APPROACH TO CONTRACEPTION IN WOMEN WITH SYSTEMIC LUPUS

- Slides: 24
APPROACH TO CONTRACEPTION IN WOMEN WITH SYSTEMIC LUPUS ERYTHEMATOSUS Dr Movahed
FACTORS TO CONSIDER The choice of the optimal method of birth control for women with SLE and/or APS depends upon multiple factors: Ø patient values and preferences efficacy and side effects of contraceptive methods underlying disease activity thromboembolic risk medication interactions Ø Ø In addition, any risk associated with a contraceptive method must be weighed against the risk of unplanned pregnancy for that particular patient.
CHOOSING A METHOD OF CONTRACEPTION Reversible contraception options for women: Ø Barrier methods IUDs Contraceptive implants Progestin-only Estrogen-progestin hormonal contraceptives Ø Ø
LONG-ACTING REVERSIBLE CONTRACEPTION LARCs such as IUDs and contraceptive implants are considered the most effective form of contraception and are generally safe for women with SLE and APS.
INTRAUTERINE DEVICES IUDs are safe and effective for most women with SLE and a. PLs, including adolescents and nulliparous women. IUDs available in the United States release either copper or the synthetic progestin LNg. The copper-containing IUD may be used for at least 10 years and may be associated with heavier menses and dysmenorrhea. The LNg-containing IUD which may remain in place for at least three to five years and significantly reduces dysmenorrhea and menstrual bleeding. Complete amenorrhea occurs in up to 50 percent of patients by 24 months, which is a significant benefit for patients who require long-term anticoagulation.
INTRAUTERINE DEVICES While data on IUD use in patients treated with immunosuppressive medications are limited, no increased infection risk is found in HIV-infected women. Guidelines developed by professional organizations do not consider immunosuppressive therapy a contraindication to IUD use. Most experts agree that the minimal risk of infection with IUD use is outweighed by the risks associated with unintended pregnancy in women with active inflammatory disease on potentially teratogenic medications. Thrombophilia does not preclude placement of an IUD. Caution is advised, however, if patients have significant thrombocytopenia that would preclude minor surgical procedures. In such cases, placement of any IUD should be avoided until the count improves in order to minimize risk of bleeding during the procedure.
CONTRACEPTIVE IMPLANTS Contraceptive implants are an alternative option to IUDs for women with SLE or a. PLs who want an effective LARC and cannot take estrogen-containing preparations. The implant most commonly used in the United States is a single rod subdermal implant that is placed in the inner upper arm and releases etonogestrel (a third-generation progestin) over a threeyear period. A LNg (a second-generation progestin) implant is also available. The risk for thromboembolism with progestin-only contraception is low, third-generation progestins do have a slightly higher risk of venous thromboembolism than do the second-generation progestins.
CONTRACEPTIVE IMPLANTS In addition, safety data on use of the etonogestrel implant in patients with APS are not available. Given the slightly greater risk of venous thrombosis associated with third-generation progestins, and the lack of data for use in a. PL-positive patients, we prefer use of the LNg-containing IUD over contraceptive implants in a. PL-positive women. Progestin-only contraceptives are not associated with an increased risk of SLE flare.
HORMONAL CONTRACEPTION Hormonal contraception includes: Ø Estrogen-progestin preparations(eg, pill, patch, ring) Ø Progestin-only preparations (eg, pill, injection, IUD, implant).
ESTROGEN-PROGESTIN CONTRACEPTIVES Estrogen-progestin contraceptives may be used in SLE patients with stable low disease activity and documented negative a. PLs. The data are also limited on the safety of estrogencontaining contraceptives in SLE patients with high disease activity; thus, alternative methods such as the progestin-only pill and IUDs are preferable in such patients.
THROMBOEMBOLIC RISK AND ESTROGEN Serious complications including venous thromboembolism, stroke, and myocardial infarction. The use of estrogen-progestin hormonal contraceptives is contraindicated in women with a. PL with or without SLE due to an increased risk of thrombosis. The safety of use in patients with fluctuating a. PL titers or positive a. PL on anticoagulation is unknown and their use is not recommended. SLE patients without a. PLs do not appear to be at increased risk for thrombosis when taking oral hormonal contraceptives.
RISK OF LUPUS FLARE Despite the common, long-held belief that estrogens provoke lupus disease activity, estrogen-progestin hormonal contraceptives are generally a safe form of contraception for stable a. PL-negative SLE patients with mild-moderate disease activity. A clinical trial evaluated the risk of flare associated with the use of estrogen-progestin oral contraceptive compared with a progestin-only oral contraceptive and a copper IUD, and found no significant differences in disease activity among the three groups
PROGESTIN-ONLY CONTRACEPTIVES Progestin-only contraceptives present an alternative option for SLE patients who cannot take estrogen-containing preparations. This includes patients with active disease and those with positive a. PLs, as well as those with other general contraindications. DMPA is more convenient than the pills, and has improved efficacy due to its suppression of ovulation. Progestin-only preparations are more likely to cause irregular, “break-through” bleeding, and this is the most common cause of discontinuation, but unpredictable bleeding is greatest within the first three months of use and diminishes significantly with time
PROGESTIN-ONLY CONTRACEPTIVES Also, DMPA, may cause reversible bone loss due to inhibition of ovulation. A history of fragility fracture, known osteoporosis, or strong risk factors for osteoporosis (such as corticosteroid use) are generally considered contraindications to use of DMPA. An additional disadvantage of DMPA in contrast to the LNg IUD and subdermal system is that there may be a delayed return to fertility. Thus, it is not recommended for patients who plan pregnancy within the next year.
