APPROACH TO PERIODIC FEVER SYNDROMES Sarah S Long







- Slides: 39
APPROACH TO PERIODIC FEVER SYNDROMES Sarah S. Long, M. D. Professor of Pediatrics Drexel University College of Medicine Chief, Section of Infectious Diseases St. Christopher’s Hospital for Children Dr. Long has no conflict to disclose
Case A 15 -year-old girl is referred because of a persistent febrile illness. Twelve weeks ago she had the acute onset of fever to 1030, headache, myalgia, sore throat and nasal congestion. A throat culture was negative for group A streptococcus. Over the next week high fever and congestion abated but parents report that she has had persisting low grade fever (to 99. 8 every 2 -3 days), complains of headache, sore throat, weakness, fatigue, and has poor color, poor appetite. She complains of sudden shooting pains in arms and legs.
Case continued On attempt to return to school 4 weeks ago she was there only 2 hours when the school nurse reported that the patient felt faint, chilly and sweaty, and was unable to stay in class. She has not returned to school and is now home tutored. What is your next diagnostic step?
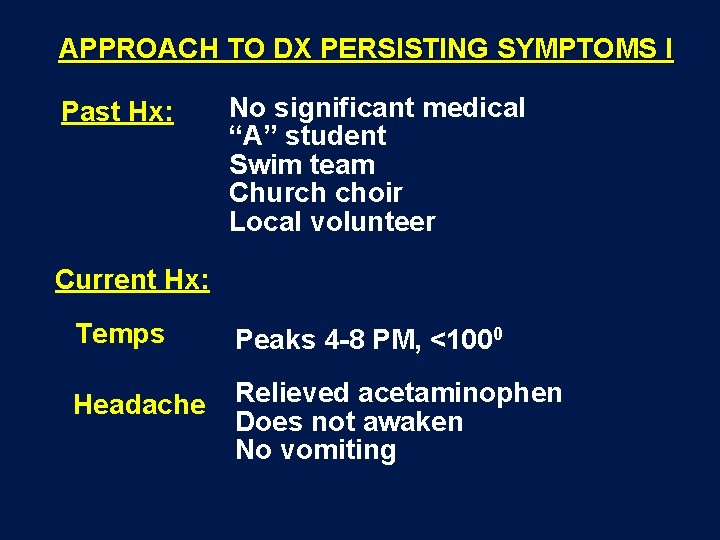
APPROACH TO DX PERSISTING SYMPTOMS I Past Hx: No significant medical “A” student Swim team Church choir Local volunteer Current Hx: Temps Peaks 4 -8 PM, <1000 Headache Relieved acetaminophen Does not awaken No vomiting
