Applying behavioural science frameworks to design quality improvement

Applying behavioural science frameworks to design quality improvement interventions: The Behaviour Change Wheel approach Dr. Fabiana Lorencatto Research Lead, UCL Centre for Behaviour Change, UK Scottish Improvement Science Collaborating Centre- Quality Improvement Seminar Series Stirling September 2018 @UCLBehave. Change @fabilorencatto
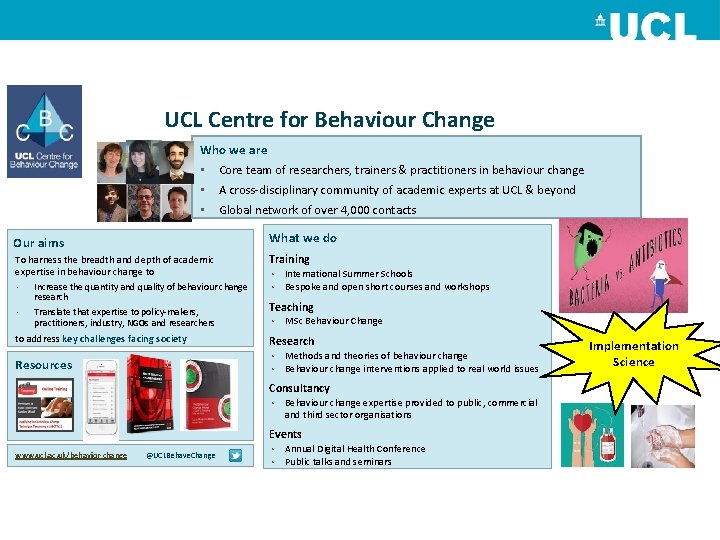
UCL Centre for Behaviour Change Who we are • Core team of researchers, trainers & practitioners in behaviour change • A cross-disciplinary community of academic experts at UCL & beyond • Global network of over 4, 000 contacts Our aims What we do To harness the breadth and depth of academic expertise in behaviour change to Training • Increase the quantity and quality of behaviour change research • Translate that expertise to policy-makers, practitioners, industry, NGOs and researchers to address key challenges facing society • • International Summer Schools Bespoke and open short courses and workshops Teaching • MSc Behaviour Change Research Methods and theories of behaviour change • Behaviour change interventions applied to real world issues • Resources Consultancy • Behaviour change expertise provided to public, commercial and third sector organisations Events www. ucl. ac. uk/behavior-change @UCLBehave. Change Annual Digital Health Conference • Public talks and seminars • Implementation Science
This talk: • Why should we think about behaviour (change) when it comes to QI? • Limitations of current approaches to designing QI interventions • A behavioural science approach – Step-by-step systematic, theory-based method – Frameworks and tools to help simplify complexity (without over simplifying!) • Workshop: Applying this approach to an improvement scenario
Why behaviour change?
Translating evidence into practice…

Reality….
Evidence-practice gaps: • Despite training and guidelines, many healthcare professionals do not always act in line with evidence-based recommendations – Making referrals, prescribing medications, giving advice Many of the gaps we are trying to address are behaviours…
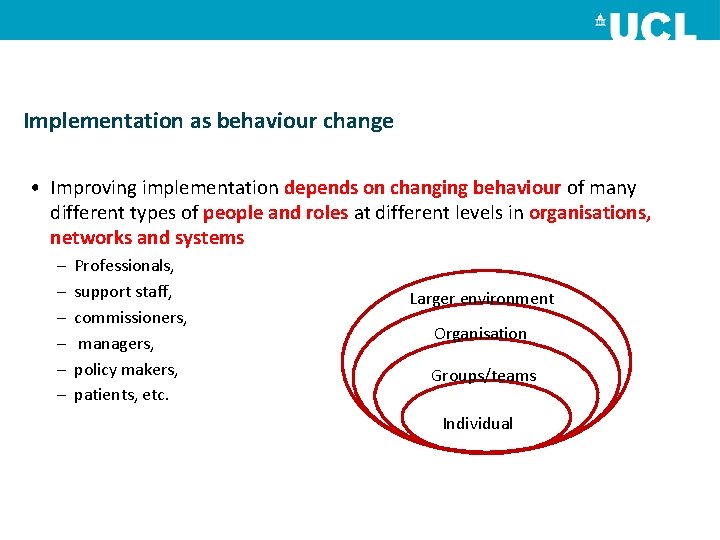
Implementation as behaviour change • Improving implementation depends on changing behaviour of many different types of people and roles at different levels in organisations, networks and systems – – – Professionals, support staff, commissioners, managers, policy makers, patients, etc. Larger environment Organisation Groups/teams Individual
Interventions to improve implementation • Significant investment of time and resources into strategies to improve effectiveness and quality of care • Many have achieved modest and variable success – Why? – One important reason: • Often not understanding the problem in terms of behaviour…
Traditional approaches to designing QI interventions:
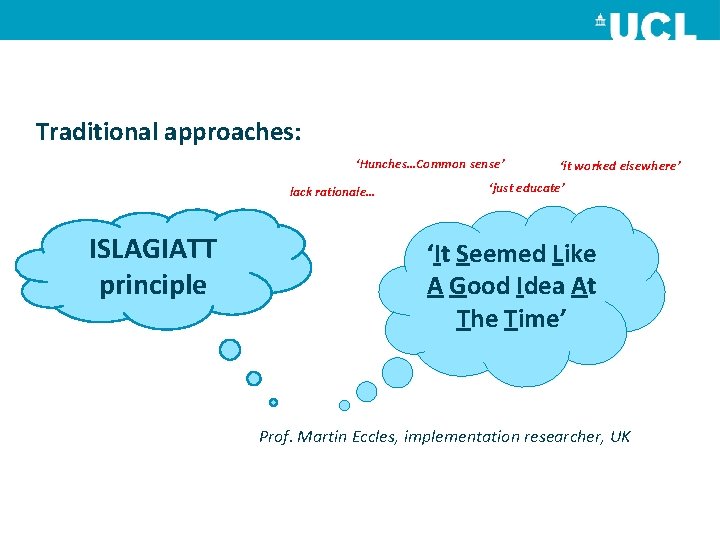
Traditional approaches: ‘Hunches…Common sense’ lack rationale… ISLAGIATT principle ‘it worked elsewhere’ ‘just educate’ ‘It Seemed Like A Good Idea At The Time’ Prof. Martin Eccles, implementation researcher, UK
Why is this a problem? Effect
An alternative approach to designing behavior change interventions…
Going to see your GP …. Approach behaviour change 1. Examine the problem interventions in similar manner… 2. Make a formulation and diagnosis 3. Prescribe a treatment
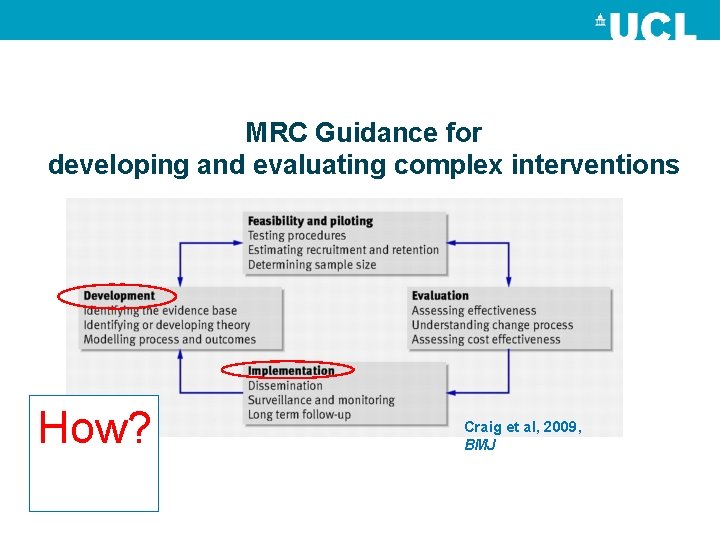
MRC Guidance for developing and evaluating complex interventions How? Craig et al, 2009, BMJ
Science of behaviour change: • Behaviour change isn’t easy or common sense • No magic bullets… • Interrelated theories, frameworks and evidence-based principles • Systematic, step-by step, transparent and more effective approach to intervention design • Policy makers, practitioners, researchers from different disciplines and levels of experience Michie S, Atkins L, West R. The behaviour change wheel. A guide to designing interventions. 1 st ed. Great Britain: Silverback Publishing. 2014. https: //www. ucl. ac. uk/behaviour-change/files/bcw-summary. pdf Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation science. 2011 Dec; 6(1): 42.
