Appropriate Use Criteria Implementation Guidance Update on Requirements

- Slides: 14
Appropriate Use Criteria Implementation Guidance Update on Requirements, Current State, and Next Steps Hans Buitendijk, M. Sc. , FHL 7 Co-Chair HL 7 Orders & Observations Director, Interoperability Strategy – Cerner Corporation Walter Suarez, MD, MPH Chair-Elect HL 7 Executive Director, Health IT Strategy and Policy - Kaiser Permanente 11/27/2020 1
Background • PAMA (Protecting Access to Medicare Act – 2014) included a provision to establish the Appropriate Use Criteria (AUC) Program. • Per the latest PFS rule (2019), January 1, 2020 the Ordering Provider must consult a CDSM while the Furnishing Provider must put certain AUC data on the claim, but will be not be denied if not using proper AUC consultation information. In 2021 claims may be denied. • Initial focus on imaging services • Must use a certified CDS Mechanism (CDSM) • Must communicate on the X 12 claim transaction: • • 11/27/2020 The NPI of Ordering Provider The CDSM consulted The Appropriateness Indication Any Exceptions claimed 2
Key Terms • PLE – A CMS recognized Provider Led Entity • AUC Method – Set of criteria developed by a Provider Led Entity • CDSM Identifier – The identifier established by CMS to a certified CDSM • AUC Indication – CMS defined categories for appropriateness (Appropriate, Not appropriate, No Criteria Apply) 11/27/2020 • Score => A/N/NCA – Translation from a score that a CDSM generates to the CMS reporting categories. • AUC Consultation Identifier – Identifies the specific consultation uniquely to enable downstream reports to go back to the CDSM source for analysis/review/audit. • Exception – A provider can claim an exception that needs to be documented (e. g. , No Internet) 3
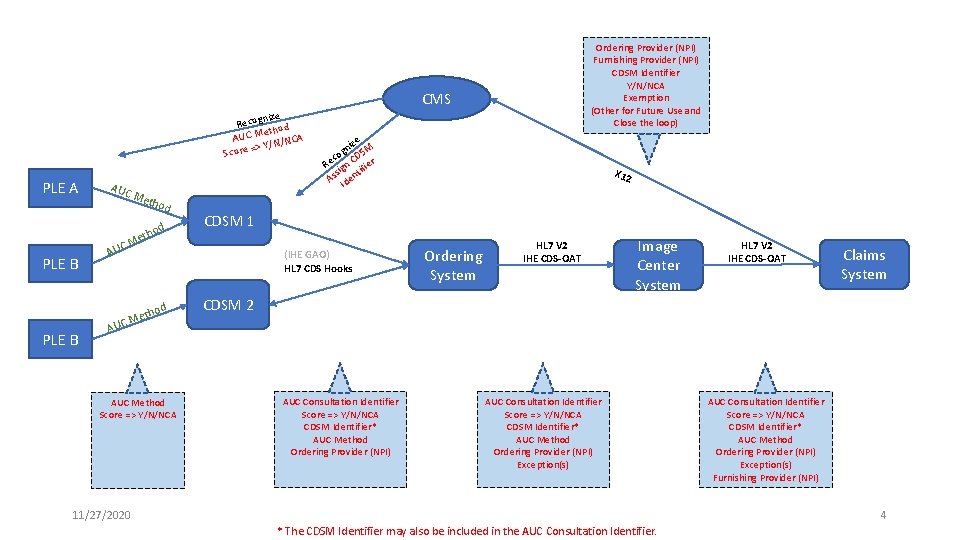
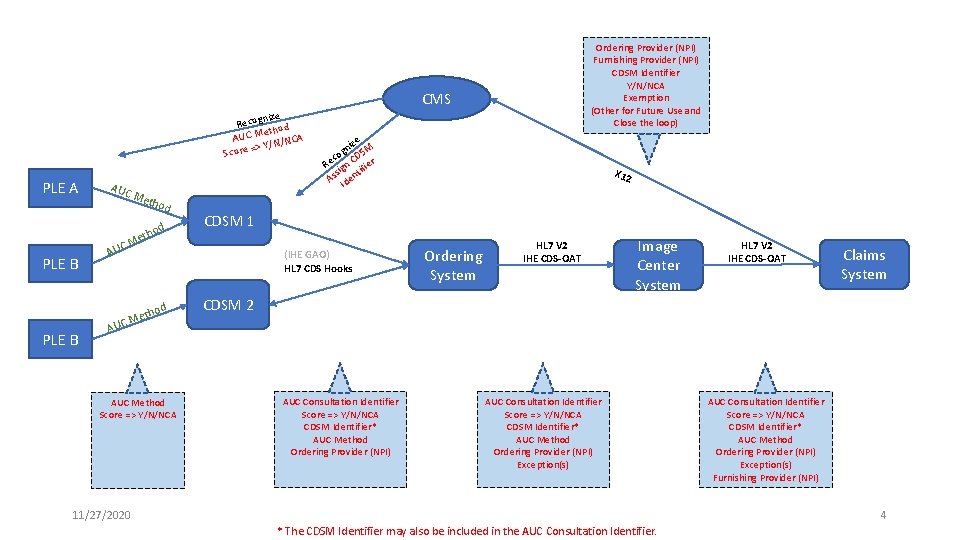
