Applied Pathophysiology A Conceptual Approach Chapter 3 Inflammation
- Slides: 63
Applied Pathophysiology: A Conceptual Approach Chapter 3: Inflammation and Tissue Repair Copyright © 2017 Wolters Kluwer Health | Lippincott Williams & Wilkins
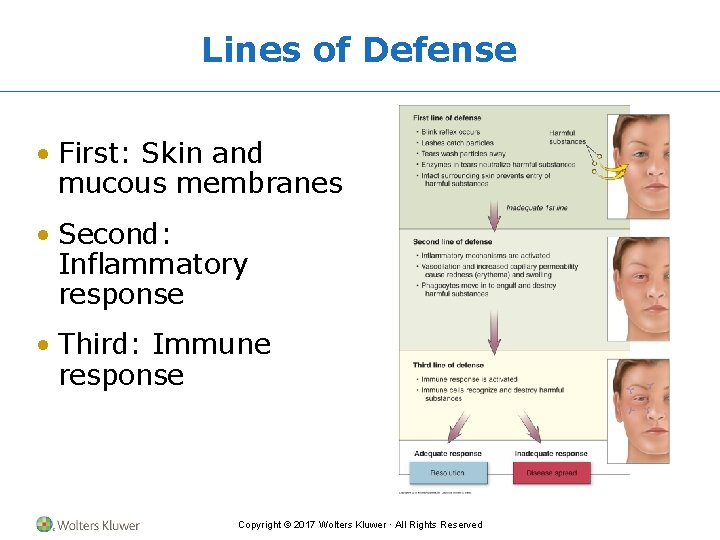
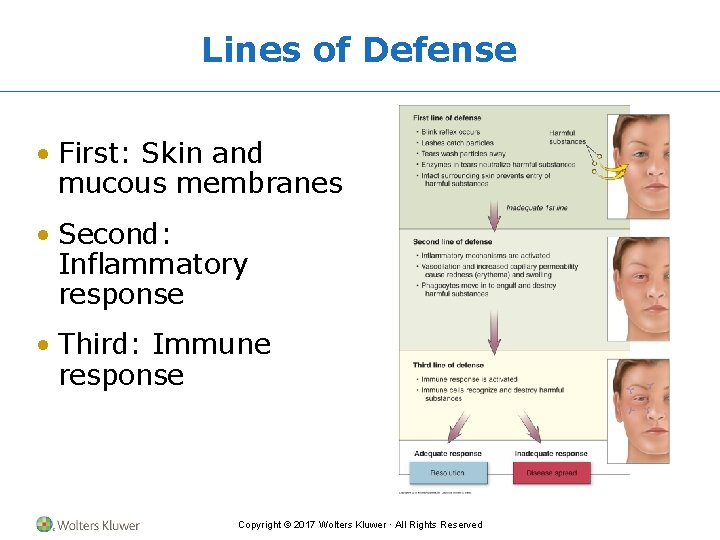
Lines of Defense • First: Skin and mucous membranes • Second: Inflammatory response • Third: Immune response Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Inflammation • Triggered by tissue injury • Goals of inflammation – Increase blood flow to site – Increase healing cells at site – Prepare for tissue repair Copyright © 2017 Wolters Kluwer · All Rights Reserved
Vascular Response • Facilitated by chemical mediators • Induces vasodilation and increases capillary permeability • Objective is to get more blood flowing to the injured area Copyright © 2017 Wolters Kluwer · All Rights Reserved
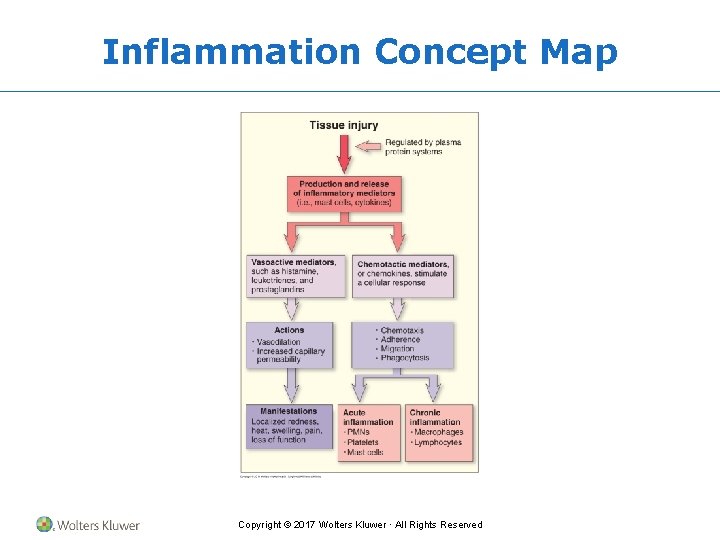
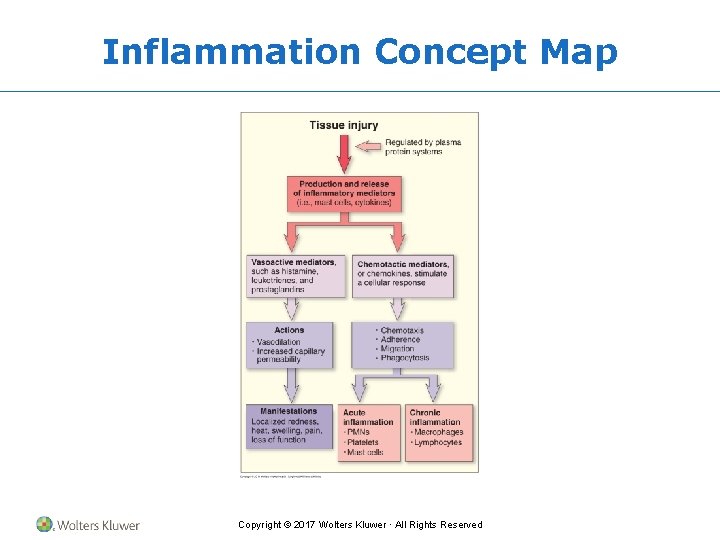
Inflammation Concept Map Copyright © 2017 Wolters Kluwer · All Rights Reserved
Inflammatory Mediators • Cell-derived – White blood cells – Platelets – Endothelial or damaged tissue cells • Plasma-derived – Complement system – Kinin system – Clotting system Copyright © 2017 Wolters Kluwer · All Rights Reserved
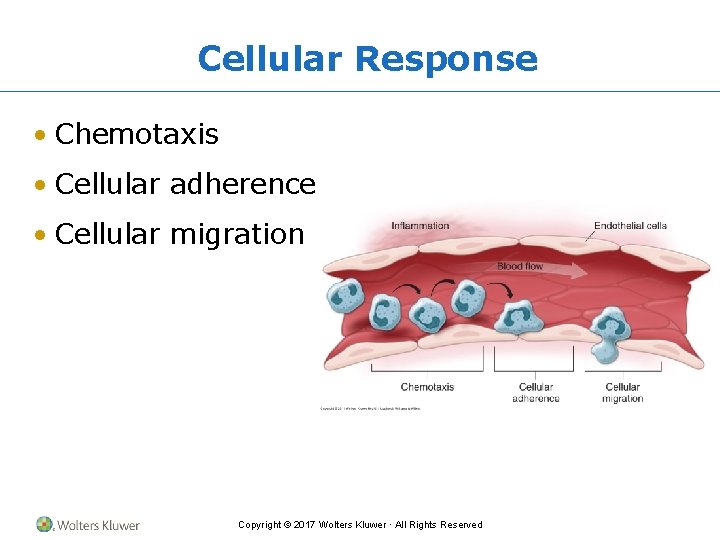
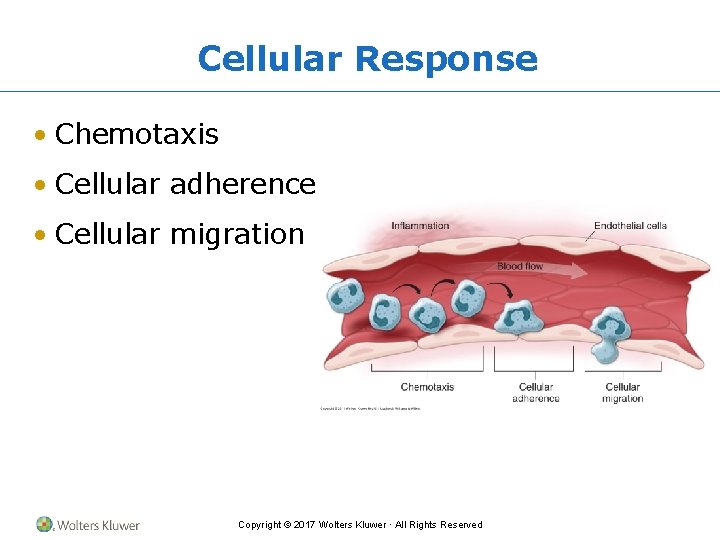
Cellular Response • Chemotaxis • Cellular adherence • Cellular migration Copyright © 2017 Wolters Kluwer · All Rights Reserved
Manifestations of Inflammation • Local manifestations include heat, incapacitation, pain, edema, redness • Systemic manifestations may include fever and increased circulating leukocytes and plasma proteins Copyright © 2017 Wolters Kluwer · All Rights Reserved
