Appraisal and revalidation 2012 Dr Paula Wright Deanery
![Significant events – ‘unexpected event which could or did harm patient [s]’ • two Significant events – ‘unexpected event which could or did harm patient [s]’ • two](https://slidetodoc.com/presentation_image/c3c5e55a105cc5b5a98976d04a66eb39/image-16.jpg)
![Feedback- from colleagues and patients [1]- once every 5 years • Must use standard Feedback- from colleagues and patients [1]- once every 5 years • Must use standard](https://slidetodoc.com/presentation_image/c3c5e55a105cc5b5a98976d04a66eb39/image-17.jpg)
![Feedback- from colleagues and patients [2] • The PCSA is recommending that GPs choose Feedback- from colleagues and patients [2] • The PCSA is recommending that GPs choose](https://slidetodoc.com/presentation_image/c3c5e55a105cc5b5a98976d04a66eb39/image-18.jpg)

![The Appraiser’s Summary [successor to Form 4] • May be integral to a NEW The Appraiser’s Summary [successor to Form 4] • May be integral to a NEW](https://slidetodoc.com/presentation_image/c3c5e55a105cc5b5a98976d04a66eb39/image-21.jpg)

- Slides: 41
Appraisal and revalidation 2012 Dr Paula Wright Deanery lead for sessional GPs
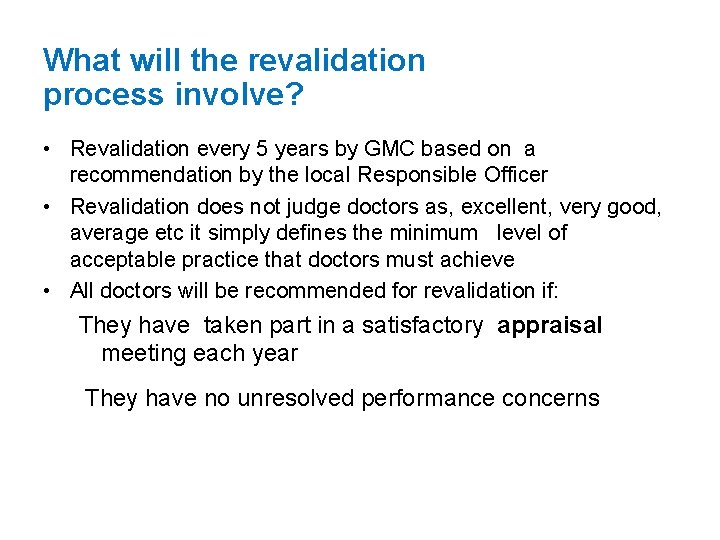
