Approach to Hemorrhagic and Ischemic Strokes ACEP South







- Slides: 35
Approach to Hemorrhagic and Ischemic Strokes ACEP South Dakota March 4, 2017 Marko Duic & Gaurav Puri
Objectives Classifying types of CVA Acute management Long-term management/treatment options
Types of CVA Ischemic CVA Hemorrhagic spontaneous traumatic
Ischemic CVA Causes: Embolic Thrombosis Dissection Vascular obstruction
Signs and Symptoms Transient or progressive symptoms: Visual symptoms Speech deficits Unilateral weakness Coordinations issues Vertigo Decreased LOC Other:

Deficits Are all strokes created? Location matters Why?


So you’re having a stroke…. . now what? Acute management: diagnosis first ABCs thrombolysis/stroke protocol antiplatelet antihypertensive other:
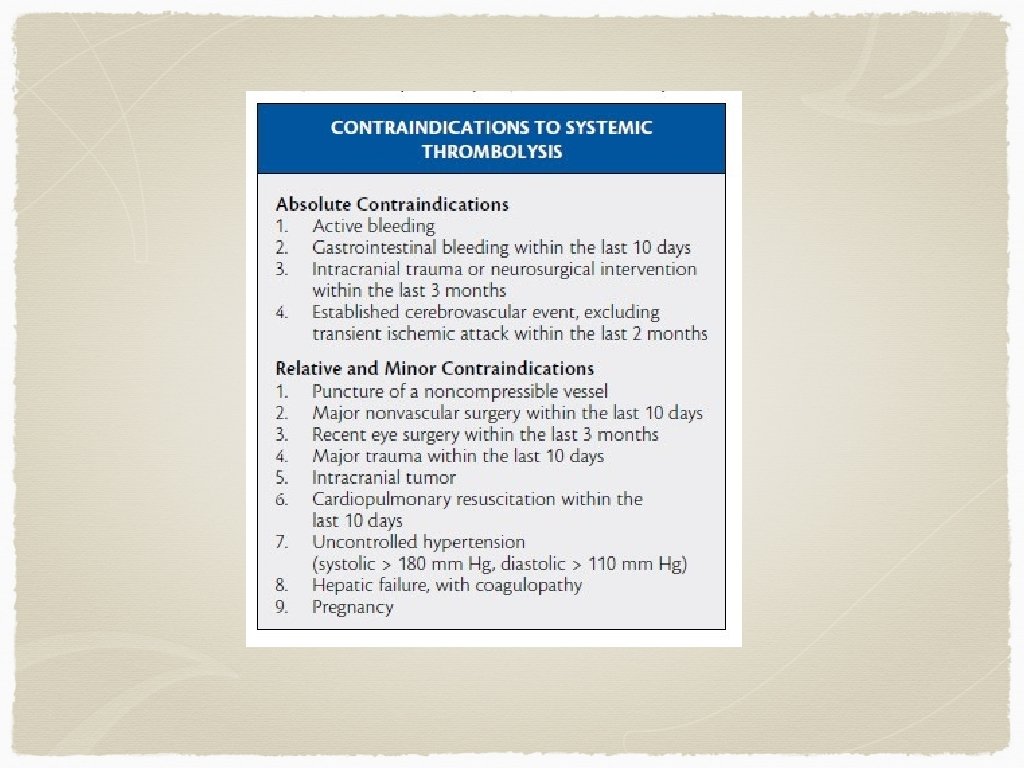
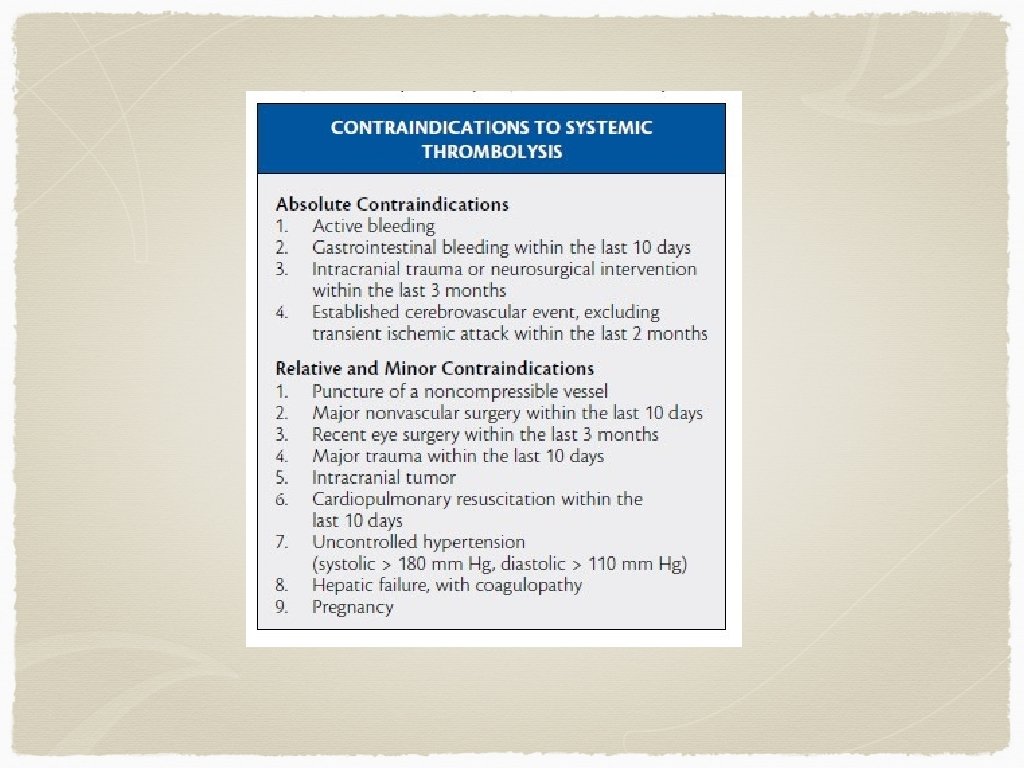
Diagnosis Clinical diagnosis initially If someone presents within the window for thrombolysis (3 -4. 