Treatment of Inflammation • Reduce blood flow • Decrease swelling • Block the action of chemical mediators • Decrease pain Copyright © 2017 Wolters Kluwer · All Rights Reserved
Healing and Tissue Repair • Inflammatory phase • Remodeling phase – Acute inflammatory response – Restore functional integrity – Seal the wound – Remodeling • Proliferative phase – Clear the debris – Restore structural integrity Copyright © 2017 Wolters Kluwer · All Rights Reserved
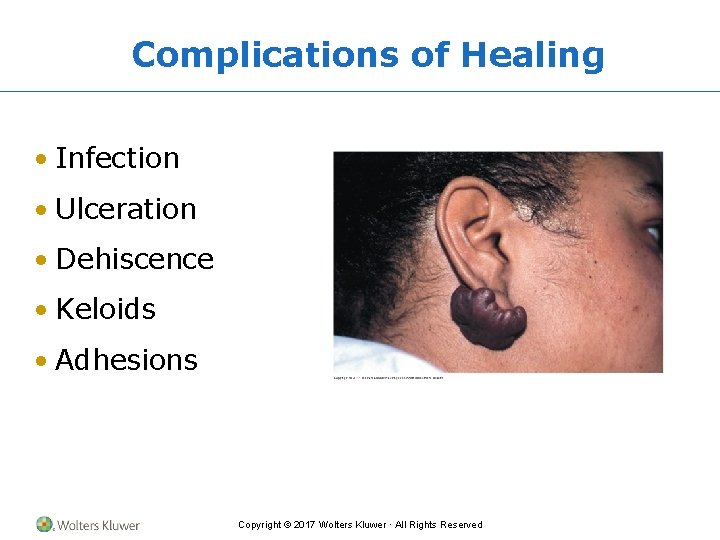
Complications of Healing • Infection • Ulceration • Dehiscence • Keloids • Adhesions Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Inflammation • Recurrent or persistent inflammation lasting several weeks or longer • Monocytes, macrophages, and lymphocytes more prominently involved • Formation of granulomas and scarring often occur Copyright © 2017 Wolters Kluwer · All Rights Reserved
Application of the Concepts of Inflammation • Sinusitis • Burns • Rheumatoid arthritis (RA) • Gastritis • Pancreatitis • Inflammatory bowel disease (IBS) Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute and Chronic Sinusitis • Pathophysiology • Clinical manifestations • Diagnostic criteria • Treatment Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Sinusitis Pathophysiology • Blockage of ostia and outflow of mucus due to allergy, viruses, or other irritants • Impaired clearance of mucus by cilia • Altered mucus quality or quantity • Cystic fibrosis Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Sinusitis Clinical Manifestations • Facial pain over sinus regions of face increasing with straining or bending down • Fever • Nasal congestion and/or excessive nasal discharge and postnasal drainage • Persistent cough • Fatigue Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Sinusitis