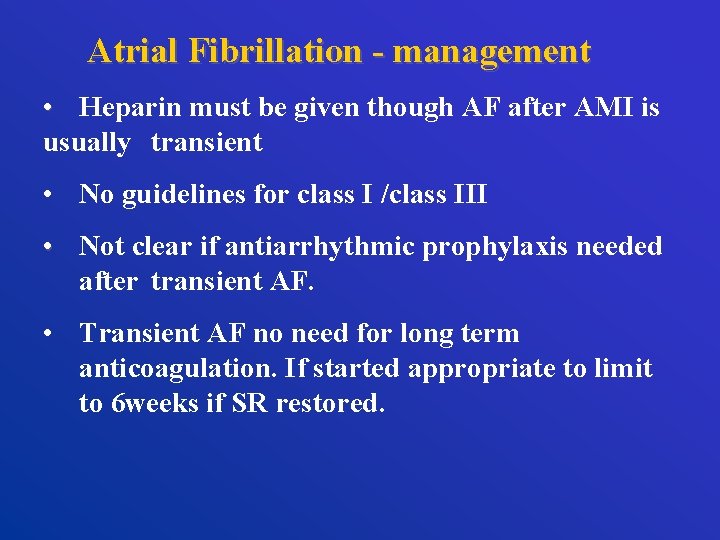
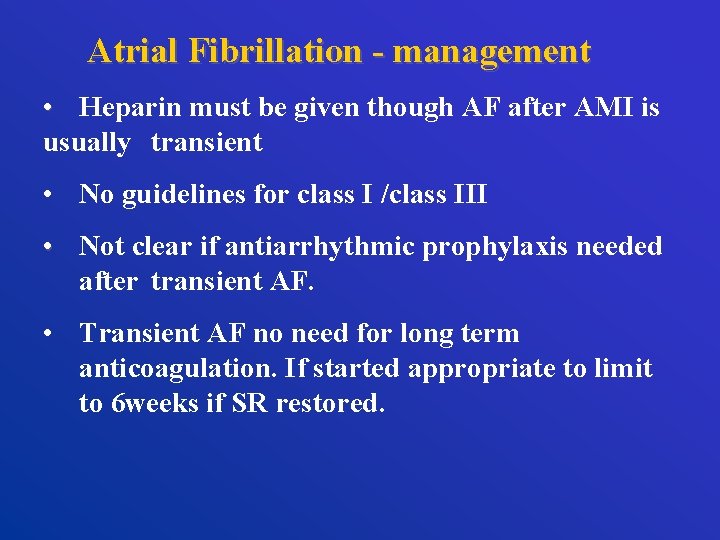
Atrial Fibrillation - management • Heparin must be given though AF after AMI is usually transient • No guidelines for class I /class III • Not clear if antiarrhythmic prophylaxis needed after transient AF. • Transient AF no need for long term anticoagulation. If started appropriate to limit to 6 weeks if SR restored.
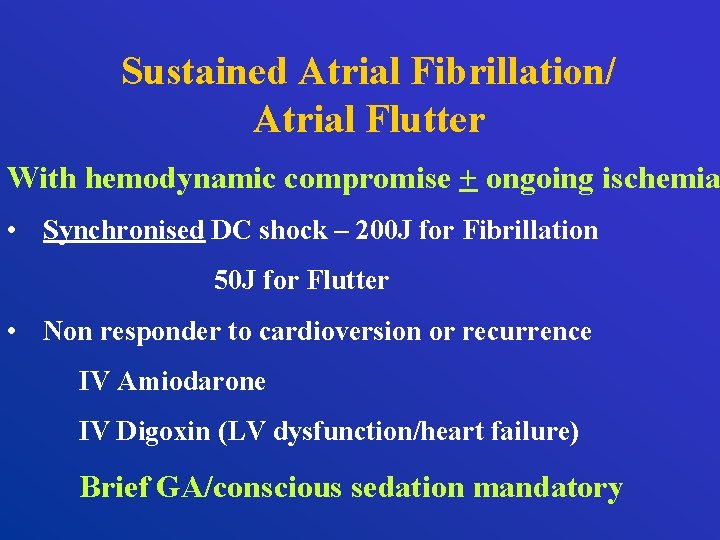
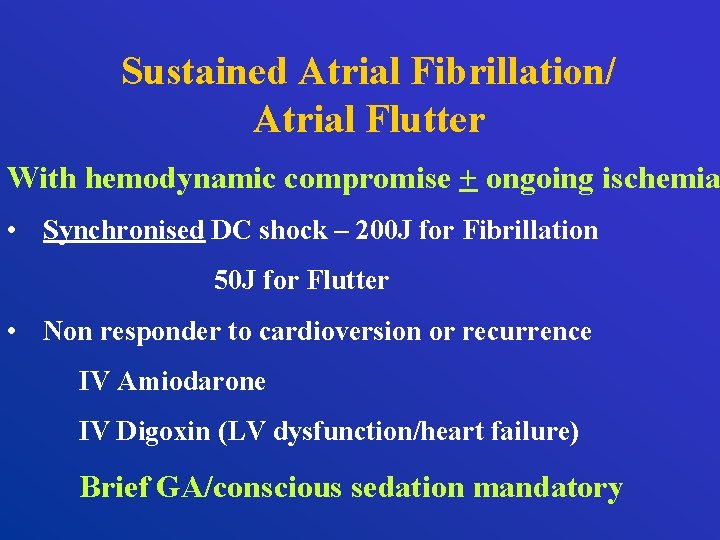
Sustained Atrial Fibrillation/ Atrial Flutter With hemodynamic compromise + ongoing ischemia • Synchronised DC shock – 200 J for Fibrillation 50 J for Flutter • Non responder to cardioversion or recurrence IV Amiodarone IV Digoxin (LV dysfunction/heart failure) Brief GA/conscious sedation mandatory
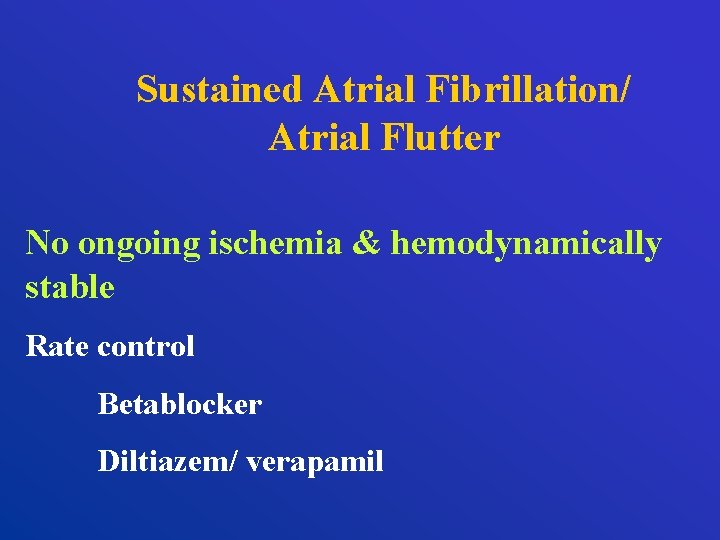
Sustained Atrial Fibrillation/ Atrial Flutter No ongoing ischemia & hemodynamically stable Rate control Betablocker Diltiazem/ verapamil
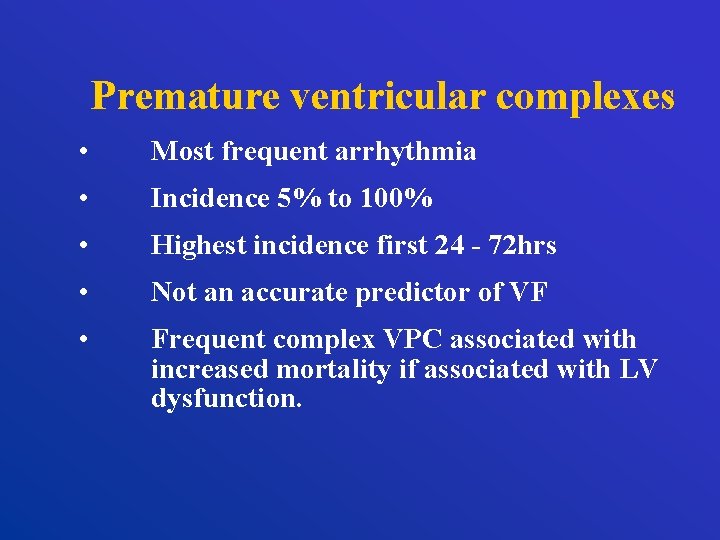
Premature ventricular complexes • Most frequent arrhythmia • Incidence 5% to 100% • Highest incidence first 24 - 72 hrs • Not an accurate predictor of VF • Frequent complex VPC associated with increased mortality if associated with LV dysfunction.
