Approach to a patient with constipation DEFINITION Typically

- Slides: 20
Approach to a patient with constipation
DEFINITION • Typically, it is infrequent bowel movements fewer than 3 per week, but the patients may experience hard stools, a feeling of incomplete evacuation, abdominal discomfort, bloating, and distention, as well as other symptoms (eg, excessive straining, a sense of anorectal blockage during defecation, and the need for manual maneuvers during defecation), which suggest a defecatory disorder. • Frequently, patients who have daily bowel movements describe constipation in form of reduced stool frequency correlated with
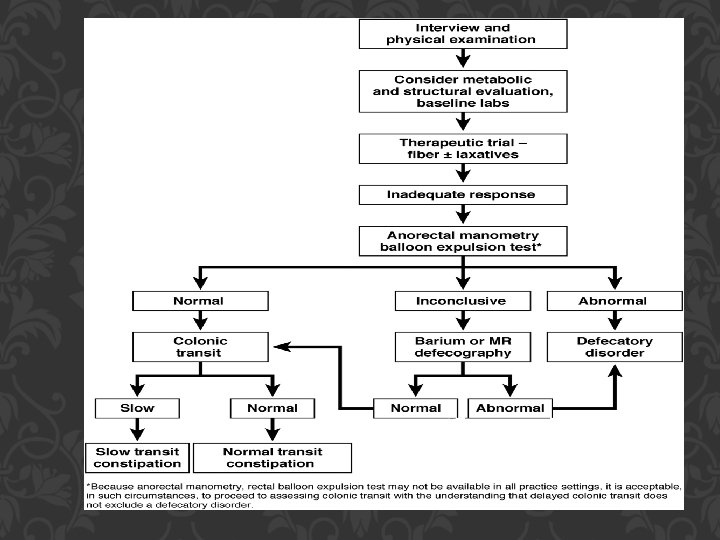
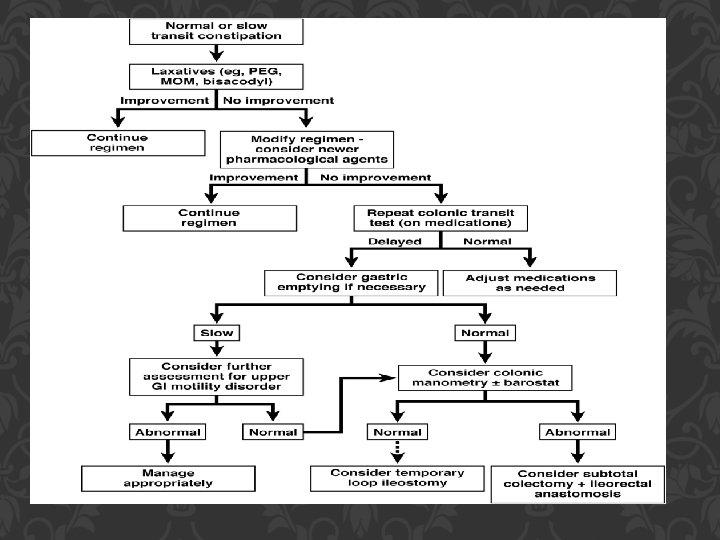
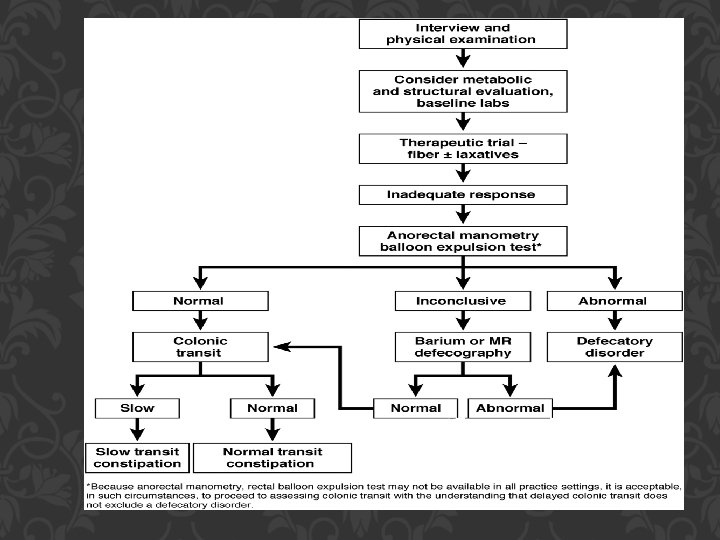
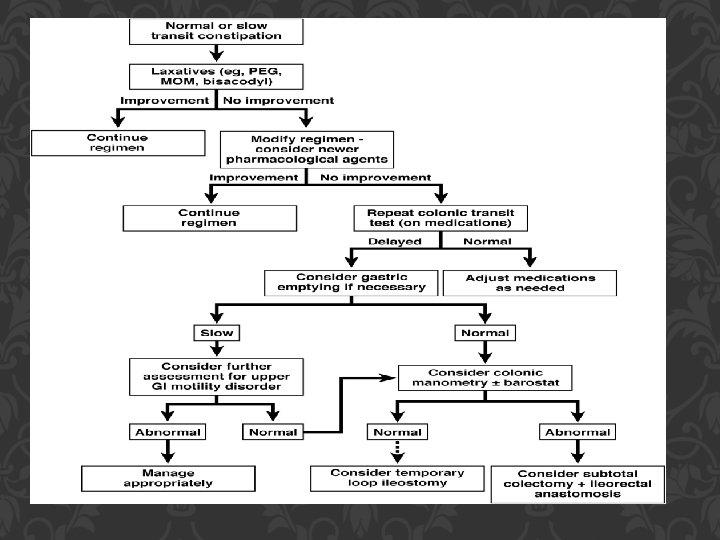
CLINICALLY Symptoms of constipation may be: - Secondary to diseases of the colon (stricture, cancer, anal fissure, proctitis), - Metabolic disturbances (hypercalcemia, hypothyroidism, diabetes mellitus), - Neurologic disorders (parkinsonism, spinal cord lesions). Some of these will respond to specific therapies, but when they are not, the challenge remains one of symptomatic treatment of constipation. - More frequently, constipation is due to disordered colonic and/or pelvic floor/anorectal function. Assessments of colonic transit and anorectal function allow patients to be categorized into 3 subgroups (ie, defecatory disorders, normal transit constipation [NTC], and slow transit constipation [STC]), which facilitates management in refractory
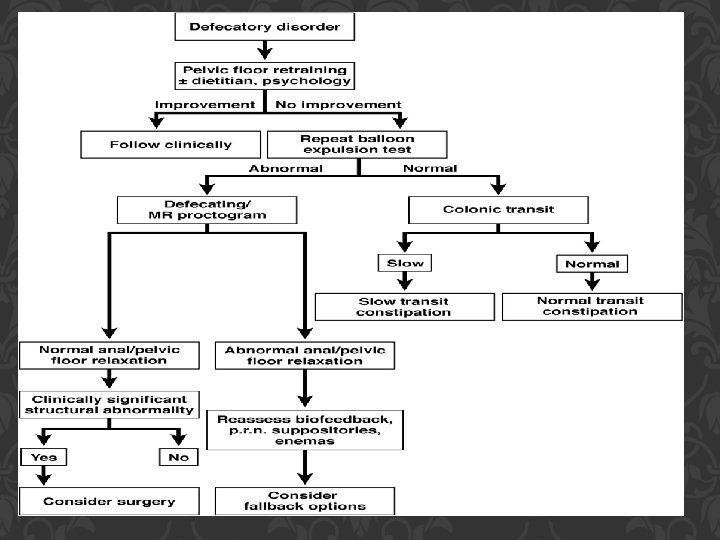
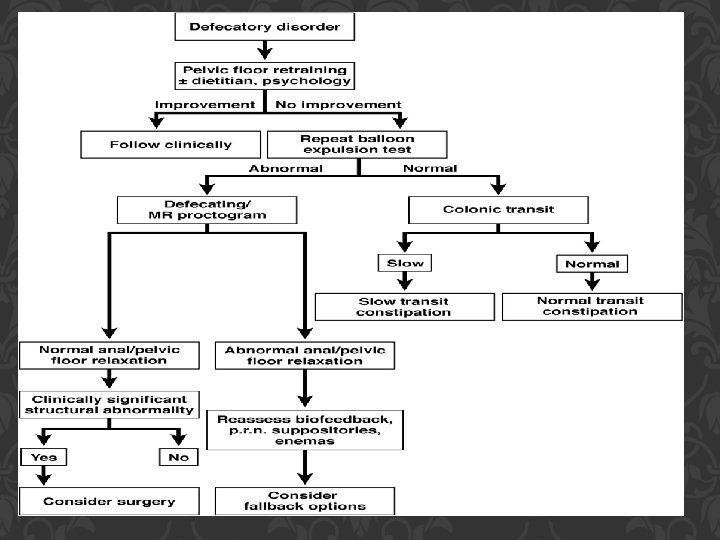