Ordering Provider (NPI) Furnishing Provider (NPI) CDSM Identifier Y/N/NCA Exemption (Other for Future Use and Close the loop) CMS nize Recog od eth AUC M N/NCA => Y/ Score PLE A PLE B AUC Met hod o eth CM AU d d etho CM e niz SM g co D Re ign C ifier t s As Iden X 12 CDSM 1 (IHE GAO) HL 7 CDS Hooks Ordering System HL 7 V 2 IHE CDS-OAT Image Center System HL 7 V 2 IHE CDS-OAT Claims System CDSM 2 AU AUC Method Score => Y/N/NCA AUC Consultation Identifier Score => Y/N/NCA CDSM Identifier* AUC Method Ordering Provider (NPI) Exception(s) 11/27/2020 AUC Consultation Identifier Score => Y/N/NCA CDSM Identifier* AUC Method Ordering Provider (NPI) Exception(s) Furnishing Provider (NPI) 4 * The CDSM Identifier may also be included in the AUC Consultation Identifier.
IHE GAO / CDS Hooks • Interactions with CDSMs are using proprietary formats. • IHE established a draft IHE Guideline Appropriate Ordering (GAO) Profile a couple of years ago. • The IHE GAO Profile is out of data, while CDS Hooks has come along. • CDS workgroup about to start a PSS to build a new IG/Profile based on CDS Hooks. • If interested, please join CDS workgroup to move that project forward. 11/27/2020 5
IHE CDS-OAT • Interactions from the Ordering Provider to Furnishing Provider to Billing are HL 7 V 2 based. • IHE established a draft IHE Clinical Decision Support – Order Appropriateness Tracking (CDS-OAT) Profile • HL 7 provided input on the proposed use of MSH, OBX, and NTE • Updated version being prepped for IHE ballot/review – target is shortly after January 25. • Waiting for CMS to provide HCPCS codes for CDSM, AUC Indication, and 11/27/2020 6
X 12 837 Claim (1) • Required elements on a claim include: • 1) Which qualified CDSM was consulted by the ordering professional; • 2) whether the service adhere or not to the applicable AUC, or whether the AUC consulted was not applicable; and • 3) the NPI of the ordering professional (when different from the furnishing professional) • In accordance with final CMS CY 2019 Physician Fee Schedule rule published December, 2018, rather than using a Unique Consultation Identifier, CMS is going back to requiring the use of code structures that are already in place (G-Codes and