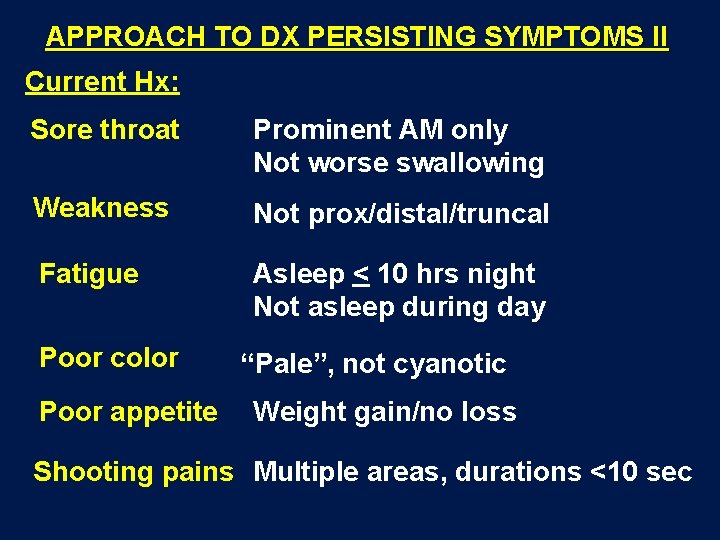
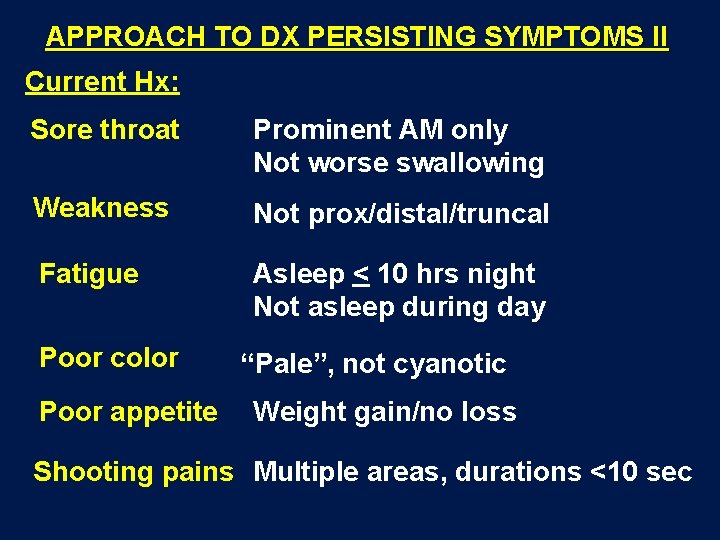
APPROACH TO DX PERSISTING SYMPTOMS II Current Hx: Sore throat Prominent AM only Not worse swallowing Weakness Not prox/distal/truncal Fatigue Asleep < 10 hrs night Not asleep during day Poor color Poor appetite “Pale”, not cyanotic Weight gain/no loss Shooting pains Multiple areas, durations <10 sec
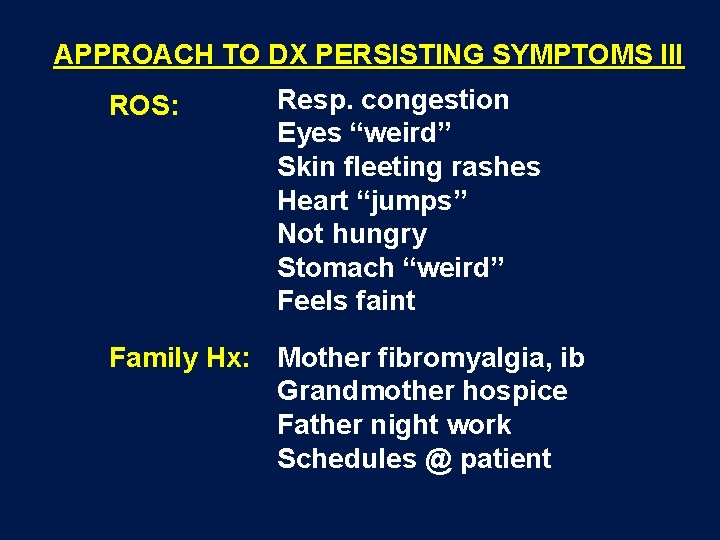
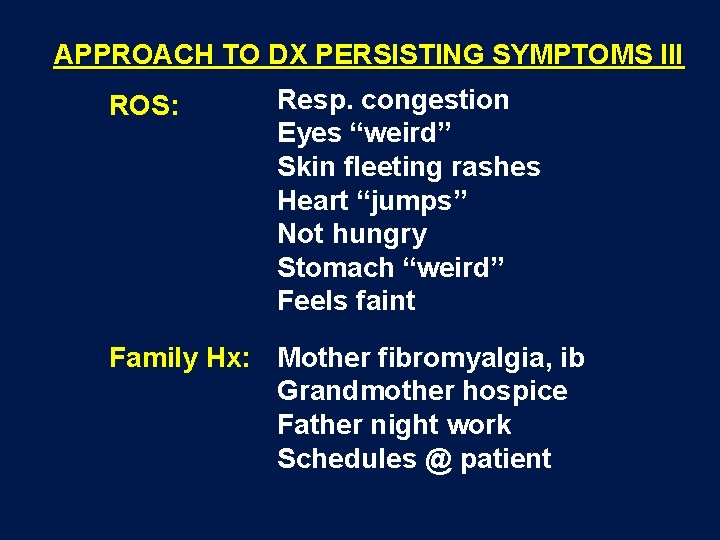
APPROACH TO DX PERSISTING SYMPTOMS III ROS: Resp. congestion Eyes “weird” Skin fleeting rashes Heart “jumps” Not hungry Stomach “weird” Feels faint Family Hx: Mother fibromyalgia, ib Grandmother hospice Father night work Schedules @ patient
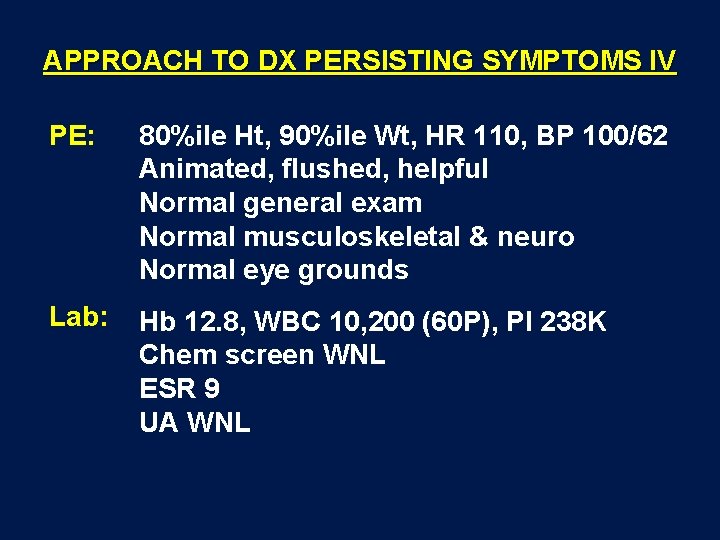
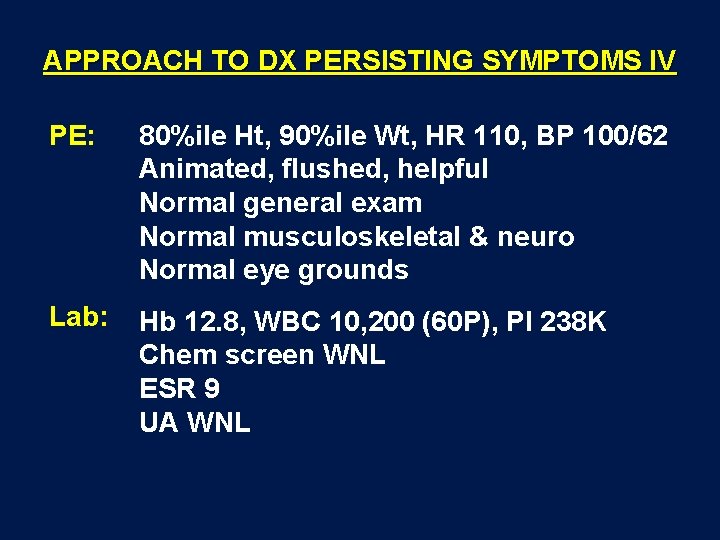
APPROACH TO DX PERSISTING SYMPTOMS IV PE: 80%ile Ht, 90%ile Wt, HR 110, BP 100/62 Animated, flushed, helpful Normal general exam Normal musculoskeletal & neuro Normal eye grounds Lab: Hb 12. 8, WBC 10, 200 (60 P), Pl 238 K Chem screen WNL ESR 9 UA WNL
What’s the differential diagnosis? What further evaluation should be done?
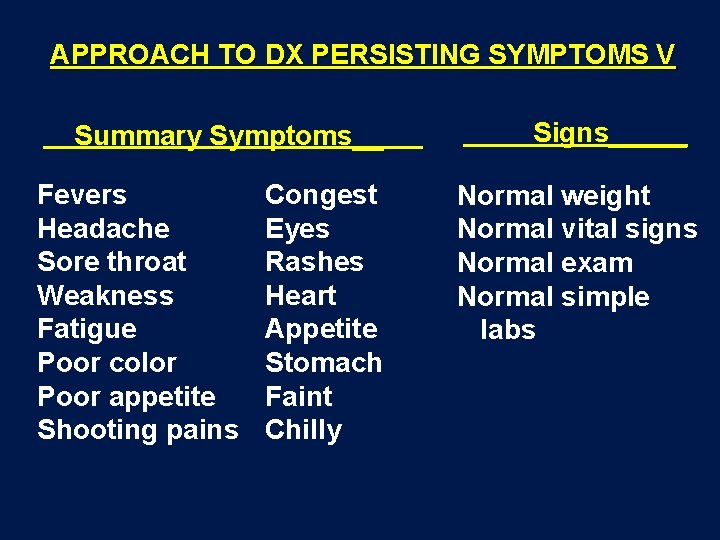
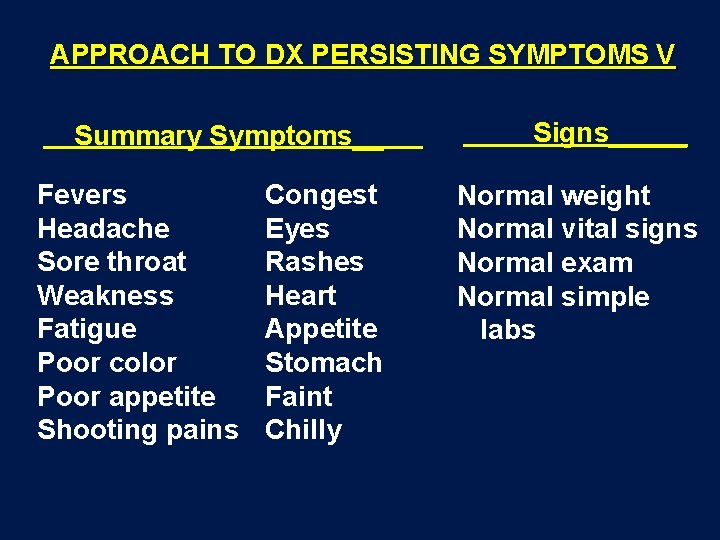
APPROACH TO DX PERSISTING SYMPTOMS V Summary Symptoms__ Fevers Headache Sore throat Weakness Fatigue Poor color Poor appetite Shooting pains Congest Eyes Rashes Heart Appetite Stomach Faint Chilly Signs_____ Normal weight Normal vital signs Normal exam Normal simple labs