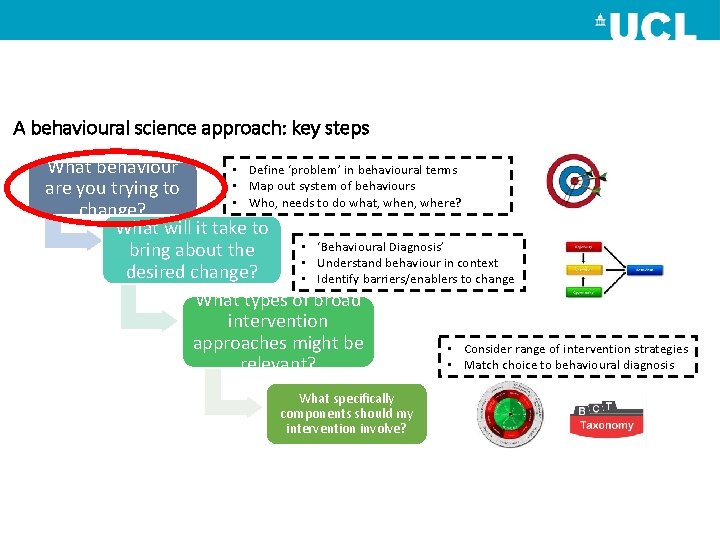
A behavioural science approach: key steps What behaviour • Define ‘problem’ in behavioural terms • Map out system of behaviours are you trying to • Who, needs to do what, when, where? change? What will it take to • ‘Behavioural Diagnosis’ bring about the • Understand behaviour in context desired change? • Identify barriers/enablers to change What types of broad intervention approaches might be • Consider range of intervention strategies • Match choice to behavioural diagnosis relevant? What specifically components should my intervention involve?
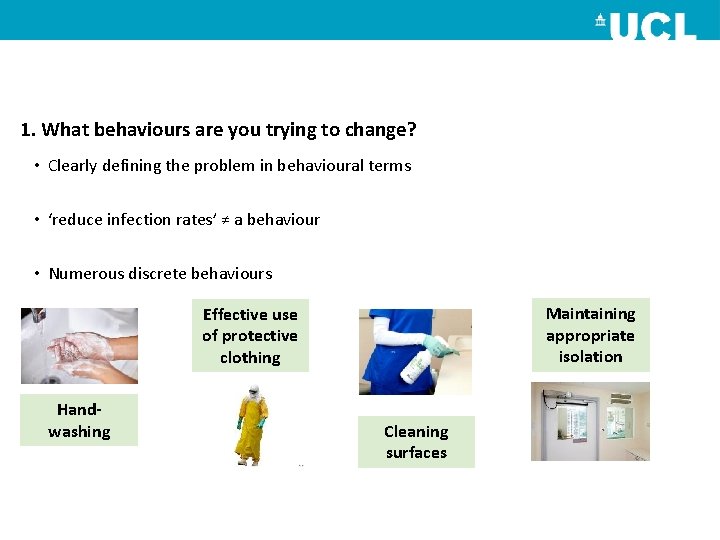
1. What behaviours are you trying to change? • Clearly defining the problem in behavioural terms • ‘reduce infection rates’ ≠ a behaviour • Numerous discrete behaviours Maintaining appropriate isolation Effective use of protective clothing Handwashing Cleaning surfaces
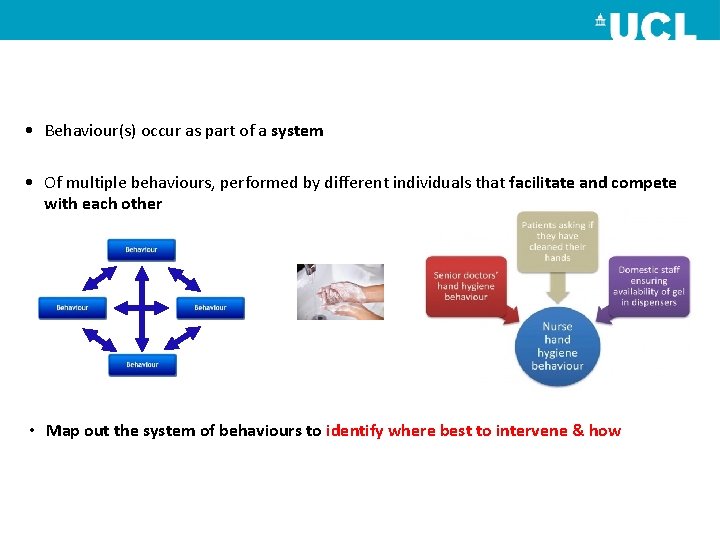
• Behaviour(s) occur as part of a system • Of multiple behaviours, performed by different individuals that facilitate and compete with each other • Map out the system of behaviours to identify where best to intervene & how
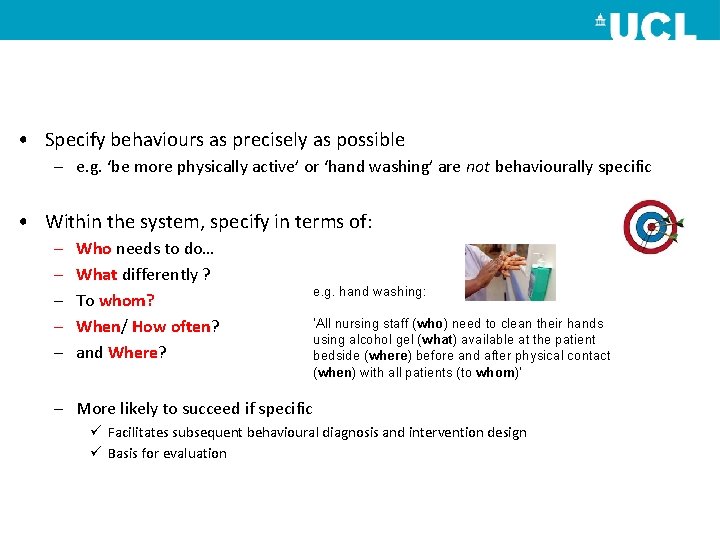
• Specify behaviours as precisely as possible – e. g. ‘be more physically active’ or ‘hand washing’ are not behaviourally specific • Within the system, specify in terms of: – – – Who needs to do… What differently ? To whom? When/ How often? and Where? e. g. hand washing: ‘All nursing staff (who) need to clean their hands using alcohol gel (what) available at the patient bedside (where) before and after physical contact (when) with all patients (to whom)’ – More likely to succeed if specific ü Facilitates subsequent behavioural diagnosis and intervention design ü Basis for evaluation