Ventricular Premature Complexes Isolated VPCs, couplets, NSVT + no hemodynamic compromise No need for treatment No role for prophylactic antiarrhythmic therapy (lidocaine)
Accelerated idioventricular rhythm • Rate less than 100 • Associated with reperfusion • Can cause loss of AV synchrony • Usually brief, spontaneous termination, hemodynamically non compromising • Treatment generally not required
Nonsustained Ventricular tachycardia • Recurrent ischemia /Coronary reperfusion • Not associated with increased risk of VT/VF • Prognosis - occurrence within 24 to 48 hrs not predictive of long term mortality. • In contrast occurrence after acute phase of MI 2 to 3 fold increase in overall mortality and sudden cardiac death. • Only agents that improve survival - beta blockers
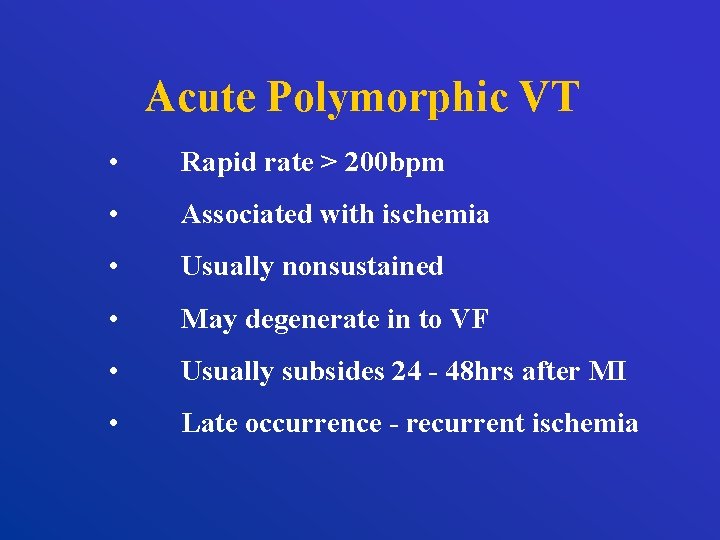
Acute Polymorphic VT • Rapid rate > 200 bpm • Associated with ischemia • Usually nonsustained • May degenerate in to VF • Usually subsides 24 - 48 hrs after MI • Late occurrence - recurrent ischemia
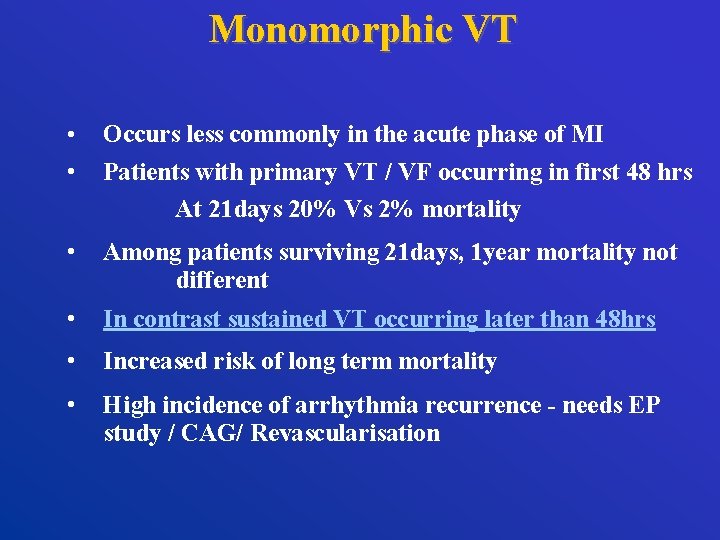