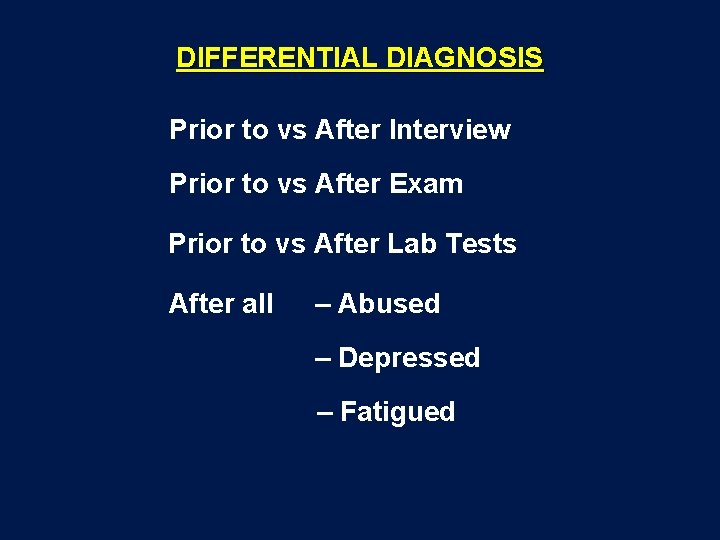
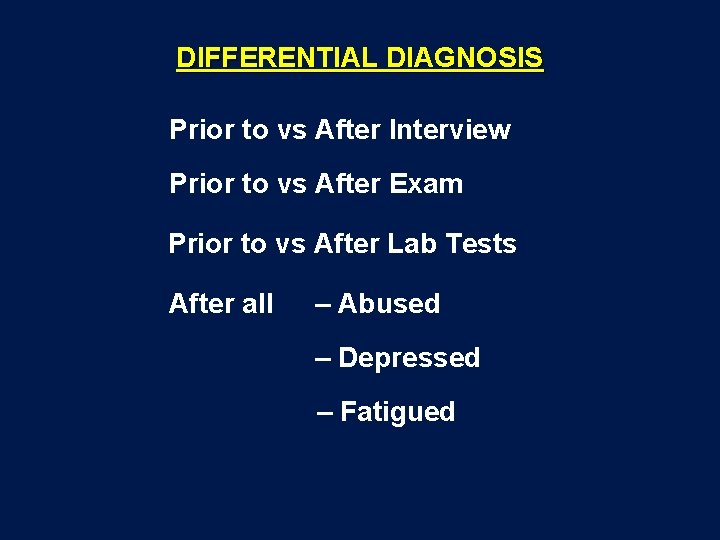
DIFFERENTIAL DIAGNOSIS Prior to vs After Interview Prior to vs After Exam Prior to vs After Lab Tests After all – Abused – Depressed – Fatigued
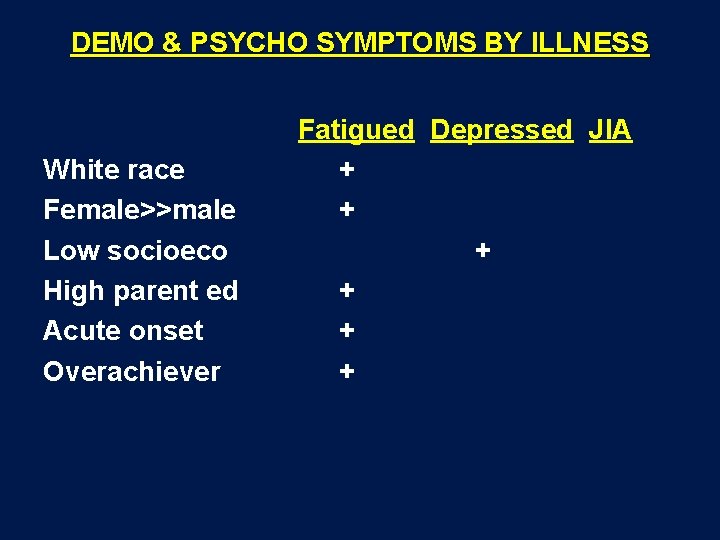
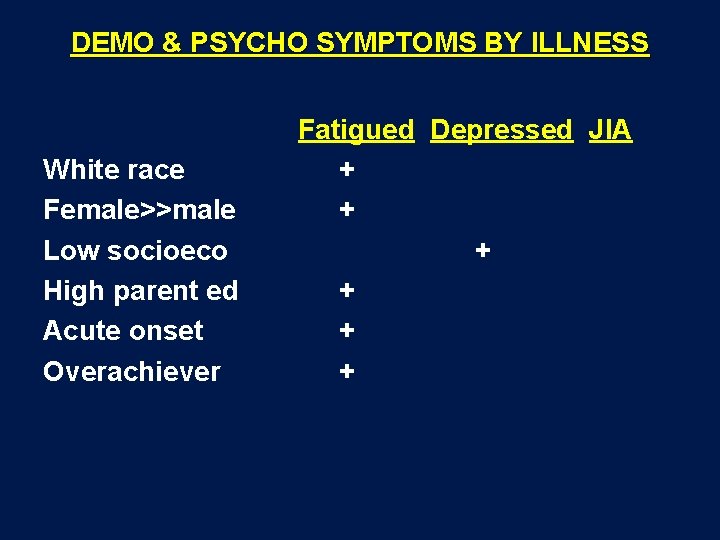
DEMO & PSYCHO SYMPTOMS BY ILLNESS White race Female>>male Low socioeco High parent ed Acute onset Overachiever Fatigued Depressed JIA + + +
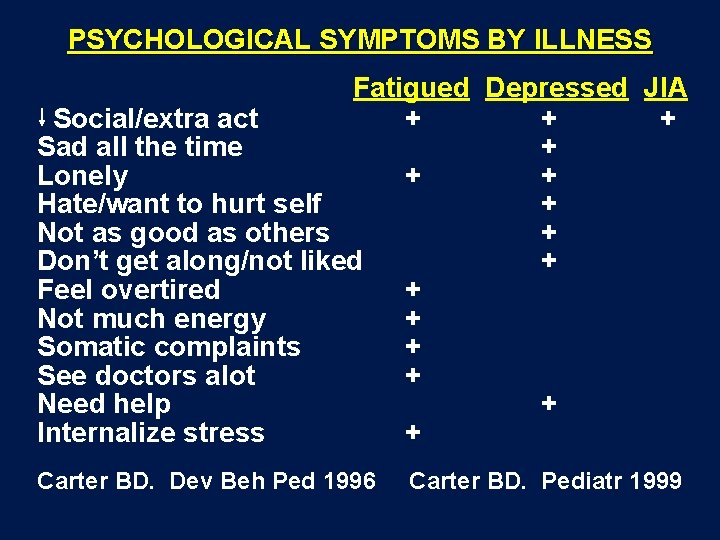
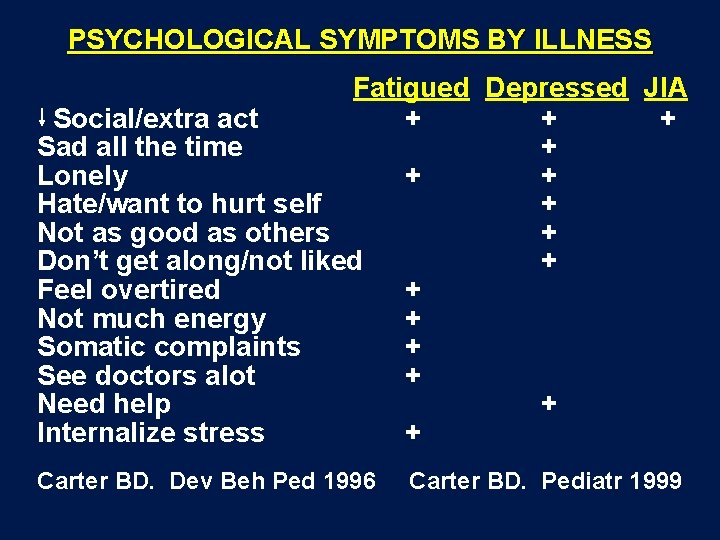
PSYCHOLOGICAL SYMPTOMS BY ILLNESS Fatigued Depressed JIA Social/extra act + + + Sad all the time + Lonely + + Hate/want to hurt self + Not as good as others + Don’t get along/not liked + Feel overtired + Not much energy + Somatic complaints + See doctors alot + Need help + Internalize stress + Carter BD. Dev Beh Ped 1996 Carter BD. Pediatr 1999
TIMELINE EVIDENCE BASE FATIGUE 1990 s NIH definition CFS Case series pediatrics Immunologic studies 2000 s EBV, other ID Lyme, other ID Follow-up case series Non Dx pediatrics Endocrine – hypoadrenia Cardio – neurally med. hypotension – postural tachy “syndrome” Joint hypermobility – ? Ehlers Danlos