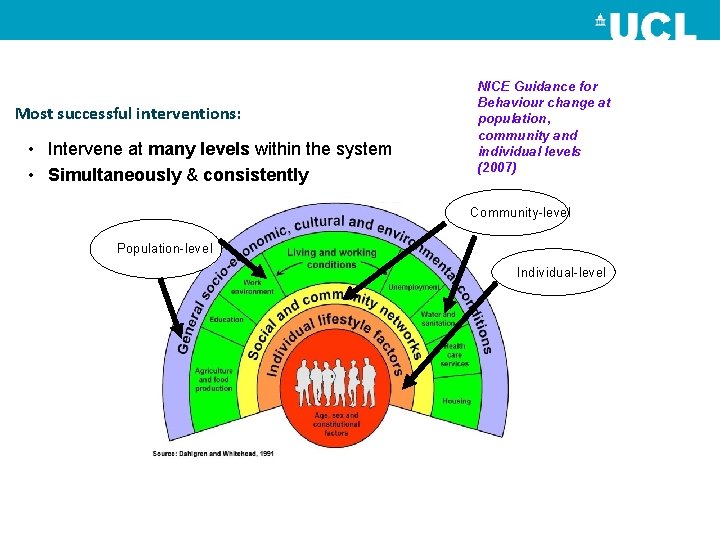
Most successful interventions: • Intervene at many levels within the system • Simultaneously & consistently NICE Guidance for Behaviour change at population, community and individual levels (2007) Community-level Population-level Individual-level
However… • May not always be feasible… • Different behaviours = different determinants • Intervene intensively on 1 -2 key behaviours • Introduce change incrementally
Which behaviour to start with? • Ask: – If I change this, what is the likely impact? – Feasibility, resources, preference, acceptability, cost? – Consider interrelationship of behaviours…. – Spillover/generalisability to other behaviours and people within the system?
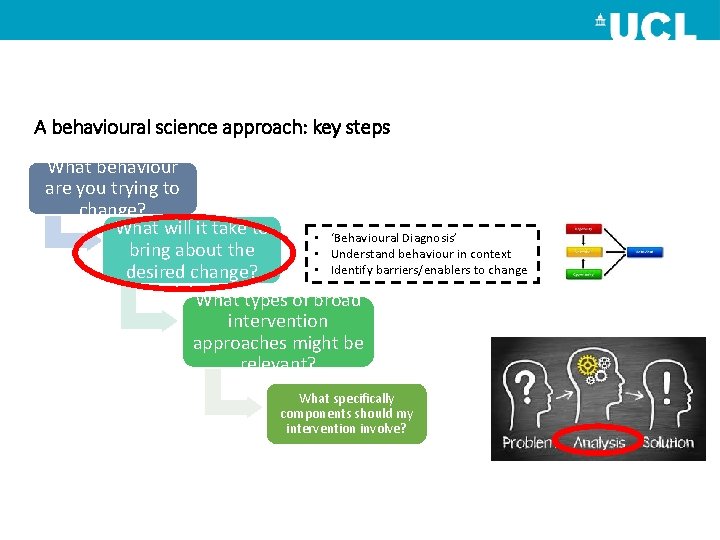
A behavioural science approach: key steps What behaviour are you trying to change? What will it take to • ‘Behavioural Diagnosis’ bring about the • Understand behaviour in context • Identify barriers/enablers to change desired change? What types of broad intervention approaches might be relevant? What specifically components should my intervention involve?
2. Understand the behaviour in context (‘Behavioural diagnosis’) • Why are behaviours as they are? • What needs to change for the desired behaviour/s to occur? • Clinical practice is a form of human behaviour… • Answering these Qs helped by a theory of behaviour change Prof. Susan Michie

Theory…. essary c e n y l e k tructs li s n o c f o al set m i n i m change o t r n o i i v e t a a h r o integ t for be t n s e t i c p i f m f e u Att and s Michie SF, West R, Campbell R, Brown J, Gainforth H. ABC of behaviour change theories. Silverback Publishing; 2014.