Modifiers) to establish reporting requirements. • Each qualified CDSM would be assigned a G-Code with a code descriptor containing the name of the qualified CDSM • HCPCS Level II modifier QQ “Ordering Professional Consulted a Qualified Clinical Decision Support Mechanism for This Service and the Related Data Was Provided to the Furnishing Professional” • Modifier QQ should be reported on the same line as the CPT code for an applicable advanced diagnostic imaging service on both the institutional and professional claims. 11/27/2020 7 • Prior to January 1, 2020, submission is voluntary – no claim rejection will occur
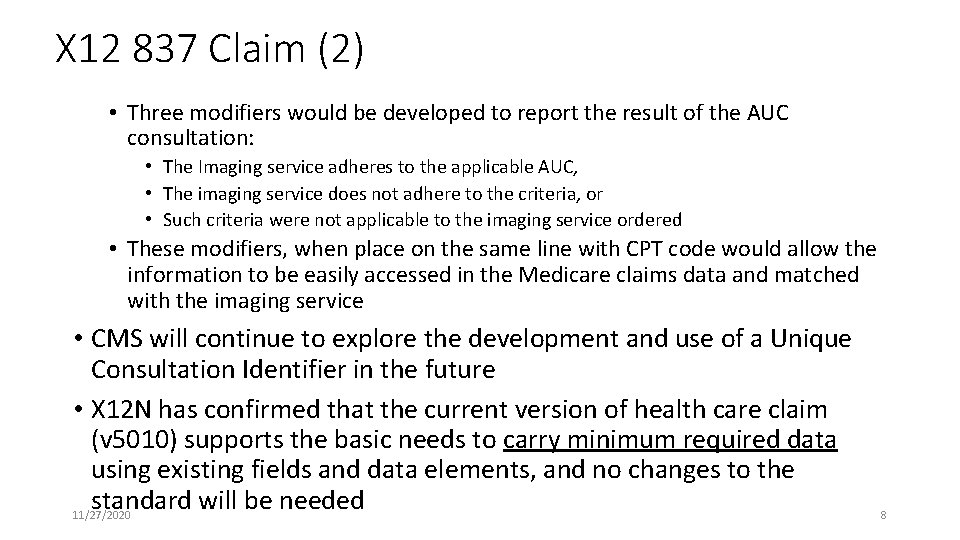
X 12 837 Claim (2) • Three modifiers would be developed to report the result of the AUC consultation: • The Imaging service adheres to the applicable AUC, • The imaging service does not adhere to the criteria, or • Such criteria were not applicable to the imaging service ordered • These modifiers, when place on the same line with CPT code would allow the information to be easily accessed in the Medicare claims data and matched with the imaging service • CMS will continue to explore the development and use of a Unique Consultation Identifier in the future • X 12 N has confirmed that the current version of health care claim (v 5010) supports the basic needs to carry minimum required data using existing fields and data elements, and no changes to the standard will be needed 11/27/2020 8
Draft IHE CDS-OAT Profile Review • Latest Draft (pre-IHE Ballot/Review) • Key concept is to use EITHER • IHE Rad Framework fully • Use AUC guidance ONLY for MSH, OBX, and NTE in any existing HL 7 V 2 order or charge message. • Pre-Adopt V 2. 9 capabilities 11/27/2020 9
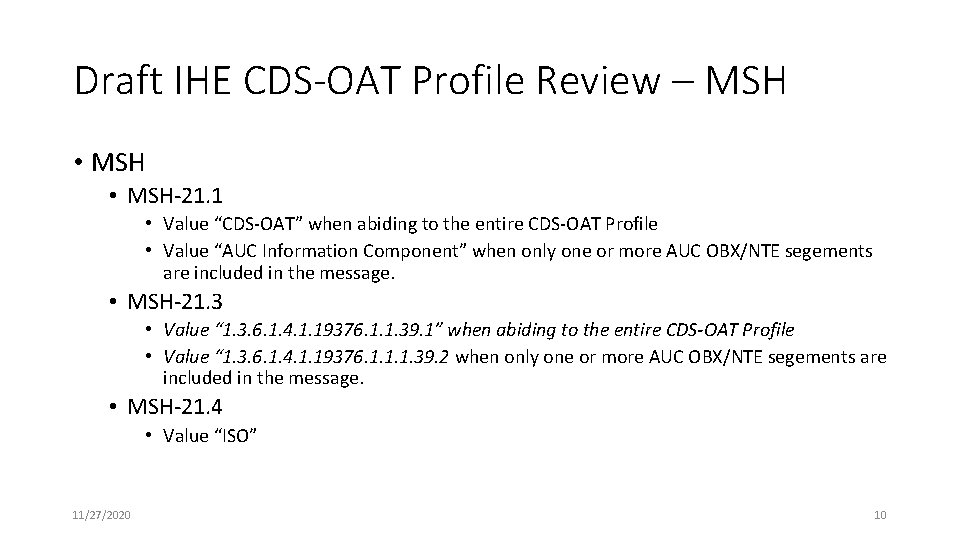
Draft IHE CDS-OAT Profile Review – MSH • MSH-21. 1 • Value “CDS-OAT” when abiding to the entire CDS-OAT Profile • Value “AUC Information Component” when only one or more AUC OBX/NTE segements are included in the message. • MSH-21. 3 • Value “ 1. 3. 6. 1. 4. 1. 19376. 1. 1. 39. 1” when abiding to the entire CDS-OAT Profile • Value “ 1. 3. 6. 1. 4. 1. 19376. 1. 1. 1. 39. 2 when only one or more AUC OBX/NTE segements are included in the message. • MSH-21. 4 • Value “ISO” 11/27/2020 10

