APPROACH TO JAUNDICE IN NEWBORN PRESENTER Dr Zafar
APPROACH TO JAUNDICE IN NEWBORN PRESENTER: Dr. Zafar Iqbal Senior Resident Dept. of Pediatrics JNMCH, AMU Aligarh
Objectives • Definition of jaundice • Metabolism of bilirubin • Types of jaundice • Causes of neonatal jaundice • Management of neonatal jaundice
Neonatal hyperbilirubinemia Definition : Jaundice is the yellow color of the skin and sclera caused by deposits of bilirubin When is visible ? Adult sclera > 2 mg / dl Newborn skin > 5 mg / dl
Incidence of neonatal jaundice Terms: occurs in 60% Preterm : 80% of preterm neonates Jaundice is the most common condition that requires medical attention in newborns.
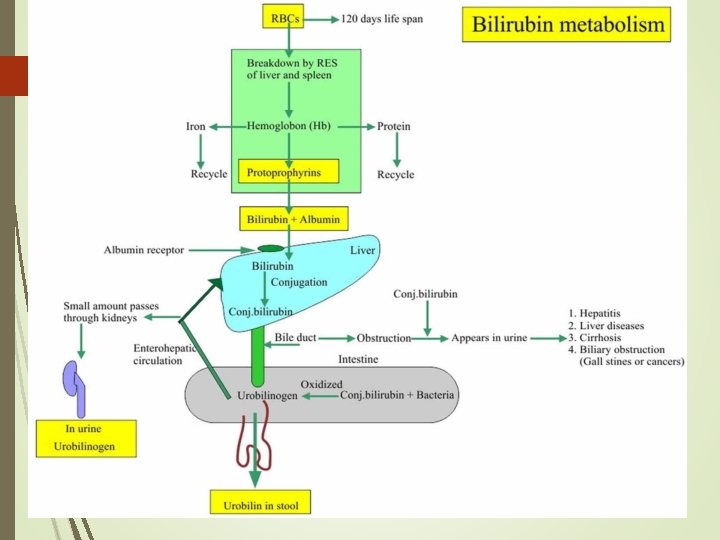
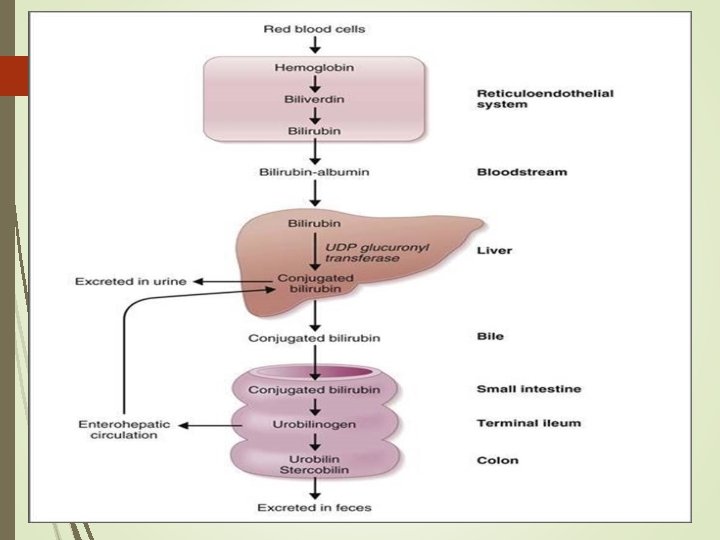
BILIRUBIN METABOLISM
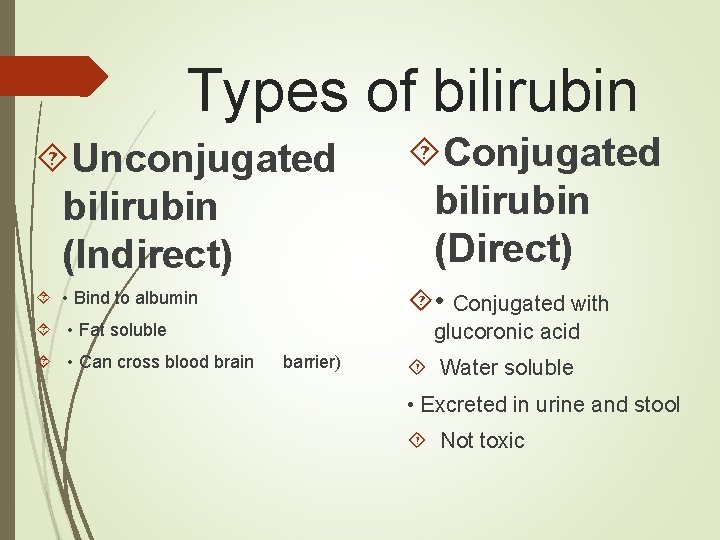
Types of bilirubin Unconjugated bilirubin (Indirect) Conjugated bilirubin (Direct) • Bind to albumin • Conjugated with glucoronic acid • Fat soluble • Can cross blood brain barrier) Water soluble • Excreted in urine and stool Not toxic