What will the revalidation process involve? • Revalidation every 5 years by GMC based on a recommendation by the local Responsible Officer • Revalidation does not judge doctors as, excellent, very good, average etc it simply defines the minimum level of acceptable practice that doctors must achieve • All doctors will be recommended for revalidation if: They have taken part in a satisfactory appraisal meeting each year They have no unresolved performance concerns
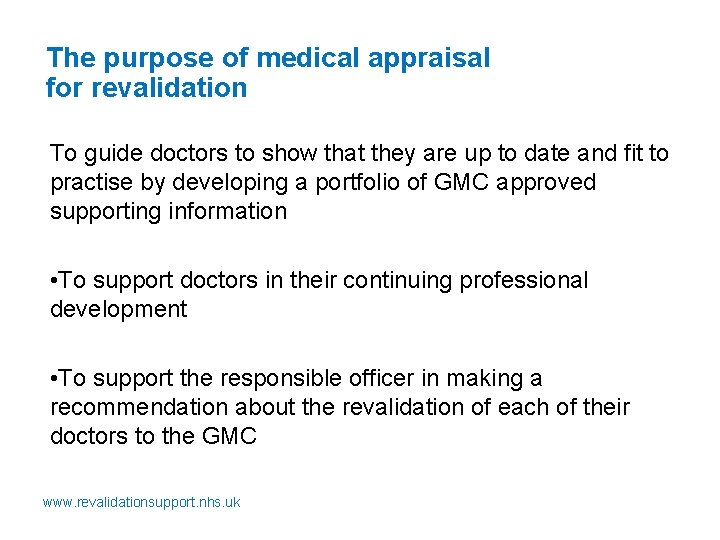
The purpose of medical appraisal for revalidation To guide doctors to show that they are up to date and fit to practise by developing a portfolio of GMC approved supporting information • To support doctors in their continuing professional development • To support the responsible officer in making a recommendation about the revalidation of each of their doctors to the GMC www. revalidationsupport. nhs. uk
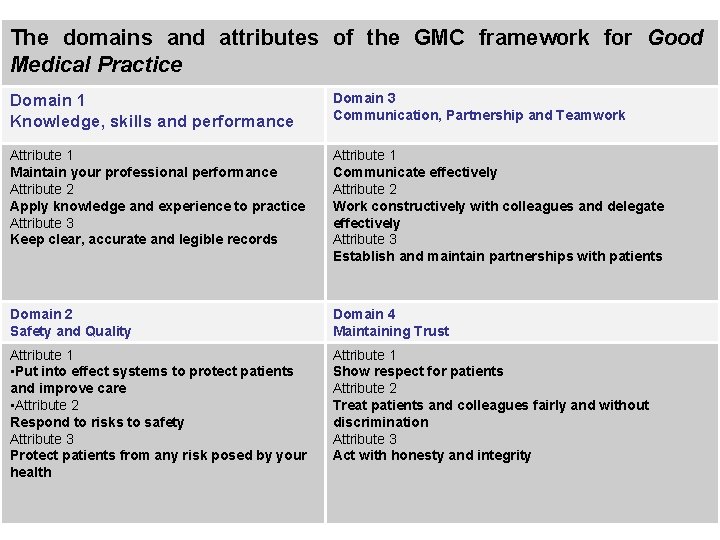
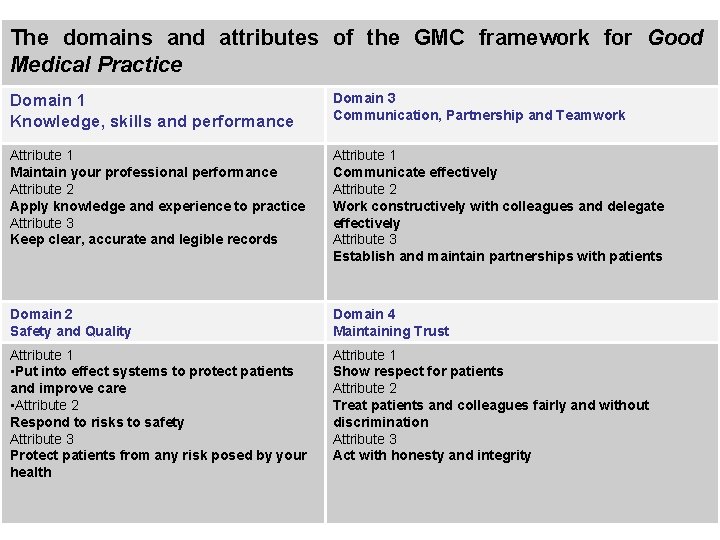
The domains and attributes of the GMC framework for Good Medical Practice Domain 1 Knowledge, skills and performance Domain 3 Communication, Partnership and Teamwork Attribute 1 Maintain your professional performance Attribute 2 Apply knowledge and experience to practice Attribute 3 Keep clear, accurate and legible records Attribute 1 Communicate effectively Attribute 2 Work constructively with colleagues and delegate effectively Attribute 3 Establish and maintain partnerships with patients Domain 2 Safety and Quality Domain 4 Maintaining Trust