DEFECATORY DISORDERS • They are characterized by impaired rectal evacuation from inadequate rectal propulsive forces and/or increased resistance to evacuation; the latter may result from high anal resting pressure (“anismus”) and/or incomplete relaxation or paradoxical contraction of the pelvic floor and external anal sphincters (“dyssynergia”)during defecation. • Structural disturbances (eg, rectocele, intussusception) and reduced rectal sensation may coexist. • Patients with defecatory disorders may have slow colonic transit that may improve once the defecatory
NTC AND STC • Some patients with STC have colonic motor disturbances (ie, reduced colonic propulsive activity or increased uncoordinated motor activity in the distal colon). • Abnormal (ie, reduced or increased) colonic sensation also been described in chronic constipation, and increased sensation may explain symptoms (ie, abdominal pain and bloating) in some patients. • Resected colonic specimens from patients with STC who undergo colectomy reveal a marked reduction in colonic intrinsic nerves.
COMBINATION DISORDERS Some patients may have combination or overlap disorders (eg, STC with defecatory disorders), perhaps even associated with features of irritable bowel syndrome.
CLINICAL EVALUATION BY HISTORY: • • • What feature is the most distressing? Is it infrequency per se, straining, hard stools, unsatisfied defecation, or symptoms unrelated to bowel habits or defecation per se (eg, bloating, pain, malaise)? The presence of these last characteristics suggests underlying irritable bowel syndrome. The current regimen and bowel pattern should be recorded. How often is a “call to stool” noted? Is the call always answered? What laxatives are being used, how often, and at what dosage? Are suppositories or enemas used in addition? How often are the bowels moved, and what is the consistency of the stools? Importantly, medications hoistry (eg, opiates, anticholinergics, calcium channel blockers). Physicians and patients need to be aware that after a complete purge it will take several days for residue to accumulate such that a normal fecal mass will be formed. Defecatory disorders suspected with prolonged and excessive straining before elimination when evacuatory defects are pronounced, soft stools