Mechanisms of Neonatal Jaundice 1. Increased Bilirubin Load due to a high hemoglobin concentration. • normal newborn infant • Hemolysis • Cephalhematoma or bruising , Polycythemia
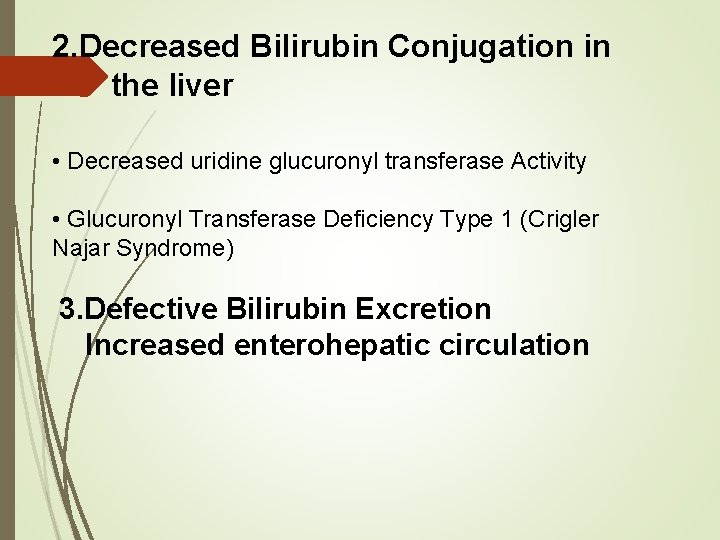
2. Decreased Bilirubin Conjugation in the liver • Decreased uridine glucuronyl transferase Activity • Glucuronyl Transferase Deficiency Type 1 (Crigler Najar Syndrome) 3. Defective Bilirubin Excretion Increased enterohepatic circulation
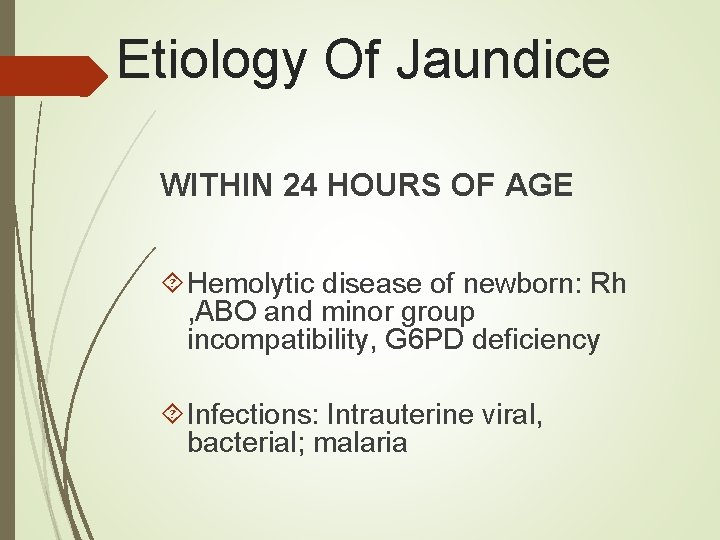
Etiology Of Jaundice WITHIN 24 HOURS OF AGE Hemolytic disease of newborn: Rh , ABO and minor group incompatibility, G 6 PD deficiency Infections: Intrauterine viral, bacterial; malaria
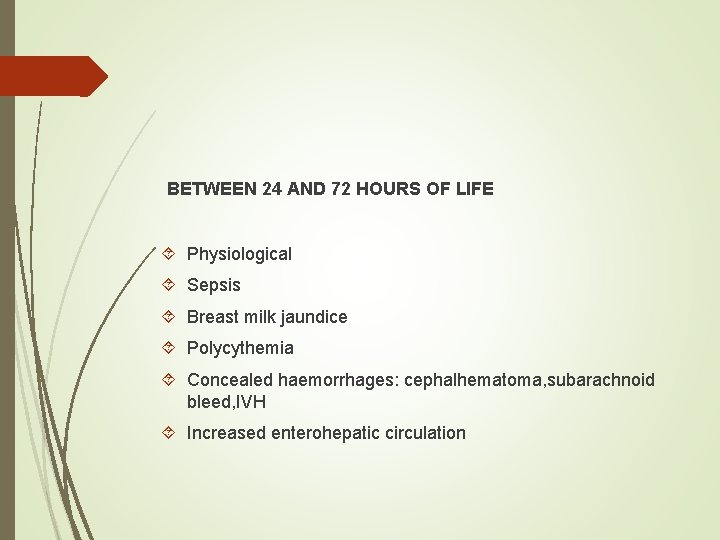
BETWEEN 24 AND 72 HOURS OF LIFE Physiological Sepsis Breast milk jaundice Polycythemia Concealed haemorrhages: cephalhematoma, subarachnoid bleed, IVH Increased enterohepatic circulation