Monomorphic VT • • Occurs less commonly in the acute phase of MI Patients with primary VT / VF occurring in first 48 hrs At 21 days 20% Vs 2% mortality • Among patients surviving 21 days, 1 year mortality not different • In contrast sustained VT occurring later than 48 hrs • Increased risk of long term mortality • High incidence of arrhythmia recurrence - needs EP study / CAG/ Revascularisation
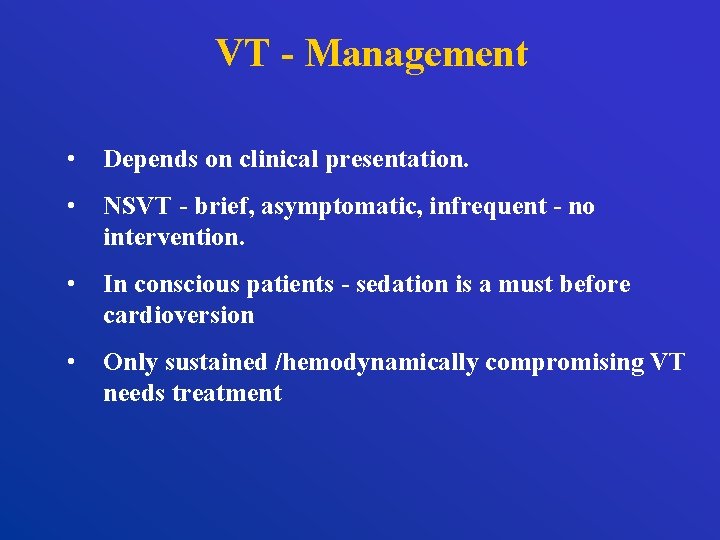
VT - Management • Depends on clinical presentation. • NSVT - brief, asymptomatic, infrequent - no intervention. • In conscious patients - sedation is a must before cardioversion • Only sustained /hemodynamically compromising VT needs treatment
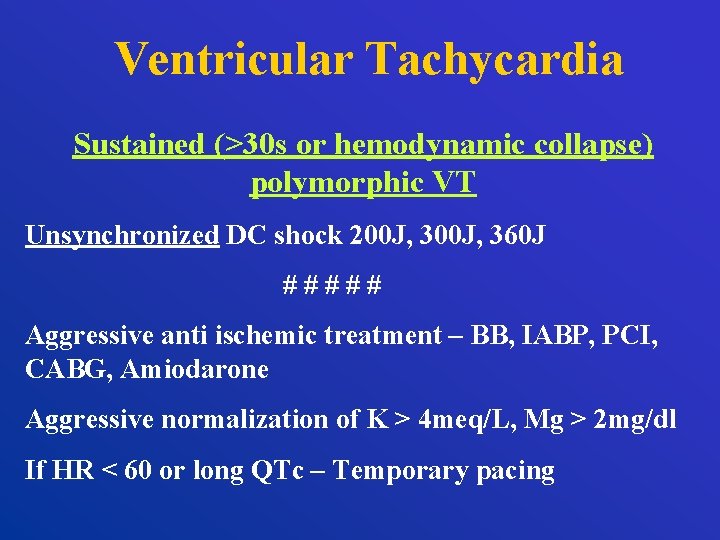
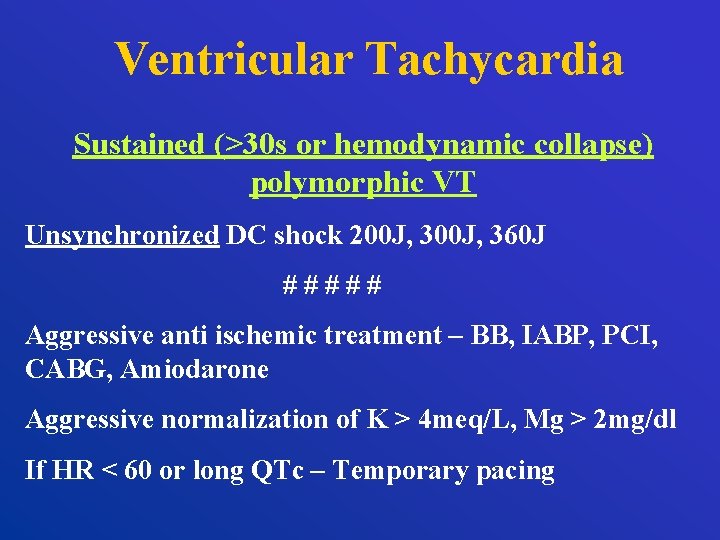
Ventricular Tachycardia Sustained (>30 s or hemodynamic collapse) polymorphic VT Unsynchronized DC shock 200 J, 360 J ##### Aggressive anti ischemic treatment – BB, IABP, PCI, CABG, Amiodarone Aggressive normalization of K > 4 meq/L, Mg > 2 mg/dl If HR < 60 or long QTc – Temporary pacing
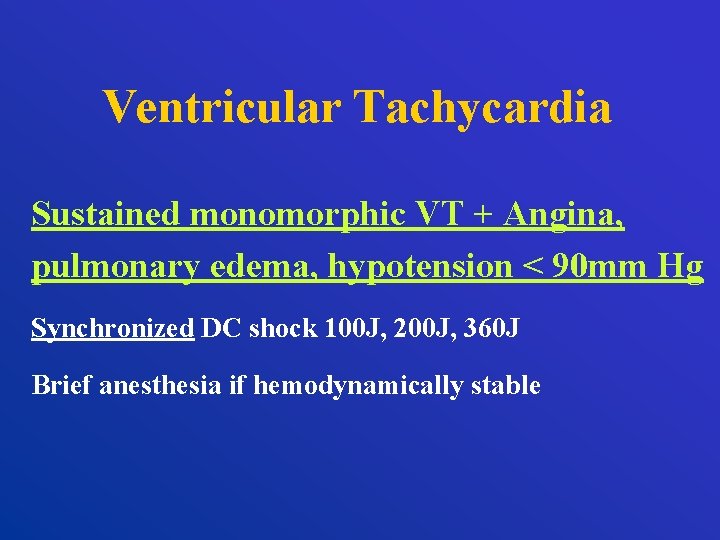
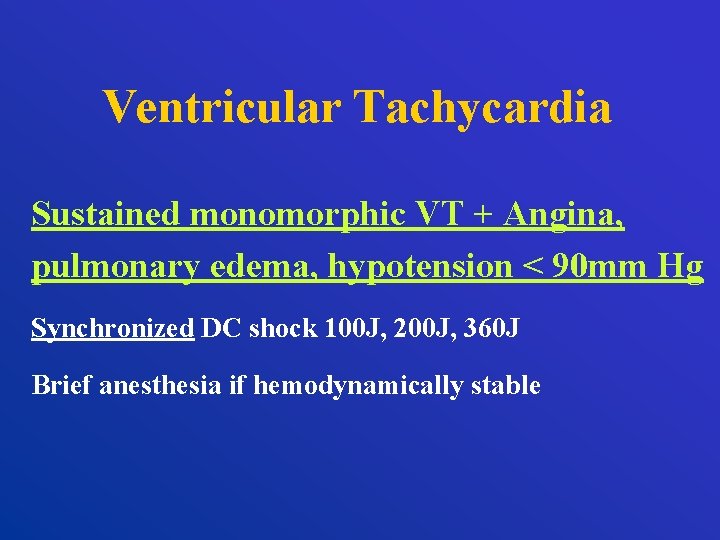