BY EXAMINATION The key components of the rectal examination include the following: • In the left lateral position, with the buttocks separated, observe the descent of the perineum during simulated evacuation and the elevation during a squeeze aimed at retention. The perianal skin can be observed for evidence of fecal soiling and the anal reflex tested by a light pinprick or scratch. • During simulated defecation, the anal verge should be observed for any patulous opening (suspect neurogenic constipation with or without incontinence) or prolapse of anorectal mucosa. • The digital examination evaluate resting tone of the sphincter segment and its augmentation by a squeezing effort. Acute localized tenderness to palpation along the puborectalis is a feature of the levator ani syndrome. Finally, the patient should be instructed to integrate the expulsion forces by requesting that she or he “expel my finger. ”
• After the initial history and physical examination we should exclude disorders that are either treatable (eg, hypothyroidism) or important to diagnose early (eg, colon cancer). • A complete blood cell count should be performed. Although metabolic tests (thyroid-stimulating hormone, serum glucose, creatinine, and calcium) • : A colonoscopy should not be performed in patients without alarm features (eg, blood in stools, anemia, weight loss) unless age-appropriate colon cancer • screening has not been performed (strong recommendation, • moderate-quality evidence).
N. B : A colonoscopy should not be performed in patients without alarm features (eg, blood in stools, anemia, weight loss) unless age-appropriate colon cancer screening has not been performed.
