Approach to dysphagia benign esophageal disease Done by
Approach to dysphagia &benign esophageal disease Done by: Thaer Omar Alqatish
Definitions: • Dysphagia ? • Aphagia ? • Odynophagia ? • Phagophobia ?
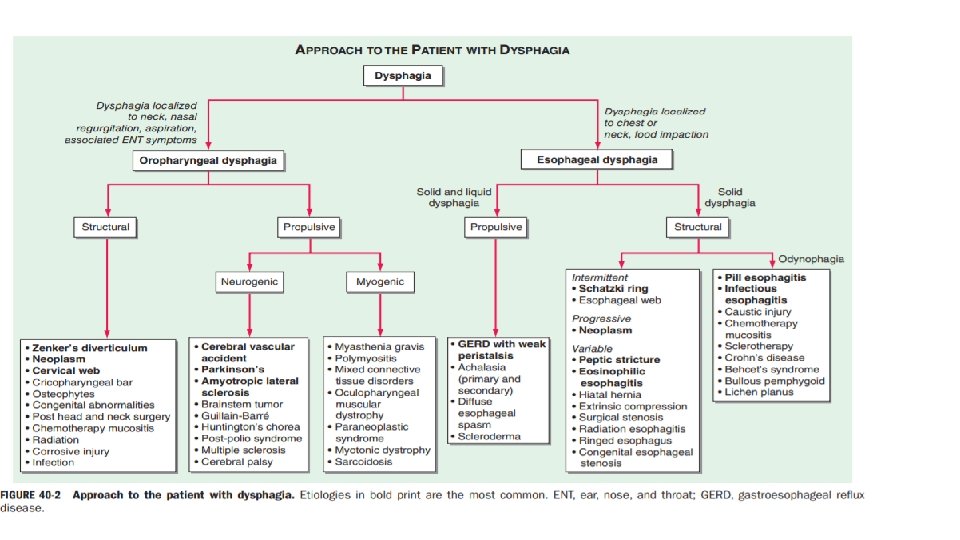
Classifications for dysphagia 1 - Oral and Pharyngeal (Oropharyngeal) Dysphagia ? 2 - Esophageal Dysphagia ?
DDx • 1 - Oropharyngeal Dysphagia: • Iatrogenic causes include surgery and radiation, • Neurogenic : from cerebrovascular accidents, Parkinson’s disease, and amyotrophic lateral sclerosis • Structural lesions causing dysphagia include Zenker’s diverticulum, cricopharyngeal bar, and neoplasia. • 2 - Esophageal Dysphagia: • Structural: Schatzki’s rings, eosinophilic esophagitis, and peptic strictures. • Neuromascular: DES, achalasia, scleroderma
Clinical approach • History ? • Physical Examination • Investigations • Treatment
History • 1 - localization of dysphagia, • 2 - other symptoms associated with dysphagia, • 3 - The type of food causing dysphagia • 4 - dysphagia progression. • 5 - accompanying odynophagia? ? , • 6 - A history of ; * A history of prolonged nasogastric intubation, esophageal or head and neck surgery, ingestion of caustic agents or pills, previous radiation or chemotherapy,
Physical Examination • 1 - Mouth and pharynx ? • 2 - Neck ? • 3 - Changes in the skin ? • 4 - Signs of neuromuscular disease?
Investigations • 1 - start with barium swallow study • 2 - For suspected esophageal dysphagia, upper endoscopy (& mucosal biopsies) is the single most useful test. • 3 - Esophageal manometry • 4 - In specific cases, computed tomography (CT) examination and endoscopic ultrasonography may be useful.
