Approach to the Patient with Elevated Creatinine By
Approach to the Patient with Elevated Creatinine By: George Tsimiklis 2004 Revised previous edition by: Lianne Tile MD FRCPC Med

Objectives • To identify appropriate strategies for investigation of the patient with increased creatinine • To discuss interventions that may alter the course of disease • To discuss indications for referral to a nephrologist

Stages of Renal Failure Mild GFR (cc/min) 60 -90 Moderate 30 -60 Severe 10 -30 End-stage <10

Creatinine is an estimate of GFR Cockcroft-Gault: (140 -age) x wt x 100 = GFR (cc/min) 72 x serum Cr GFR (females) = GFR (males) x 0. 85

CASES: What is Considered an ELEVATED Creatinine? 55 yo 70 kg male with Cr of 220: GFR =37 moderate 75 yo 45 kg female with Cr of 220: GFR = 16 severe 75 yo 45 kg female with Cr of 85: GFR =40 moderate 75 yo 45 kg female with Cr of 45: GFR =76 mild

Workup of the patient with high Cr • Approach – 1. Identify chronicity (Acute vs chronic) – 2. Identify the cause, especially reversible causes – 3. Identify Indications for Referral to a Nephrologist – 4. Initiate a cause specific management plan in a multidisciplinary team.

Acute vs Chronic Renal Failure ACUTE - Fever/ hematuria - Hypovolemia - Hydroureter - Sepsis - New hypertension - Recent nephrotoxins - No hypocalcemia - No hyperphosphatemia - No anemia CHRONIC - previous confirmed nephropathy - Already diminished Cr. Cl - Atrophic kidneys (<10 cm on U/S) - Normochromic normocytic anemia - Hypocalcemia - Hyperphosphatemia
Major Causes of Renal Failure • Prerenal: decreased glomerular perfusion – volume depletion: diuretics, poor intake – decreased effective circulating volume: forward heart failure, cirrhosis, sepsis • Renal – Vascular disease: acute (vasculitis, thromboembolic, HUS/TTP, malignant hypertension) vs. chronic (renal artery stenosis, HTN/nephrosclerosis) – Glomerular disease: nephritic vs. nephrotic – Tubular/interstitial disease: acute (ATN, AIN, myeloma) vs. chronic (PCKD, pyelo, autoimmune, analgesic abuse) • Post-Renal/ Obstructive Nephropathy – Malignancy, prostate hyperplasia/ cancer
History and Physical Exam • signs or symptoms of – underlying disorder: i. e. volume status, flank pain, obstruction, diabetes, hypertension, vasculitis – altered kidney function: urine output, urine discoloration, edema – renal failure: anorexia, vomiting, altered mental status, HTN • medications: NSAID, ACEI, analgesics, aminoglycosides, contrast, Chinese herbs

Initial Laboratory Investigations • • • Urinalysis: hematuria, pyuria, proteinuria Urinary Sediment: casts, GN Urine Volume: oliguric, obstruction 24 -hour Urine protein and Cr. Cl Urea: Electrolytes CBC: thrombocytopenia: TTP, HUS; Anemia: cause or effect of renal disease; Leukocytosis: ? pyelo, infection Glucose: DM? Bicarbonate: metabolic acidosis Calcium and Phosphate Protein and albumin Serum protein electrophoresis

Upto. Date

Subsequent Laboratory Investigations Blood Tests • Immunity Studies: ANA, anti-DNA, RF, ANCA, C 3, C 4 • Inflammatory Studies: ESR, CRP • Serology: Hep B, HIV, Bence-Jones • Urinary Eosinophilia: AIN, embolic disease • CK • Liver enzymes, hepatitis: secondary GN
Imaging • Ultrasound – rule out obstruction, stones, mass – small kidneys suggest chronic process – normal sized kidneys do not exclude chronic disease (amyloid, DM, myleoma, PCKD). – Doppler may be used to assess blood flow of arteries (RAS) or veins (thrombosis) • CT Scan - useful for stones and masses • If suspected renal artery stenosis: MR angiography (no nephrotoxic dye), renal angiogram
Renal Biopsy • Should be considered: – if noninvasive tests have failed to establish a diagnosis in a patient with: • nephrotic syndrome (except in DM) • Certain cases of non-nephrotic proteinuria if associated with renal dysfunction • Lupus nephritis (for dx and staging) • acute nephritic syndrome • unexplained acute/ subacute renal failure • to differentiate GN from vasculitis – to direct and evaluate effectiveness of therapy

Management of Renal Disease • Treatment of Reversible Causes • Preventing or Slowing Progression – Hypertension Control (<130/80) – Control Proteinuria (<500 -1000 mg/day or 60% from baseline values) • Treating and Preventing the Complications • Identifying Individuals Requiring Renal Replacement Therapy