5 hours), and does not have contraindications for thrombolysis, they should be transferred to a stroke centre for consideration of thrombolysis Controversial - why? Any other options?
Thrombolysis To date, roughly 12 trials examining thrombolysis with over 60000 patients 2 of 12 showed a benefit for thrombolysis unfortunately, both use nonstandard data analysis and reporting Several studies showed harm
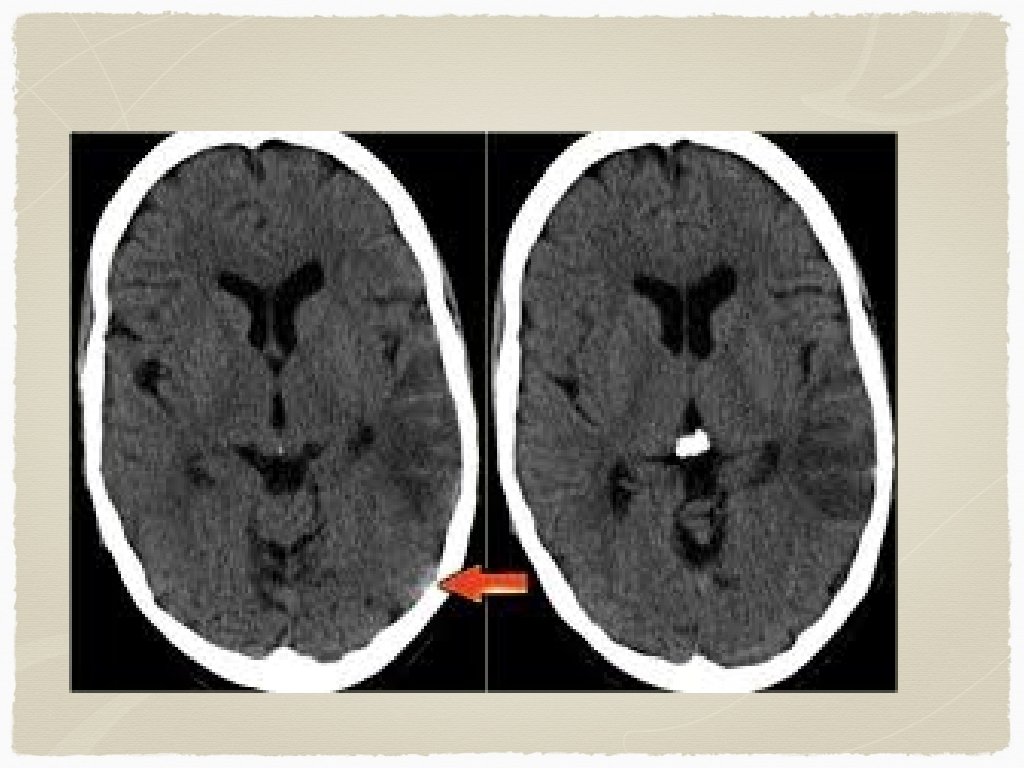
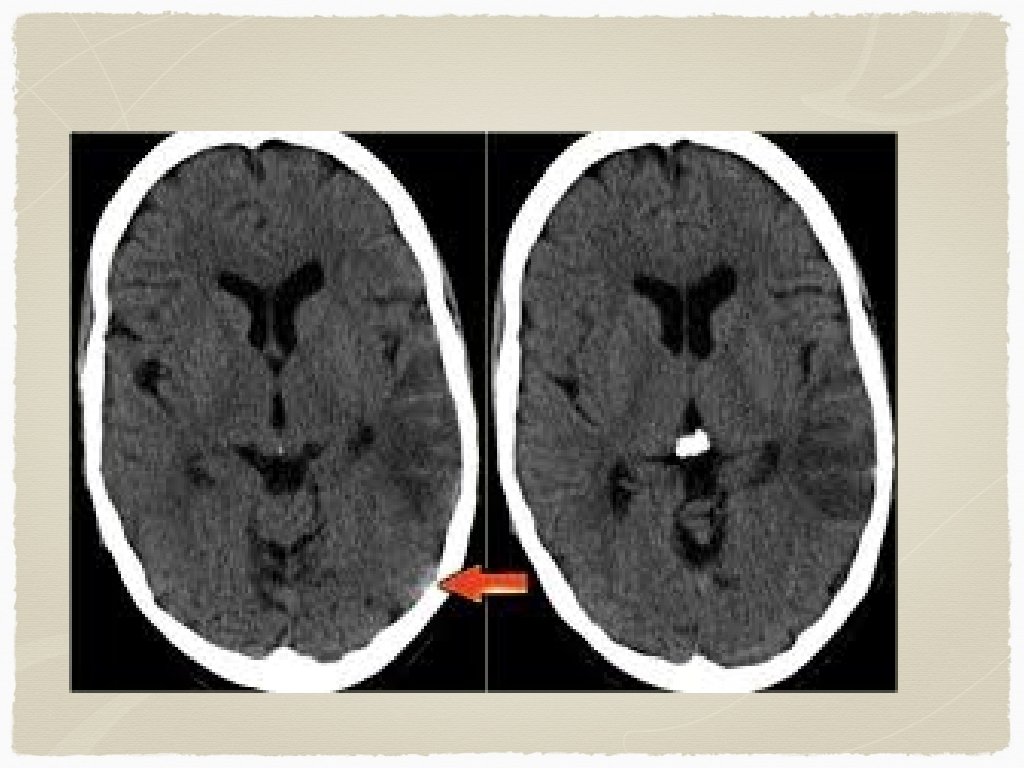
Outside of the window for TPA - Diagnosis CT head: findings? early vs late findings?