AFTER 72 HOURS Sepsis Neonatal hepatitis Extrahepatic biliary atresia Metabolic disorders Hypothyroidism
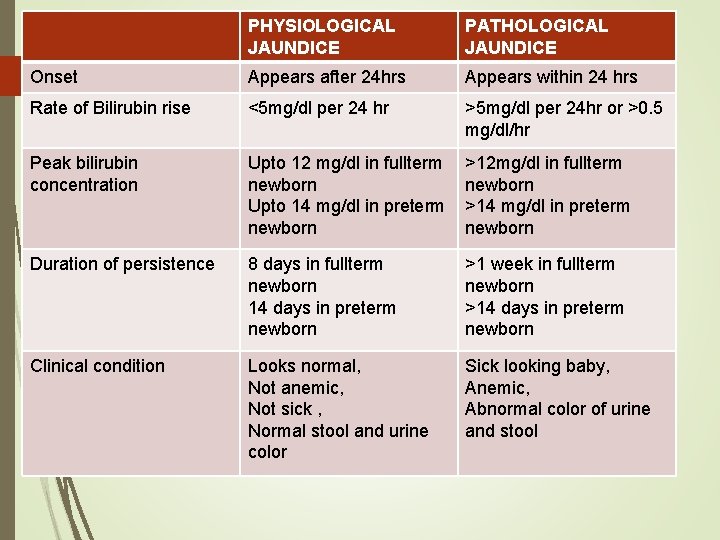
PHYSIOLOGICAL JAUNDICE PATHOLOGICAL JAUNDICE Onset Appears after 24 hrs Appears within 24 hrs Rate of Bilirubin rise <5 mg/dl per 24 hr >5 mg/dl per 24 hr or >0. 5 mg/dl/hr Peak bilirubin concentration Upto 12 mg/dl in fullterm newborn Upto 14 mg/dl in preterm newborn >12 mg/dl in fullterm newborn >14 mg/dl in preterm newborn Duration of persistence 8 days in fullterm newborn 14 days in preterm newborn >1 week in fullterm newborn >14 days in preterm newborn Clinical condition Looks normal, Not anemic, Not sick , Normal stool and urine color Sick looking baby, Anemic, Abnormal color of urine and stool
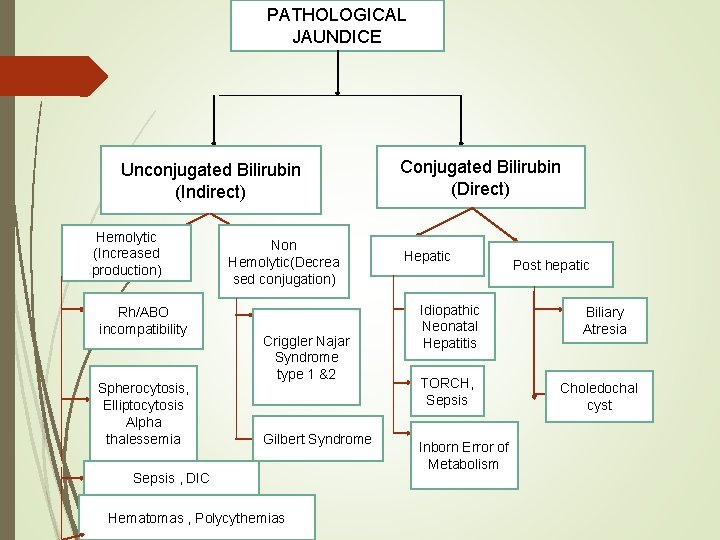
PATHOLOGICAL JAUNDICE Unconjugated Bilirubin (Indirect) Hemolytic (Increased production) Rh/ABO incompatibility Spherocytosis, Elliptocytosis Alpha thalessemia Non Hemolytic(Decrea sed conjugation) Criggler Najar Syndrome type 1 &2 Gilbert Syndrome Sepsis , DIC Hematomas , Polycythemias Conjugated Bilirubin (Direct) Hepatic Idiopathic Neonatal Hepatitis TORCH, Sepsis Inborn Error of Metabolism Post hepatic Biliary Atresia Choledochal cyst
ABO VS Rh incompatibility
ABO Incompatibility Anti A Anti B ANTIBODIES- IGM Type Early onset jaundice and mild splenomegaly Anemia abesent DCT –generally negative / weakly positive

