Approach To Patient With Iron Deficiency Anaemia By
Approach To Patient With Iron Deficiency Anaemia By Sin Kaan Chan 11/7/02
Scenario A 40 years old lady, presented with pallor, lethargy, palpitations and SOB on exertion. FBC: Hb 7. 5 g/dl MCV 64 fl MCH 18. 5 pg WBC and differential normal Platelet normal range What is next?
Differential Diagnosis of Hypochromic Microcytic Anaemia Fe deficiency n Anaemia of chronic disease n Thalassaemia n Sideroblastic anaemia (rare) n
Causes of Iron Deficiency Bleeding: n n Menorrhagia GI bleed Peptic ulcer Oesophageal varices Aspirin ingestion Hookworm Neoplasm IBD Haemorrhoids
Factors contributing to Iron Deficiency Increased demands: n Pregnancy (commonest factor and increases with parity) n Growth (infancy and adolescent) n Erythropoietin therapy

Causes of Iron Deficiency Malabsorption: n Gluten-induced enteropathy n Gastrectomy Poor diet
History Any ongoing bleeding? n Menstrual history n Passing bloody stool / black stool n Any abdominal symptoms? n Easy bruising or bleed? (clotting or platelet ab. N) n Medications n Diet n How long has the patient been anaemic? n
History n Past medical history: Any chronic diseases? (renal, liver, connective tissue…etc) n Family history: Thalassaemia, cancer, other illness n Social History: Racial origin (thalassaemia more common in Mediterranean/Southern Asian) Smoking, alcohol Vegetarian
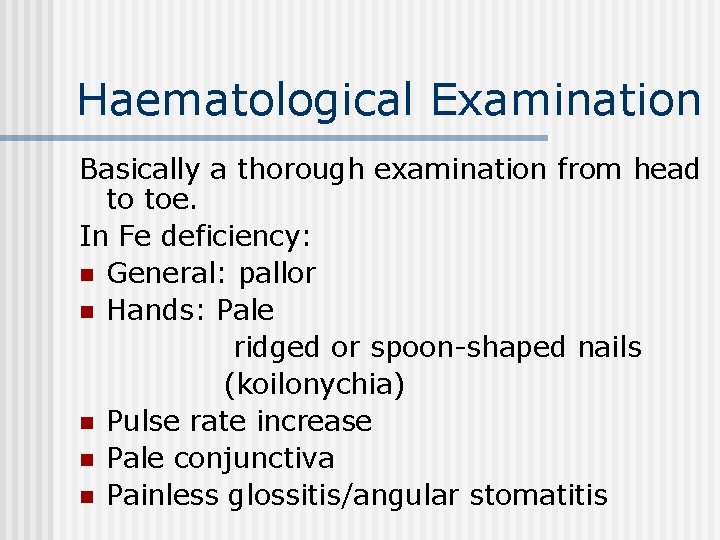
Haematological Examination Basically a thorough examination from head to toe. In Fe deficiency: n General: pallor n Hands: Pale ridged or spoon-shaped nails (koilonychia) n Pulse rate increase n Pale conjunctiva n Painless glossitis/angular stomatitis
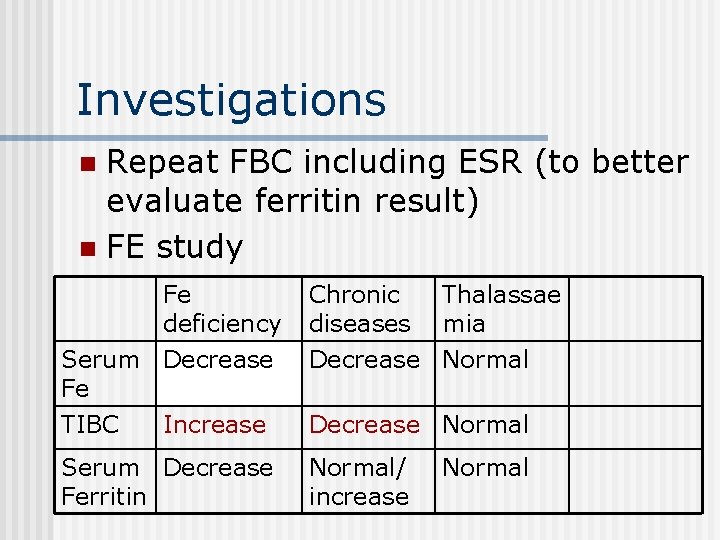