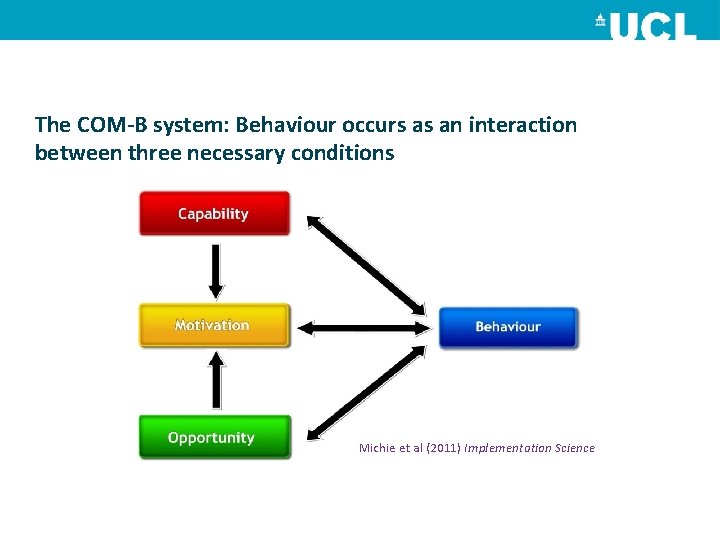
The COM-B system: Behaviour occurs as an interaction between three necessary conditions Michie et al (2011) Implementation Science
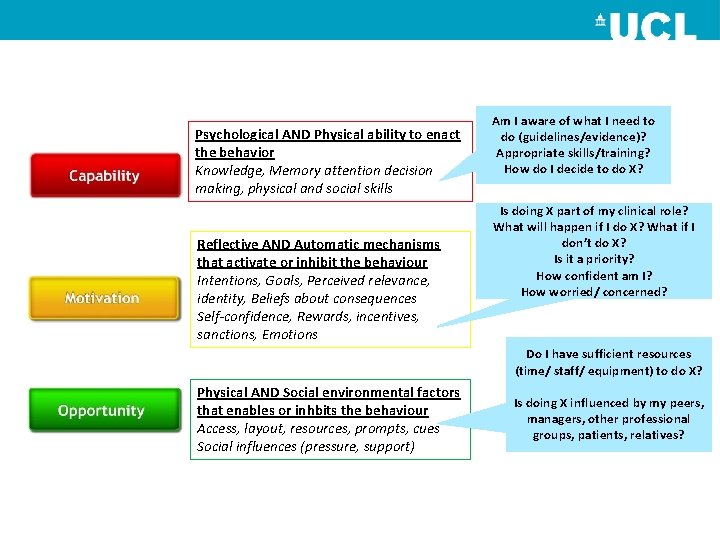
Psychological AND Physical ability to enact the behavior Knowledge, Memory attention decision making, physical and social skills Reflective AND Automatic mechanisms that activate or inhibit the behaviour Intentions, Goals, Perceived relevance, identity, Beliefs about consequences Self-confidence, Rewards, incentives, sanctions, Emotions Am I aware of what I need to do (guidelines/evidence)? Appropriate skills/training? How do I decide to do X? Is doing X part of my clinical role? What will happen if I do X? What if I don’t do X? Is it a priority? How confident am I? How worried/ concerned? Do I have sufficient resources (time/ staff/ equipment) to do X? Physical AND Social environmental factors that enables or inhbits the behaviour Access, layout, resources, prompts, cues Social influences (pressure, support) Is doing X influenced by my peers, managers, other professional groups, patients, relatives?
Gathering ‘behavioural diagnosis’ data using COM-B • Interviews/focus groups: for in-depth qualitative data • Questionnaires: for larger samples • Observations • Structured discussion: if resource poor
E. g. Conducting behavioural diagnosis using COM-B • High rates of inappropriate antibiotic use in care homes – contributing to antimicrobial resistance • Applied COM-B to explore factors influencing antibiotic prescribing • Semi-structured interviews with general practitioners, consultants, nurses and community pharmacists. • Structured interview questions around COM-B
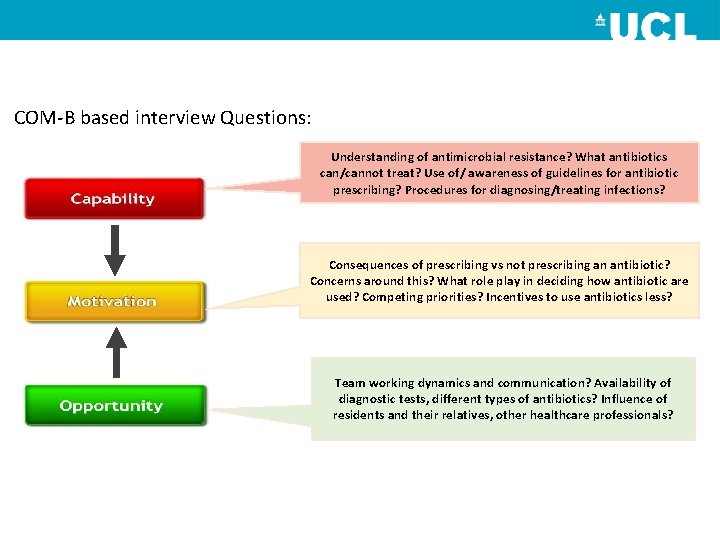
COM-B based interview Questions: Understanding of antimicrobial resistance? What antibiotics can/cannot treat? Use of/ awareness of guidelines for antibiotic prescribing? Procedures for diagnosing/treating infections? Consequences of prescribing vs not prescribing an antibiotic? Concerns around this? What role play in deciding how antibiotic are used? Competing priorities? Incentives to use antibiotics less? Team working dynamics and communication? Availability of diagnostic tests, different types of antibiotics? Influence of residents and their relatives, other healthcare professionals?
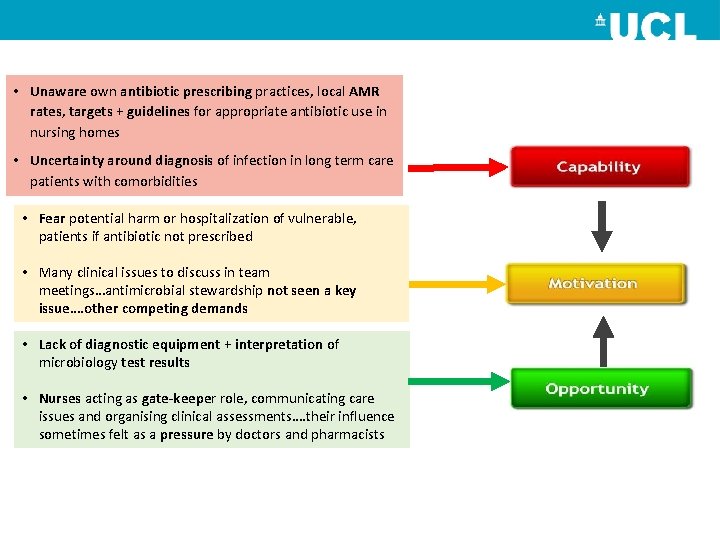
• Unaware own antibiotic prescribing practices, local AMR rates, targets + guidelines for appropriate antibiotic use in nursing homes • Uncertainty around diagnosis of infection in long term care patients with comorbidities • Fear potential harm or hospitalization of vulnerable, patients if antibiotic not prescribed • Many clinical issues to discuss in team meetings…antimicrobial stewardship not seen a key issue…. other competing demands • Lack of diagnostic equipment + interpretation of microbiology test results • Nurses acting as gate-keeper role, communicating care issues and organising clinical assessments…. their influence sometimes felt as a pressure by doctors and pharmacists
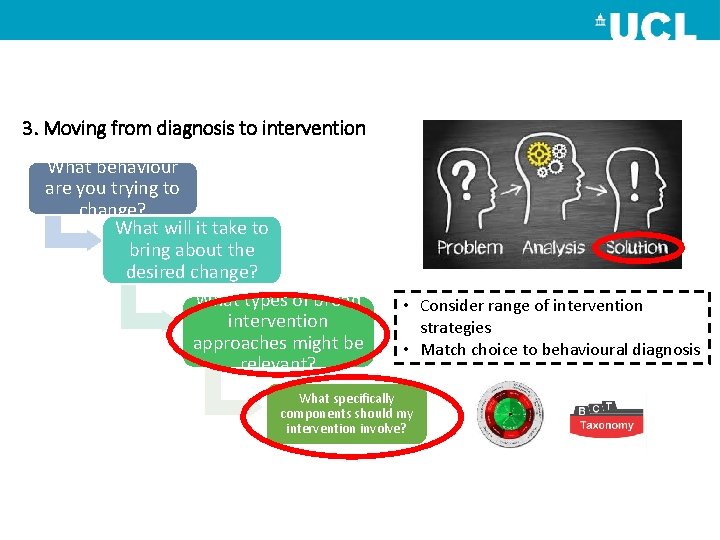
3. Moving from diagnosis to intervention What behaviour are you trying to change? What will it take to bring about the desired change? What types of broad intervention approaches might be relevant? • Consider range of intervention strategies • Match choice to behavioural diagnosis What specifically components should my intervention involve?