Rh Incompatibility Jaundice within few hours of birth Severe anemia and hepatosplenomegaly Hydrops fetalis Hypoglycemia, Leukopenia Thrombocytopenia

Jaundice accompanying G 6 PD deficiency: • Patients having G 6 PD deficiency also have genetic defects in bilirubin conjugation as seen in gilbert's disease. • It is uncommon to have jaundice in G 6 PD def infant due to severe hemolytic attack. • Those G 6 PD deficient neonates who develop higher maximal serum total bilirubin values had significantly lower serum conjugated bilirubin fractions.
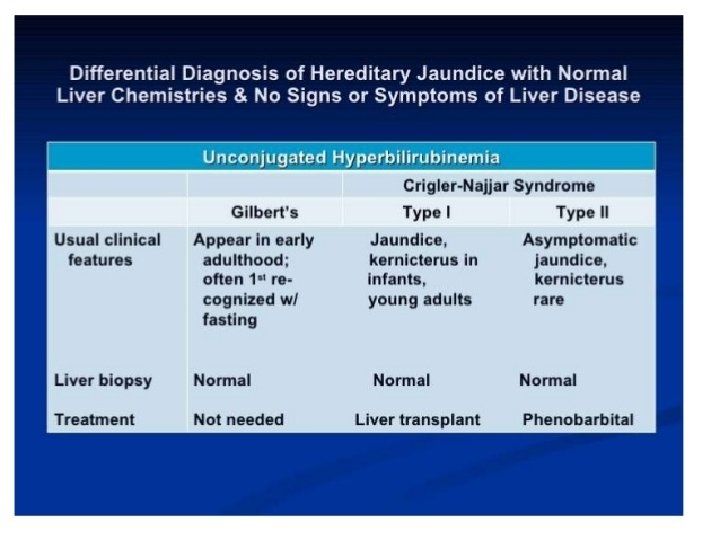
GILBERT DISEASE 3 to 8 % of population, male predominance Autosomal recessive Unconjugated hyperbilirubinemia occuring in absence of overt hemolysis or liver disease Typically, there are mild chronic or intermittent episodes of jaundice that increase with intercurrent illness, fasting, stress , fatigue, menses, ethanol and nicotinic acid intake

