Approaches of the Ankle for Pilon Fractures Tyler
- Slides: 1
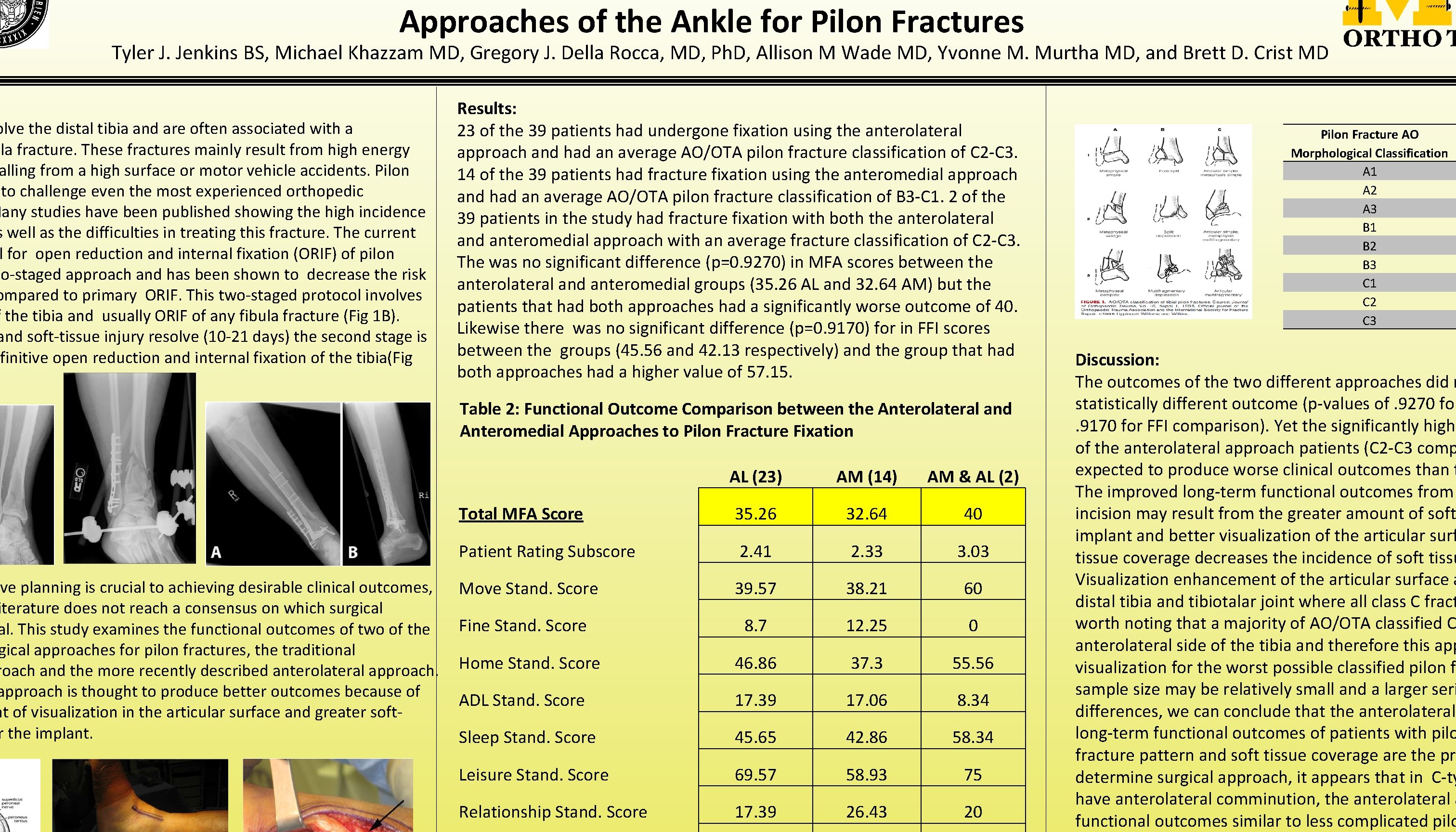
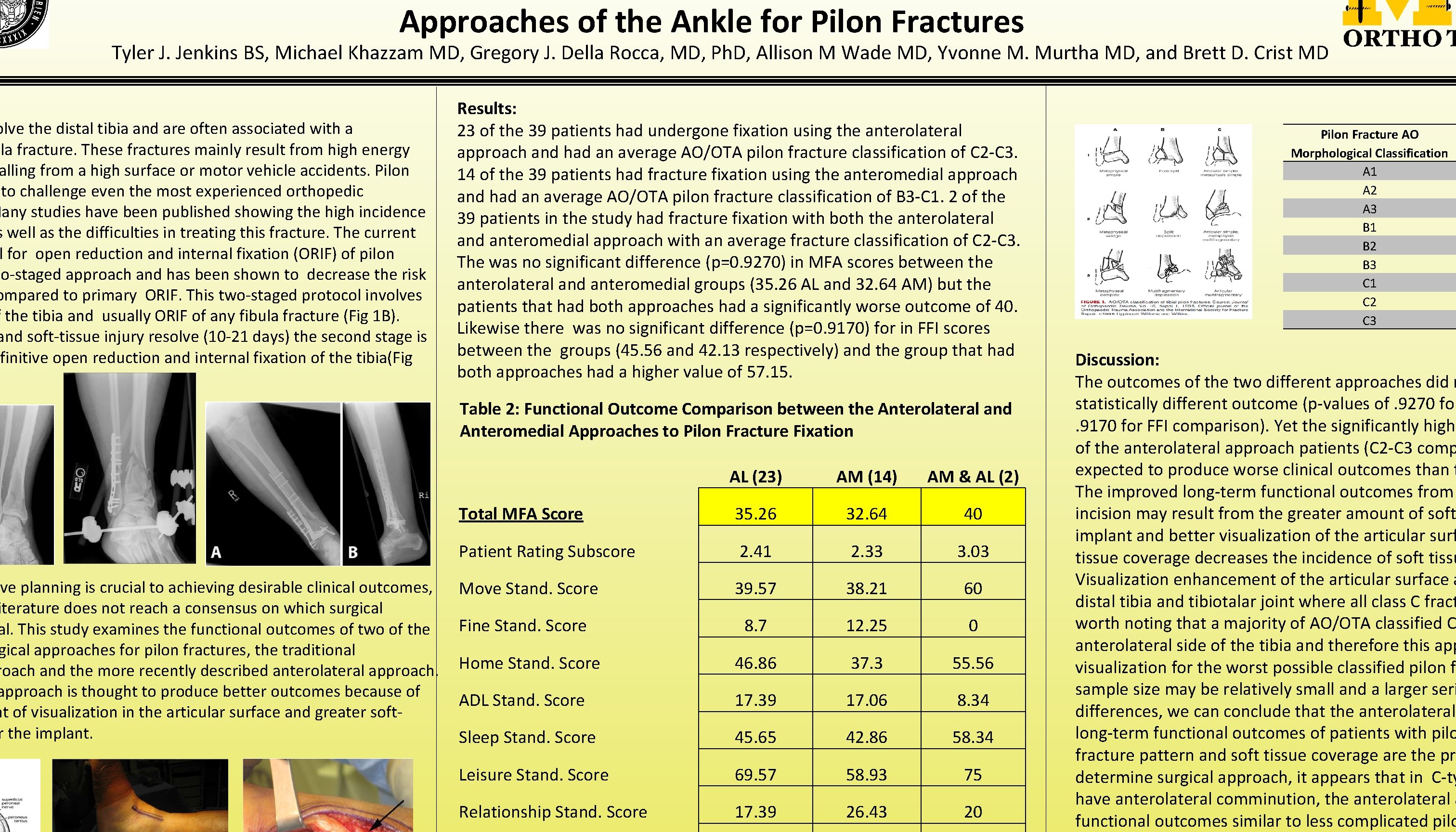
Approaches of the Ankle for Pilon Fractures Tyler J. Jenkins BS, Michael Khazzam MD, Gregory J. Della Rocca, MD, Ph. D, Allison M Wade MD, Yvonne M. Murtha MD, and Brett D. Crist MD olve the distal tibia and are often associated with a ula fracture. These fractures mainly result from high energy alling from a high surface or motor vehicle accidents. Pilon to challenge even the most experienced orthopedic Many studies have been published showing the high incidence s well as the difficulties in treating this fracture. The current l for open reduction and internal fixation (ORIF) of pilon wo-staged approach and has been shown to decrease the risk ompared to primary ORIF. This two-staged protocol involves f the tibia and usually ORIF of any fibula fracture (Fig 1 B). and soft-tissue injury resolve (10 -21 days) the second stage is finitive open reduction and internal fixation of the tibia(Fig ve planning is crucial to achieving desirable clinical outcomes, iterature does not reach a consensus on which surgical al. This study examines the functional outcomes of two of the gical approaches for pilon fractures, the traditional roach and the more recently described anterolateral approach is