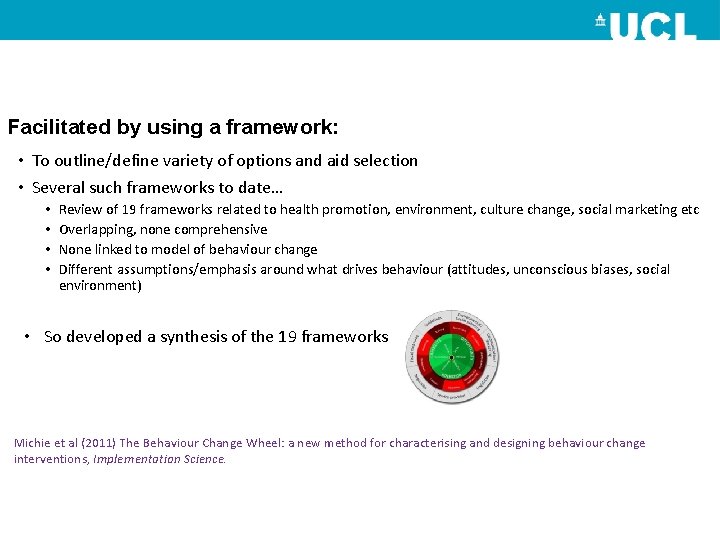
Facilitated by using a framework: • To outline/define variety of options and aid selection • Several such frameworks to date… • • Review of 19 frameworks related to health promotion, environment, culture change, social marketing etc Overlapping, none comprehensive None linked to model of behaviour change Different assumptions/emphasis around what drives behaviour (attitudes, unconscious biases, social environment) • So developed a synthesis of the 19 frameworks Michie et al (2011) The Behaviour Change Wheel: a new method for characterising and designing behaviour change interventions, Implementation Science.
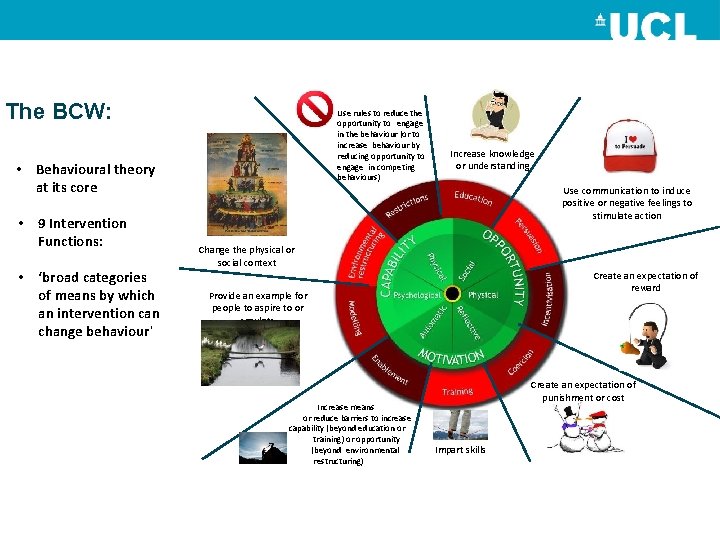
The BCW: Use rules to reduce the opportunity to engage in the behaviour (or to increase behaviour by reducing opportunity to engage in competing behaviours) • Behavioural theory at its core • 9 Intervention Functions: • ‘broad categories of means by which an intervention can change behaviour’ Increase knowledge or understanding Use communication to induce positive or negative feelings to stimulate action Change the physical or social context Create an expectation of reward Provide an example for people to aspire to or emulate Increase means or reduce barriers to increase capability (beyond education or training) or opportunity (beyond environmental restructuring) Create an expectation of punishment or cost Impart skills
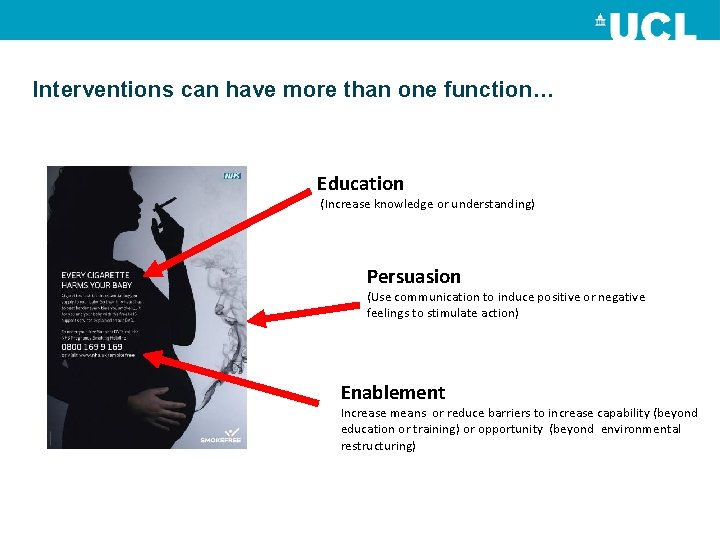
Interventions can have more than one function… Education (Increase knowledge or understanding) Persuasion (Use communication to induce positive or negative feelings to stimulate action) Enablement Increase means or reduce barriers to increase capability (beyond education or training) or opportunity (beyond environmental restructuring)
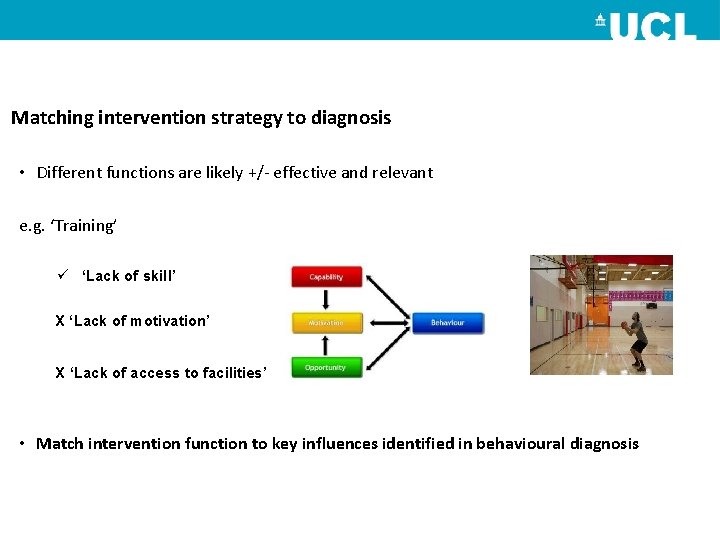
Matching intervention strategy to diagnosis • Different functions are likely +/- effective and relevant e. g. ‘Training’ ü ‘Lack of skill’ X ‘Lack of motivation’ X ‘Lack of access to facilities’ • Match intervention function to key influences identified in behavioural diagnosis