Crigler-Najjar syndrome type I Rare Complete absence of UDPGT and is by severe hyperbilirubinemia characterized The ongoing risk of kernicterus at any point an individual's lifespan. during Currently, liver transplantation is the only definitive therapy
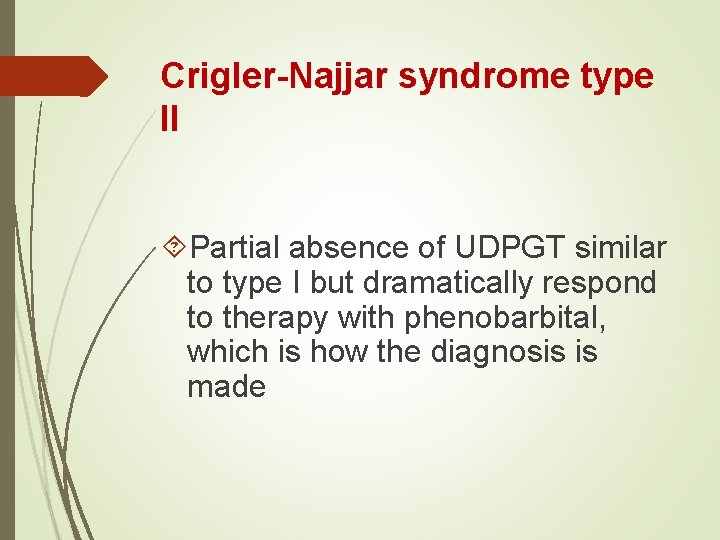
Crigler-Najjar syndrome type II Partial absence of UDPGT similar to type I but dramatically respond to therapy with phenobarbital, which is how the diagnosis is made