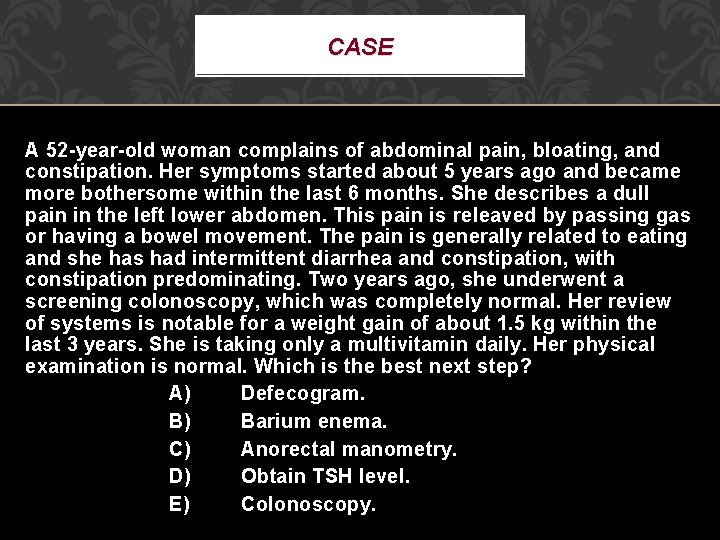
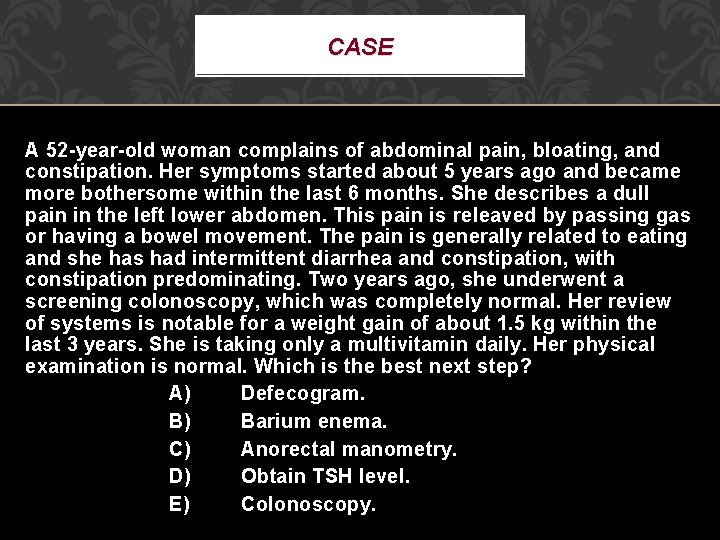
CASE A 52 -year-old woman complains of abdominal pain, bloating, and constipation. Her symptoms started about 5 years ago and became more bothersome within the last 6 months. She describes a dull pain in the left lower abdomen. This pain is releaved by passing gas or having a bowel movement. The pain is generally related to eating and she has had intermittent diarrhea and constipation, with constipation predominating. Two years ago, she underwent a screening colonoscopy, which was completely normal. Her review of systems is notable for a weight gain of about 1. 5 kg within the last 3 years. She is taking only a multivitamin daily. Her physical examination is normal. Which is the best next step? A) Defecogram. B) Barium enema. C) Anorectal manometry. D) Obtain TSH level. E) Colonoscopy.
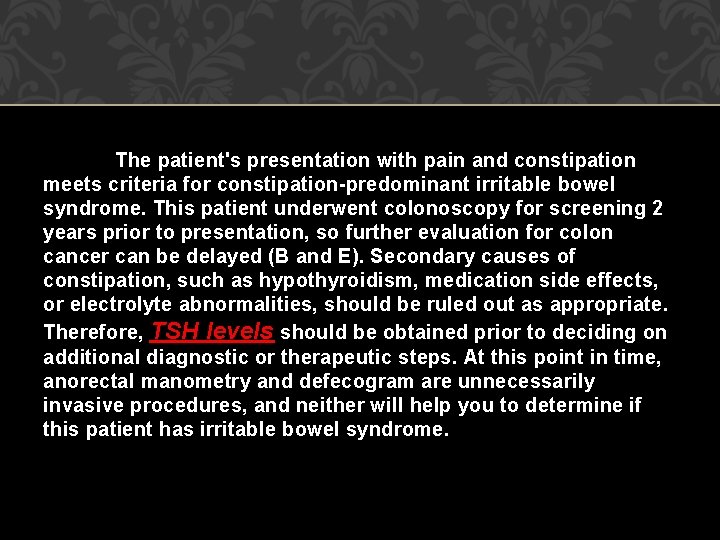
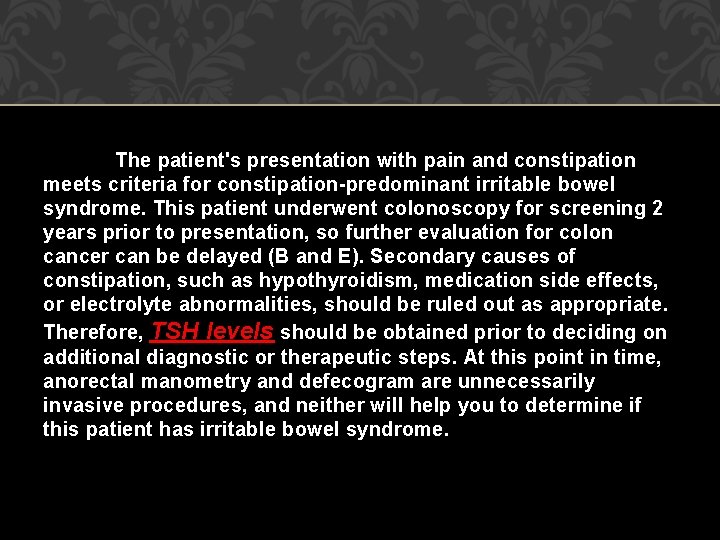
The patient's presentation with pain and constipation meets criteria for constipation-predominant irritable bowel syndrome. This patient underwent colonoscopy for screening 2 years prior to presentation, so further evaluation for colon cancer can be delayed (B and E). Secondary causes of constipation, such as hypothyroidism, medication side effects, or electrolyte abnormalities, should be ruled out as appropriate. Therefore, TSH