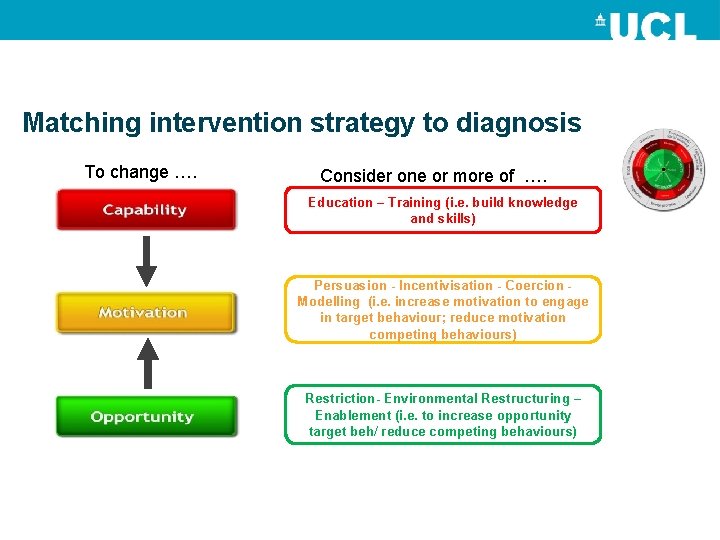
Matching intervention strategy to diagnosis To change …. Consider one or more of …. Education – Training (i. e. build knowledge and skills) Persuasion - Incentivisation - Coercion Modelling (i. e. increase motivation to engage in target behaviour; reduce motivation competing behaviours) Restriction- Environmental Restructuring – Enablement (i. e. to increase opportunity target beh/ reduce competing behaviours)
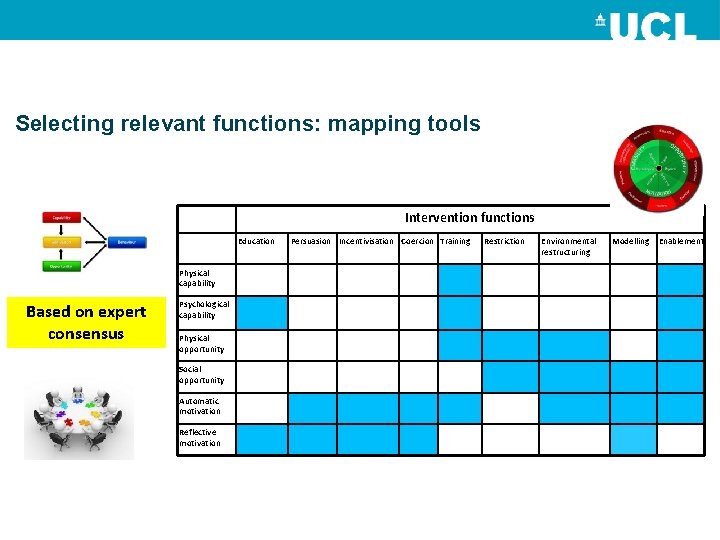
Selecting relevant functions: mapping tools Intervention functions Education Physical capability Based on expert consensus Psychological capability Physical opportunity Social opportunity Automatic motivation Reflective motivation Persuasion Incentivisation Coercion Training Restriction Environmental restructuring Modelling Enablement
But how will you ‘educate, ’ ‘enable, ’ ‘restrict, ’ ‘model…’? • Intervention functions are made up of component Behaviour change techniques (BCTs) • ‘active ingredients’ • E. g. – – – – Goal setting Action planning Self-monitoring rewards (material, social) Feedback on behavior Demonstration of the behavior Verbal persuasion about capability
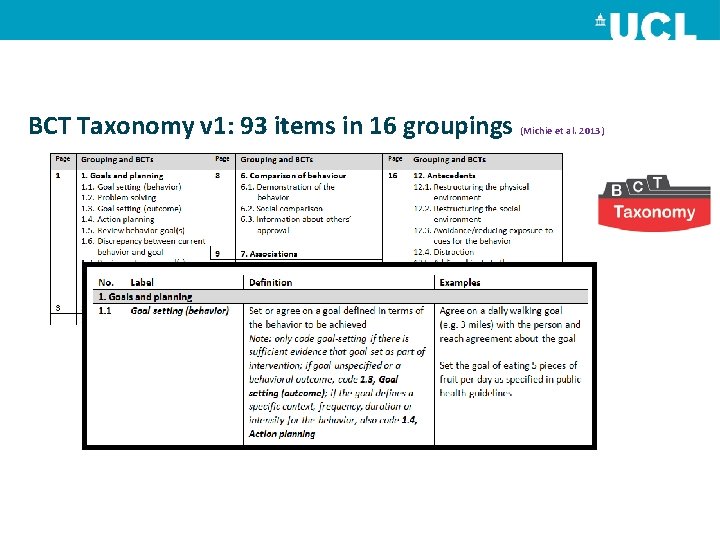
BCT Taxonomy v 1: 93 items in 16 groupings (Michie et al. 2013)
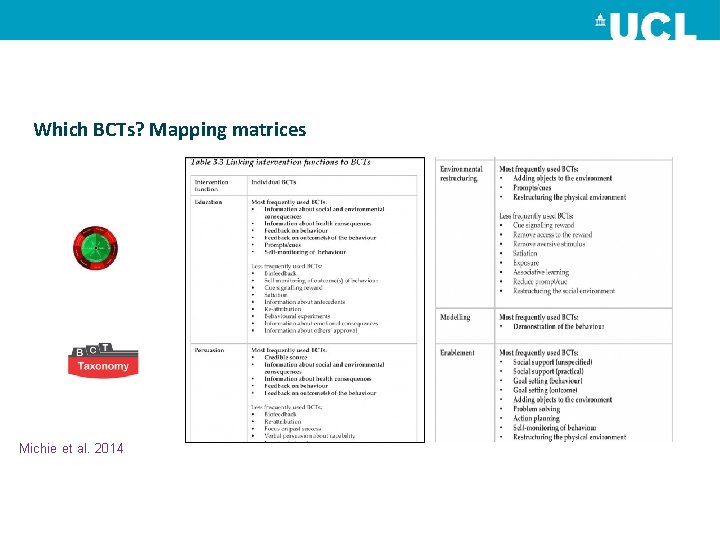
Which BCTs? Mapping matrices Michie et al. 2014
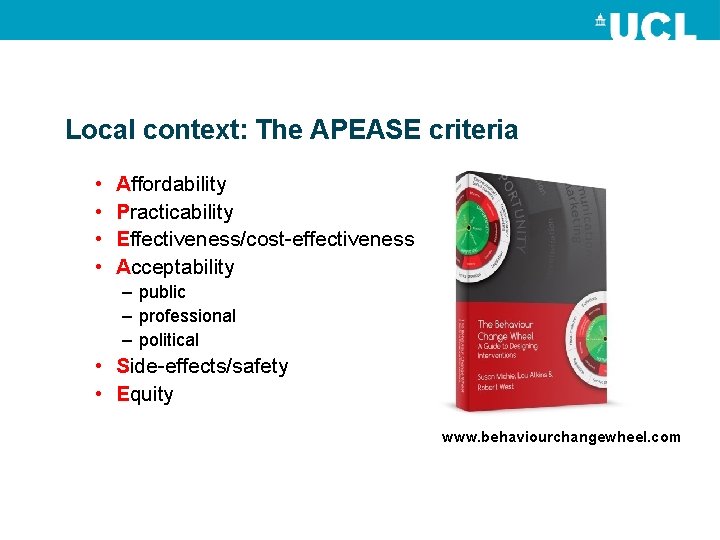
Local context: The APEASE criteria • • Affordability Practicability Effectiveness/cost-effectiveness Acceptability – public – professional – political • Side-effects/safety • Equity www. behaviourchangewheel. com
E. g. Moving from behavioural diagnosis to intervention using BCW • Used findings to recommend intervention strategies for antimicrobial stewardship interventions in LTCFs • Categorised responses in interview according to COM-B • Used mapping tools to identify potential functions and BCTs relevant to addressing barriers/enablers within each COM-B component