Hypertension • Controlling BP slows progression of disease • target <125/80, lower if normotensive at baseline or with more proteinuria • Slowing of disease is related to decreased systemic BP, decreased glomerular hypertension, and decreased urine protein excretion • Microalbuminuria is a major cardiovascular risk factor!
AII Inhibition • ACEI/ ARBS are more effective than other medications in slowing progression: – Also benefit normotensive diabetics – Secondary actions include decrease glomerular remodelling • preferential antiproteinuric effect • decreases AII effects • slows the progression of renal disease in type 1 and 2 DM independent of the effect on BP • in nondiabetics, most convincing effect is in patients with greater proteinuria

Other Antihypertensives • ARB: – benefit similar to ACEI seen in DM-2 – may be additive benefit with ACEI • Verapamil, Diltiazem or beta-blocker – antiproteinuric effect in diabetics • Other medications to achieve BP goals

Diet: Protein Restriction • Dietary protein restriction (0. 4 -0. 6 g/kg/day) reduced the risk for renal failure or death in nondiabetic renal disease and slowed nephropathy in type I DM • beneficial effects were unrelated to change in blood pressure or glycemic control. • NNT 5 to 50 • realistic to restrict to 0. 8 -1 g/kg/day Ann Intern Med. 1996 April 1; 124: 627 -32.

Dyslipidemia • Abnormal lipid metabolism is common in RF • Primary problem is hypertriglyceridemia – LDL, HDL, chol may also be deranged • CRF is considered a high cardiovascular risk and therefore target lipid levels are as those with CAD • Some suggest that statins may benefit the kidney independent of lipid lowering effects

Erythropoietin • Indicated for Hgb <110 • Chk iron stores, folate, and B 12 • In patients with ferritin <100 and sat <20%, must supplement prior to commencement of therapy and continue supplement while on EPO • Follow response to EPO and ensure adequate residual stores
Case • Your patient returns for follow-up after 6 months. He has no new symptoms. You repeat his serum creatinine. It is now 185 (from 155). • At what creatinine level would you refer him to a nephrologist? a) Now (185) b) 250 C) 310

Referral to Nephrologist • Late referral (< 12 months pre dialysis) is common • Survey of Ontario Family MDs: – 84% would not refer with creat 120 -150 (>50% loss of GFR) – 28% would not refer with creat 150 -300 – almost all would refer with creat>300 • Consequences of referral shortly before dialysis: • • more complications longer hospitalization to initiate dialysis more difficulty with initiation of dialysis worse survival! • Better outcomes with early multidisciplinary care CMAJ 1999: 161: 413 -17

Canadian Guidelines • Renal replacement therapy is NOT rationed (i. e. everyone should be considered) • Reversible causes should be sought at diagnosis • At least 1 year is required to prepare for dialysis • Refer, at the latest, at Cr clearance of 30 ml/min, or Cr of 300 • But…there are probably not enough nephrologists/ clinics to meet this demand – Adequate communication with the Nephrologist will allow proper stratification of patients CMAJ 1999: 161: 413 -17

For AIMGP Clinic • It is reasonable to follow stable renal failure patients, and work up and manage appropriately • Refer to nephrology when: – Cr >300 or Cr clearance <30 ml/min – Renal biopsy indicated – Indicators of aggressive disease are present: • • • Rapid decline in creatinine homeostatic derangement i. e. acidosis, volume overload, high K high protein excretion Difficult to control BP low HDL black race
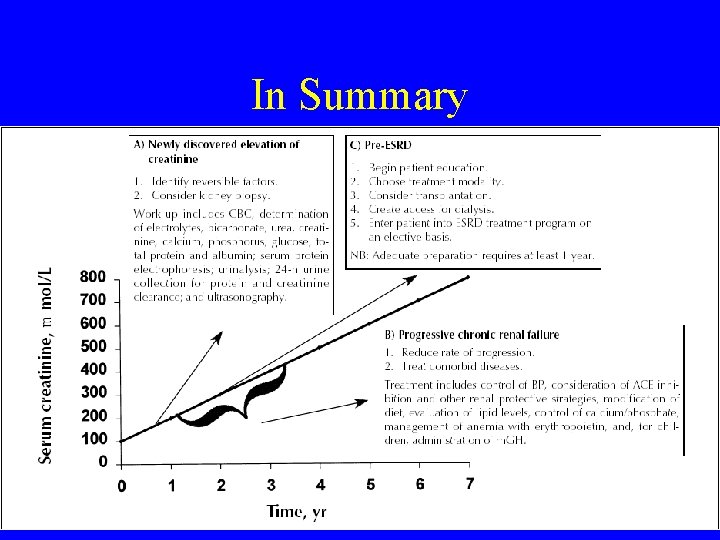
In Summary
Conclusions • When evaluating a patient with increased creatinine, internists should: – Identify and treat reversible causes of renal failure – Initiate management to slow the decline in renal function – Manage coexisting conditions – Have clear indications for when to refer to nephrology subspecialists
References • Elevated Serum creatinine: recommendations for management and referral. CMAJ 1999: 161: 41317 • Approach to managing elevated creatinine. Can Fam Physician. 2004; 50: 735 -740. • Upto. Date
- Slides: 28