Treatment • 1 - conservative measures: • changing postures or maneuvers • altering the consistency of ingested food and liquid • severe and persistent cases may require gastrostomy and enteral feeding. • 2 - medical treatment • 3 - Dilators & Surgical intervention
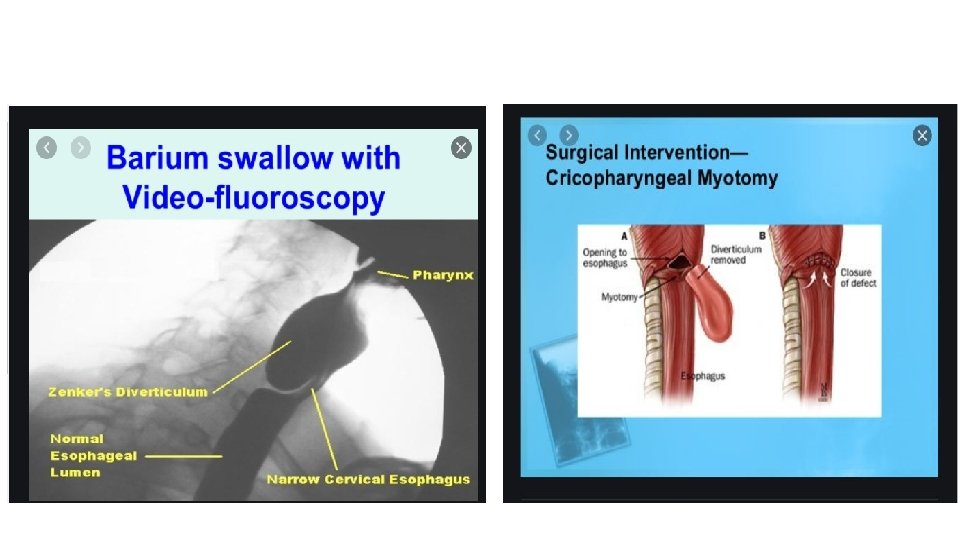
Zenker’s Diverticulum • Definition: • is a diverticulum (outpouching) of the mucosa of the pharynx, just above the cricopharyngeal muscle (i. e. above the upper sphincter of the esophagus). It is a pseudo diverticulum (not involving all layers of the esophageal wall). • Pathophysiology: • If swallowing is Uncoordinated so that the cricopharyngeus does not relax, the week unsupported area above these fibers bulges out. (Killian’s dehiscence) • Clinical Features: • Signs and Symptoms: 1 - Dysphagia 2 - Halitosis (bad smell) 3 - Food regurgitation. 4 - Posterior neck mass.
• Diagnosis: • Barium swallow. ** Endoscopy and NG tube are contraindicated (due to the risk of perforation) • Treatment: • Surgical resection 1. One stage cricopharyngeal myotomy and diverticulectomy 2. Other options are cricopharyngeal myotomy and diverticulopexy
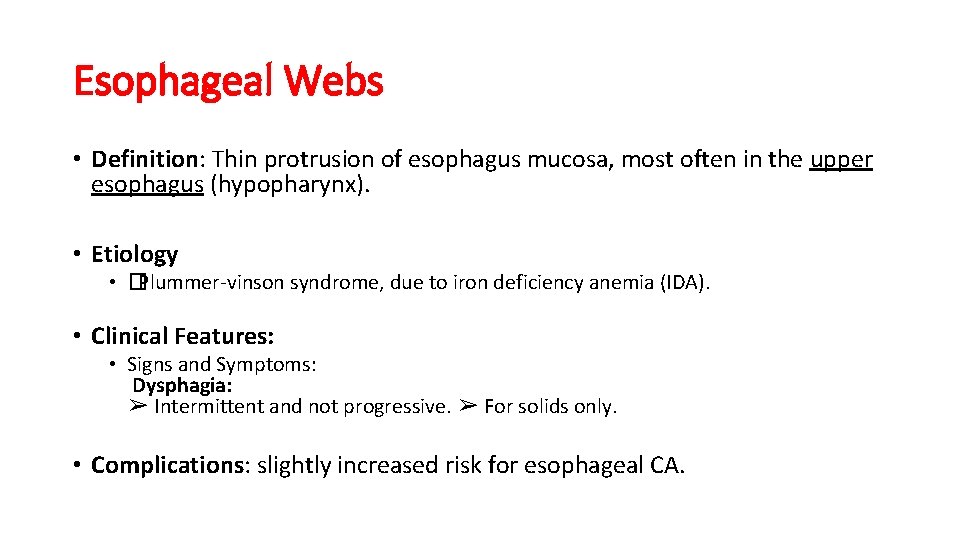
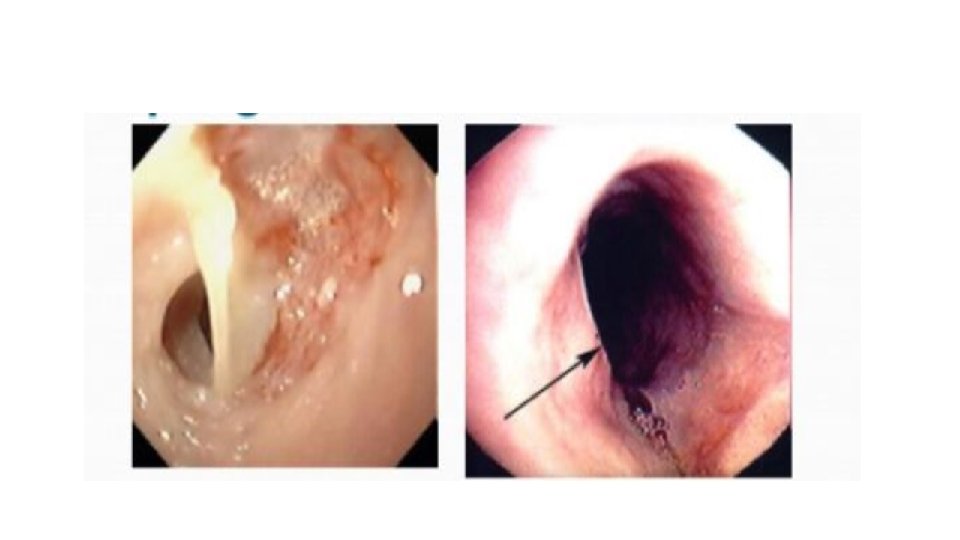