Attribute 1 • Put into effect systems to protect patients and improve care • Attribute 2 Respond to risks to safety Attribute 3 Protect patients from any risk posed by your health Attribute 1 Show respect for patients Attribute 2 Treat patients and colleagues fairly and without discrimination Attribute 3 Act with honesty and integrity
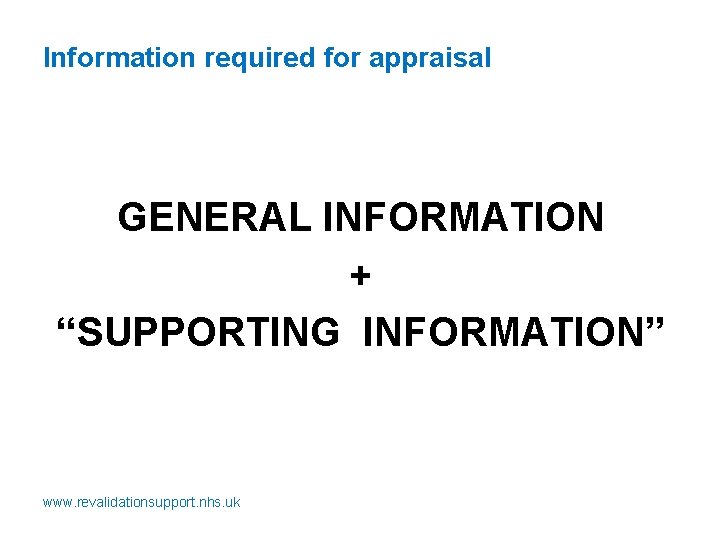
Information required for appraisal GENERAL INFORMATION + “SUPPORTING INFORMATION” www. revalidationsupport. nhs. uk
General information • Personal details • Scope of work –list of all the roles undertaken (documents showing review of these roles should be submitted to your appraiser ) • Record of previous annual appraisals • Personal Development Plan and its review • Probity and health declarations
Supporting Information • GMC “Good Medical Practice” (revised) • GMC “Supporting information for appraisal and revalidation” • RCGP Guide To revalidation for GPs (version 6)
GMC and Royal Colleges • GMC guidance is considered mandatory and the basis for any legal challenge in the future • Colleges are all making some additional guidance but ultimately this is advisory –doctors will be able to argue that they should be able to revalidate based on adherence to the GMC guidance alone • RCGP has just published latest version of their guide www. rcgp. org. uk- the main differences between this and the GMC document have been high-lighted