APPROACH TO JAUNDICE IN NEWBORN Determine birth weight, gestation and postnatal age Assess clinical condition (well or ill) , degree of jaundice Decide whether jaundice is physiological or pathological Look for evidence of kernicterus in deeply jaundiced Newborn
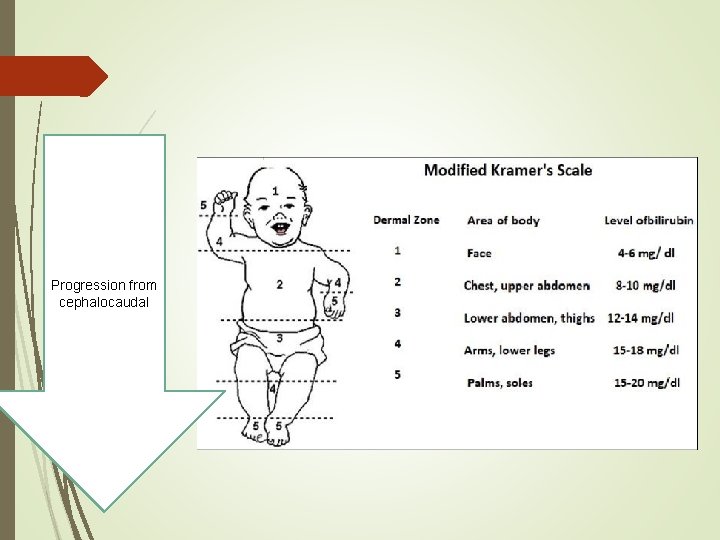
Progression from cephalocaudal
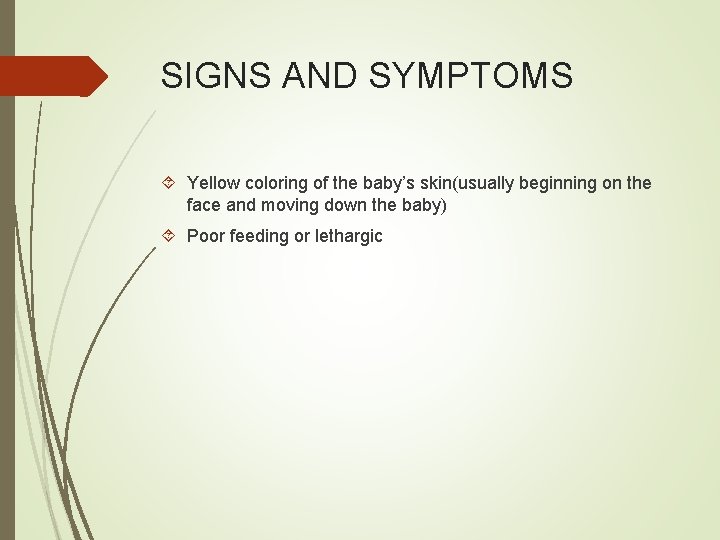
SIGNS AND SYMPTOMS Yellow coloring of the baby’s skin(usually beginning on the face and moving down the baby) Poor feeding or lethargic
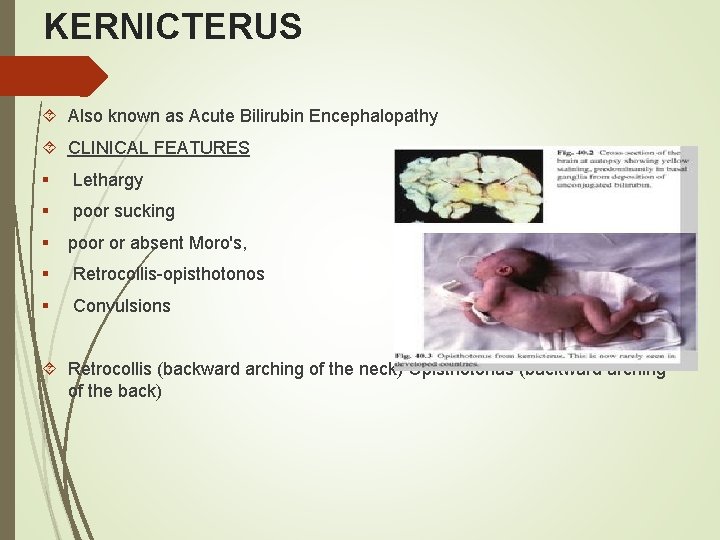
KERNICTERUS Also known as Acute Bilirubin Encephalopathy CLINICAL FEATURES § Lethargy § poor sucking § poor or absent Moro's, § Retrocollis-opisthotonos § Convulsions Retrocollis (backward arching of the neck) Opisthotonus (backward arching of the back)
Chronic Bilirubin Encephalopathy ü Athetosis ü Upward gaze ü Sensorineural ü Hearing loss ü Intellectual deficits, ü Mild MR
LABORATORY TESTS q Total & direct bilirubin* q Blood group and Rh for mother and baby* q Hematocrit, retic count and peripheral smear* q G 6 PD assay q Coomb’s test q Sepsis screen q Liver and thyroid function q TORCH titers q Liver scan when conjugated hyperbilirubinemia q Ultrasonography of the liver and bile ducts in cholestatsis
TRANSCUTANEOUS BILIRUBINOMETRY Measurement of bilirubin by jaundice meter