Esophageal Webs • Definition: Thin protrusion of esophagus mucosa, most often in the upper esophagus (hypopharynx). • Etiology • �Plummer-vinson syndrome, due to iron deficiency anemia (IDA). • Clinical Features: • Signs and Symptoms: Dysphagia: ➢ Intermittent and not progressive. ➢ For solids only. • Complications: slightly increased risk for esophageal CA.
• Daignosis: 1 - Barium swallow. 2 - endoscopy • Treatment: • Esophageal dilatation, using bougie or balloon dilators. • Treat IDA
Schatzki ring • Definition: Lower esophageal ring, usually at the squamo-columner junction. { lower esophagus } • �almost always associated with esophageal hiatal hernia • Clinical Features: • 1 - Dysphagia: ➢ Intermittent and not progressive. ➢ For solids only, especially meat and fibers. • Daignosis: 1 - Barium swallow (the ring should be >13 mm to cause symptoms) 2 - endoscopy • Treatment: • treat it like esophageal webs, by dilatation. . ➢ The patients are placed on PPI after diltation.


Esophageal stricture ( peptic stricture ) • Definition: Narrowing of the esophagus. • Etiology: • ➢ Long history of incompletely treated reflux. ➢ Prolonged NG tube placement. ➢ Lye (bleaching agent) ingestion decades ago (alkali is worse than acids)→ erosive esophagitis. • Pathophysiology: • Prolonged/severe Esophageal irritation→erosion of the mucosa→ fibrosis (stricture).