Ventricular Tachycardia Sustained monomorphic VT + Angina, pulmonary edema, hypotension < 90 mm Hg Synchronized DC shock 100 J, 200 J, 360 J Brief anesthesia if hemodynamically stable
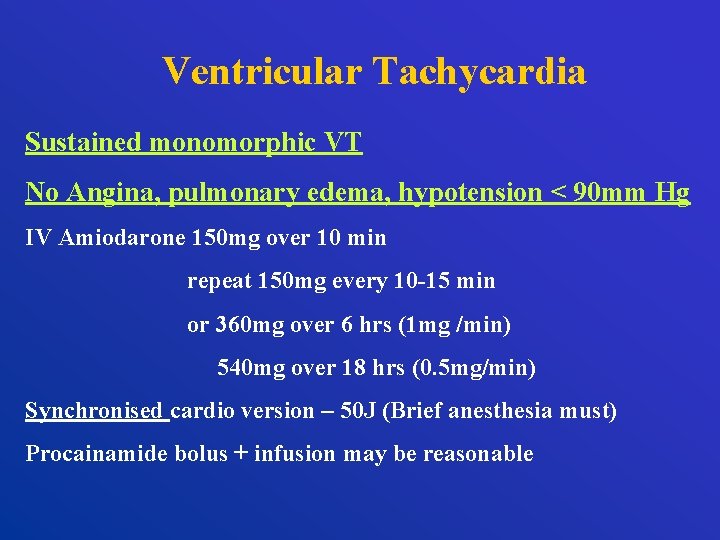
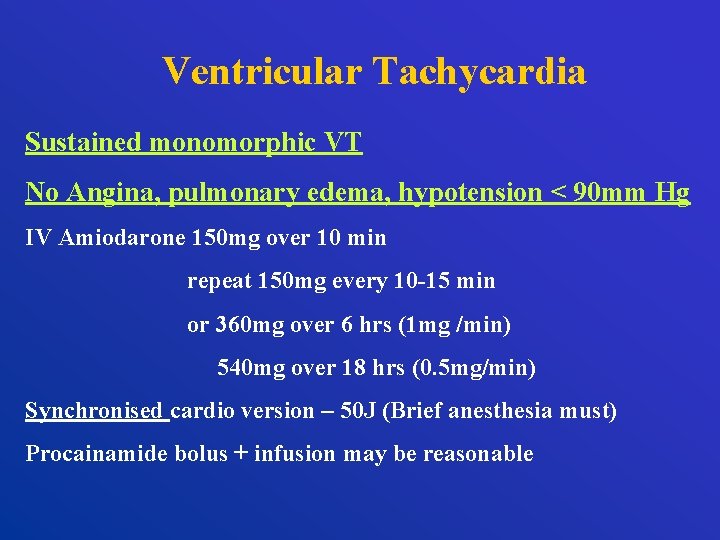
Ventricular Tachycardia Sustained monomorphic VT No Angina, pulmonary edema, hypotension < 90 mm Hg IV Amiodarone 150 mg over 10 min repeat 150 mg every 10 -15 min or 360 mg over 6 hrs (1 mg /min) 540 mg over 18 hrs (0. 5 mg/min) Synchronised cardio version – 50 J (Brief anesthesia must) Procainamide bolus + infusion may be reasonable
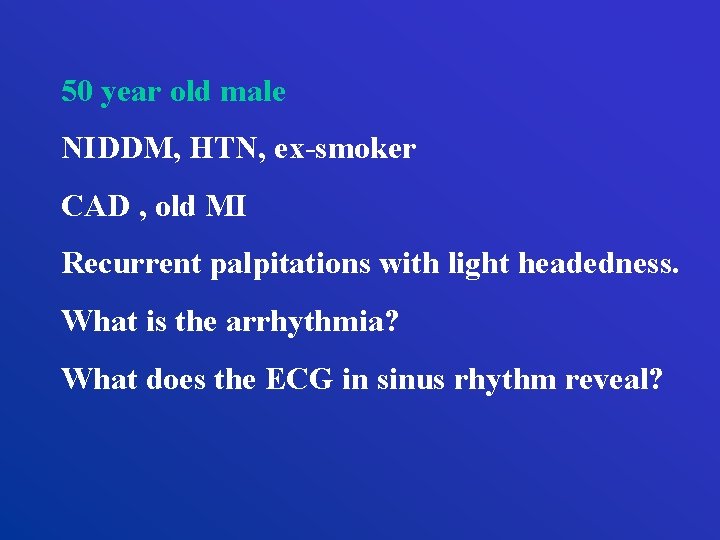
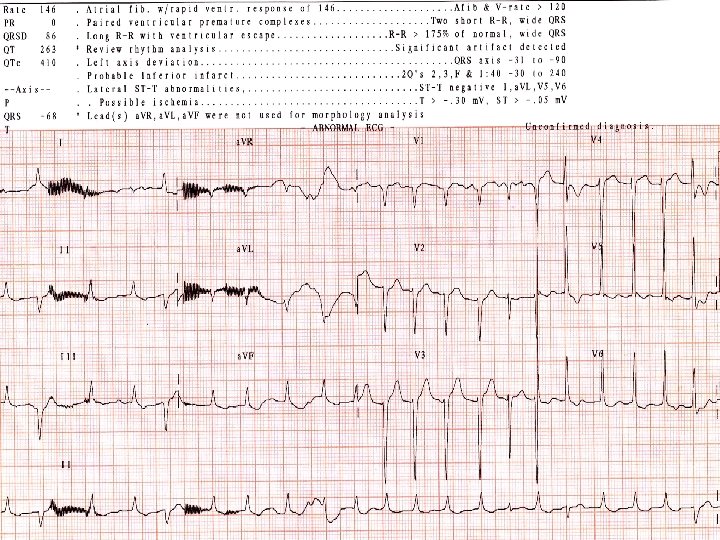
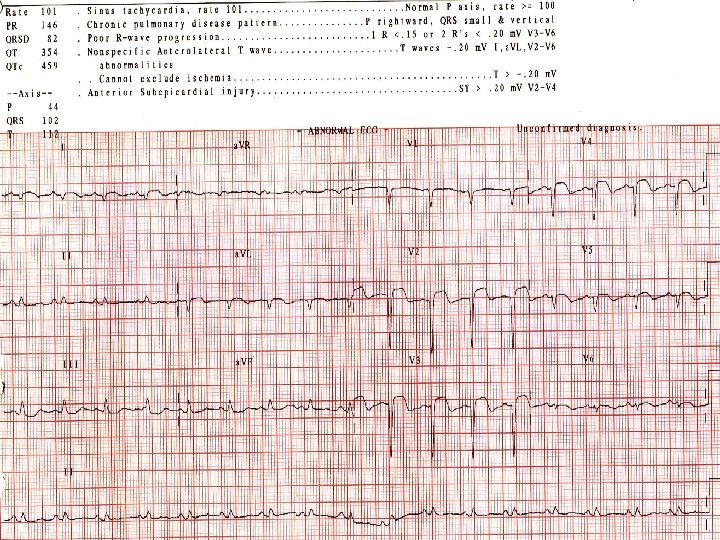
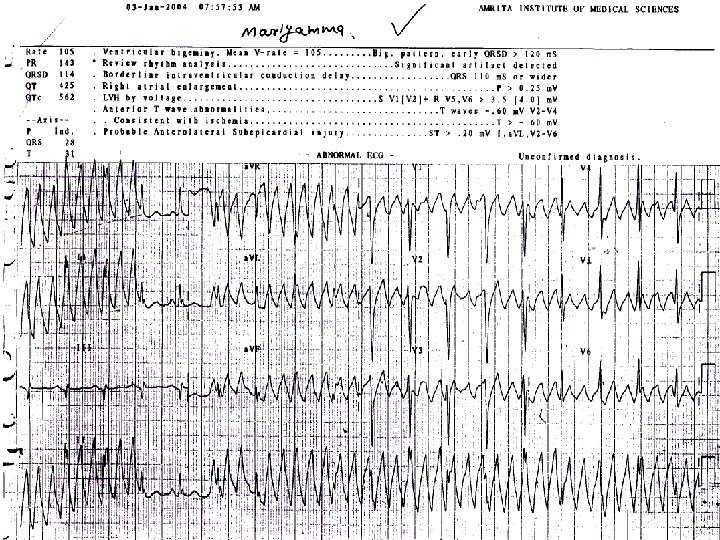
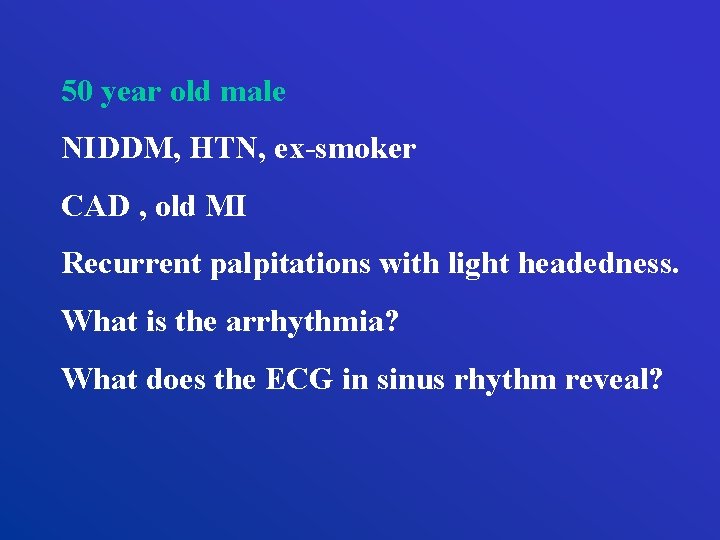
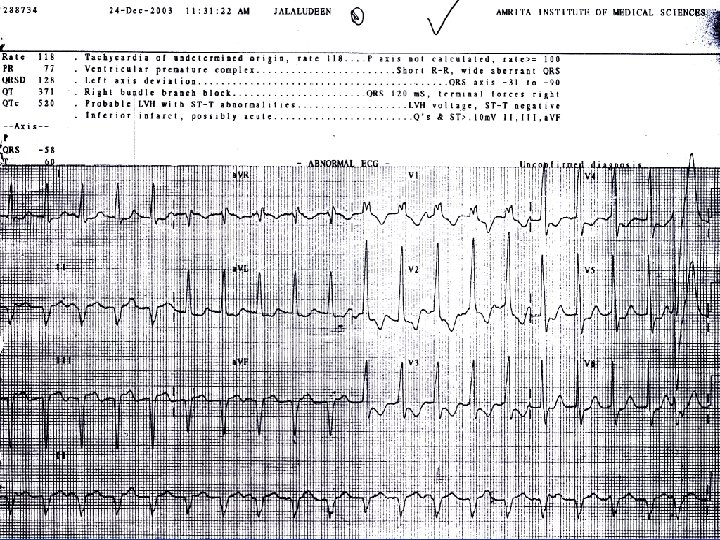
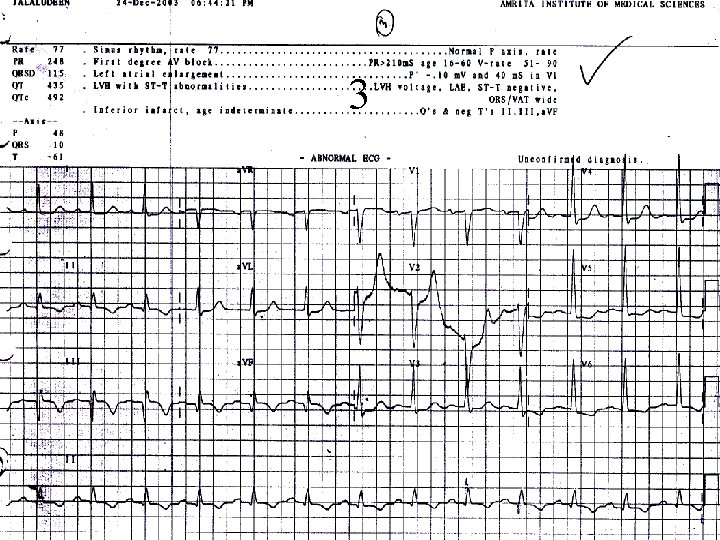
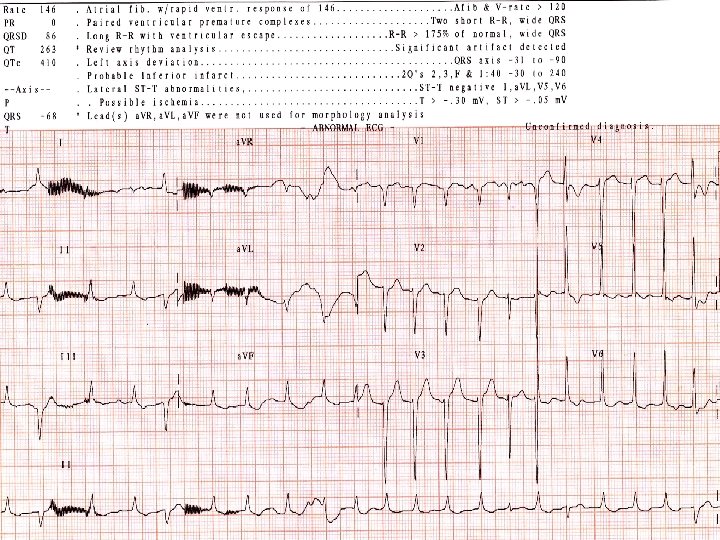
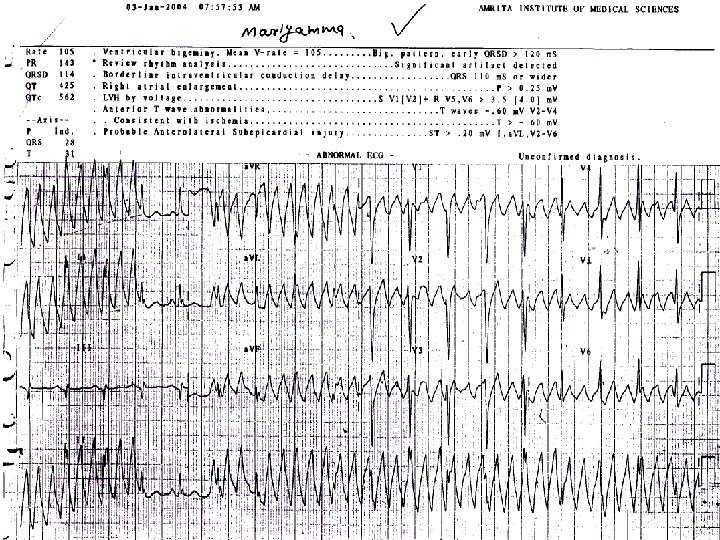
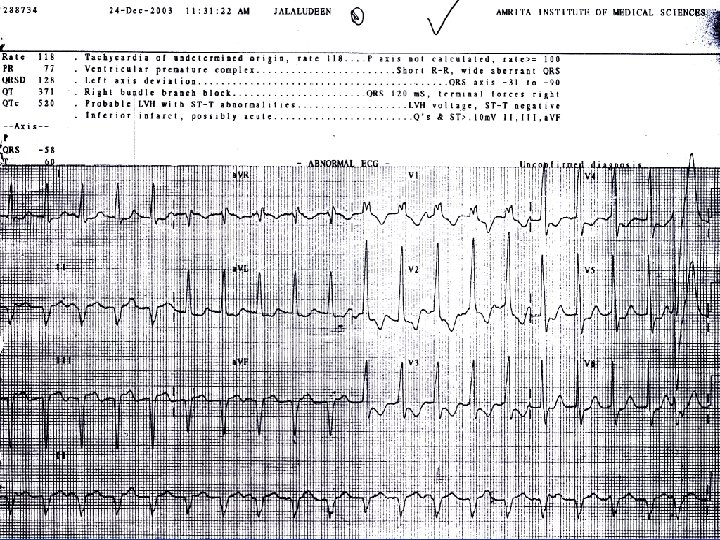
50 year old male NIDDM, HTN, ex-smoker CAD , old MI Recurrent palpitations with light headedness. What is the arrhythmia? What does the ECG in sinus rhythm reveal?