Treatment? Medical therapy Antiplatelet: ASA, Plavix
Antihypertensives For candidates of thrombolysis, target BP is less than 185 systolic and 110 diastolic For non TPA patients, blood pressure reduction is targeted at 10 -15% reduction Initial agents usually: Labetolol 10 -20 mg IV initially, can repeat, consider infusion Nitroglycerine Enalapril 1. 25 mg Nicarapine 5 mg/hr (can titrate to effect)
What’s the point of BP control? Need to match changes in ICP and CPP to ensure perfusion to affected area/collateral circulation Aggressive BP management can be harmful

Other treatment/diagnostics Bed position Cholesterol/blood glucose control Echo, holter, doppler, MRI
Questions?
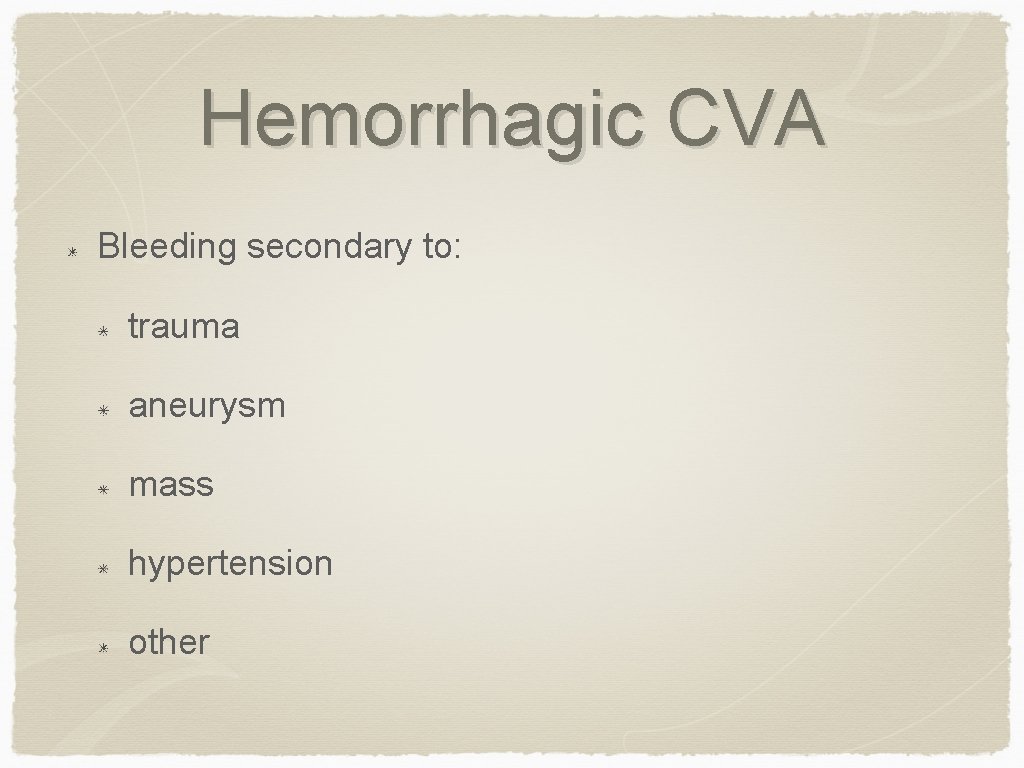
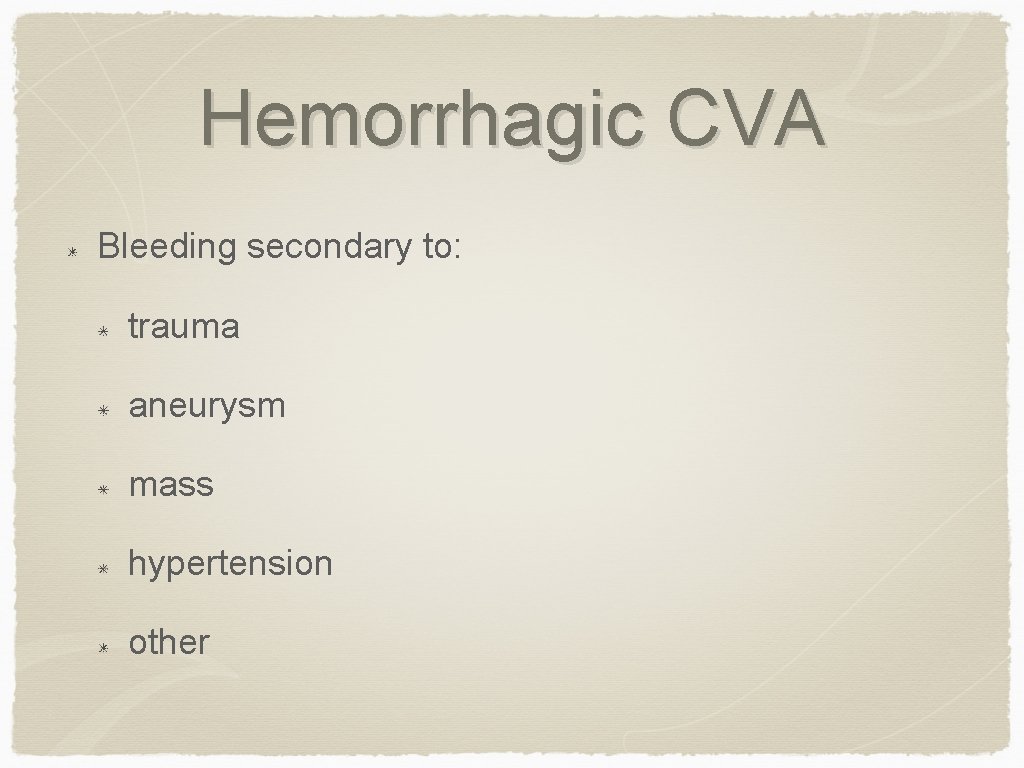
Hemorrhagic CVA Bleeding secondary to: trauma aneurysm mass hypertension other

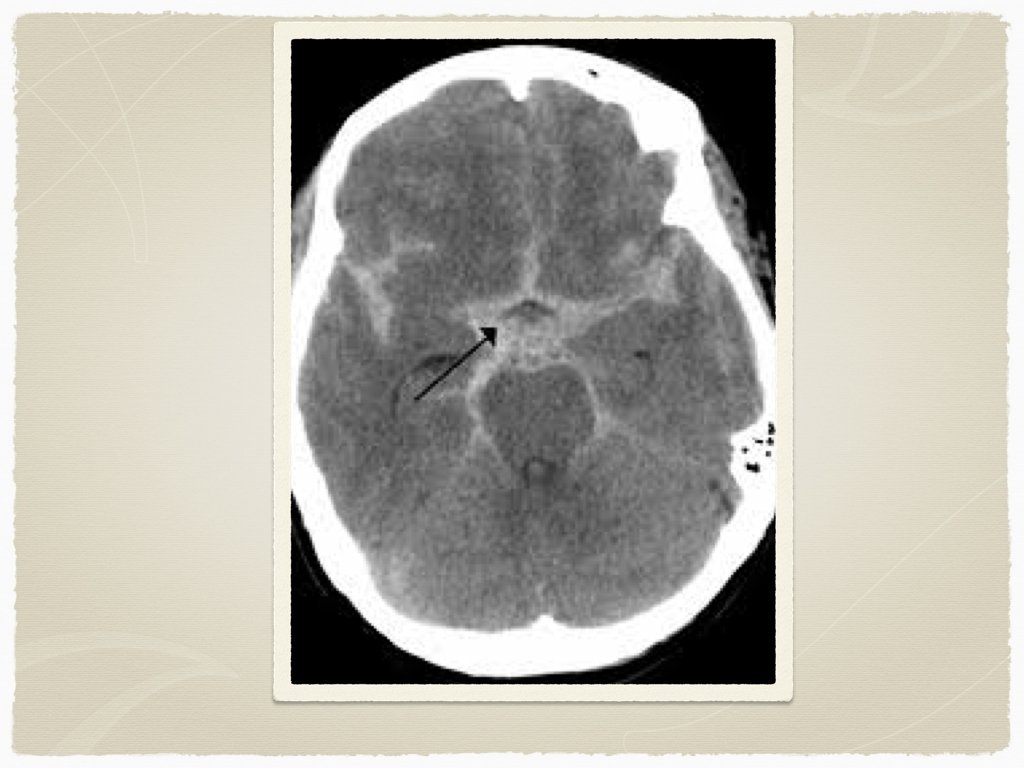
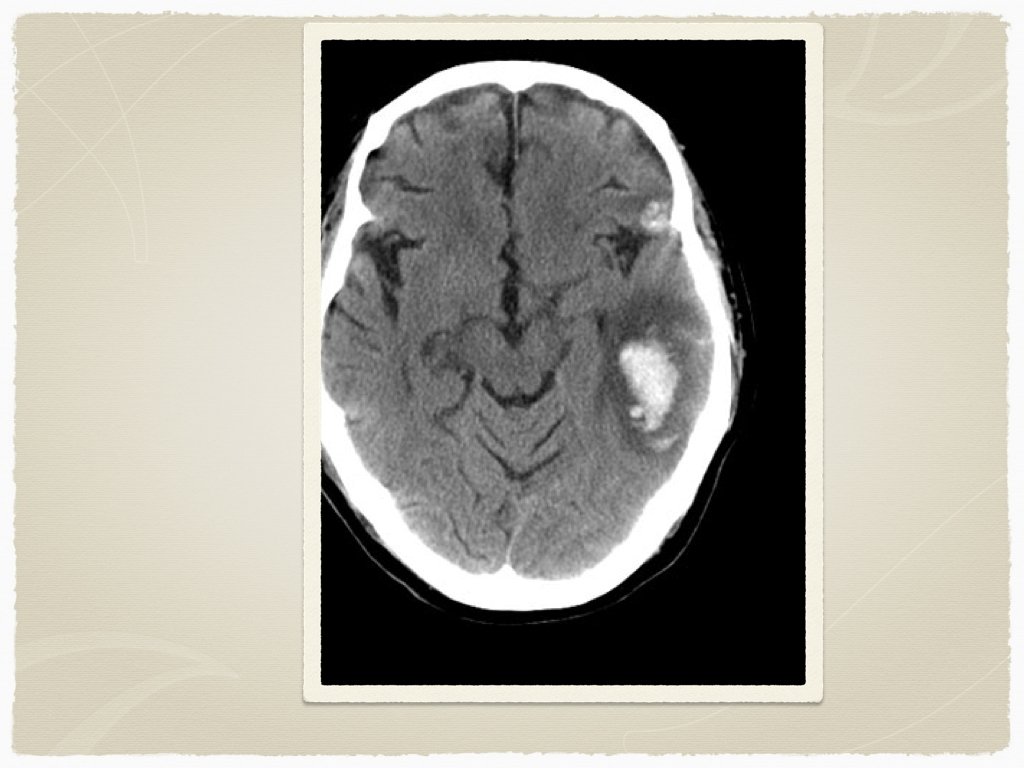
Types Subdural Epidural Subarachnoid Intraparenchymal Are all bleeds the same?