Liver function tests: Aspartate aminotransferase (ASAT or SGOT) and alanine aminotransferase (ALAT or SGPT) levels are elevated in hepatocellular disease. Alkaline phosphatase and γ -glutamyltransferase (GGT) levels are often elevated in cholestatic disease. A γ -GT/ALAT ratio of more than 1 is strongly suggestive of biliary obstruction. However, it does not distinguish between intrahepatic and extrahepatic cholestasis (do ultrasoud)

Reducing substance in urine: is a useful screening test for galactosemia, provided the infant has received sufficient quantities of milk.

Other Tests Ø Hearing tests (Brainstem auditory-evoked potentials) should be obtained in aftermath of severe neonatal jaundice to exclude sensorineural hearing loss.
Other Tests Hearing tests (Brainstem auditory-evoked potentials) should be obtained in aftermath of severe neonatal jaundice to exclude sensorineural hearing loss.

MRI in kernicterus Hyperintensities in globus pallidus

Management Phototherapy Intravenous immune globulin (IVIG) Exchange transfusion Drugs

Principle of phototherapy Native bilirubin ( water Insoluble) 450 -460 nm of light `Photo isomers of bilirubin (water Soluble) Urine

Phototherapy Technique 1) Perform hand wash 2) Place baby naked in cradle or incubator 3) Fix eye shades 4) Keep baby at least 45 cm from lights 5) Start phototherapy 6) Frequent extra breast feeding every 2 hourly 7) Turn baby after each feed 8) Temperature record 2 to 4 hourly 9) Weight record- daily 10) Monitor urine frequency 11) Monitor bilirubin level