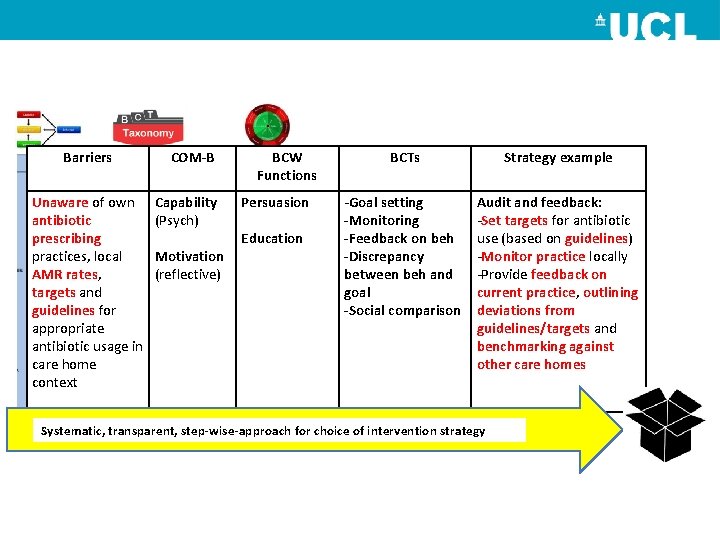
Barriers Unaware of own antibiotic prescribing practices, local AMR rates, targets and guidelines for appropriate antibiotic usage in care home context COM-B Capability (Psych) Motivation (reflective) BCW Functions Persuasion Education BCTs Strategy example -Goal setting -Monitoring -Feedback on beh -Discrepancy between beh and goal -Social comparison Audit and feedback: -Set targets for antibiotic use (based on guidelines) -Monitor practice locally -Provide feedback on current practice, outlining deviations from guidelines/targets and benchmarking against other care homes Systematic, transparent, step-wise-approach for choice of intervention strategy
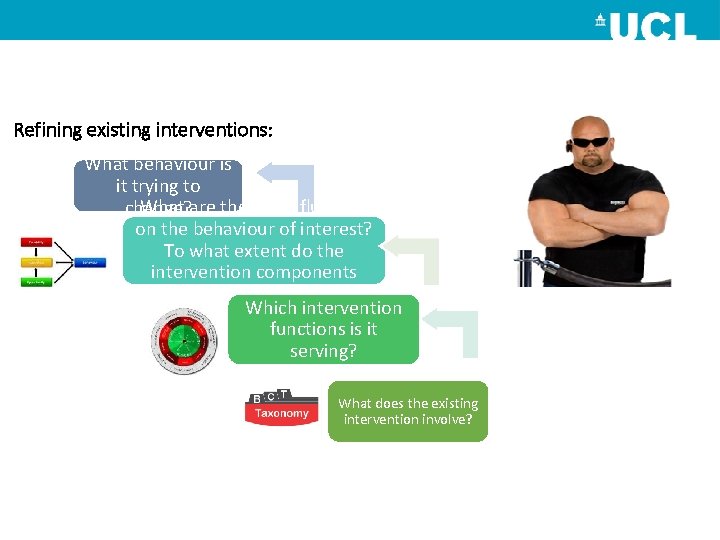
Refining existing interventions: What behaviour is it trying to What are the key influences change? on the behaviour of interest? To what extent do the intervention components target these? Which intervention functions is it serving? What does the existing intervention involve?

e. g.
Summary • Implementation requires behaviour change and systems thinking • No magic bullets • Avoid ISLAGIATT- Need to understand behaviours in context to determine how best to support change • Systematic development of interventions more likely to be effective • Transparency: facilitate evaluation, replication and learning from implementation ‘successes and failures’
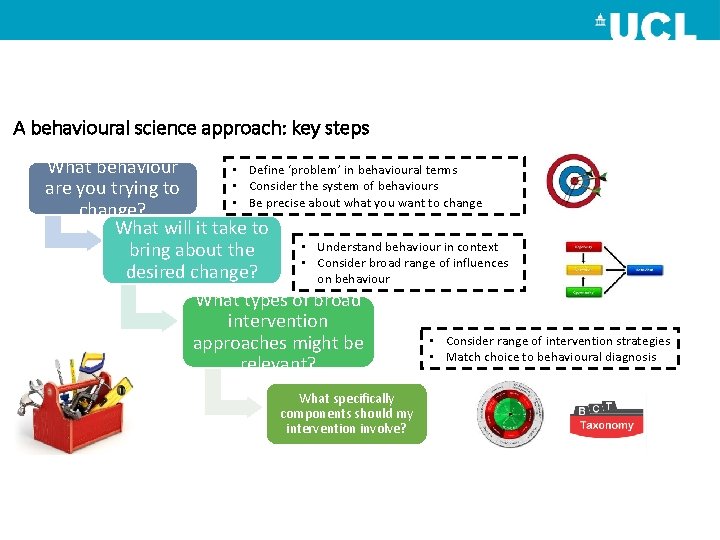
A behavioural science approach: key steps What behaviour • Define ‘problem’ in behavioural terms • Consider the system of behaviours are you trying to • Be precise about what you want to change? What will it take to • Understand behaviour in context bring about the • Consider broad range of influences desired change? on behaviour What types of broad intervention • Consider range of intervention strategies approaches might be • Match choice to behavioural diagnosis relevant? What specifically components should my intervention involve?