Signs and Symptoms Decreased LOC Obvious Trauma Pupil abnormalities Unilateral weakness Headache Elevated BP Low heart rate other:
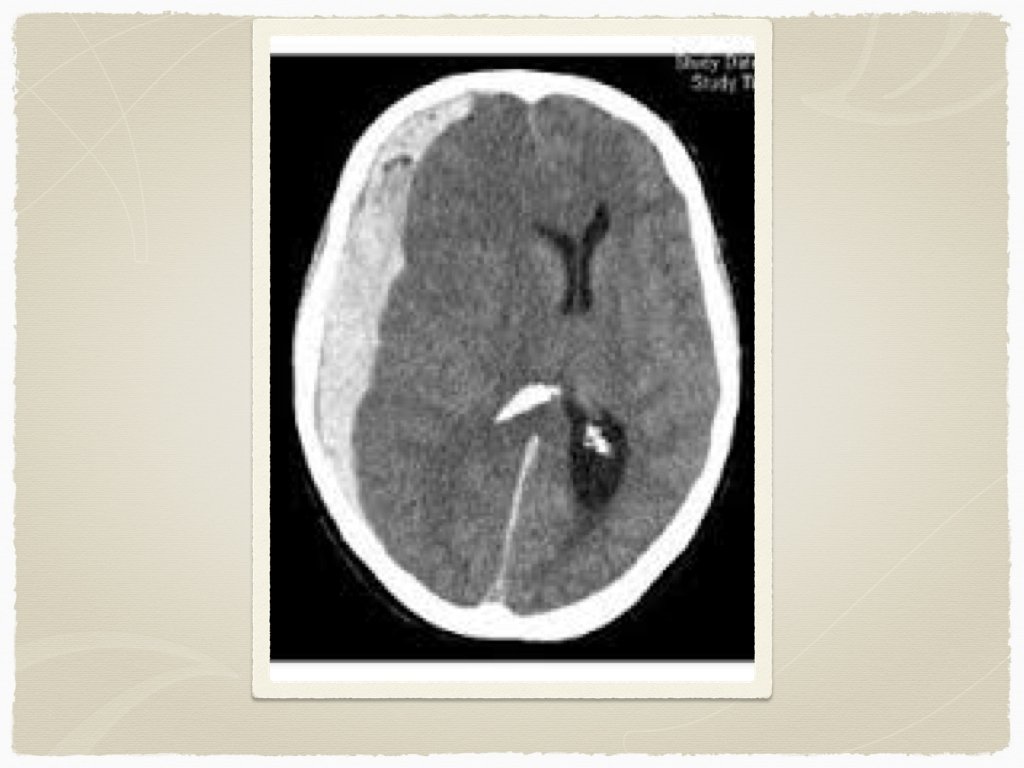
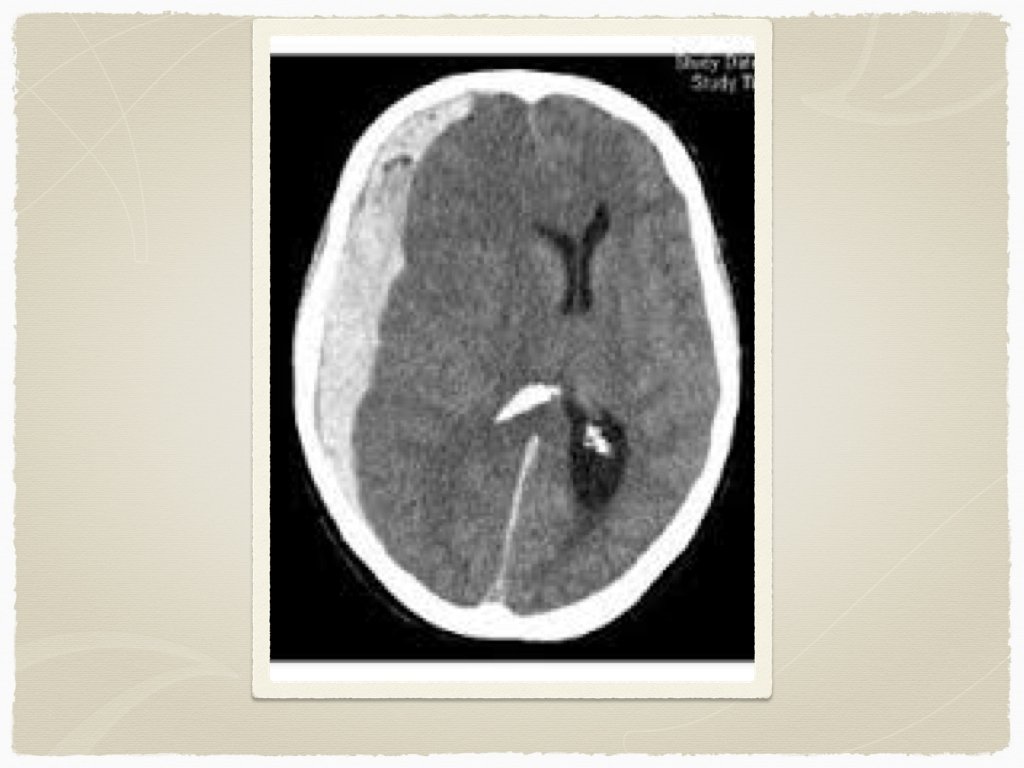
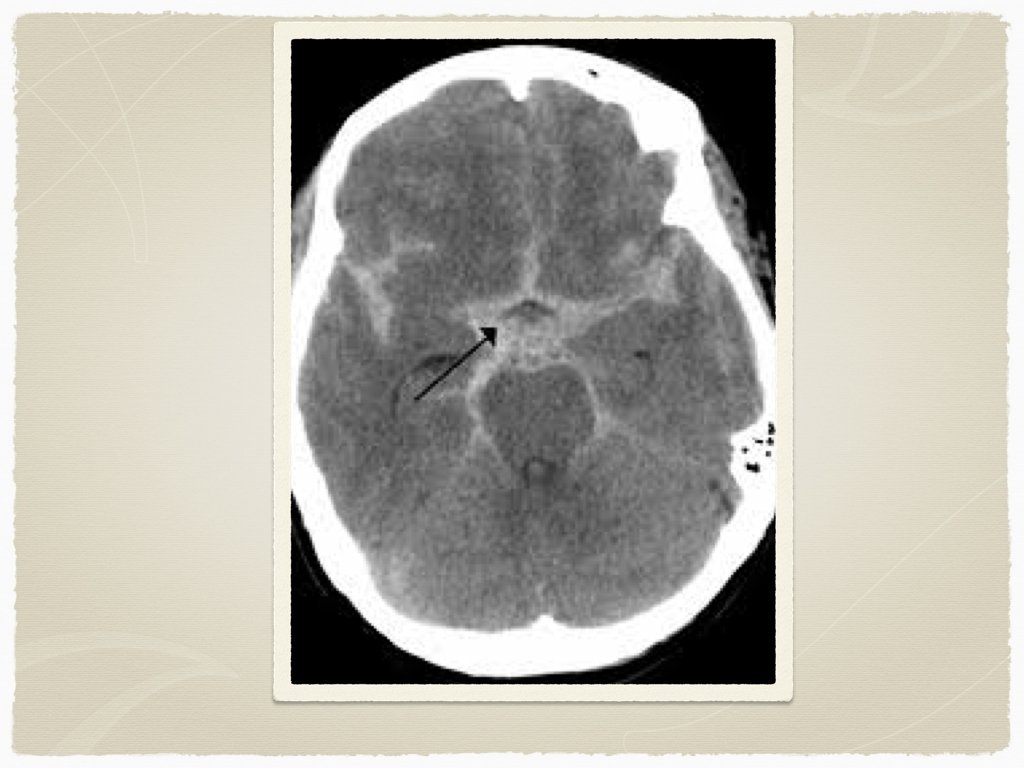
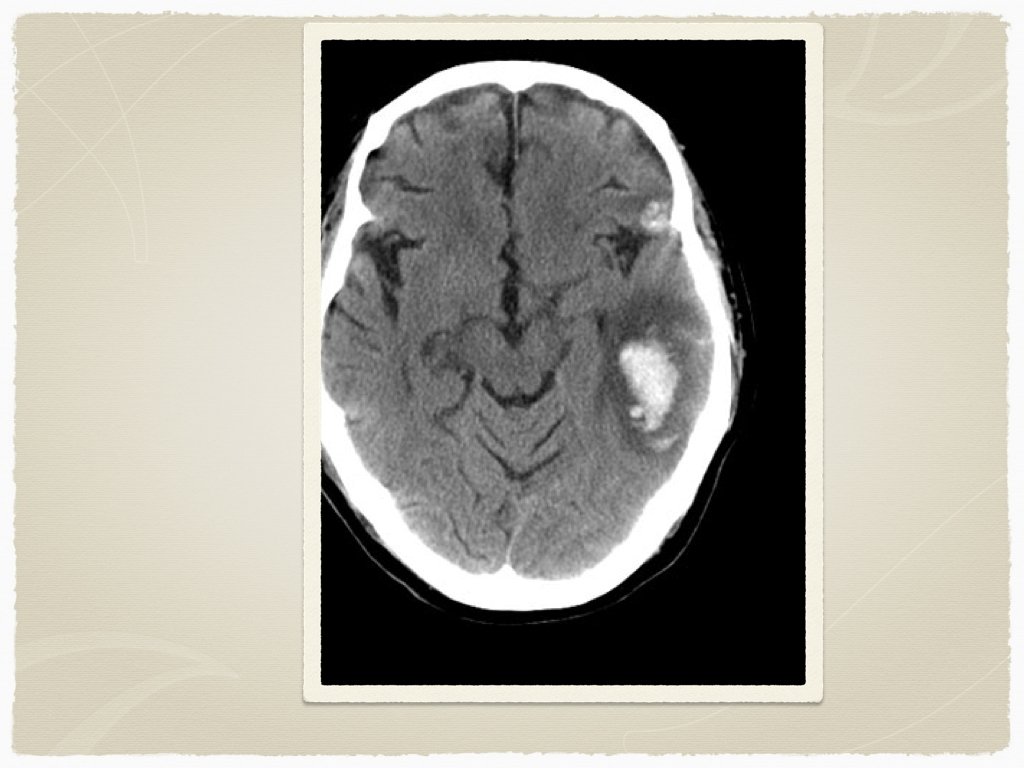
Diagnostics CT is the initial test of choice In sentinel bleed for aneurysmal SAH, can be negative LP to follow if suspicion Lab work: INR Troponin ECG
Initial Management ABCs first If surgical bleed, consultation with neurosurgery for transfer Reversal of coagulation issues Tranexamic acid? Blood pressure management Anticonvulsants ICP management

Coagulation issues Oral anticoagulants Warfarin - Octaplex/beriplex, Vitamin K FFP Pradaxa - Praxbind Platelet dysfunction Hepatic failure - Vitamin K, FFP Renal failure - Platelets Heparin - protamine sulfate
Traumatic ICH Tranexamic acid - 1 g IV CRASH 2 trial - Early administration of TXA safely reduced the risk of death in bleeding trauma patients Administration beyond 3 hours of trauma is unlikely to provide benefit
Blood Pressure Management No clear guidelines/studies describe optimal BP levels in hemorrhagic CVA Significantly elevated BP may lead to rebreeding/hematoma expansion INTERAC 1 & 2 trials showed that early intensive BP control (less than SBP < 140) led to less hematoma expansion This was more important in patients