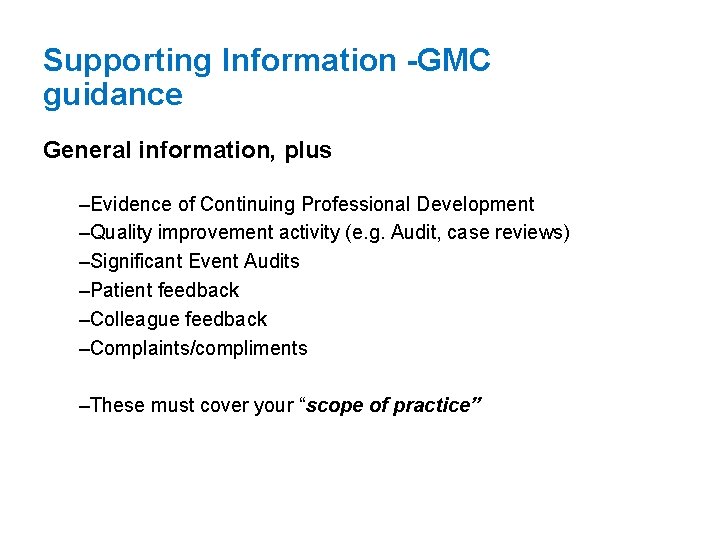
Supporting Information -GMC guidance General information, plus –Evidence of Continuing Professional Development –Quality improvement activity (e. g. Audit, case reviews) –Significant Event Audits –Patient feedback –Colleague feedback –Complaints/compliments –These must cover your “scope of practice”
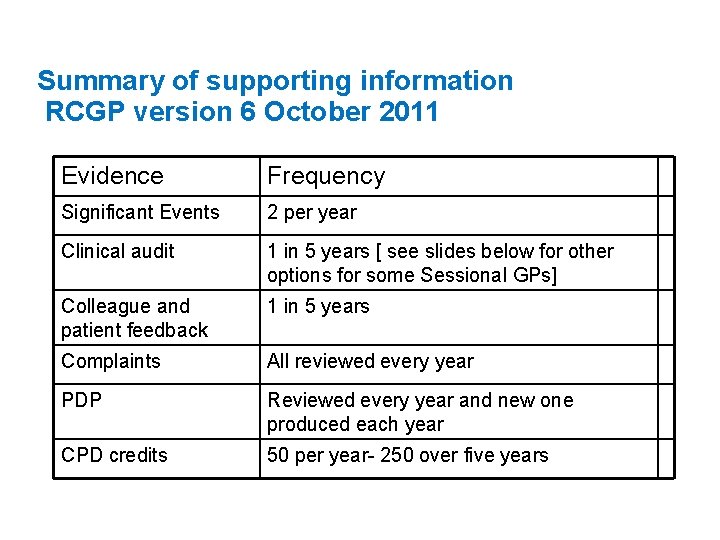
Summary of supporting information RCGP version 6 October 2011 Evidence Frequency Significant Events 2 per year Clinical audit 1 in 5 years [ see slides below for other options for some Sessional GPs] Colleague and patient feedback 1 in 5 years Complaints All reviewed every year PDP Reviewed every year and new one produced each year CPD credits 50 per year- 250 over five years
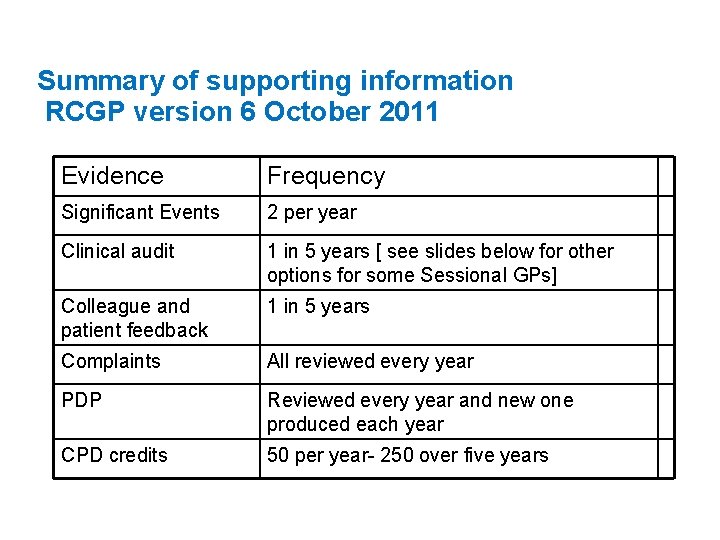
Supporting information: non standard GPs • RCGP guide recognises that peripatetic locums, OOHs doctors, rural remote GPs, etc may have difficulty with some of these evidence requirements , especially audit /SEA and MSF • All GPs need to demonstrate that they regularly participate in activities that review and evaluate the quality of their work. These should include an element of evaluation and action, and where possible, demonstrate an outcome or change. See guidance from NEPCSA: on supporting information for ‘non standard’ GPs.