levels should be obtained prior to deciding on additional diagnostic or therapeutic steps. At this point in time, anorectal manometry and defecogram are unnecessarily invasive procedures, and neither will help you to determine if this patient has irritable bowel syndrome.
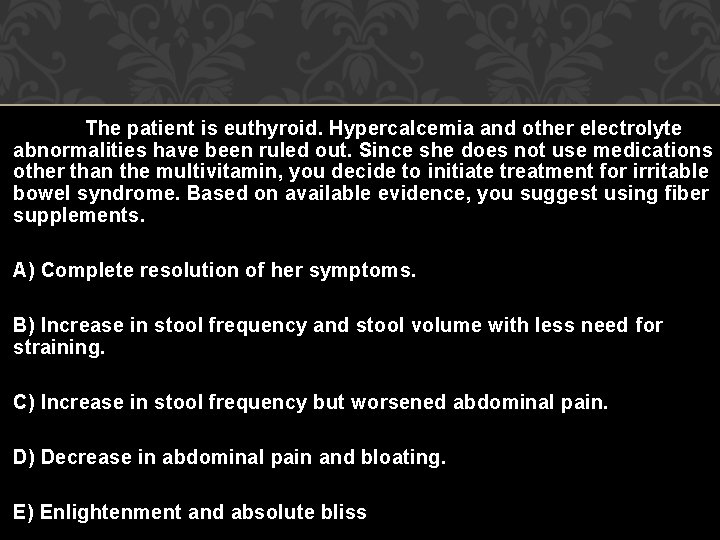
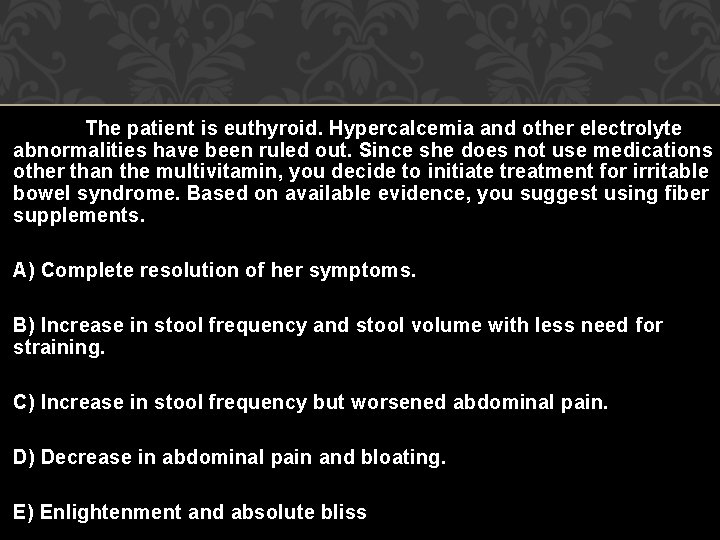
The patient is euthyroid. Hypercalcemia and other electrolyte abnormalities have been ruled out. Since she does not use medications other than the multivitamin, you decide to initiate treatment for irritable bowel syndrome. Based on available evidence, you suggest using fiber supplements. A) Complete resolution of her symptoms. B) Increase in stool frequency and stool volume with less need for straining. C) Increase in stool frequency but worsened abdominal pain. D) Decrease in abdominal pain and bloating. E) Enlightenment and absolute bliss
Fiber supplements increase stool volume and frequency and soften stools, thereby releaving symptoms of constipation. While bowel habits can be successfully changed with bulking agents for constipation or loperamide for diarrhea-predominant irritable bowel syndrome, pain is generally not affected by these measures. In fact, increased fiber intake may transiently worsen some symptoms due to fermentation and generation of gas, potentially resulting in flatulence or bloating.