EVIDENCE BASE FATIGUE Orthostatic instability in a population-based study of chronic fatigue syndrome. Jones JF et al. Am J Med, December 2005 – 58 adults CFS & 55 controls – Inpatient 2 -day evaluation – Head-up tilt test pos. 30% CFS vs 48% controls Endurance exercise training in orthostatic intolerance: a randomized controlled trial. Winker R et al. Hypertension Mar 2005 – Military recruits 36 orthostatic intol – Randomized to “training” vs “control” x 3 mo – Outcome OI: 6/11 training vs 10/11 control – Symptom scores sig in trained
• • • TYPICAL FINDINGS IN PATIENTS WITH “DECONDITIONING” Age > 12 years Preillness achievement high Family expectations high Acute febrile illness with onset easily dated Family and outside attention high Lengthy list, but vague complaints Odd complaints (eg, “shooting” pains; 30 second “blindness”; stereotypic sporadic, brief unilateral tremors, jerks, or “paralysis”) No daytime sleep Preserved weight Extreme cooperation with examination Normal physical and neurologic examination Normal results of screening laboratory tests
MANAGEMENT “DECONDITIONING” Patient: Validate symptoms as accurate Incremental, forced return to school Exercise Predict symptoms No school absence w/o ped. visit No expectation performance Family: Validate their concern Validate their medical pursuit Justify your diagnosis Change focus to health Avoid “How do you feel? ” No expectation performance 10 Provider = Quarterback Long approach >1975
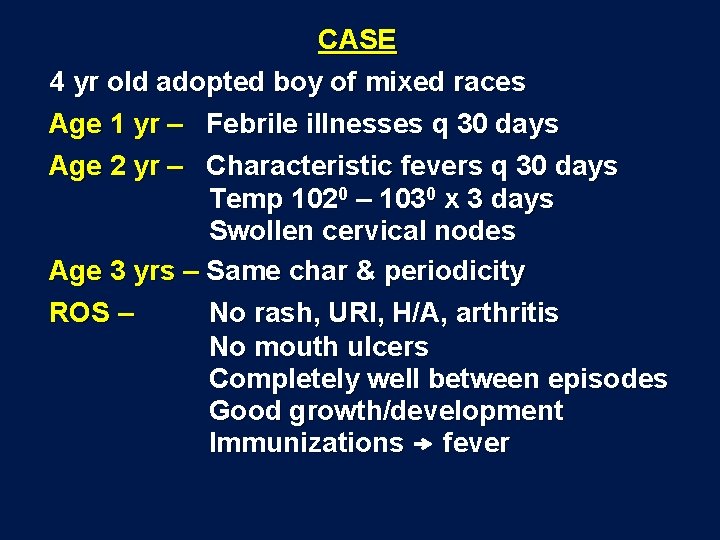
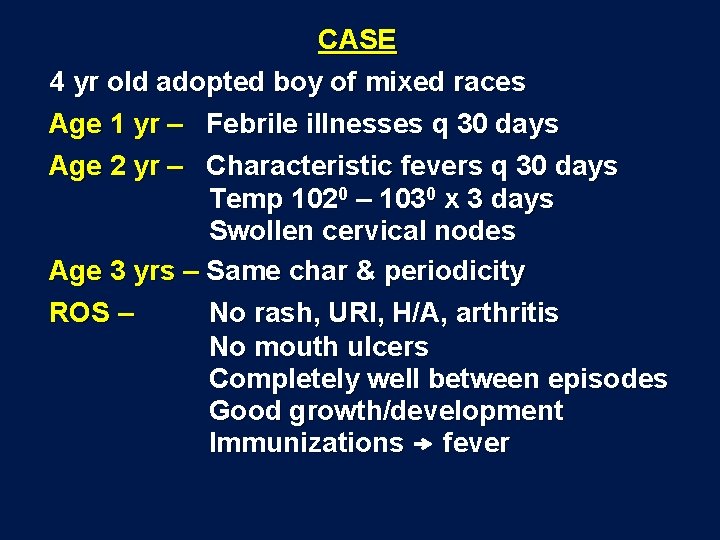