Detailed guidance for sessional Gps Deanery Sessional GP page: NEPCSA Guidance on Supporting Information for Non. Standard GPs http: //northerndeanery. ncl. ac. uk/Northern. Deanery/primarycare/continuing-practice/retainer-scheme/information-forsessional-gps Also Career Break Advice December 2011 www. revalidationsupport. nhs. uk
Continuing Professional Development • CPD log must demonstrate at least 50 CREDITS • 1 hour=1 credit • CPD should cover whole scope of practice-ie all clinical and other roles • Impact multiples hours by 2 • Record of educational activities [meetings, conferences, reading etc] and core learning points
Audit and sessional GPs No Access to records outside of consulting time Lack of Skills and help with in searches No “specific clinical role” to audit; No organisational influence Mobility between practices if locum Numbers with a single conditions seen by locum or parttime GP is very small personally delivered care means “process” based for which there is no evidence base (e. g. Record keeping) “Key is to demonstrate reflection, learning and improvement”-RCGP www. revalidationsupport. nhs. uk
Quality improvement activities • • • Clinical audit (1/5 yr, or alternative) Case review, (GMC) Quality Improvement Plan [QUIP], (GMC) Review of referrals, review of record keeping * Review of 20 consultations in random surgery with feedback from colleague * • Prospective condition based review * • Audit effectiveness of teaching or health policy change (GMC) Key is to demonstrate reflection, learning and improvement *NEPCSA interpretation of RCGP statement above
![Significant events unexpected event which could or did harm patient s two Significant events – ‘unexpected event which could or did harm patient [s]’ • two](https://slidetodoc.com/presentation_image/c3c5e55a105cc5b5a98976d04a66eb39/image-16.jpg)
Significant events – ‘unexpected event which could or did harm patient [s]’ • two SEAs each year [RCGP guidance] • Personal to you (involvement in the care not just the discussion meeting) • Lessons learnt , areas for future learning and actions taken as a result of SEA should also be discussed- • SEAs can be discussed in a learning/study group if practice meeting not accessible
![Feedback from colleagues and patients 1 once every 5 years Must use standard Feedback- from colleagues and patients [1]- once every 5 years • Must use standard](https://slidetodoc.com/presentation_image/c3c5e55a105cc5b5a98976d04a66eb39/image-17.jpg)
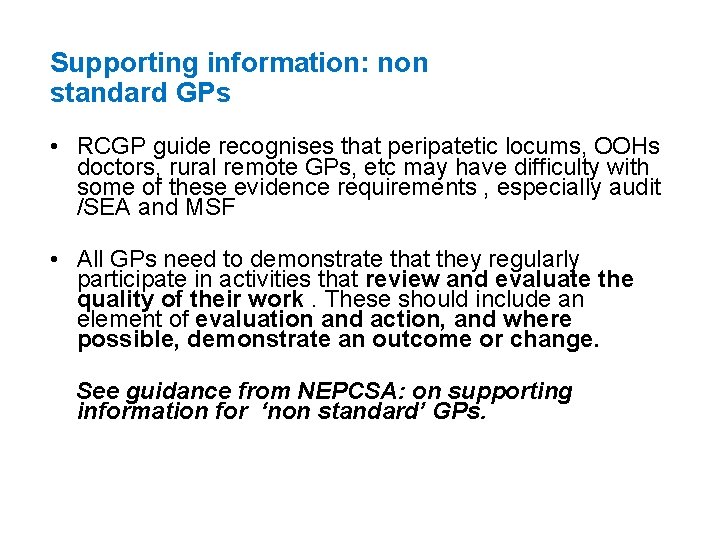
Feedback- from colleagues and patients [1]- once every 5 years • Must use standard surveys–usually require a minimum of 15 colleagues and 35 patients • Feedback should come from whole scope of practice [all the roles eg clinical, academic etc] • The feedback is discussed at the appraisal meetingsupport from GP tutors on request for appraisees • Feedback should be seen as FORMATIVE-not a pass or fail exercise- development areas are identified and addressed in the PDP • Serious performance issues threatening patient safety arise very rarely ‘de novo’ via feedback exercises