Diagnostic Criteria • Physical examination • General laboratory tests – Erythrocyte sedimentation rate (ESR) – C-reactive protein (CRP) test – White blood cell (WBC) count • Sinus radiographs Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Sinusitis Treatment • Pharmacologic – Antibiotics – Antihistamines – Decongestants – Nasal sprays • Surgical Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Sinusitis Pathophysiology • Multifactorial – Environmental factors • Persistent infection • Allergens – Genetic factors • Metabolic abnormalities • Immune deficiencies • Disruption of mucociliary clearance Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Sinusitis Clinical Manifestations • Nasal congestion • Fatigue, anorexia • Nasal and postnasal discharge • Chronic cough • Sore throat • Foul breath, unpleasant taste • Low-grade fever • Hyposmia (reduced ability to smell) • Facial fullness, discomfort, pain, and headache (with polyps) Copyright © 2017 Wolters Kluwer · All Rights Reserved
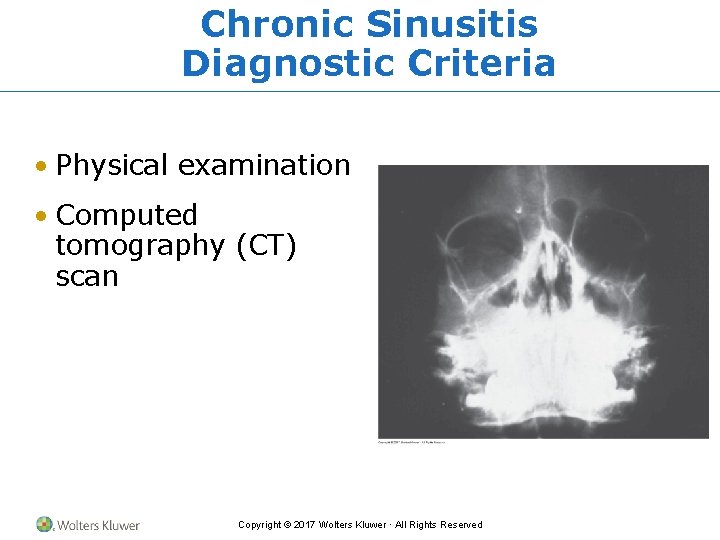
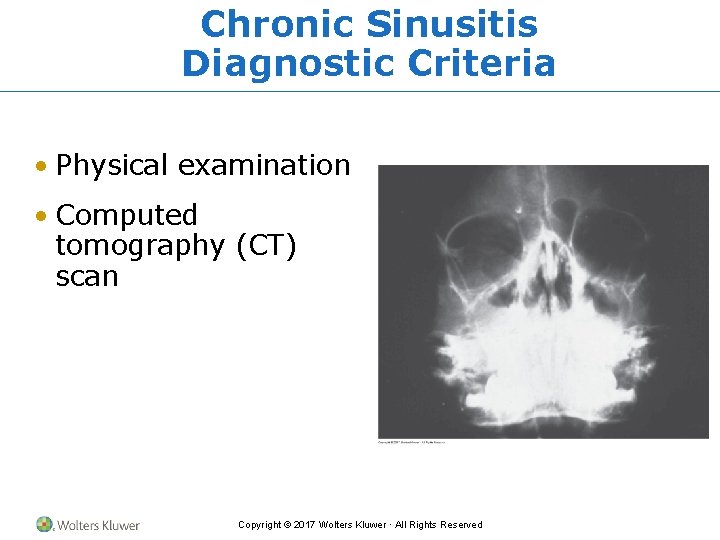
Chronic Sinusitis Diagnostic Criteria • Physical examination • Computed tomography (CT) scan Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Sinusitis Treatment • Pharmacologic – Glucocorticoids – Antibiotics • Nonpharmacologic – Nasal saline irrigation • Surgical Copyright © 2017 Wolters Kluwer · All Rights Reserved
Burns • Pathophysiology • Clinical manifestations • Diagnostic criteria • Treatment Copyright © 2017 Wolters Kluwer · All Rights Reserved
Burns Pathophysiology • Cause: direct contact with excessive heat or radiation, caustic chemicals, or electricity • Result: acute inflammatory response • Burn severity is correlated with exposure type and time Copyright © 2017 Wolters Kluwer · All Rights Reserved