CASE 4 yr old adopted boy of mixed races Age 1 yr – Febrile illnesses q 30 days Age 2 yr – Characteristic fevers q 30 days Temp 1020 – 1030 x 3 days Swollen cervical nodes Age 3 yrs – Same char & periodicity ROS – No rash, URI, H/A, arthritis No mouth ulcers Completely well between episodes Good growth/development Immunizations fever
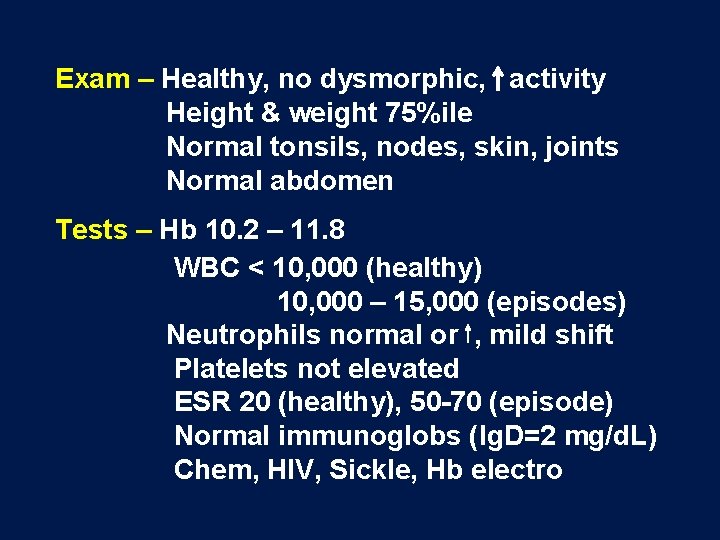
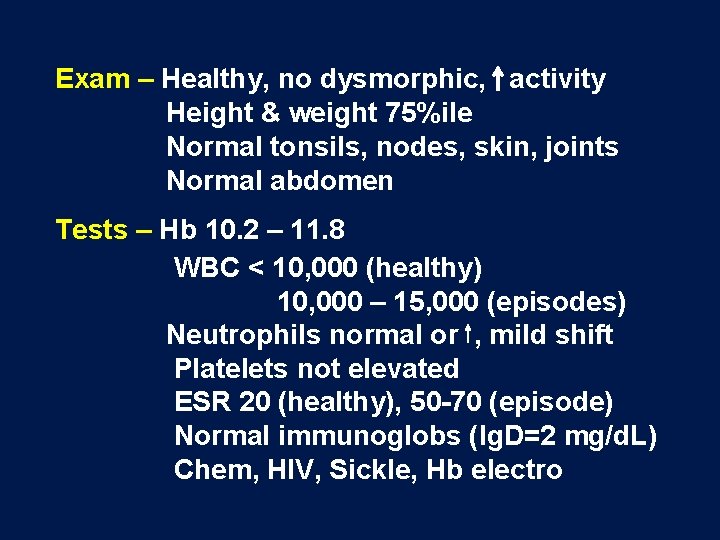
Exam – Healthy, no dysmorphic, activity Height & weight 75%ile Normal tonsils, nodes, skin, joints Normal abdomen Tests – Hb 10. 2 – 11. 8 WBC < 10, 000 (healthy) 10, 000 – 15, 000 (episodes) Neutrophils normal or , mild shift Platelets not elevated ESR 20 (healthy), 50 -70 (episode) Normal immunoglobs (Ig. D=2 mg/d. L) Chem, HIV, Sickle, Hb electro
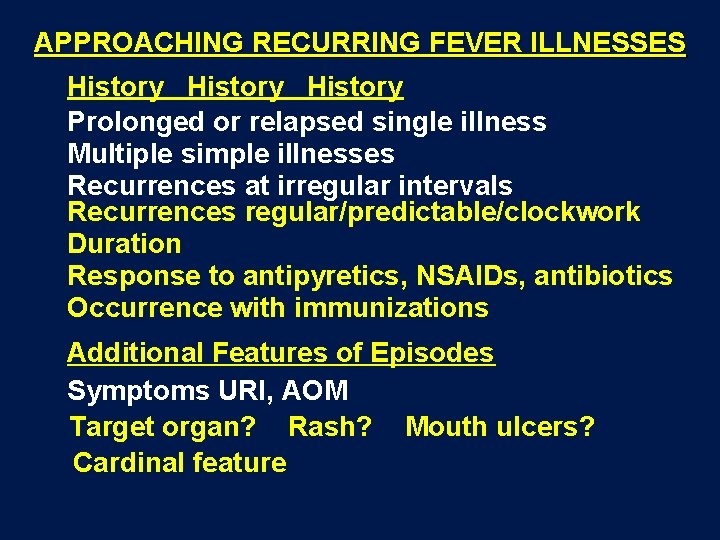
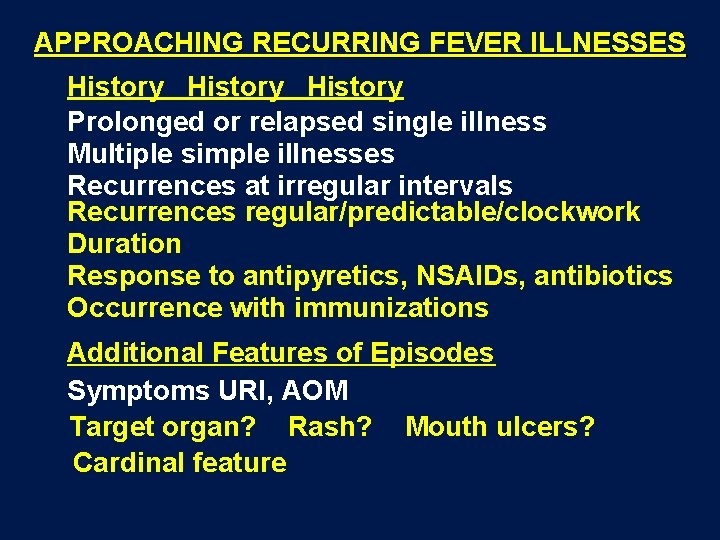
APPROACHING RECURRING FEVER ILLNESSES History Prolonged or relapsed single illness Multiple simple illnesses Recurrences at irregular intervals Recurrences regular/predictable/clockwork Duration Response to antipyretics, NSAIDs, antibiotics Occurrence with immunizations Additional Features of Episodes Symptoms URI, AOM Target organ? Rash? Mouth ulcers? Cardinal feature

MORE HISTORY Interval between episodes Lingering symptoms Multiple URIs, asthma Severe bacterial/viral infections Perfectly well, energetic Few “regular” illnesses Good growth & development Family History Genetic background Sibs not ill with patient Autoimmune, -inflammatory dis Amyloidosis Parent w fevers as child