![Feedback from colleagues and patients 2 The PCSA is recommending that GPs choose Feedback- from colleagues and patients [2] • The PCSA is recommending that GPs choose](https://slidetodoc.com/presentation_image/c3c5e55a105cc5b5a98976d04a66eb39/image-18.jpg)
Feedback- from colleagues and patients [2] • The PCSA is recommending that GPs choose from list in RCGP guide-these are approved for patients and colleagues • CFEP surveys http: //www. cfepsurveys. co. uk/products/general-practice/360. aspx • Edgecumbe -http: //www. edgecumbehealth. co. uk/edgecumbe-doctor 360. php • GMC surveys –free to use but need to be collated independently Further guidance of feedback is coming from both the revalidation Support Team and the GMC in the next 2 -3 months –so we advise to wait until after 1/4/12 before recommending appraisees start collecting feedback Training on use and interpretation of these tools will be provided for appraisers later in the year
Complaints • All patient complaints must be discussed each year at appraisal • Learning points and actions must be recorded • Compliments can be listed in this section

Where to get advice Your appraiser well in advance and also submit your folder 2 -3 weeks in advance so they can alert you to any gaps GP tutor for Sessional Gps: Paula Wright pfwright@doctors. org. uk Steve Blades stephen. blades@nhs. net www. revalidationsupport. nhs. uk
![The Appraisers Summary successor to Form 4 May be integral to a NEW The Appraiser’s Summary [successor to Form 4] • May be integral to a NEW](https://slidetodoc.com/presentation_image/c3c5e55a105cc5b5a98976d04a66eb39/image-21.jpg)
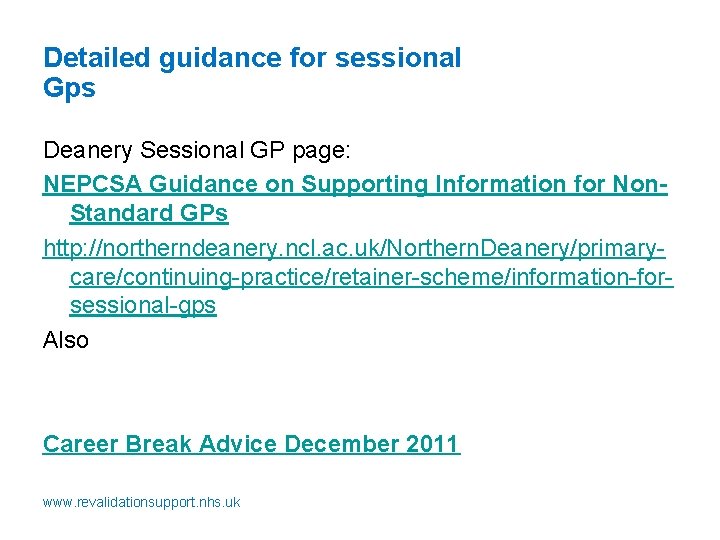
The Appraiser’s Summary [successor to Form 4] • May be integral to a NEW PDF DOCUMENT : MAG BEING PILOTED (Into which you can upload documents). • Four sections =Domains of Good Medical Practice (revised) • The appraiser will indicate whether process delivers coverage of all four domains [without specific mapping of evidence to specific domains] • extra comments box to highlight any additional issues , challenges or aspirations • Further guidance as soon as the final version of the PDF form is published in April 2012
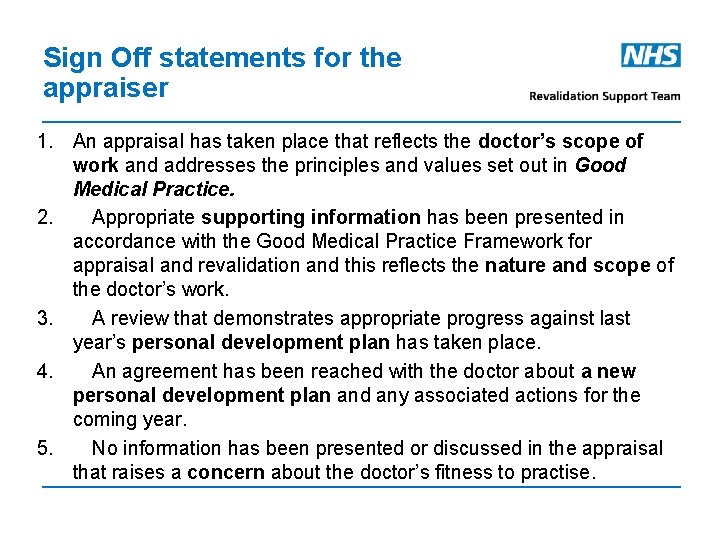
Sign Off statements for the appraiser 1. An appraisal has taken place that reflects the doctor’s scope of work and addresses the principles and values set out in Good Medical Practice. 2. Appropriate supporting information has been presented in accordance with the Good Medical Practice Framework for appraisal and revalidation and this reflects the nature and scope of the doctor’s work. 3. A review that demonstrates appropriate progress against last year’s personal development plan has taken place. 4. An agreement has been reached with the doctor about a new personal development plan and any associated actions for the coming year. 5. No information has been presented or discussed in the appraisal that raises a concern about the doctor’s fitness to practise.