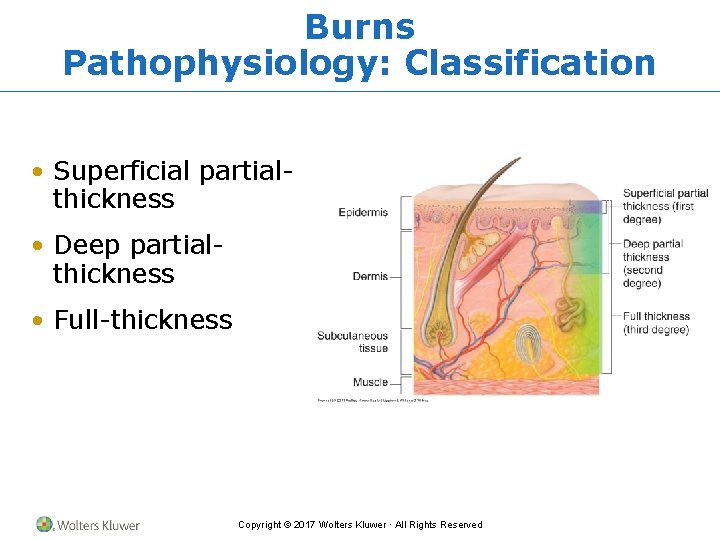
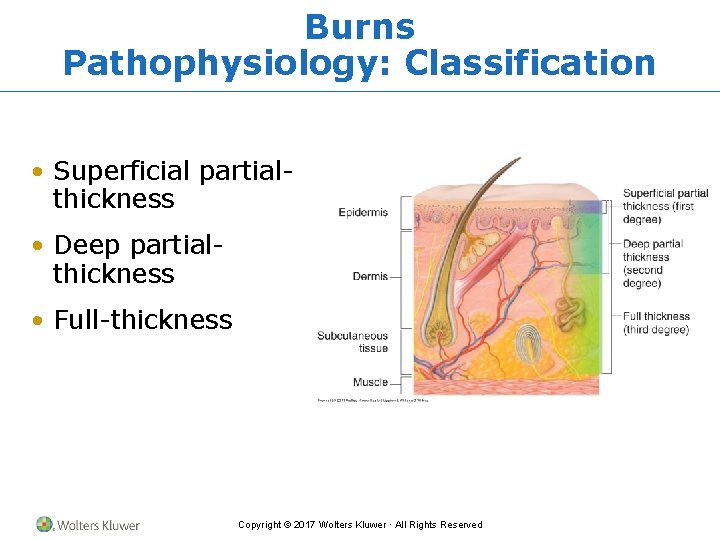
Burns Pathophysiology: Classification • Superficial partialthickness • Deep partialthickness • Full-thickness Copyright © 2017 Wolters Kluwer · All Rights Reserved
Burns Clinical Manifestations • Superficial partial-thickness burns – Heat, swelling, pain, redness, loss of function • Deep partial-thickness burns – Blistering, redness, heat, pain, edema, serous exudate • Full-thickness burns – Redness, eschar, edema, exudate Copyright © 2017 Wolters Kluwer · All Rights Reserved
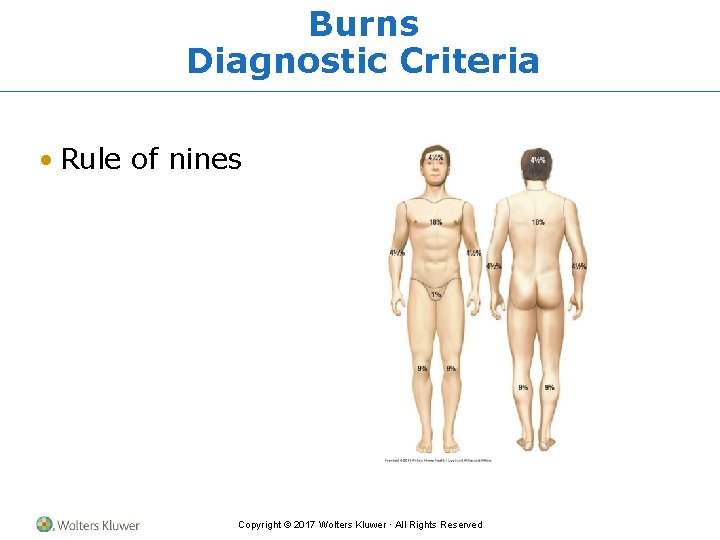
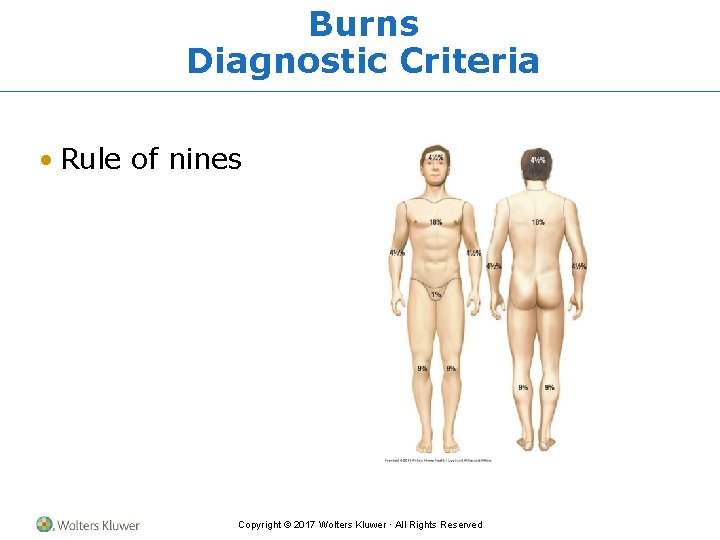
Burns Diagnostic Criteria • Rule of nines Copyright © 2017 Wolters Kluwer · All Rights Reserved
Burns Diagnostic Criteria (cont’d) • American Burn Association has designated criteria for distinguishing minor, moderate, and major burns based on – Wound depth – Surface area – Required level of treatment Copyright © 2017 Wolters Kluwer · All Rights Reserved
Burns Treatment • American Burn Association criteria • Remove source of injury and cool/rinse skin • Airway, breathing, circulation • Fluids, nutrition, antibiotics, analgesics • Wound management may include – Hydrotherapy – Skin grafting Copyright © 2017 Wolters Kluwer · All Rights Reserved
Rheumatoid Arthritis (RA) • Pathophysiology • Clinical manifestations • Diagnostic criteria • Treatment Copyright © 2017 Wolters Kluwer · All Rights Reserved
RA Pathophysiology • Chronic inflammation of synovial membranes and synovial hyperplasia • Etiology combines – Genetics – Triggering event – Autoimmunity Copyright © 2017 Wolters Kluwer · All Rights Reserved