PHYSICAL EXAMINATION Growth chart Thorough general Target organ Mouth ulcers, rashes, joints, nodes TESTS Simple - during episode & interval CBC, Chem, ESR Immunoglobulins Urine culture Imaging only as directed by exam
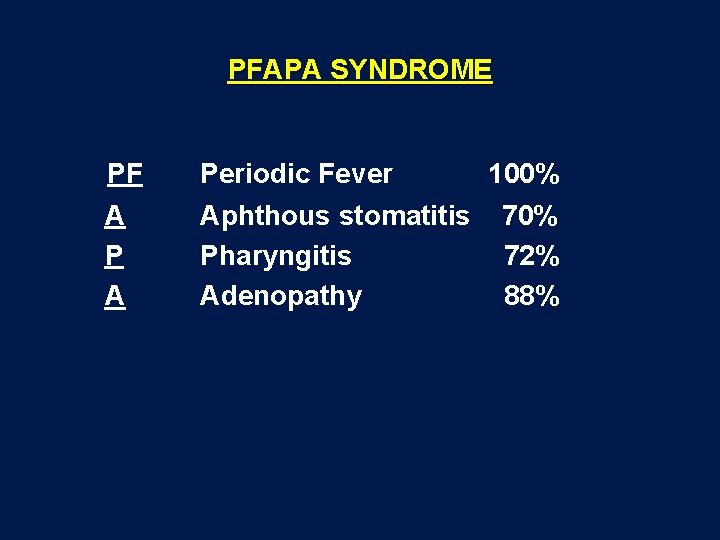
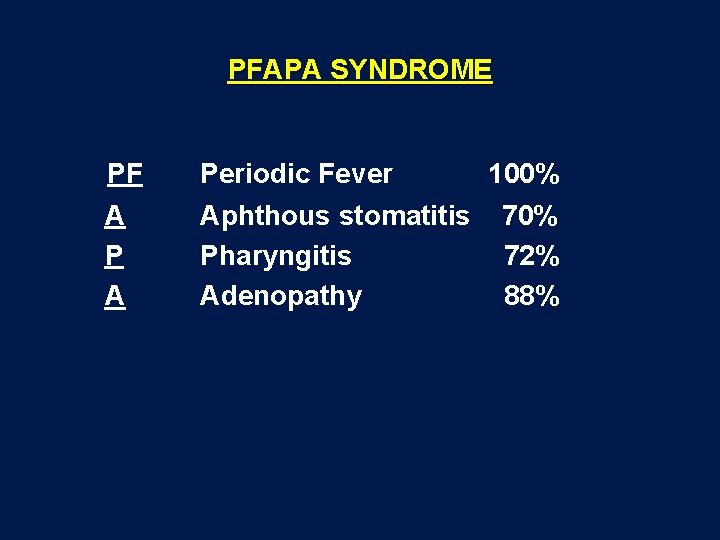
PFAPA SYNDROME PF Periodic Fever A P A Aphthous stomatitis Pharyngitis Adenopathy 100% 72% 88%
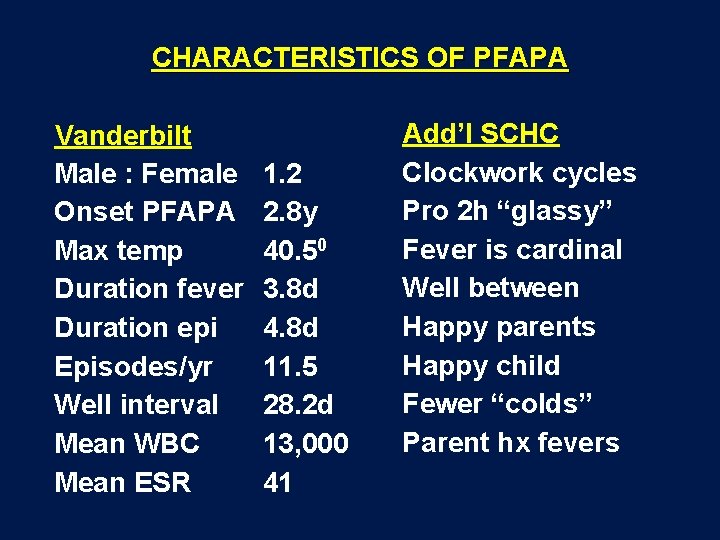
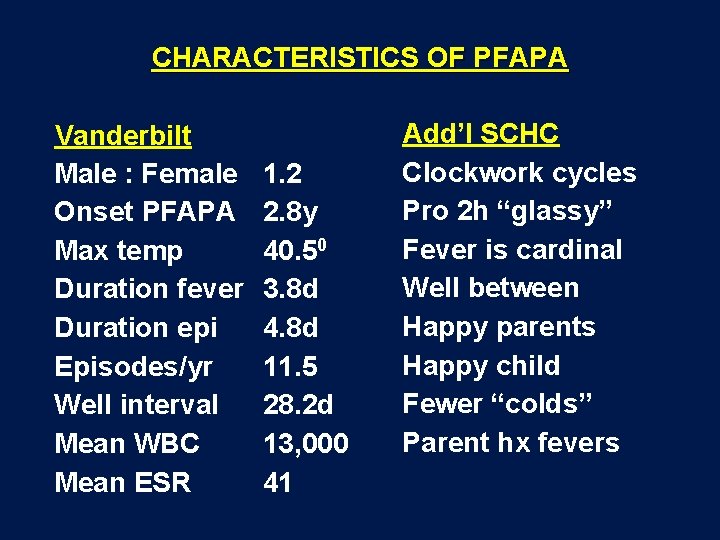
CHARACTERISTICS OF PFAPA Vanderbilt Male : Female Onset PFAPA Max temp Duration fever Duration epi Episodes/yr Well interval Mean WBC Mean ESR 1. 2 2. 8 y 40. 50 3. 8 d 4. 8 d 11. 5 28. 2 d 13, 000 41 Add’l SCHC Clockwork cycles Pro 2 h “glassy” Fever is cardinal Well between Happy parents Happy child Fewer “colds” Parent hx fevers
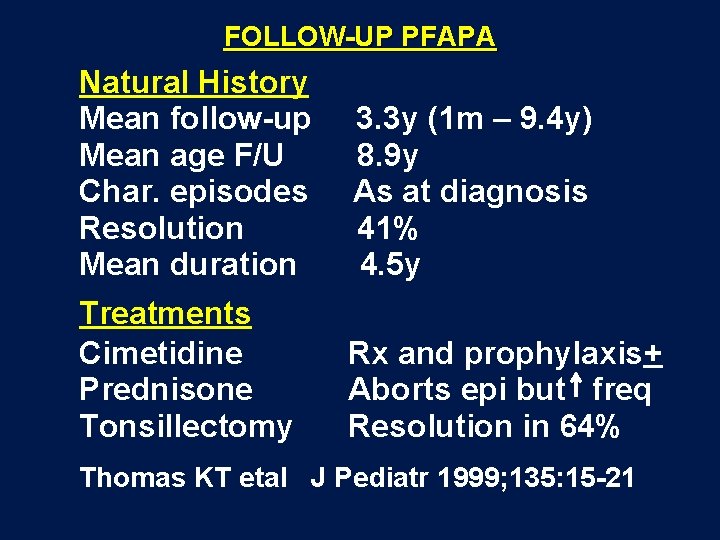
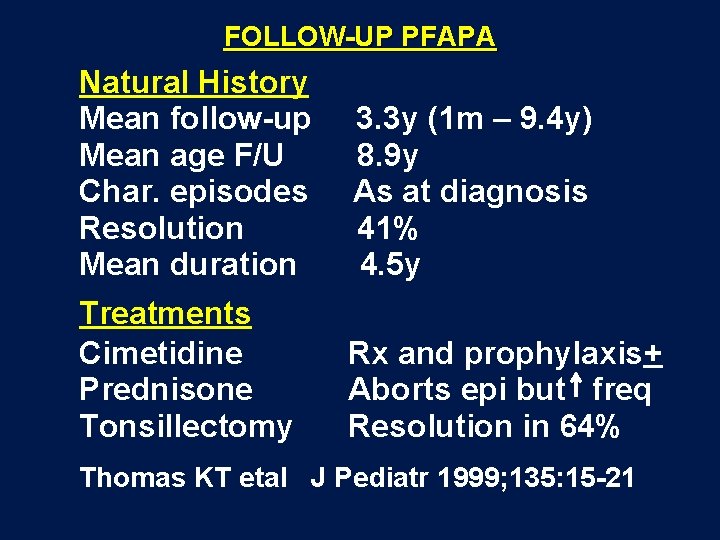
FOLLOW-UP PFAPA Natural History Mean follow-up Mean age F/U Char. episodes Resolution Mean duration 3. 3 y (1 m – 9. 4 y) 8. 9 y As at diagnosis 41% 4. 5 y Treatments Cimetidine Prednisone Tonsillectomy Rx and prophylaxis+ Aborts epi but freq Resolution in 64% Thomas KT etal J Pediatr 1999; 135: 15 -21
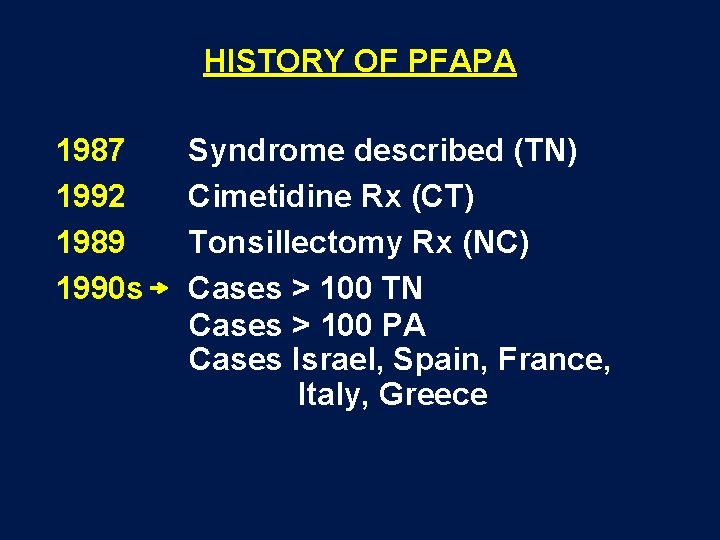
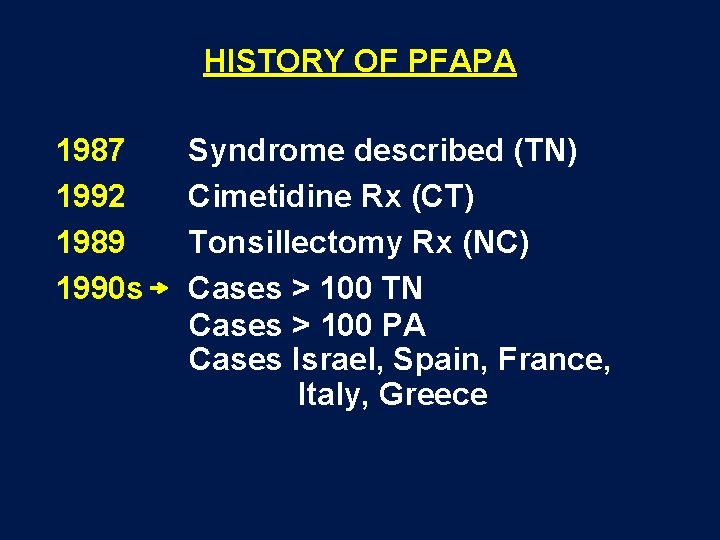