THROMBOEMBOLIC RISK AND PROGESTIN The risk for thromboembolism with progestin-only contraception is very low, and they are generally safe for most SLE patients with or without positive a. PLs. Guidelines of the CDC: Progestin-only contraceptives in woman with SLE and positive (or unknown) a. PL are categorized as a "3" (where the risk of use may exceed the benefits). By contrast, the ACOG guidelines for contraceptive use in women with chronic medical conditions specifically suggest that progestin-only contraceptives may be safer alternatives than estrogen-progestin contraceptives for women with SLE with a. PL, active nephritis, and vascular disease
RISK OF LUPUS FLARE Progestin-only contraceptives have not been observed to increase risk of lupus flare.
BARRIER METHODS Barrier methods of contraception, which include condoms, diaphragms, and spermicides, have low rates of typical use effectiveness. Since highly effective methods are preferred to avoid unintended pregnancy, barrier methods are not appropriate first-line methods. However, reliance on barrier methods may be necessary during periods of acute illness, including acute thrombosis, when other methods may be contraindicated, or as an interim method until more effective methods can be safely instituted. An additional consideration is that condoms are effective for reducing the risk of transmission of sexually transmitted diseases.
EMERGENCY CONTRACEPTION Emergency contraception is an option for all patients with SLE, including those with positive antiphospholipid antibodies (a. PLs).

SUMMARY AND RECOMMENDATIONS
FOR PATIENTS WHO WANT TO USE A LONG-ACTIN REVERSIBLE CONTRACEPTIVE The levonorgestrel (LNg)-containing intrauterine device (IUD) is a safe and effective option for most patients with SLE and/or positive antiphospholipid antibodies (a. PLs).
FOR PATIENTS WHO WANT TO USE AN ORAL HORMONAL CONTRACEPTIVE The OCP may be used in patients with stable low disease activity and documented negative a. PLs. In women with high disease activity; alternative methods such as progestin-only contraceptives and IUDs are preferable. The use of OCP are contraindicated in women with a. PLs with or without SLE, due to the increased risk for thrombosis. The safety of OCP use in patients with fluctuating a. PL titers or positive a. PL on anticoagulation is unknown and is not recommended.
FOR SLE PATIENTS WHO DO NOT WANT TO USE AN IUD AND HAVE HIGH DISEASE ACTIVITY, A POSITIVE APL We suggest progestin-only contraceptives such as the progestin -only pill. Barrier methods are the least effective contraceptive method, and should be reserved for situations when hormone-containing contraceptives or IUDs must be avoided.
RHEUMATOID ARTHRITIS AND CONTRACEPTION The data on the effect of oral contraceptives on RA are conflicting: Ø A case-control study that reviewed the records of 229 women with RA and 458 controls reported no association between RA and the use of oral contraceptives. Ø Two other reports noted a decreased risk of RA among current users of oral contraceptives, as well as a lower risk among women who had used oral contraceptives in the past. Ø The Nurses’ Health Study found that the risk of RA was not altered by a history of oral contraceptive use but reported that a modest protective effect of current users could not be excluded.
RHEUMATOID ARTHRITIS AND CONTRACEPTION In summary, data do not support the concept that oral contraceptives protect against the development of RA, at least among women who have used these medications in the past. The use of oral contraceptives appears neither to worsen nor to improve disease activity.
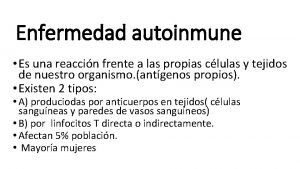
 Case study 87: systemic lupus erythematosus
Case study 87: systemic lupus erythematosus Sle criteria 2020
Sle criteria 2020 Human diseases a systemic approach
Human diseases a systemic approach Voluntary surgical contraception
Voluntary surgical contraception Contraception for over 40s
Contraception for over 40s Lactational amenorrhea
Lactational amenorrhea Ogn and pgn full form in contraception
Ogn and pgn full form in contraception Contraception
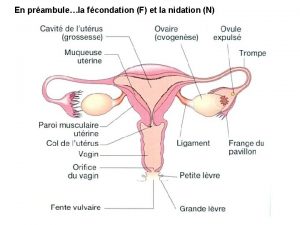
Contraception Mode d'action de la pilule contraceptive
Mode d'action de la pilule contraceptive Victorian era birth control
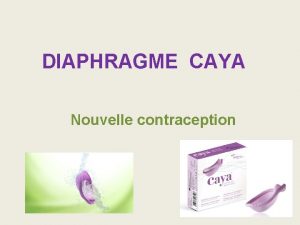
Victorian era birth control Caya diafragma
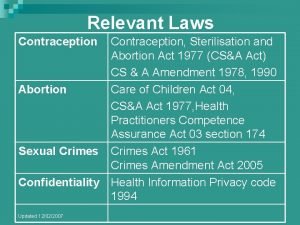
Caya diafragma Contraception sterilisation and abortion act 1977
Contraception sterilisation and abortion act 1977 Diaporama sur la contraception
Diaporama sur la contraception Lupus presentation powerpoint
Lupus presentation powerpoint Lupus research alliance
Lupus research alliance Padrao full house lupus
Padrao full house lupus Nekrotizan papillit nedir
Nekrotizan papillit nedir Jaccoud's arthropathy lupus
Jaccoud's arthropathy lupus Roman hakl
Roman hakl Cetacea canidae panacea ursidae primates
Cetacea canidae panacea ursidae primates Tiopentano
Tiopentano Declinazione lupus
Declinazione lupus Iud and lupus
Iud and lupus Lupus definition
Lupus definition Lupus eritematoso sistémico
Lupus eritematoso sistémico