• Clinical Features: • Signs and Symptoms: 1 - Dysphagia: ➢ Constant, slowly progressive. ➢ For solids then liquids. • Daignosis: • Barium swallow. • Treatment: • Dilation
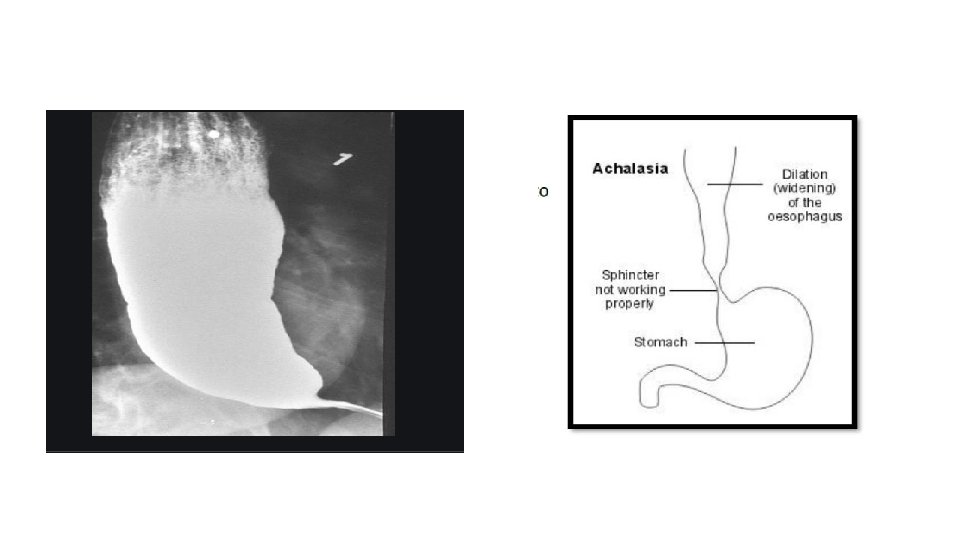
Achalasia • Definition: a failure of smooth muscle fibers to relax, which can cause a sphincter to remain closed and fail to open when needed. • Etiology: • �Of unknown etiology. �pseudoachalasia/secondary achalasia: 1. Esophageal CA. 2. Lymphoma 3. Chagas disease (trypanosoma cruzi infection). 4. Eosinophilic esophagitis 5. Neurodegenerative diseases. • Pathophysiology: • Loss of intralumenal neurons → inc. LES tone (failure of relaxation)→Dilation of the Distal esophagus. • No esophageal peristalsis.
• Diagnosis: • 1. Barium swallow: (best initial test) → bird’s beak appearance ? 2. Upper endoscopy+ biopsy: why ? 3. Esophageal manometry: (the definitive diagnosis) ? • Treatment: 1 - Pneumodilatation: (BEST initial therapy) ➢ 3 -4 diameter ballon is inflated in the LES→ produce higher pressure. ➢ Effective in 85% of patients. ➢ 5% risk of perforation. ** Pneumodilatation effective only for short duration of weeks , best to mix it with botox 2 - Botox (botulinum toxin injection) ➢ Effective in 65% of patients. ➢ Requires repeating therapy within 6 -12 months. 3 - Surgical myotomy. ➢ ”Heller” myotomy. ➢ Incision of circular muscle layer of LES. (cut through the muscle to relief the tension ) ➢ High risk of GERD 4 - Medical treatment (CCB and nitrates) is not that effective.
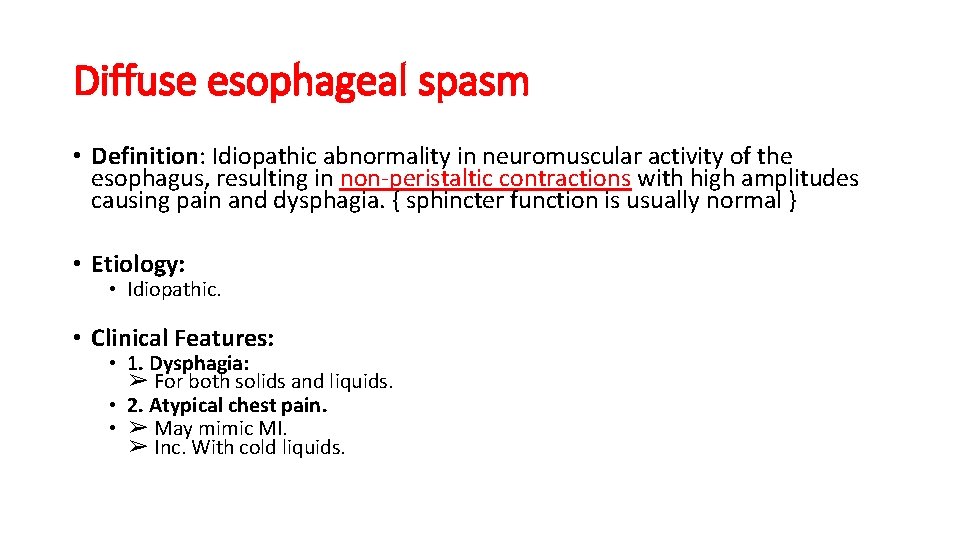
Diffuse esophageal spasm • Definition: Idiopathic abnormality in neuromuscular activity of the esophagus, resulting in non-peristaltic contractions with high amplitudes causing pain and dysphagia. { sphincter function is usually normal } • Etiology: • Idiopathic. • Clinical Features: • 1. Dysphagia: ➢ For both solids and liquids. • 2. Atypical chest pain. • ➢ May mimic MI. ➢ Inc. With cold liquids.