HISTORY OF PFAPA 1987 1992 1989 1990 s Syndrome described (TN) Cimetidine Rx (CT) Tonsillectomy Rx (NC) Cases > 100 TN Cases > 100 PA Cases Israel, Spain, France, Italy, Greece
Resolution of PFAPA post tonsillectomy
WHAT IT ISN’T WHAT IS IT? “K I N E C T I O N”

MANAGEMENT PFAPA Diagnosis – Clinical “best” (Tests: Ig. A&D, WBCs) – Re-visit – Beware “extra” S&S – Must be well between Management (Sequential) – Support +Cimetidine +Pred dx trial + Pred special circ + Tonsillectomy GET HELP IF “OFF” EXPECTED
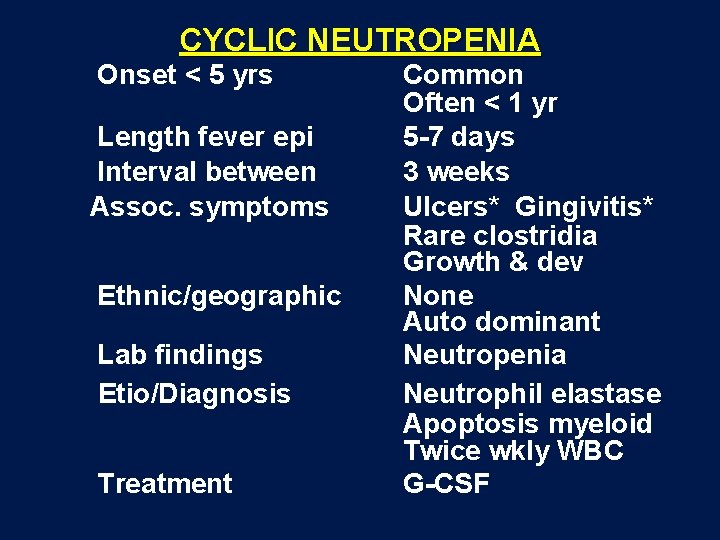
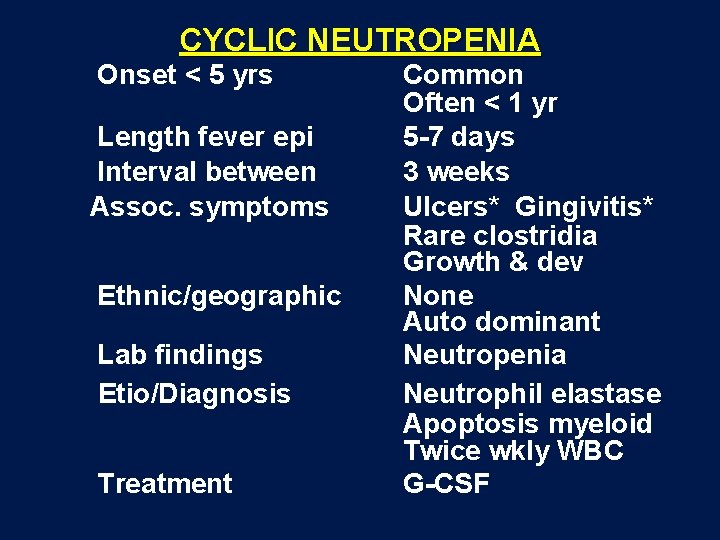
CYCLIC NEUTROPENIA Onset < 5 yrs Length fever epi Interval between Assoc. symptoms Ethnic/geographic Lab findings Etio/Diagnosis Treatment Common Often < 1 yr 5 -7 days 3 weeks Ulcers* Gingivitis* Rare clostridia Growth & dev None Auto dominant Neutropenia Neutrophil elastase Apoptosis myeloid Twice wkly WBC G-CSF

Autoinflammatory syndromes – Seemingly unprovoked inflammation without significant autoantibodies and autoreactive T lymphocytes Mc. Dermott
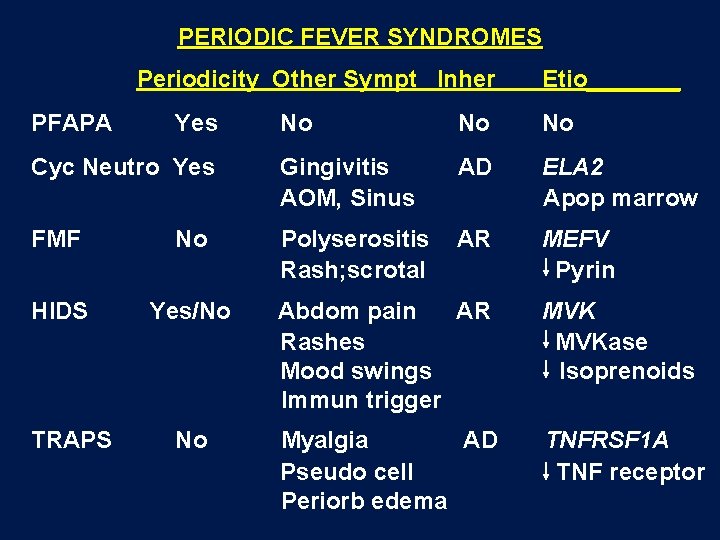
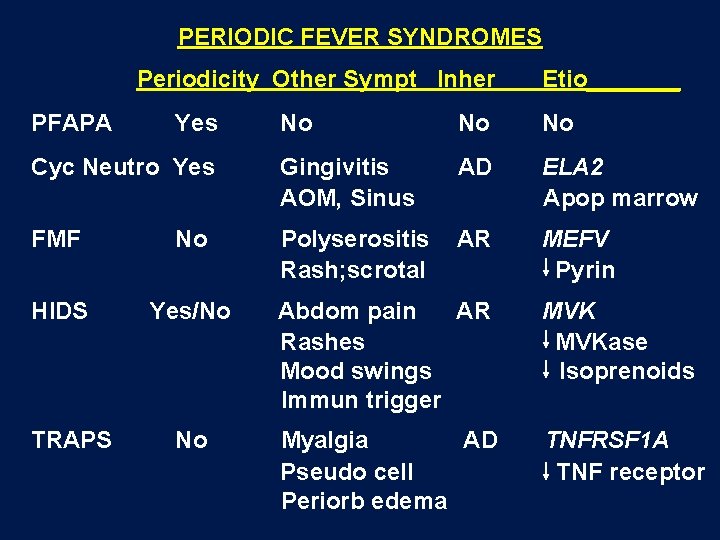
PERIODIC FEVER SYNDROMES Periodicity Other Sympt Inher PFAPA No No No Cyc Neutro Yes Gingivitis AOM, Sinus AD ELA 2 Apop marrow FMF No Polyserositis Rash; scrotal AR MEFV Pyrin HIDS Yes/No Abdom pain AR Rashes Mood swings Immun trigger MVKase Isoprenoids No Myalgia AD Pseudo cell Periorb edema TNFRSF 1 A TNF receptor TRAPS Yes Etio_______