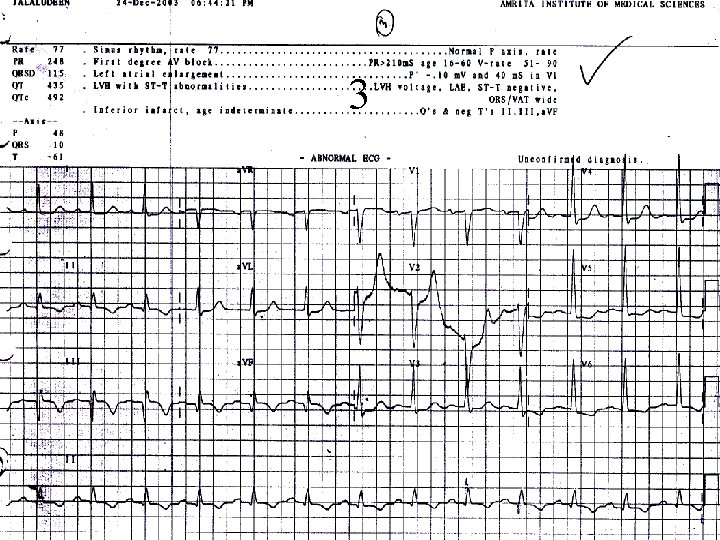
3
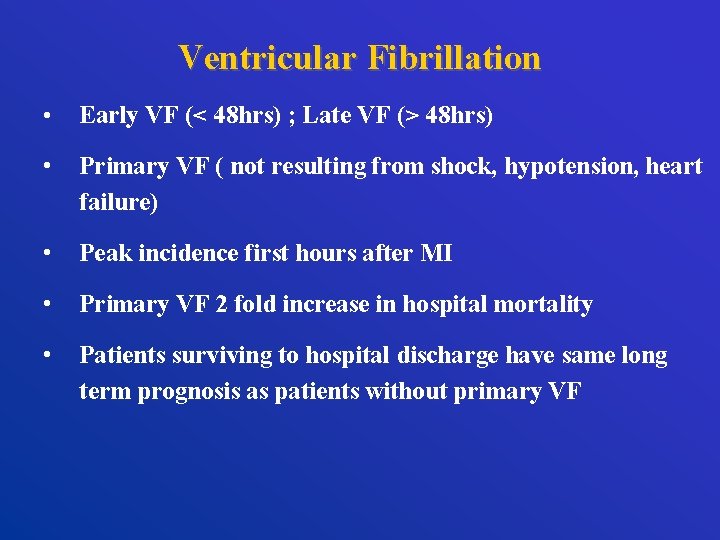
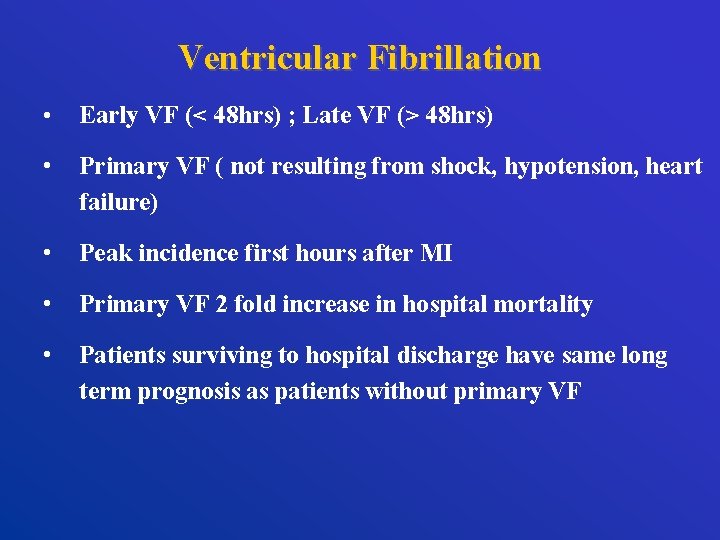
Ventricular Fibrillation • Early VF (< 48 hrs) ; Late VF (> 48 hrs) • Primary VF ( not resulting from shock, hypotension, heart failure) • Peak incidence first hours after MI • Primary VF 2 fold increase in hospital mortality • Patients surviving to hospital discharge have same long term prognosis as patients without primary VF
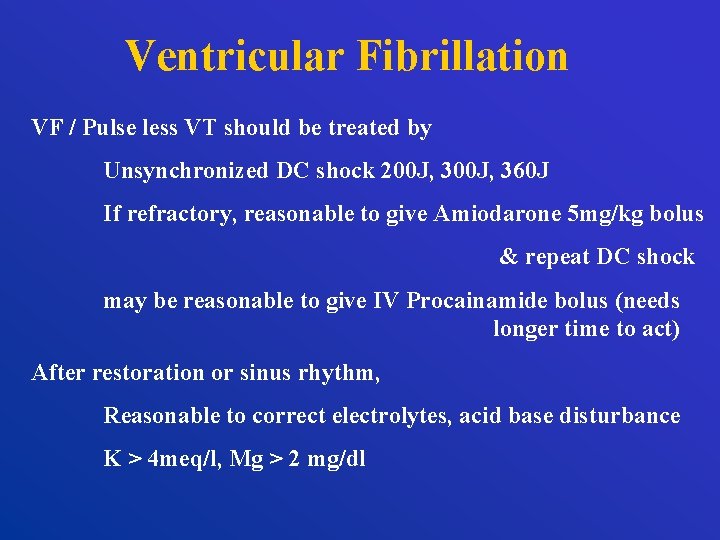
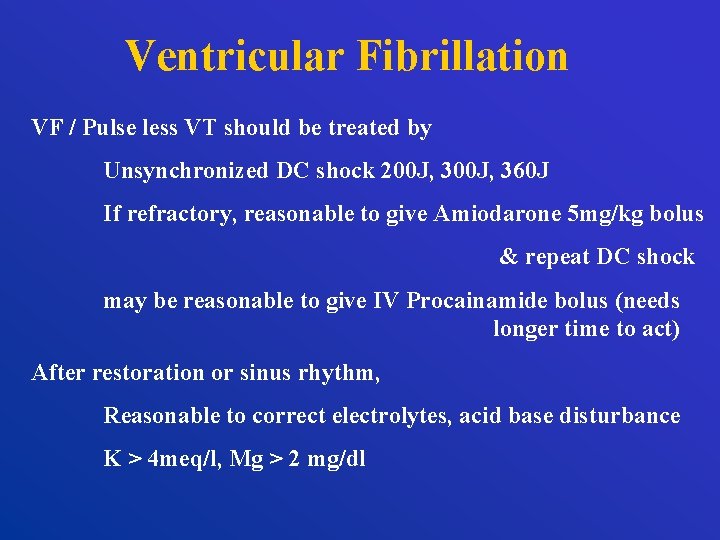
Ventricular Fibrillation VF / Pulse less VT should be treated by Unsynchronized DC shock 200 J, 360 J If refractory, reasonable to give Amiodarone 5 mg/kg bolus & repeat DC shock may be reasonable to give IV Procainamide bolus (needs longer time to act) After restoration or sinus rhythm, Reasonable to correct electrolytes, acid base disturbance K > 4 meq/l, Mg > 2 mg/dl
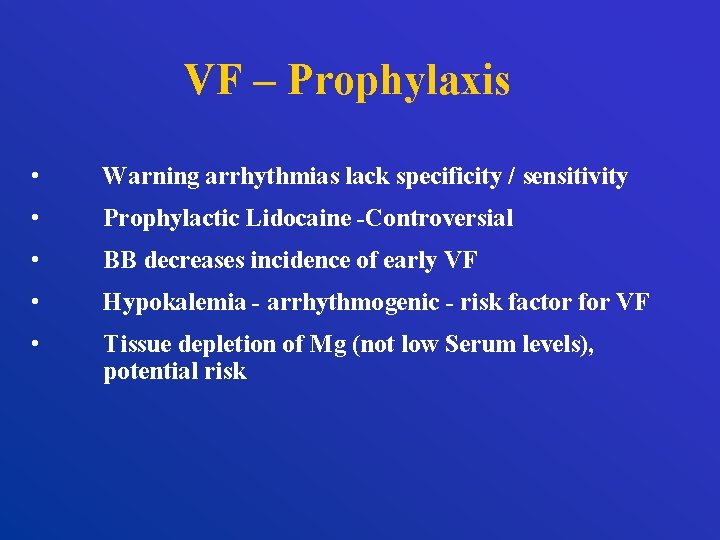
VF – Prophylaxis • Warning arrhythmias lack specificity / sensitivity • Prophylactic Lidocaine -Controversial • BB decreases incidence of early VF • Hypokalemia - arrhythmogenic - risk factor for VF • Tissue depletion of Mg (not low Serum levels), potential risk
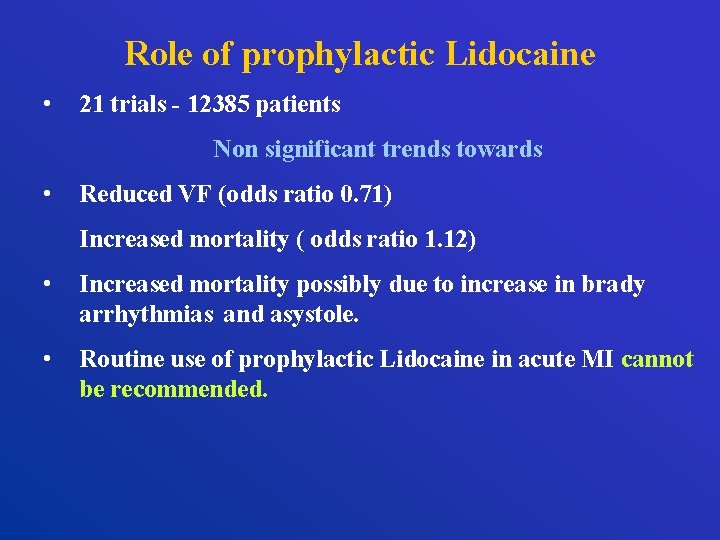