RA Pathophysiology (cont’d) • Remissions and exacerbations • Pannus formation • Cartilage erosion • Fibrosis • Ankylosis Copyright © 2017 Wolters Kluwer · All Rights Reserved
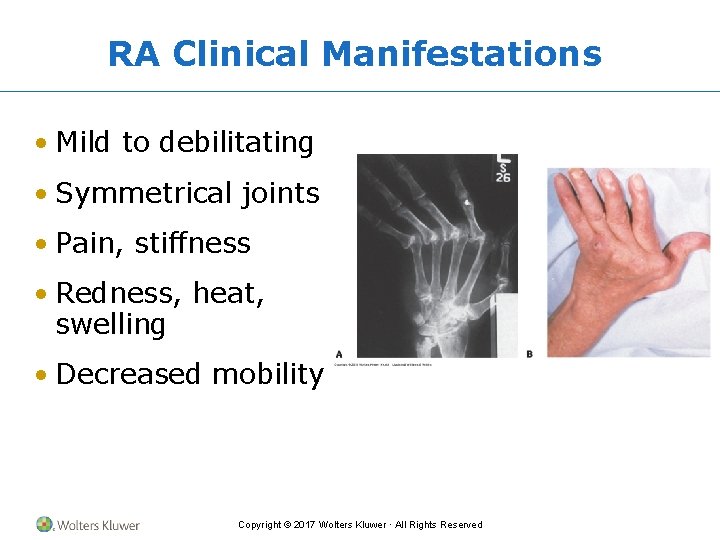
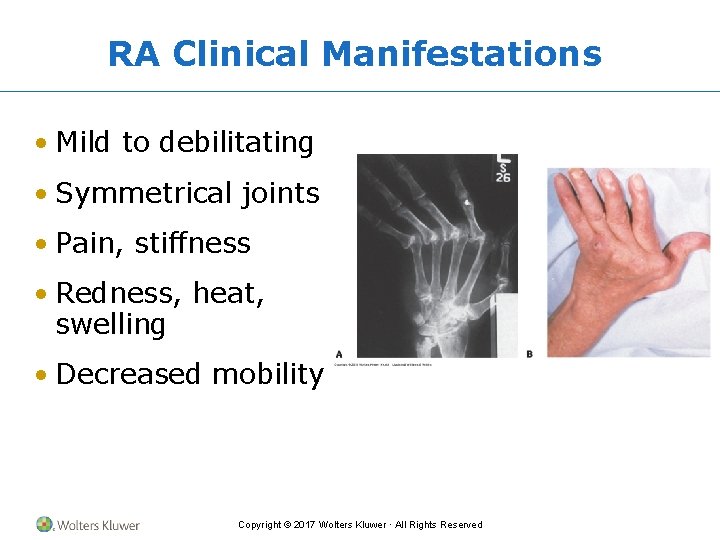
RA Clinical Manifestations • Mild to debilitating • Symmetrical joints • Pain, stiffness • Redness, heat, swelling • Decreased mobility Copyright © 2017 Wolters Kluwer · All Rights Reserved
RA Diagnostic Criteria • No definitive test • Increased likelihood with positive findings – Erythrocyte sedimentation rate (ESR) – C-reactive protein (CRP) – Rheumatoid factor (Ig. G) – Antinuclear antibodies (ANA) Copyright © 2017 Wolters Kluwer · All Rights Reserved
RA Treatment • Pharmacologic: drugs that induce remission • Nonpharmacologic: – Rest/activity balance – Physical therapy exercises – Splints – Surgery Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute and Chronic Gastritis • Pathophysiology • Clinical manifestations • Diagnostic criteria • Treatment Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Gastritis Pathophysiology • Ingestion of irritating substances and/or poor gastric perfusion results in acute inflammation of the gastric mucosa • Gastric epithelial cell necrosis • Gastric acid erodes underlying tissue Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Gastritis Clinical Manifestations • Mild to severe abdominal pain • Indigestion • Loss of appetite • Nausea • Vomiting • Hiccups Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Gastritis Diagnostic Criteria • History and physical examination • Endoscopic examination • Stool analysis (presence of blood in stool) • Complete blood count (anemia) Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Gastritis Treatment • Discontinue ingestion of irritating substance • Buffer or