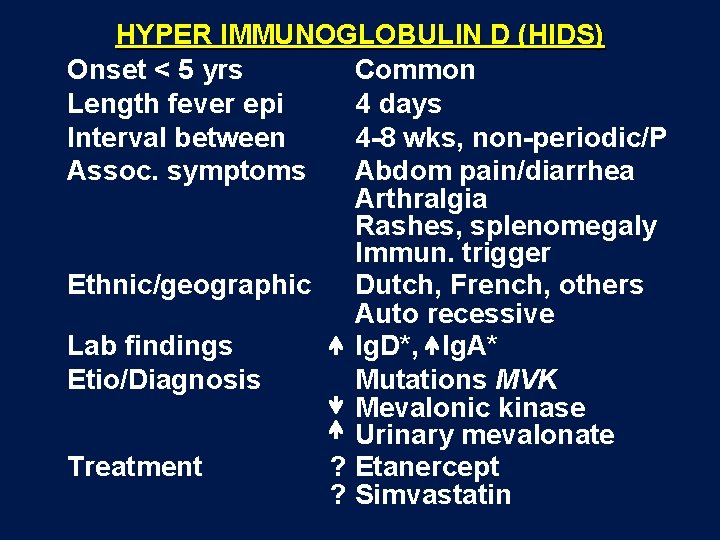
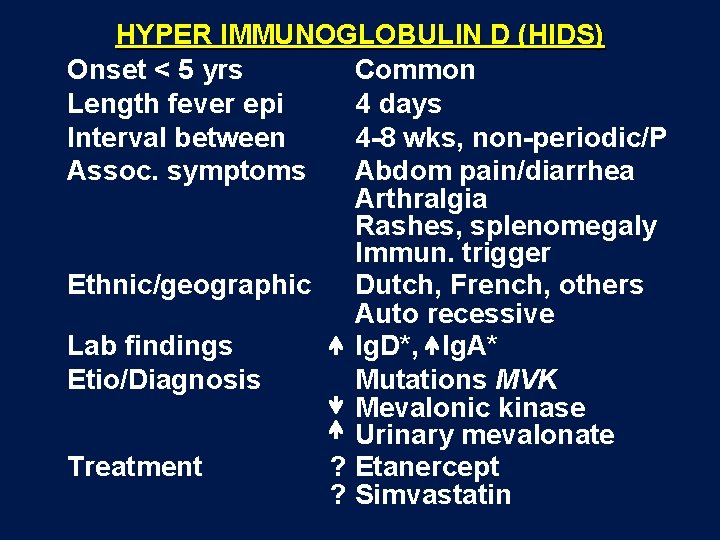
HYPER IMMUNOGLOBULIN D (HIDS) Onset < 5 yrs Common Length fever epi 4 days Interval between 4 -8 wks, non-periodic/P Assoc. symptoms Abdom pain/diarrhea Arthralgia Rashes, splenomegaly Immun. trigger Ethnic/geographic Dutch, French, others Auto recessive Lab findings Ig. D*, Ig. A* Etio/Diagnosis Mutations MVK Mevalonic kinase Urinary mevalonate Treatment ? Etanercept ? Simvastatin
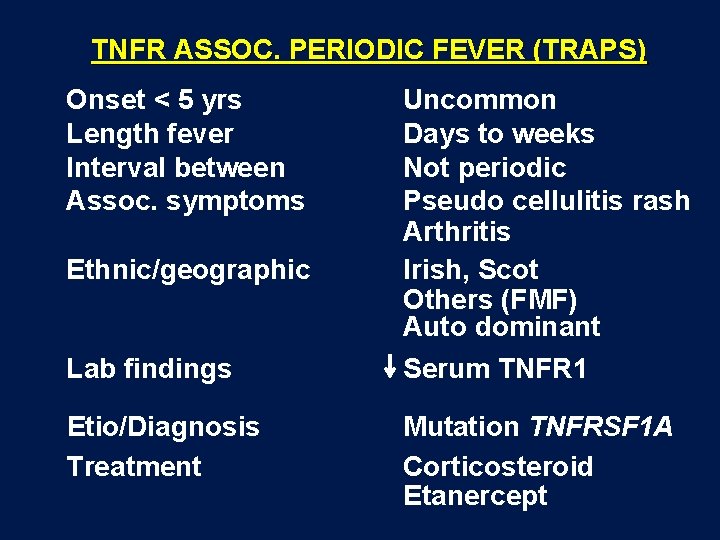
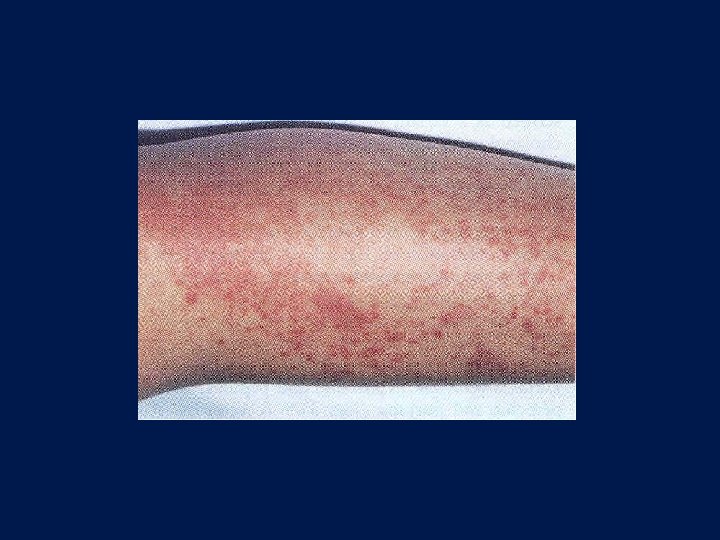
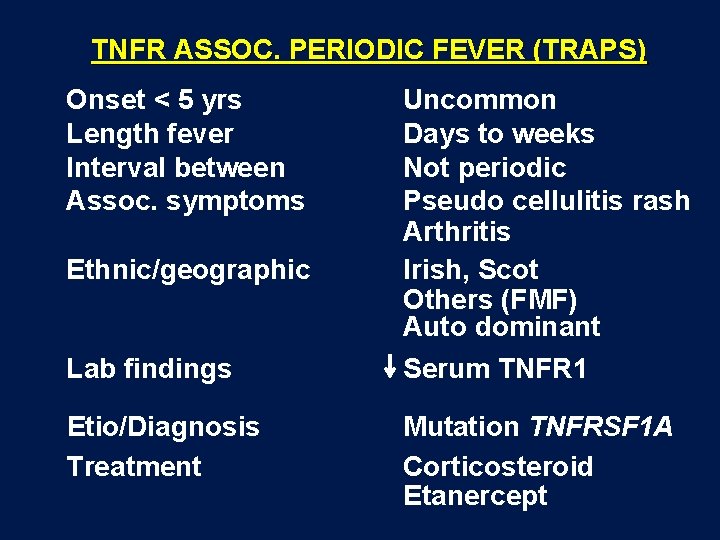
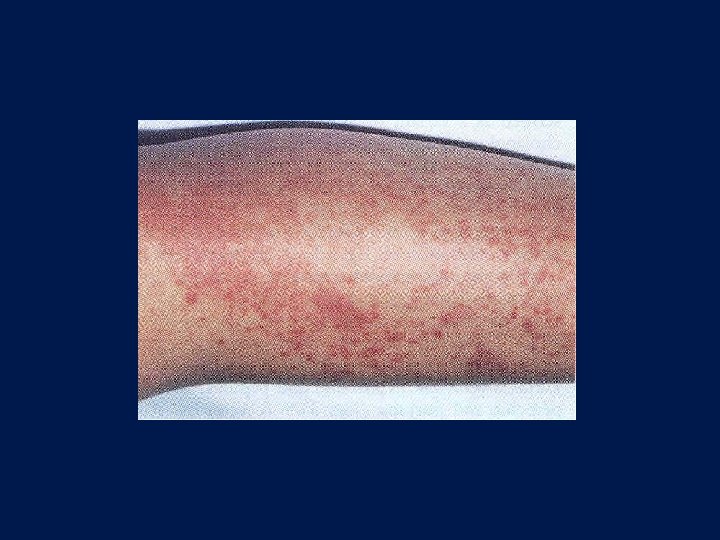
TNFR ASSOC. PERIODIC FEVER (TRAPS) Onset < 5 yrs Length fever Interval between Assoc. symptoms Ethnic/geographic Lab findings Etio/Diagnosis Treatment Uncommon Days to weeks Not periodic Pseudo cellulitis rash Arthritis Irish, Scot Others (FMF) Auto dominant Serum TNFR 1 Mutation TNFRSF 1 A Corticosteroid Etanercept

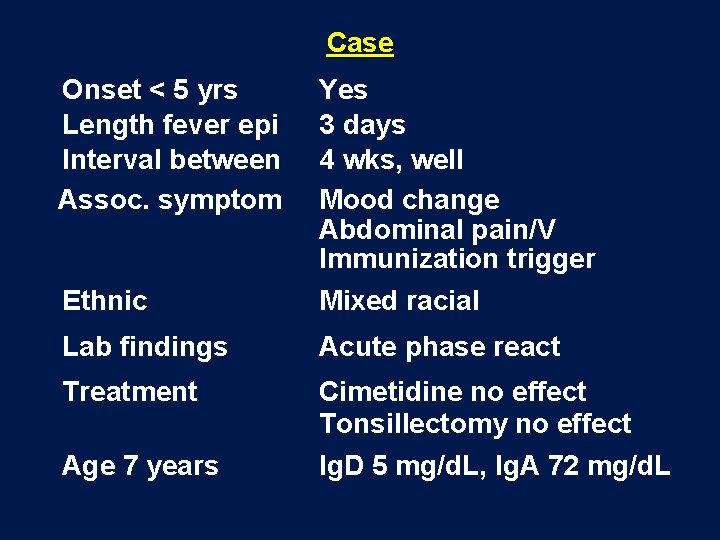
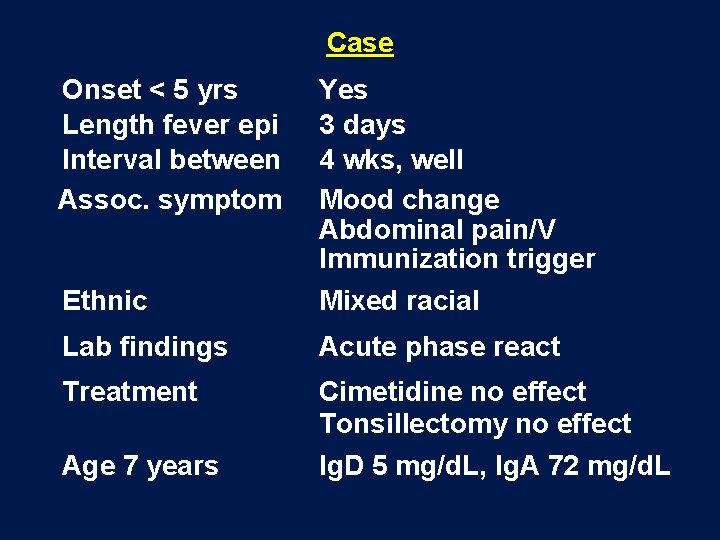
Case Onset < 5 yrs Length fever epi Interval between Assoc. symptom Yes 3 days 4 wks, well Mood change Abdominal pain/V Immunization trigger Ethnic Mixed racial Lab findings Acute phase react Treatment Cimetidine no effect Tonsillectomy no effect Age 7 years Ig. D 5 mg/d. L, Ig. A 72 mg/d. L

Missense mutations MVK HIDS