Role of prophylactic Lidocaine • 21 trials - 12385 patients Non significant trends towards • Reduced VF (odds ratio 0. 71) Increased mortality ( odds ratio 1. 12) • Increased mortality possibly due to increase in brady arrhythmias and asystole. • Routine use of prophylactic Lidocaine in acute MI cannot be recommended.
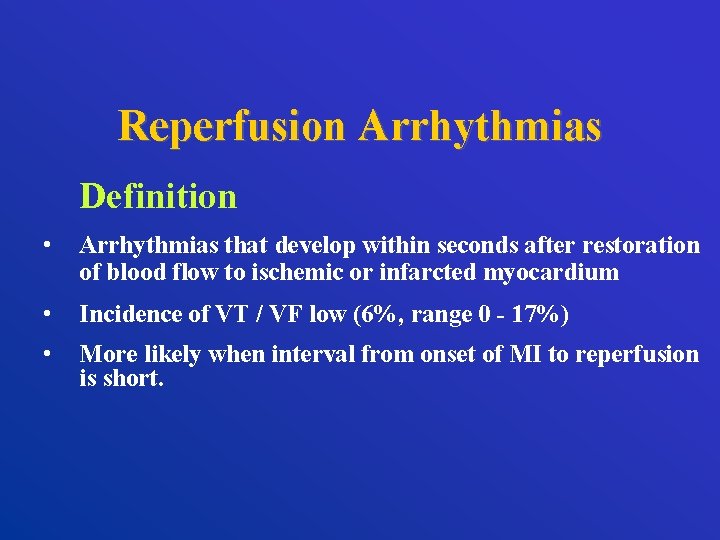
Reperfusion Arrhythmias Definition • Arrhythmias that develop within seconds after restoration of blood flow to ischemic or infarcted myocardium • Incidence of VT / VF low (6%, range 0 - 17%) • More likely when interval from onset of MI to reperfusion is short.
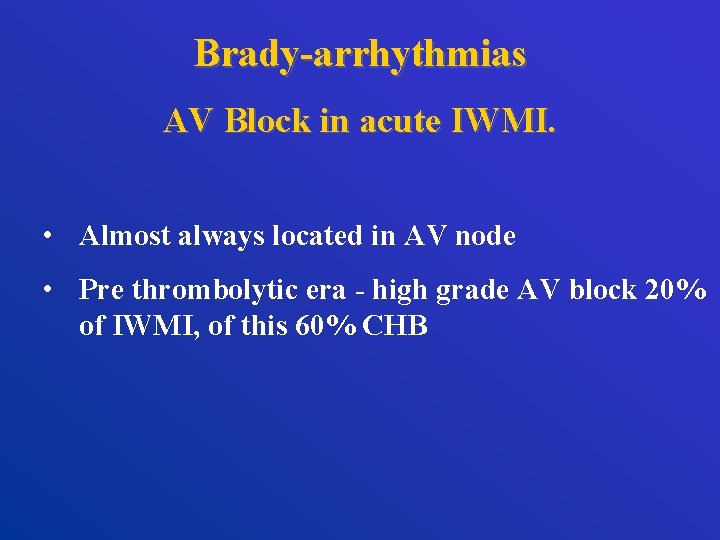
Brady-arrhythmias AV Block in acute IWMI. • Almost always located in AV node • Pre thrombolytic era - high grade AV block 20% of IWMI, of this 60% CHB
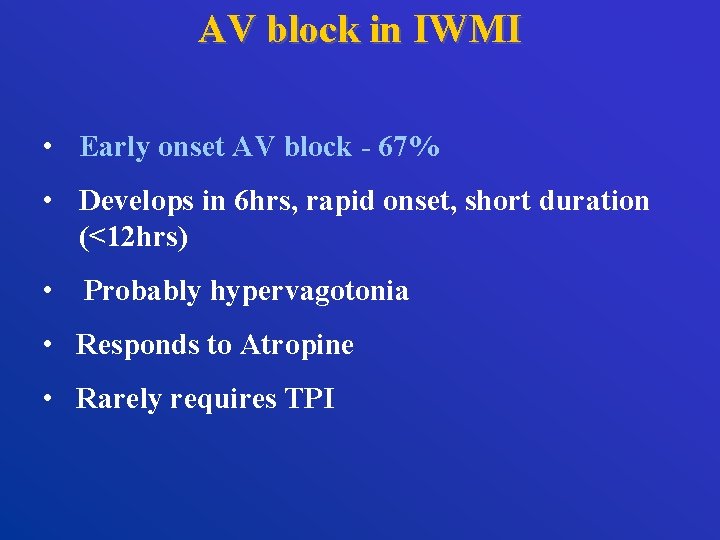
AV block in IWMI • Early onset AV block - 67% • Develops in 6 hrs, rapid onset, short duration (<12 hrs) • Probably hypervagotonia • Responds to Atropine • Rarely requires TPI
AV Block in Acute AWMI • Extensive necrosis of septum, His bundle, Bundle branches. • Setting of severe LV dysfunction. • High mortality reflects myocardial damage • Slow unreliable ventricular rhythm at 30 -40/min.