Draft IHE CDS-OAT Profile Review – OBX • OBX-2 Value Type = “ST” • OBX-3 Observation Identifier = LOINC for AUC Consultation • • OBX-3. 1 = “ 76516 -6” OBX-3. 2 = “Requested Procedure is Appropriate” OBX-3. 3 = “LN” OBX-3. 14 = “ 2. 16. 840. 1. 113883. 6. 1” • OBX-5 Observation Value = the score • OBX-8 Interpretation Codes = the AUC Indication • OBX-8. 1 = valid HCPCS code for A, N, or NCA • OBX-8. 2 = either “Adhere”, “Not Adhere”, or “No Criteria Applicable” • OBX-8. 3 = “HCPCS” 11/27/2020 11
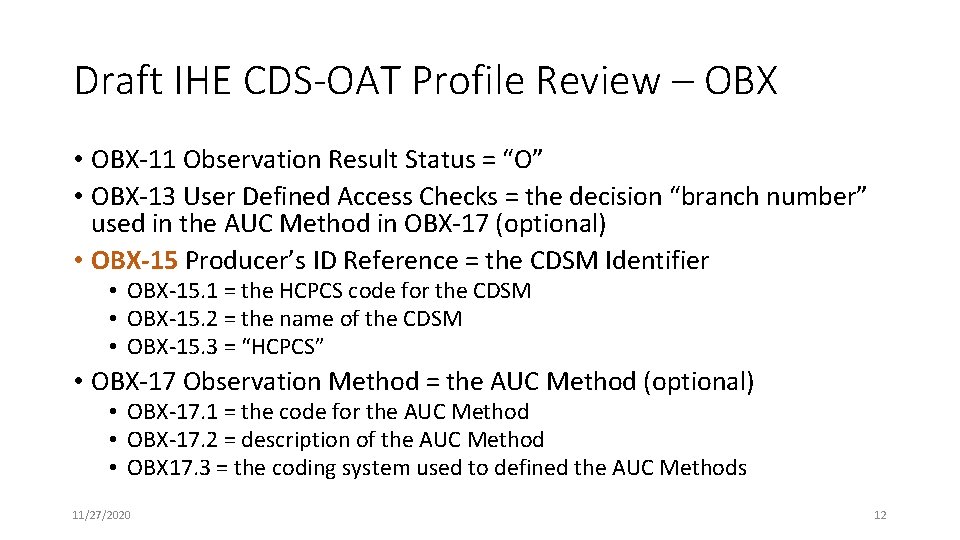
Draft IHE CDS-OAT Profile Review – OBX • OBX-11 Observation Result Status = “O” • OBX-13 User Defined Access Checks = the decision “branch number” used in the AUC Method in OBX-17 (optional) • OBX-15 Producer’s ID Reference = the CDSM Identifier • OBX-15. 1 = the HCPCS code for the CDSM • OBX-15. 2 = the name of the CDSM • OBX-15. 3 = “HCPCS” • OBX-17 Observation Method = the AUC Method (optional) • OBX-17. 1 = the code for the AUC Method • OBX-17. 2 = description of the AUC Method • OBX 17. 3 = the coding system used to defined the AUC Methods 11/27/2020 12
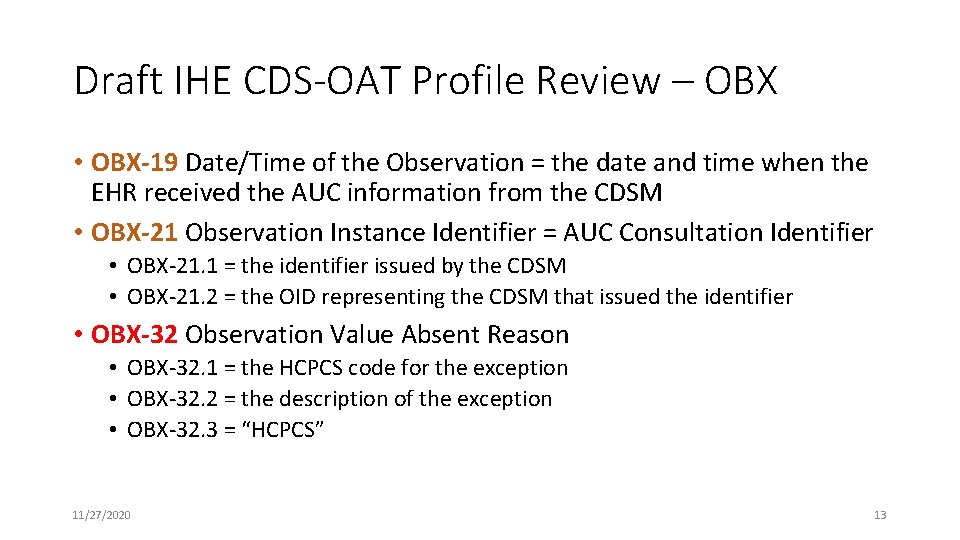
Draft IHE CDS-OAT Profile Review – OBX • OBX-19 Date/Time of the Observation = the date and time when the EHR received the AUC information from the CDSM • OBX-21 Observation Instance Identifier = AUC Consultation Identifier • OBX-21. 1 = the identifier issued by the CDSM • OBX-21. 2 = the OID representing the CDSM that issued the identifier • OBX-32 Observation Value Absent Reason • OBX-32. 1 = the HCPCS code for the exception • OBX-32. 2 = the description of the exception • OBX-32. 3 = “HCPCS” 11/27/2020 13
Draft IHE CDS-OAT Profile Review – NTE • There may only be one NTE per AUC OBX segment • If an NTE is included, it shall be stored by the receiver 11/27/2020 14