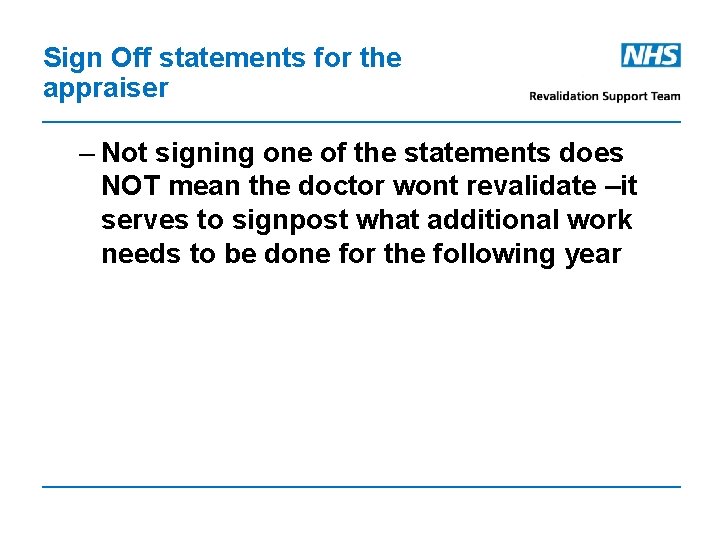
Sign Off statements for the appraiser – Not signing one of the statements does NOT mean the doctor wont revalidate –it serves to signpost what additional work needs to be done for the following year
Additional information RO information sharing The RO should be aware of the following issues when considering the above statements
PDP- definition (RCGP) a formal agreement, between the appraisee and appraiser, on the learning and development needs of the appraisee, identified at the appraisal interview, with an outcome based learning plan for the subsequent year
PDPs - What Goes Into Them Personal development Targeted learning Practice development OK if also involves personal learning Professional goals Professional or career development Collection of evidence Acceptable as a one off
Personal Development aims - best practice 1. 2. 3. 4. 5. Link to actions from appraisal summary Meet SMART criteria Reflect appraisee’s approach to learning Link to improving patient care Address gaps in supporting information or mandatory training 6. identify development needs identified through reflection on practice, SEAs, case reviews , audit etc 7. add any other development goals or aspirations identified by the
PDPs: produce –SMART objectives • SMART is Specific, Manageable, Achievable, Realistic, Time frame • Make sure core gaps from appraisal are addressed. • Some clinical skills are easy to express specifically e. g ‘To learn how to perform soft tissue injections’ • Be specific in defining knowledge gaps • eg ‘need to know how to initiate insulin’ rather than ‘Diabetes Mellitus’ • Aim for 5 -8 items –too long a list is unrealistic-fewer may be acceptable if large eg ‘become a trainer’
GMC actions at the point of revalidation • REVALIDATE=RO recommendation that Dr has engaged in appraisal and no concerns • DEFER DECISION [usually for one year] where insufficient information eg maternity leave, sick leave or sabbatical or concerns still pending • REFER to GMC Performance Procedures-if serious unresolved concerns • ADMINISTRATIVE REMOVAL from GMC register if the Dr has failed to engage for no clear reason
What will happen to doctors who do not revalidate? • Annual appraisal should identify doctors in difficulty at an early stage • Support can be offered - [ remediation, educational support, occupational health review] • No doctor should ‘fail’ revalidation who has had satisfactory appraisals and no unresolved performance concerns • A few doctors [? ? 1 -2 %] will not pass revalidation and will lose their licence to practise if remediation fails
When will revalidation be introduced? • Legal sign-off by Government in 2012 • ‘early adopter’ volunteers will start in 2012 • Aim is for all doctors to get through the first cycle of revalidation by 2016 • 2016 -2017 will be a year of review of the process • New 5 year cycle will start in 2017
Handling concerns • Most appraisals will be satisfactory with no concerns about engagement or the Supporting Information • On very rare occasions the appraisal will be stopped because of serious threat to patient safety • A small number may raise concerns that do not currently affect performance , but might do so in the future if not addressed- eg health/stress/partnership/family issues – Discuss these with your GP tutor, or directly with the Clinical Lead for Appraisal or with the Responsible Officer – Indicate on the checklist that the Summary should be read and whether a 6 month follow up is advised – Use the list of support agencies if appropriate to do so