Investigations Repeat FBC including ESR (to better evaluate ferritin result) n FE study n Fe deficiency Chronic diseases Thalassae mia Serum Decrease Fe Decrease Normal TIBC Decrease Normal Increase Serum Decrease Ferritin Normal/ increase Normal
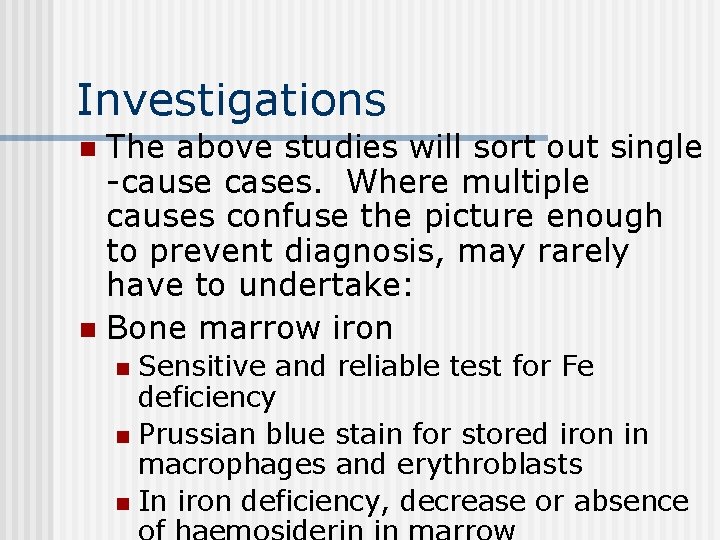
Investigations The above studies will sort out single -cause cases. Where multiple causes confuse the picture enough to prevent diagnosis, may rarely have to undertake: n Bone marrow iron n Sensitive and reliable test for Fe deficiency n Prussian blue stain for stored iron in macrophages and erythroblasts n In iron deficiency, decrease or absence n
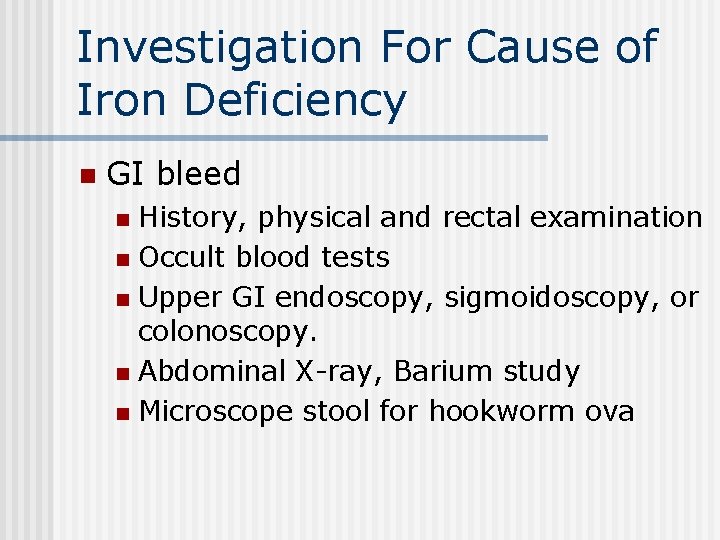
Investigation For Cause of Iron Deficiency n GI bleed History, physical and rectal examination n Occult blood tests n Upper GI endoscopy, sigmoidoscopy, or colonoscopy. n Abdominal X-ray, Barium study n Microscope stool for hookworm ova n

Investigation For Cause of Iron Deficiency n Malabsorption If history highly suspected, - Test for endomysial and gluten antibodies. - Duodenal biopsy
Management Principle: n Determine and treat underlying cause. n Correct anemia and replenish iron stores by oral iron.
Oral Iron Ferrous sulphate n Ferrous gluconate n Should be given long enough to correct anaemia and replenish iron stores. Therefore given for at least 6 months. n
Failure to Response to Oral Iron n n Possible cause considered b 4 parenteral iron used. Possible causes: n n n Continuing bleeding Failure to take tablets Wrong dx – thalassaemia trait / sideroblastic anaemia Other causes – malignancy, inflammation Malabsorption

Parenteral Iron-sorbitol-citrate Repeated deep IM injections n Ferric hydroxide-sucrose Slow IV injection or infusion n May have hypersensitivity or anaphylactic reaction n
Summary…… n Approach to iron deficiency: n Determine and treat the underlying cause!
- Slides: 18