• Diagnosis: • 1 - ECG to role out MI. • 2 - Barium swallow : ➢ Corkscrew appearance (see picture). • 3 - Manometry (most accurate test): ➢ High intensity, intermittent, disorganized contractions. • Treatment: • Medical (antireflux measures, calcium channel blockers, nitrates) • Long esophagomyotomy in refractory cases (a cut through the muscle )

• Nutcracker Esophagus ? ? ?
Gastroesophageal reflux disease (GERD) • Definition: also known as acid reflux, is a long-term condition where stomach contents come back up into the esophagus resulting in either symptoms or complications. • Pathophysiology: • �Loss of anti-reflux mechanisms: • 1. Loss of LES tone &/or peristalsis; due to smoking, alcohol, peppermint, Chocolate, CCB & nitrates. Or hiatal hernia • 2. Inc. Gastric volume; due Diabetic gastroparesis or pyloric stenosis. • 3. Inc. Gastric pressure; due to Ascites or pregnancy.
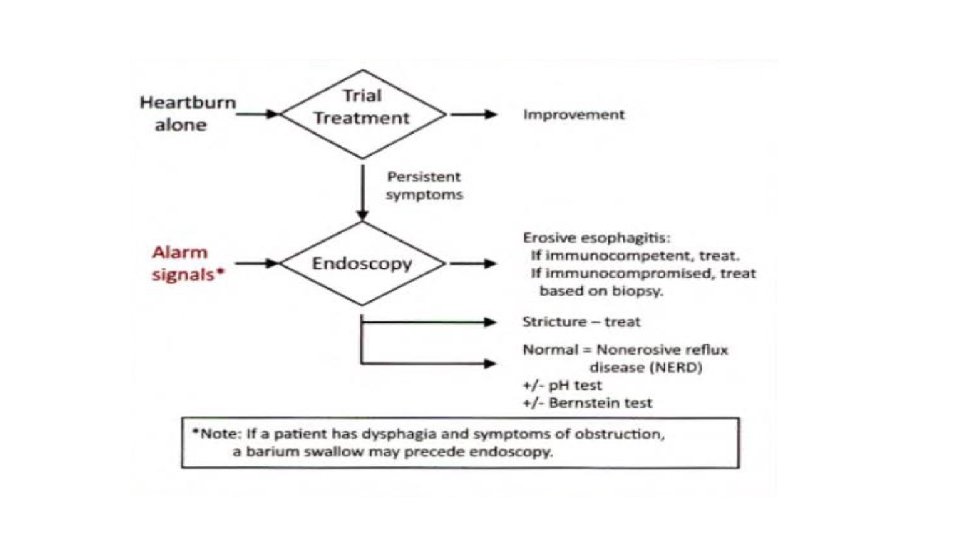
• Signs and Symptoms: • 1. Heartburn/ sore throat. 2. Water brush. 3. Epigastric/substernal pain (the most common cause of non-cardiac chest pain is GERD). 4. Bad, metal-like taste in mouth. 5. Cough, wheezing or hoarseness (it may exacerbate asthma). • Alarming signs: 1. Dysphagia/odynophagia 2. Wight loss/ anorexia/ anemia/ blood in stool. 3. Family history of peptic ulcer disease. 4. Failure to respond to PPI. 5. Long duration of symptoms.