decrease production of gastric acid Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Gastritis Pathophysiology • Chronic infection or autoimmune process leading to chronic inflammation – Infection with Helicobacter pylori bacterium • Gastric epithelial and mucosal cell atrophy • Gastric acid production impaired Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Gastritis Clinical Manifestations • Dyspepsia • Loss of appetite • Vomiting • Anemia • Can be asymptomatic Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Gastritis Diagnostic Criteria • Endoscopic examination • Biopsy of gastric tissue • Breath test • Blood test (protein antibodies) Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Gastritis Treatment • Antibiotics for chronic infectious processes • Proton pump inhibitors or bismuth (antimicrobial and raise gastric p. H) • Immunosuppressive drugs for autoimmune processes • Vitamin B 12 Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute and Chronic Pancreatitis • Pathophysiology • Clinical manifestations • Diagnostic criteria • Treatment Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Pancreatitis Pathophysiology • Injury to • Caused by – Acinar cells – Duct blockage by gallstones – Zymogen – Pancreatic duct – Excessive alcohol use – Protective digestive feedback mechanisms Copyright © 2017 Wolters Kluwer · All Rights Reserved
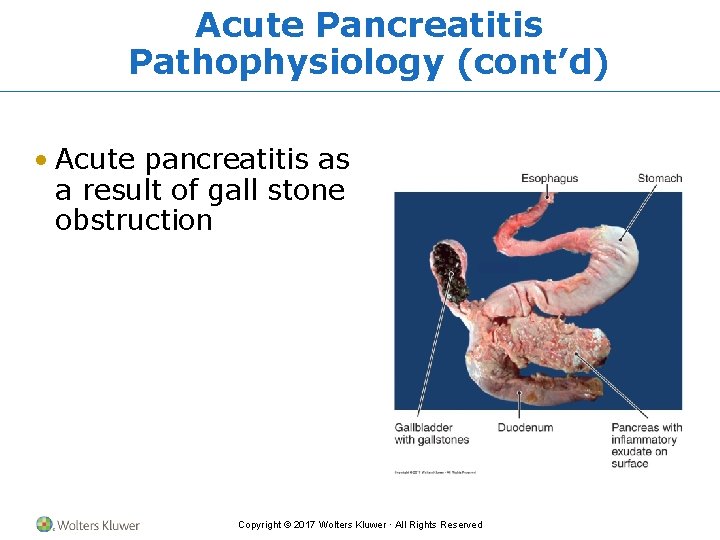
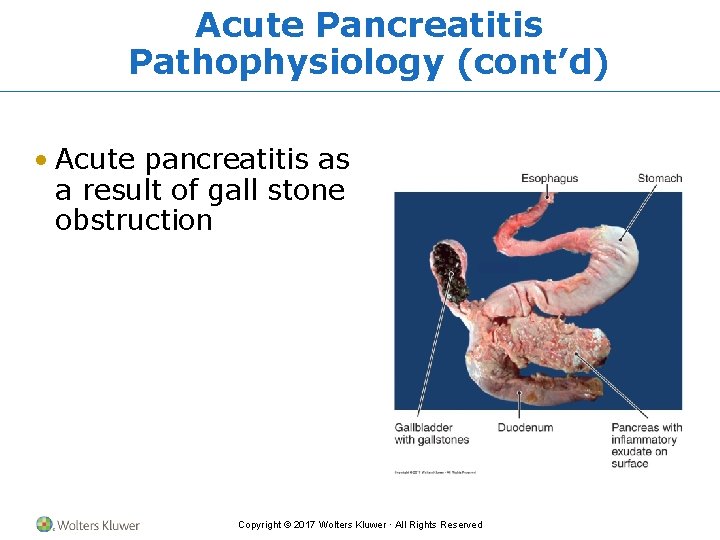
Acute Pancreatitis Pathophysiology (cont’d) • Acute pancreatitis as a result of gall stone obstruction Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Pancreatitis Clinical Manifestations • Upper abdominal pain – Sudden onset – Growing intensity – Dull, steady ache • Nausea • Vomiting • Anorexia • Diarrhea – Radiating