thought to produce better outcomes because of nt of visualization in the articular surface and greater softr the implant. Results: 23 of the 39 patients had undergone fixation using the anterolateral approach and had an average AO/OTA pilon fracture classification of C 2 -C 3. 14 of the 39 patients had fracture fixation using the anteromedial approach and had an average AO/OTA pilon fracture classification of B 3 -C 1. 2 of the 39 patients in the study had fracture fixation with both the anterolateral and anteromedial approach with an average fracture classification of C 2 -C 3. The was no significant difference (p=0. 9270) in MFA scores between the anterolateral and anteromedial groups (35. 26 AL and 32. 64 AM) but the patients that had both approaches had a significantly worse outcome of 40. Likewise there was no significant difference (p=0. 9170) for in FFI scores between the groups (45. 56 and 42. 13 respectively) and the group that had both approaches had a higher value of 57. 15. Table 2: Functional Outcome Comparison between the Anterolateral and Anteromedial Approaches to Pilon Fracture Fixation AL (23) AM (14) AM & AL (2) Total MFA Score 35. 26 32. 64 40 Patient Rating Subscore 2. 41 2. 33 3. 03 Move Stand. Score 39. 57 38. 21 60 8. 7 12. 25 0 Home Stand. Score 46. 86 37. 3 55. 56 ADL Stand. Score 17. 39 17. 06 8. 34 Sleep Stand. Score 45. 65 42. 86 58. 34 Leisure Stand. Score 69. 57 58. 93 75 Relationship Stand. Score 17. 39 26. 43 20 Fine Stand. Score Pilon Fracture AO Morphological Classification A 1 A 2 A 3 B 1 B 2 B 3 C 1 C 2 C 3 Discussion: The outcomes of the two different approaches did n statistically different outcome (p-values of. 9270 for. 9170 for FFI comparison). Yet the significantly highe of the anterolateral approach patients (C 2 -C 3 comp expected to produce worse clinical outcomes than t The improved long-term functional outcomes from incision may result from the greater amount of soft implant and better visualization of the articular surf tissue coverage decreases the incidence of soft tissu Visualization enhancement of the articular surface a distal tibia and tibiotalar joint where all class C fract worth noting that a majority of AO/OTA classified C anterolateral side of the tibia and therefore this app visualization for the worst possible classified pilon fr sample size may be relatively small and a larger seri differences, we can conclude that the anterolateral long-term functional outcomes of patients with pilo fracture pattern and soft tissue coverage are the pri determine surgical approach, it appears that in C-ty have anterolateral comminution, the anterolateral a functional outcomes similar to less complicated pilo