• Complications: • 1. Exacerbation of asthma. 2. Esophageal ulcers 3. Strictures, 4. bleeding 5. Barrett esophagus ? • Treatment: • 1. Life style modification. ? ? • 2. Antacids • 3. H 2 blockers or PPI • �Surgical: ( indications ? ? ) 1. Lap Nissen 2. Belsey Mark IV 3. Hill 4. Toupet
• ➢ Indications for surgery: 1. Failure of medical treatment. 2. Respiratory problems. 3. Severe esophageal injury
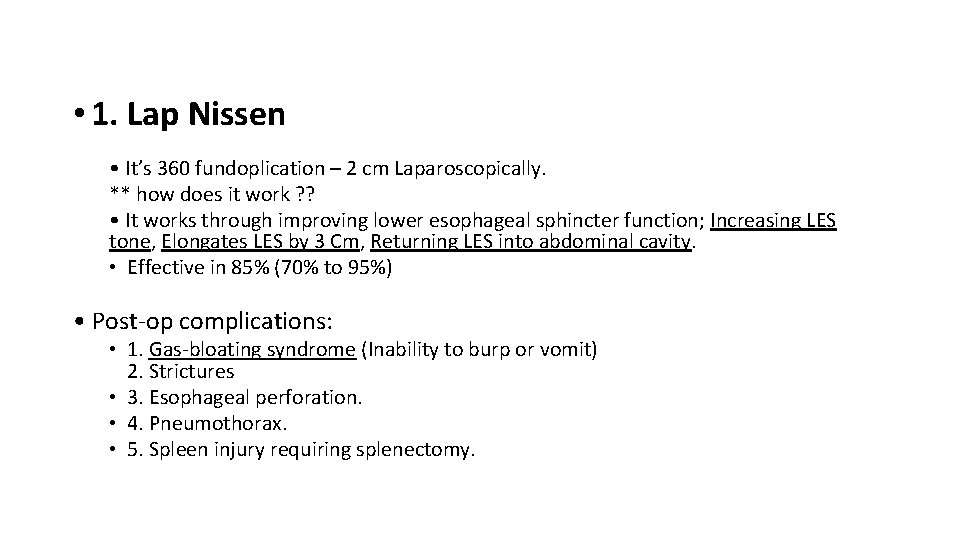
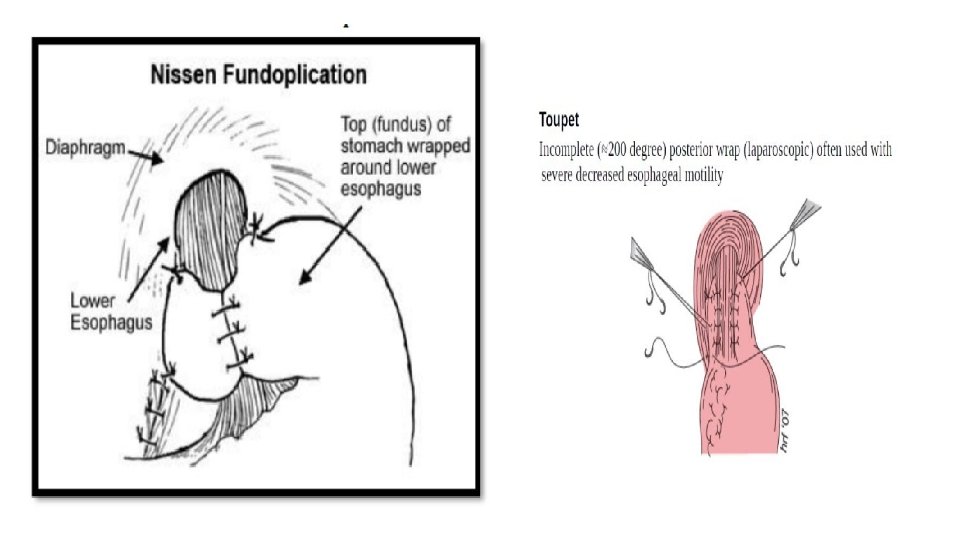
• 1. Lap Nissen • It’s 360 fundoplication – 2 cm Laparoscopically. ** how does it work ? ? • It works through improving lower esophageal sphincter function; Increasing LES tone, Elongates LES by 3 Cm, Returning LES into abdominal cavity. • Effective in 85% (70% to 95%) • Post-op complications: • 1. Gas-bloating syndrome (Inability to burp or vomit) 2. Strictures • 3. Esophageal perforation. • 4. Pneumothorax. • 5. Spleen injury requiring splenectomy.