to back Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Pancreatitis Diagnostic Criteria • History and physical examination • Laboratory testing – Complete blood count, ESR, CRP – Serum amylase and lipase – Serum alkaline phosphatase – Total bilirubin – Aspartate aminotransferase (AST) – Alanine aminotransferase (ALT) Copyright © 2017 Wolters Kluwer · All Rights Reserved
Acute Pancreatitis Treatment • Intravenous hydration • Analgesics • Surgical removal of gallstones Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Pancreatitis Pathophysiology • Excessive alcohol use • Duct obstruction by enzymes and proteins • Ischemia • Acinar cells become atrophic and fibrotic • Loss of function • Oxidation: cellular injury and organ damage • Autoimmunity Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Pancreatitis Clinical Manifestations • Abdominal pain – Severe, intermittent – Mid or upper right-sided, radiating to back – Lasting several hours at unpredictable intervals • Diarrhea • Steatorrhea (fatty stools) • Weight loss Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Pancreatitis Diagnostic Criteria • Endoscopic retrograde cholangiopancreatography (ERCP) • Serum amylase and lipase levels • Direct aspiration of pancreatic duct or duodenum Copyright © 2017 Wolters Kluwer · All Rights Reserved
Chronic Pancreatitis Treatment • Pain management • Behavior modification – Alcohol cessation – Smoking cessation – Exercise – Nutrition • Surgery Copyright © 2017 Wolters Kluwer · All Rights Reserved
Inflammatory Bowel Diseases: Crohn Disease and Ulcerative Colitis • Pathophysiology • Clinical manifestations • Diagnostic criteria • Treatment Copyright © 2017 Wolters Kluwer · All Rights Reserved
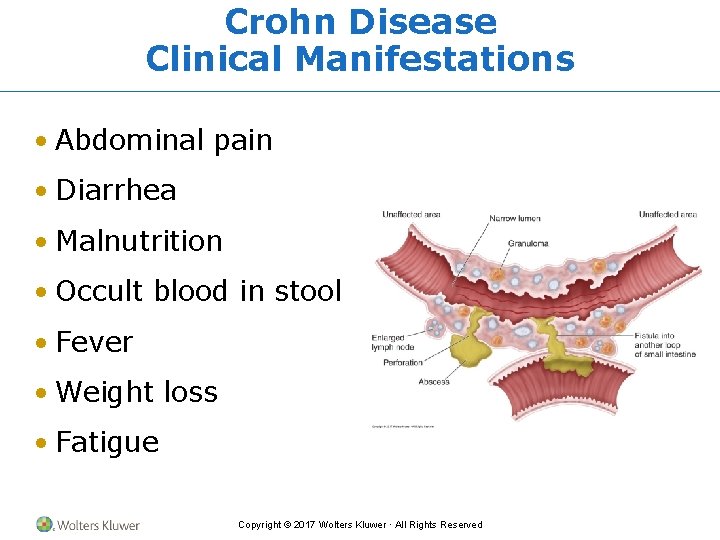