RST Key messages Appraisers all receiving top up training based on RST module: Key messages are to appraisers: First, do no harm If in doubt – ask
NEPCSA-Early Adopter Status for Revalidation • The purpose is to test the GMC’s systems and processes • It will test the PCSA processes as well • Will enable some GPs who wish to, to revalidate later this year • We are likely to offer this first to appraisers and GP tutors • It is voluntary • We do know as yet how the GMC wishes to identify who will go first to revalidate- it may be through joint working with GMC via the ELO
Booking your appraisal • 200 appraisers covering North east and 2500 Gps. • Appraisals by birthday month • Must book via new website being launched feb march 2012 www. gpappraisalsne. nhs. uk • Select appraiser according to their availability that month • Website has Bio/profile on the appraiser • Maternity leave, Sabbaticals, Sick leave etc –apply for deferrment via website
Career breaks RCGP talks about minimum portfolio: • 3 out of 5 appraisals • 200 clinical sessions (of which 100 should be undertaken in the 2 years prior to revalidation). • 150 credits All yet to be tested in real life www. revalidationsupport. nhs. uk
Responsible Officers – key messages • ROs are accountable to the CEO of the PCO and the GMC • Every 5 years we are required to make a recommendation to the GMC registrar about a doctors suitability to be revalidated – includes appraisal and information from clinical governance systems where the doctor works • Clinical governance is important and with appraisal is the cornerstone of the RO’s work • Appraisal is mandatory !!– you will lose your license if you don’t participate without good reason, or fail to provide information requested by the GMC - even if you have done nothing else wrong!! • Revalidation is going to happen later this year
Responsible Officers – who are they? • Dr Mike Guy NHS North of Tyne • Dr Geoff Stephenson NHS South of Tyne and Wear • Dr Hilton Dixon NHS Durham and Darlington • Dr James Gossow NHS Tees • NB In the event of any conflict of interest , Mike and Geoff act as deputies for each others organisations as do Hilton and James

Responsible Officers –roles and responsibilities – evaluate doctors’ fitness to practise; – ensure annual appraisals are carried out and make recommendations to the GMC around doctors’ revalidation – monitor doctors’ conduct and performance; – investigate and take appropriate action to deal with concerns about doctors; – where appropriate, report concerns to the General Medical Council; – carry out pre-employment checks on doctors
Responsible Officers – Employment Liaison Officer • The GMC have appointed an Employment Liaison Officer for every SHA region • Helen Dolan is the ELO for the North East her role is : – To enable closer working relationships between Trusts and GMC – To facilitate greater consistency of decision making where there are performance concerns • Appraisers may have involvement when appraising GPs who have performance concerns or GMC conditions
Useful websites for further information • UK Revalidation Support Team http: //www. revalidationsupport. co. uk/ • Royal College of General Practitioners http: //www. rcgp. org. uk/revalidation. aspx • General Medical Council http: //www. gmc-uk. org/