on antithrombotic therapy Agent of choice was either labetolol, enalapril or nicardipine (can also use hydralazine in refractory cases) ATACH-II trial ongoing currently to assess outcomes with BP control less than 140 with nicardipine
Seizures in ICH Acutely, benzodiazepines can be used to stop an active seizure Dilantin load can be used to prevent further seizures Patients with ICH and seizure will likely require intubation and sedation Conflicting evidence for prophylactic anticonvulsants in ICH/SAH - more to come on this
Key concepts ICP - intracranial pressure CPP - cerebral perfusion pressure MAP - mean arterial pressure
ICP is usually elevated in ICH Elevation of the bed to 30 degrees improves venous outflow and decreases ICP No evidence for use of mannitol No evidence for use of corticosteroids - may result in complications
Questions?
 Ischemic vs hemorrhagic stroke
Ischemic vs hemorrhagic stroke Pocus fast
Pocus fast Safer sign out form acep
Safer sign out form acep Pathogenesis of stroke ppt
Pathogenesis of stroke ppt Cns ischemic response
Cns ischemic response Stroke protocol
Stroke protocol Cns ischemic response
Cns ischemic response Cns ischemic response flow chart
Cns ischemic response flow chart Bainbridge reflex
Bainbridge reflex Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Antianginal drugs classification
Antianginal drugs classification Ischemic heart disease