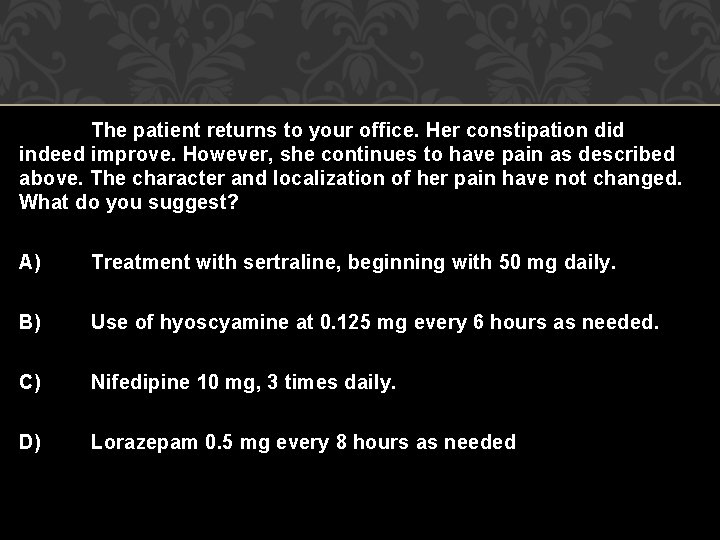
The patient returns to your office. Her constipation did indeed improve. However, she continues to have pain as described above. The character and localization of her pain have not changed. What do you suggest? A) Treatment with sertraline, beginning with 50 mg daily. B) Use of hyoscyamine at 0. 125 mg every 6 hours as needed. C) Nifedipine 10 mg, 3 times daily. D) Lorazepam 0. 5 mg every 8 hours as needed
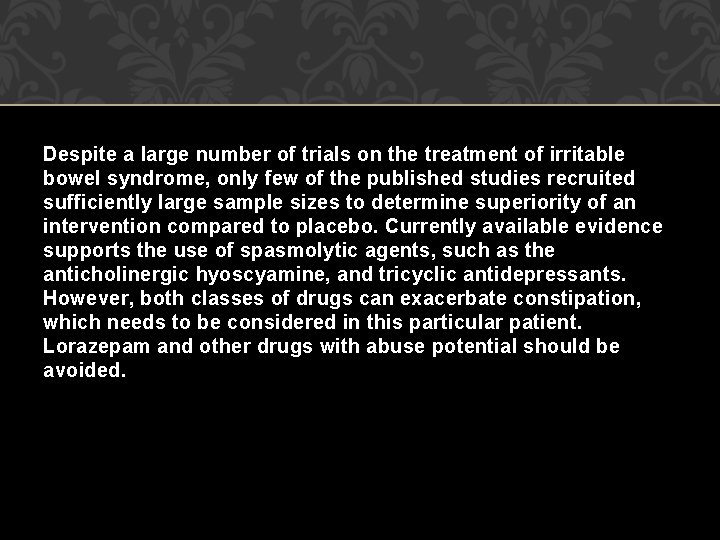
Despite a large number of trials on the treatment of irritable bowel syndrome, only few of the published studies recruited sufficiently large sample sizes to determine superiority of an intervention compared to placebo. Currently available evidence supports the use of spasmolytic agents, such as the anticholinergic hyoscyamine, and tricyclic antidepressants. However, both classes of drugs can exacerbate constipation, which needs to be considered in this particular patient. Lorazepam and other drugs with abuse potential should be avoided.

THANKS