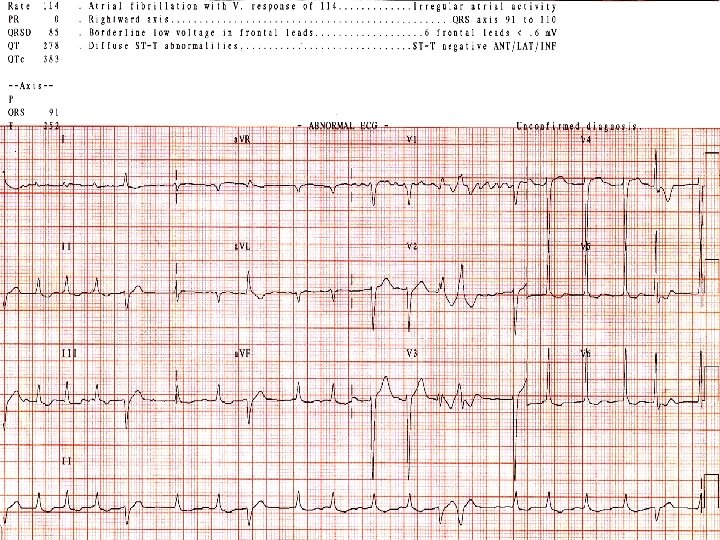
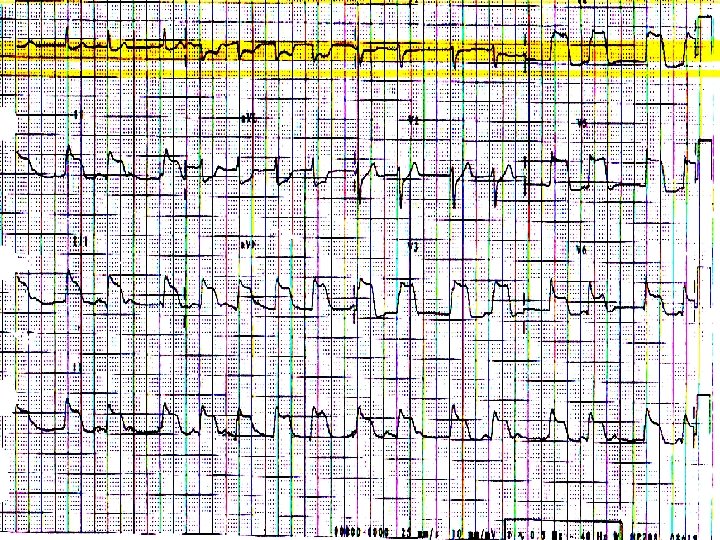
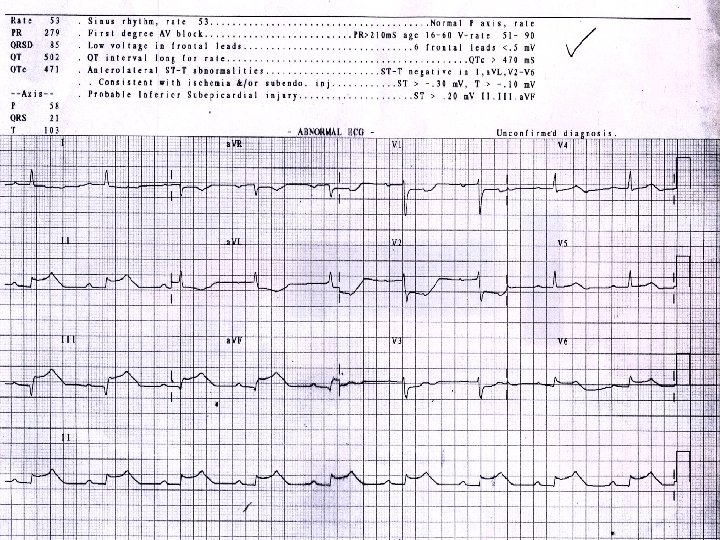
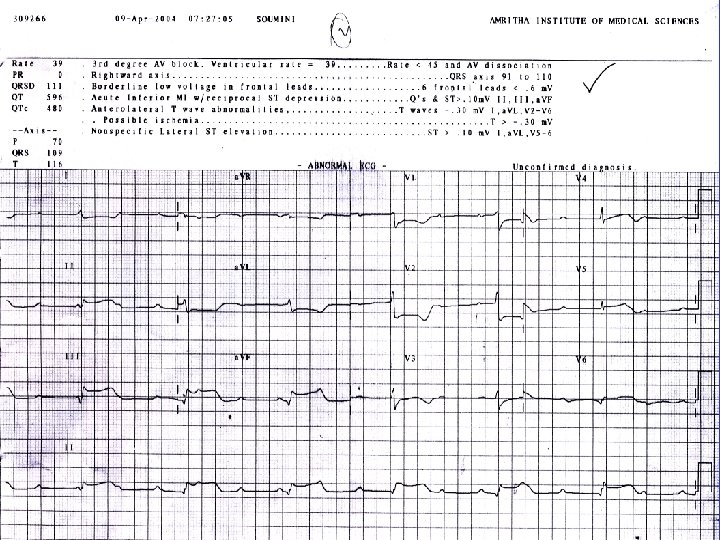
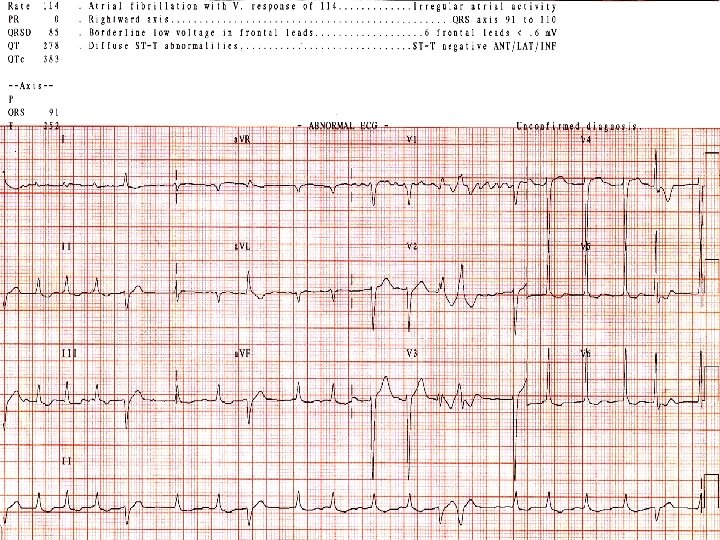
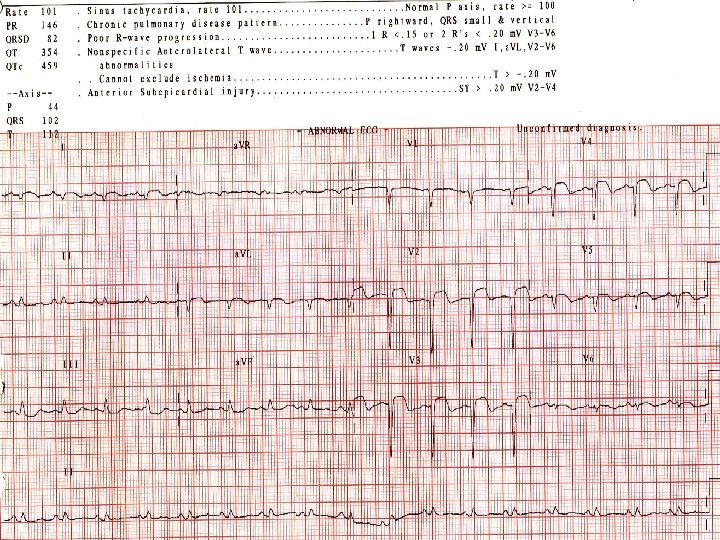
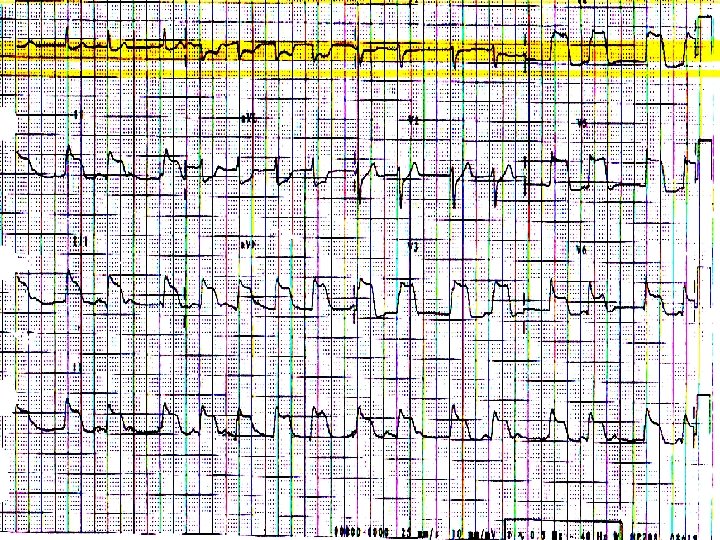
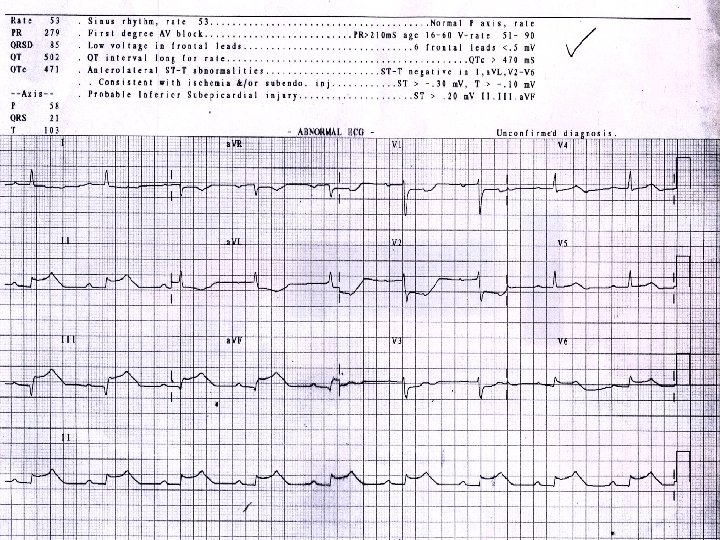
55 year old male Presented to Casualty with persistent retrosternal chest discomfort of 4 hrs duration WHAT IS THE ECG FINDING?