Crohn Disease Pathophysiology • Chronic inflammation anywhere throughout the GI tract but most commonly in small intestine • Noncontinuous penetrating ulcerations and fibrosis • Impaired intestinal absorption and bowel obstruction can result Copyright © 2017 Wolters Kluwer · All Rights Reserved
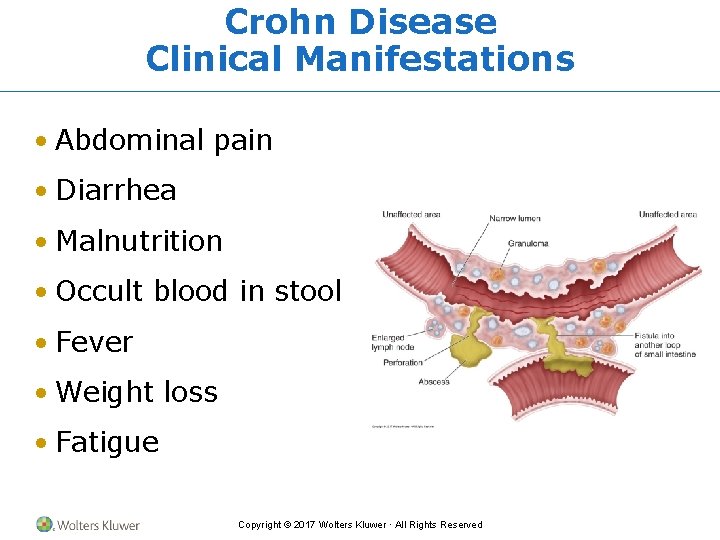
Crohn Disease Clinical Manifestations • Abdominal pain • Diarrhea • Malnutrition • Occult blood in stool • Fever • Weight loss • Fatigue Copyright © 2017 Wolters Kluwer · All Rights Reserved
Crohn Disease Diagnostic Criteria • History and physical examination • Endoscopic examination • Radiographs • Computed tomography scans • Stool cultures Copyright © 2017 Wolters Kluwer · All Rights Reserved
Crohn Disease Treatment • Symptom management • Pharmacologic treatment • Dietary changes • Surgical treatment Copyright © 2017 Wolters Kluwer · All Rights Reserved
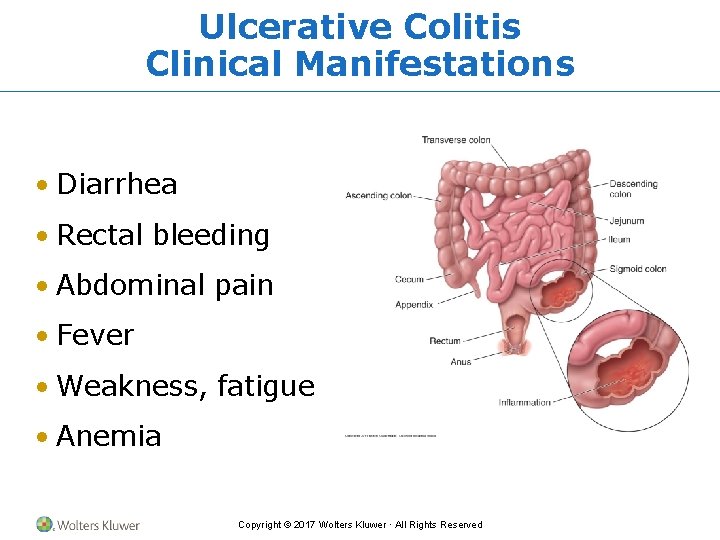
Ulcerative Colitis Pathophysiology • Chronic inflammation begins in rectum and ascends the descending colon • Continuous superficial areas of ulceration • Perforation, obstruction, and massive hemorrhage can result Copyright © 2017 Wolters Kluwer · All Rights Reserved
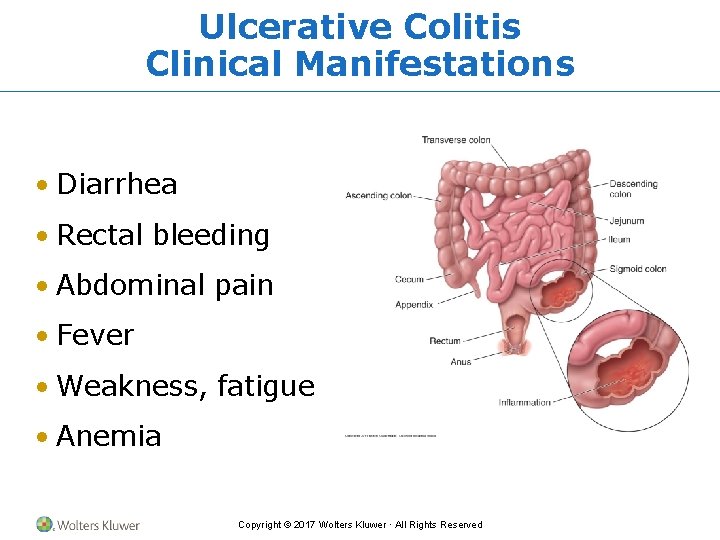
Ulcerative Colitis Clinical Manifestations • Diarrhea • Rectal bleeding • Abdominal pain • Fever • Weakness, fatigue • Anemia Copyright © 2017 Wolters Kluwer · All Rights Reserved
Ulcerative Colitis Diagnostic Criteria • History and physical examination • Endoscopic examination • Radiographs • Complete blood count (anemia) Copyright © 2017 Wolters Kluwer · All Rights Reserved
Ulcerative Colitis Treatment • Symptom management • Pharmacologic treatment • Dietary changes • Surgical treatment Copyright © 2017 Wolters Kluwer · All Rights Reserved