PHOTOTHERAPY RANGE
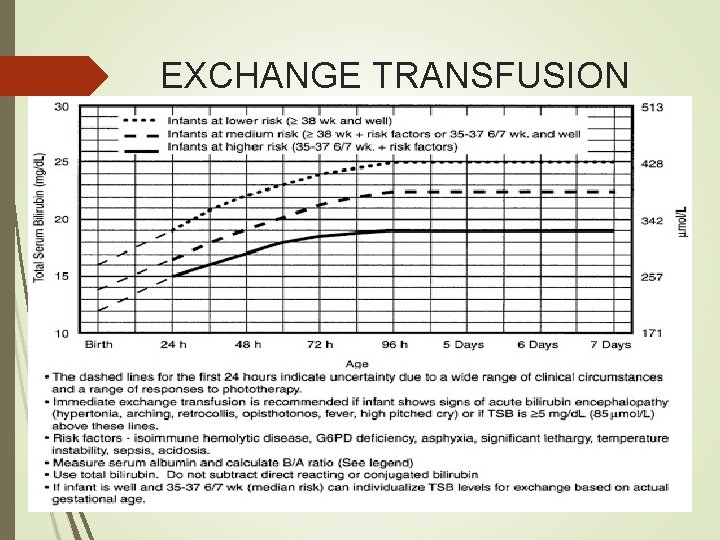
EXCHANGE TRANSFUSION RANGE
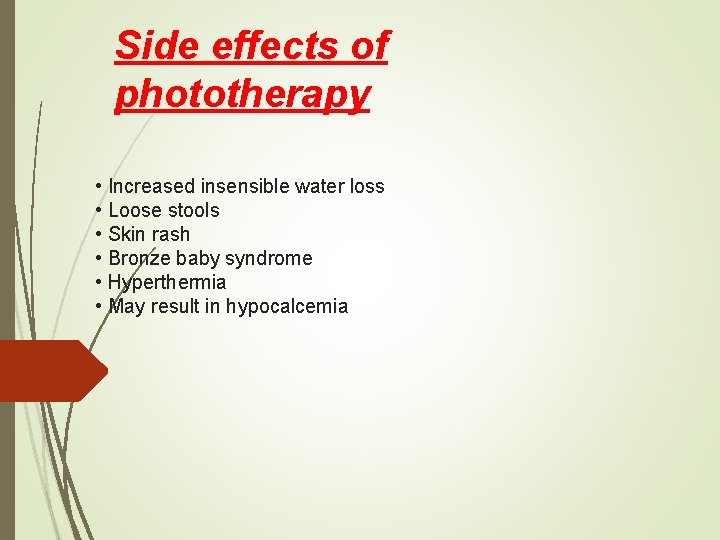
Side effects of phototherapy • Increased insensible water loss • Loose stools • Skin rash • Bronze baby syndrome • Hyperthermia • May result in hypocalcemia
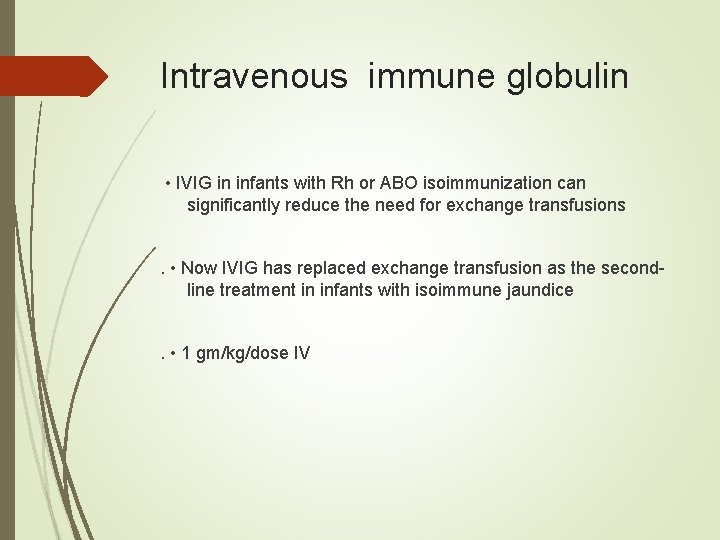
Intravenous immune globulin • IVIG in infants with Rh or ABO isoimmunization can significantly reduce the need for exchange transfusions. • Now IVIG has replaced exchange transfusion as the secondline treatment in infants with isoimmune jaundice. • 1 gm/kg/dose IV
TIN MESOPORPHYRIN TREATMENT Tin- mesoporphyrin(Sn. MP) is used in the treatment of refractory hyperbilirubinemia due to Rh incompatability Sn. MP inhibits the activity of haemeoxygenase, the rate limiting enzyme in the haem catabolic path way and it supresse bilirubin formation.


Exchange transfusion is indicated for avoiding bilirubin neurotoxicity when otherapeutic modalities have failed or are not sufficient. The procedure may be indicated in infants with erythroblastosis who present with severe anemia, hydrops, or both, even in the absence of high serum bilirubin

Phenobarbital (Luminal) Hyperbilirubinemia: 3 -8 mg/kg/d PO/IV initially; may increase up to 12 mg/kg/d Not to exceed IV administration rate of 1 mg/kg/min or 30 mg/min for infants

Prolonged indirect jaundice Causes Ø Breast milk jaundice Ø Hypothyroidism Ø Pyloric stenosis Ø Ongoing hemolysis Ø Crigler Najjar syndrome

Conjugated hyperbilirubinemia Suspect • High colored urine • White or clay colored stool Caution: Always refer to hospital for investigations so that biliary atresia or metabolic disorders can be diagnosed and managed early

Remember that: Jaundice is the most frequent cause of admission after early discharge from nursery. It is not physiological if: 1. appear in first 24 hrs 2. increases by > 0. 5 mg/d. L/hr 3. evidence of hemolysis, 4. abnormal examination, 5. direct bilirubin is > 20% of total, 6. or persists > 3 weeks.

THANK YOU
- Slides: 51