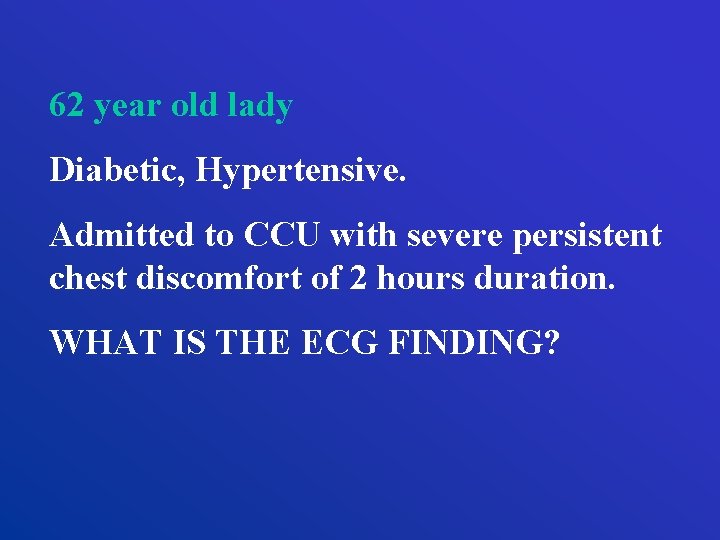
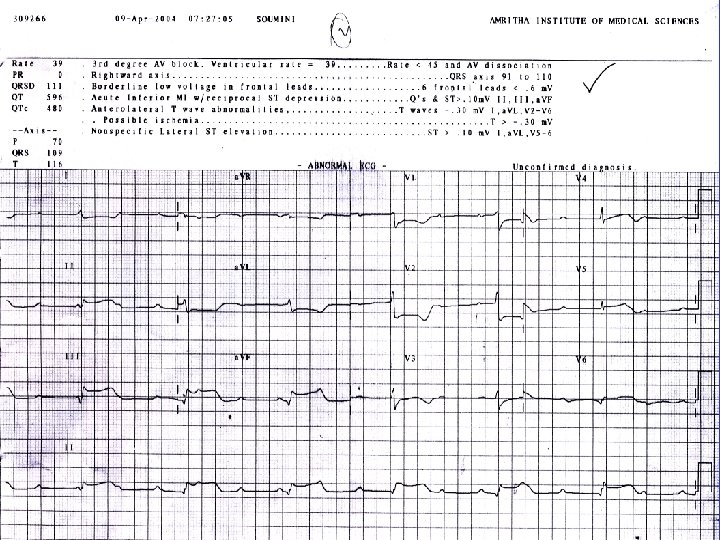
62 year old lady Diabetic, Hypertensive. Admitted to CCU with severe persistent chest discomfort of 2 hours duration. WHAT IS THE ECG FINDING?
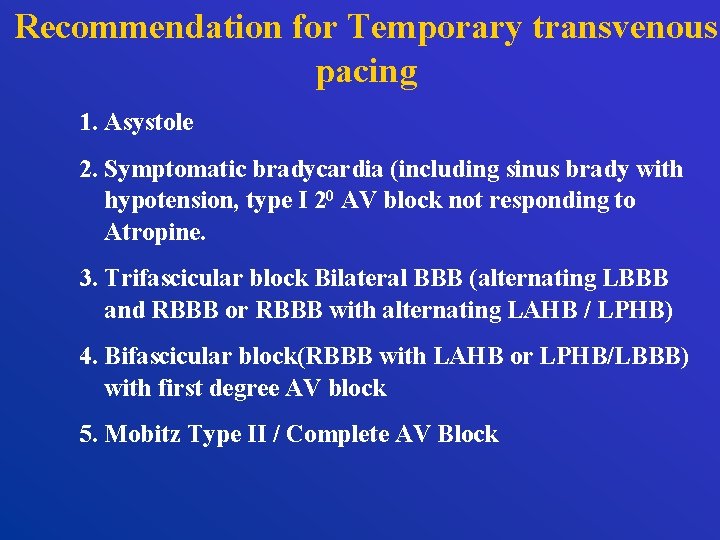
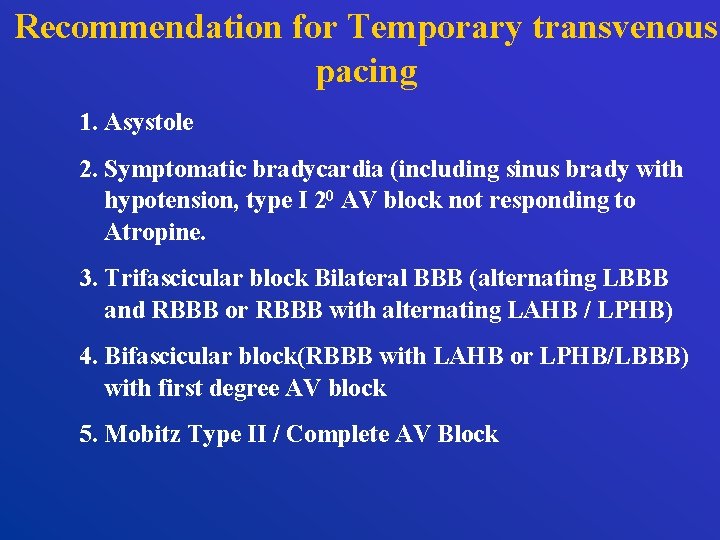
Recommendation for Temporary transvenous pacing 1. Asystole 2. Symptomatic bradycardia (including sinus brady with hypotension, type I 20 AV block not responding to Atropine. 3. Trifascicular block Bilateral BBB (alternating LBBB and RBBB or RBBB with alternating LAHB / LPHB) 4. Bifascicular block(RBBB with LAHB or LPHB/LBBB) with first degree AV block 5. Mobitz Type II / Complete AV Block
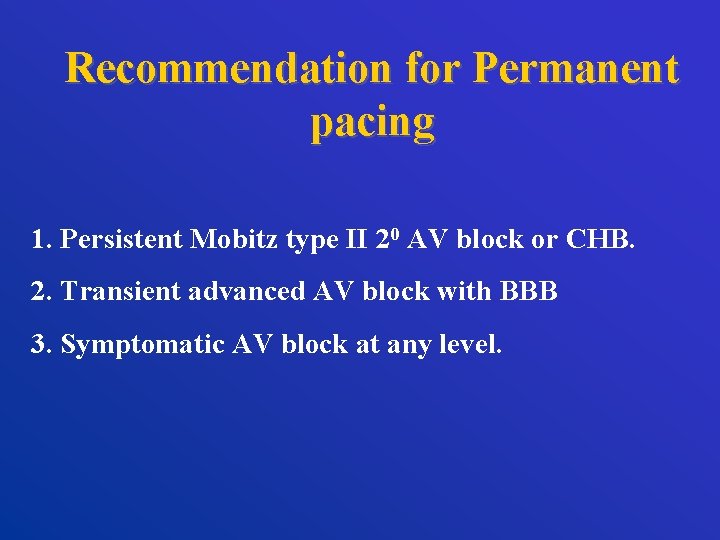
Recommendation for Permanent pacing 1. Persistent Mobitz type II 20 AV block or CHB. 2. Transient advanced AV block with BBB 3. Symptomatic AV block at any level.
TO CONCLUDE……. • Any form of arrhythmia can complicate AMI • Most arrhythmias are transient • Always search for appropriate causes • Treatment depends on hemodynamic consequences • Late onset ventricular arrhythmia increases long term mortality – further risk stratification required
EVOLUTION OF MAN

LIKEWISE …… We also started 50 years ago with open chest defibrillation Now we have monitors, sophisticated defibrillators, PTCA, IABP, advanced pacemakers, AICD etc.
But……. We have to use them APPROPRIATELY OPTIMALLY For best patient outcome