Thank you for listening! F. lorencatto@ucl. ac. uk @UCLBehave. Change @Fabilorencatto www. ucl. ac. uk/behaviourchange CBC Summer Schools, London 2018 Summer Schools 23 rd – 27 th July 13 th – 17 th August Advanced Summer School 30 th July- 3 rd August https: //www. ucl. ac. uk/behaviourchange/training/summer-school All proceeds from CBC teaching, training, books and products go to further development
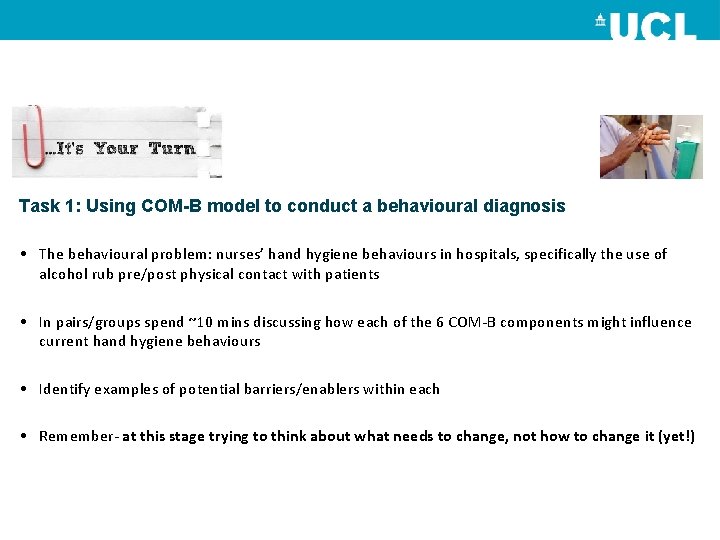
Task 1: Using COM-B model to conduct a behavioural diagnosis • The behavioural problem: nurses’ hand hygiene behaviours in hospitals, specifically the use of alcohol rub pre/post physical contact with patients • In pairs/groups spend ~10 mins discussing how each of the 6 COM-B components might influence current hand hygiene behaviours • Identify examples of potential barriers/enablers within each • Remember- at this stage trying to think about what needs to change, not how to change it (yet!)
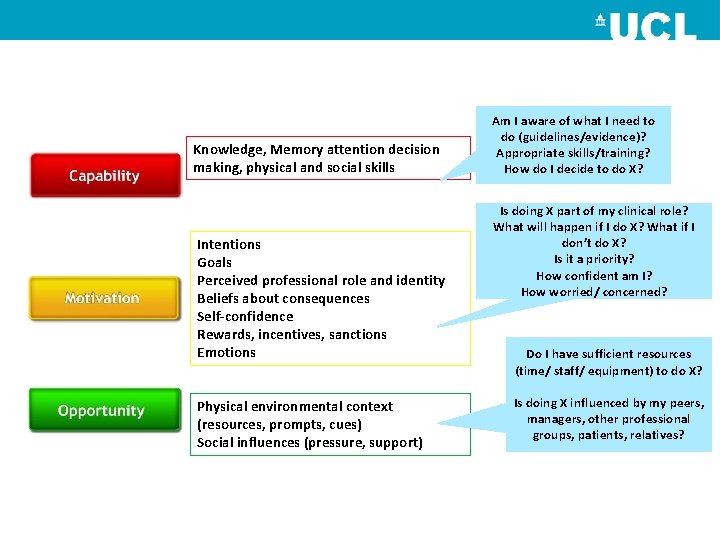
Knowledge, Memory attention decision making, physical and social skills Intentions Goals Perceived professional role and identity Beliefs about consequences Self-confidence Rewards, incentives, sanctions Emotions Physical environmental context (resources, prompts, cues) Social influences (pressure, support) Am I aware of what I need to do (guidelines/evidence)? Appropriate skills/training? How do I decide to do X? Is doing X part of my clinical role? What will happen if I do X? What if I don’t do X? Is it a priority? How confident am I? How worried/ concerned? Do I have sufficient resources (time/ staff/ equipment) to do X? Is doing X influenced by my peers, managers, other professional groups, patients, relatives?
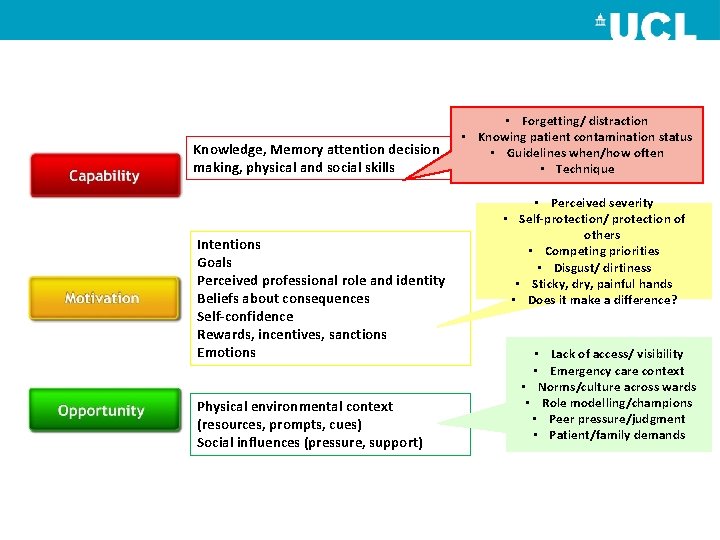
Knowledge, Memory attention decision making, physical and social skills Intentions Goals Perceived professional role and identity Beliefs about consequences Self-confidence Rewards, incentives, sanctions Emotions Physical environmental context (resources, prompts, cues) Social influences (pressure, support) • Forgetting/ distraction • Knowing patient contamination status • Guidelines when/how often • Technique • Perceived severity • Self-protection/ protection of others • Competing priorities • Disgust/ dirtiness • Sticky, dry, painful hands • Does it make a difference? • Lack of access/ visibility • Emergency care context • Norms/culture across wards • Role modelling/champions • Peer pressure/judgment • Patient/family demands
Task 2: Moving from diagnosis to intervention • • Following on from task 1… Select one COM-B component Use matrices mapping COM-B against the BCW function sand BCTs In pairs/groups spend ~10 mins using the APEASE criteria to discuss which functions and techniques might be appropriate to addressing barriers/enablers identified • Discuss how might be delivered in ways that are feasible, relevant, engaging • Feedback to rest of group
Reporting back
- Slides: 55