Other surgical options • 2. Belsey Mark IV: 240 to 270 fundoplication through thoracic approach. • 3. Hill: Arcuate ligament repair (close large esophageal hiatus) + gastropexy (suture stomach to diaphragm). • 4. Toupet: laparoscopic Incomplete Wrap (200)
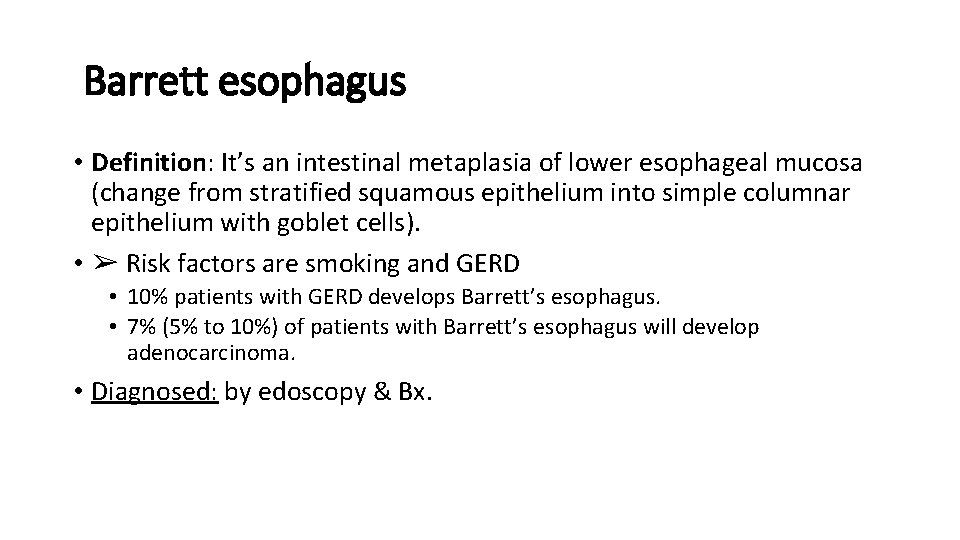
Barrett esophagus • Definition: It’s an intestinal metaplasia of lower esophageal mucosa (change from stratified squamous epithelium into simple columnar epithelium with goblet cells). • ➢ Risk factors are smoking and GERD • 10% patients with GERD develops Barrett’s esophagus. • 7% (5% to 10%) of patients with Barrett’s esophagus will develop adenocarcinoma. • Diagnosed: by edoscopy & Bx.
• Management is by PPI, resection and follow up: • i. No dysplasia → 3 -5 years ii. Low-grade dysplasia→ 6 -12 months iii. High-grade dysplasia → 3 months ** from Dr. Mansour : (in high grade dysplasia we don’t wait and follow the pt instead of that, we go and remove the esophagus as if it was a case of esophageal CA) • Resection options: • endoscopic mucosal resection and photodynamic therapy, radiofrequency ablation, and cryoablation
Other medical disorders • 1 - Scleroderma esophagus • 2 - Pill-induced esophagitis • 3 - Infective esophagitis • 4 - Eosinophilic (allergic) esophagitis

- Slides: 39