Ischemic heart disease Tenecteplase stroke
Tenecteplase stroke Giant cell arteritis
Giant cell arteritis Ischemic bile duct injury
Ischemic bile duct injury Baby fever chart
Baby fever chart Reactionary hemorrhage definition
Reactionary hemorrhage definition Atls classes of hemorrhagic shock
Atls classes of hemorrhagic shock Hemorrhagic diathesis
Hemorrhagic diathesis Which vitamin is antihemorrhagic
Which vitamin is antihemorrhagic Necrotizing fasciitis hemorrhagic bullae
Necrotizing fasciitis hemorrhagic bullae Causes of viral hemorrhagic fever
Causes of viral hemorrhagic fever Icp monitoring
Icp monitoring Hemorrhagic transformation mri
Hemorrhagic transformation mri Dr kenneth stahl
Dr kenneth stahl Pancreatitis pathophysiology
Pancreatitis pathophysiology Stages of hemorrhagic shock
Stages of hemorrhagic shock Hemorrhagic fever with renal syndrome
Hemorrhagic fever with renal syndrome Hemorrhagic
Hemorrhagic Appositive brush stroke
Appositive brush stroke Absolute brush stroke examples
Absolute brush stroke examples Stokes theorem is relation between
Stokes theorem is relation between Recurrent stroke causes
Recurrent stroke causes Head strokes physical affection
Head strokes physical affection Rational root theorom
Rational root theorom As cannons overcharged with double cracks meaning
As cannons overcharged with double cracks meaning