APLASTIC ANEMIA Dr Ramadas Nayak Professor HOD Pathology
- Slides: 21
APLASTIC ANEMIA Dr. Ramadas Nayak Professor & HOD Pathology Yenepoya Medical college Mangalore
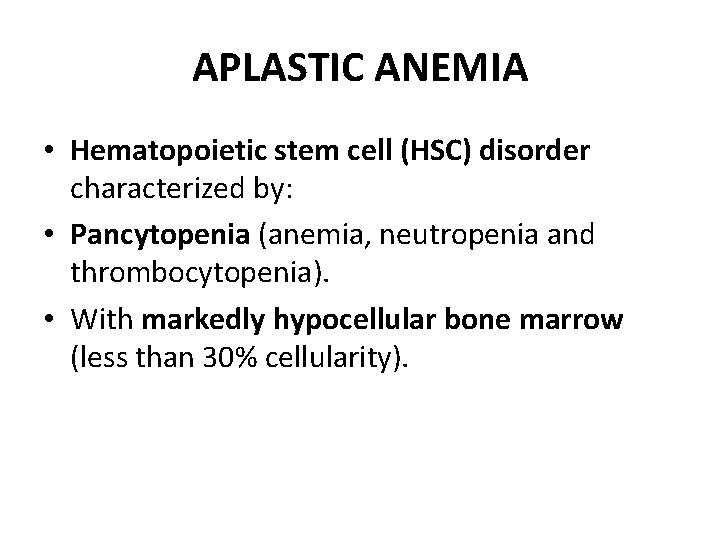
APLASTIC ANEMIA • Hematopoietic stem cell (HSC) disorder characterized by: • Pancytopenia (anemia, neutropenia and thrombocytopenia). • With markedly hypocellular bone marrow (less than 30% cellularity).
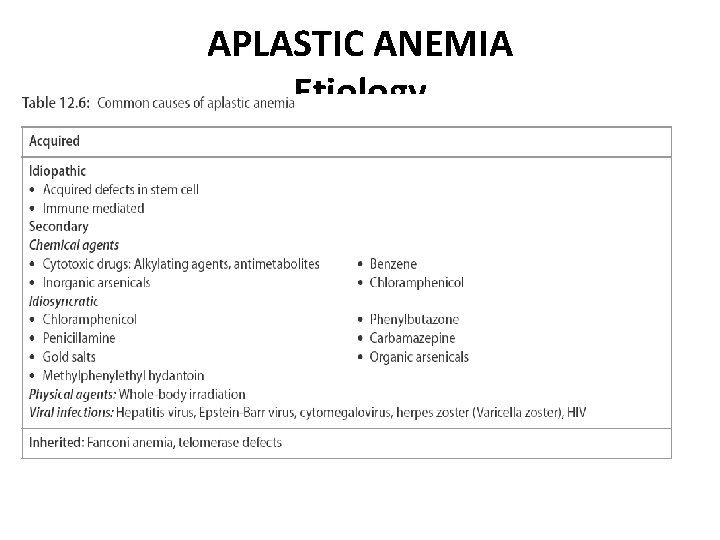
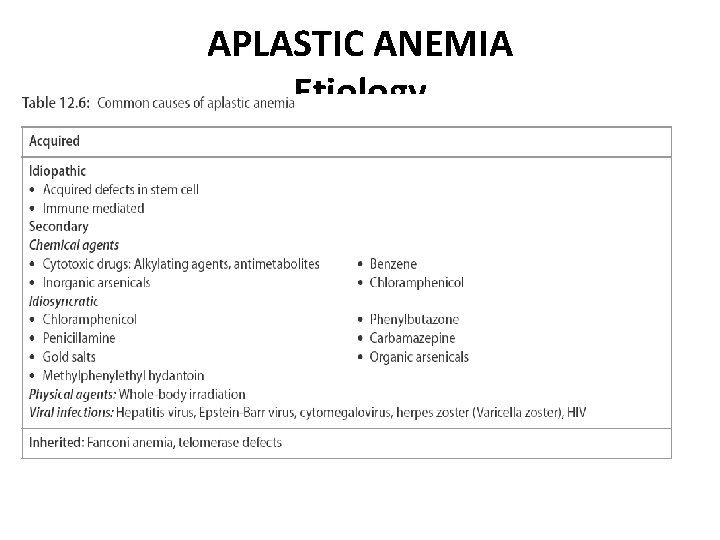
APLASTIC ANEMIA Etiology
APLASTIC ANEMIA Clinical Features Any age of both sexes Insidious Progressive weakness, pallor and dyspnea due to anemia. • Frequent (mucocutaneous bacterial infections) or fatal infections due to neutropenia. • Bleeding manifestations in the form of petechiae, bruises and ecchymoses due to thrombocytopenia. • •
APLASTIC ANEMIA • • • Laboratory Findings Peripheral Blood Hemoglobin : Reduced PCV: Reduced Reticulocyte count: Markedly decreased.
APLASTIC ANEMIA • Peripheral smear: Pancytopenia, i. e. decreased red cells, neutrophils and platelets. • RBCs: Normocytic normochromic anemia– • WBCs: Total leukocyte count decreased. Neutrophils markedly diminished and neutropenia is a reflection of the severity of aplasia. • Initial stages, lymphocytes normal in number as the disease progresses their count decreases. • Platelets: Count is decreased.
Bone Marrow in aplastic anemia • Marrow aplasia—best appreciated in a bone marrow (trephine) biopsy • Cellularity: Marked hypocellularity. • Hematopoiesis: Paucity of all erythroid, myeloid and megakaryocytic precursors. – • Other cells: Lymphocytes and plasma cells are prominent.
• No Splenomegaly • Diagnosis: Diagnosis is made with peripheral blood and bone marrow biopsy findings. • Prognosis: Unpredictable.
HEMOLYTIC ANEMIA • Definition • Hemolytic anemias are due to increase in the rate of red cell destruction (hemolysis).
HEREDITARY SPHEROCYTOSIS • Hereditary spherocytosis (HS) is a rare inherited hemolytic anemia resulting from the defect in the red cell membrane.
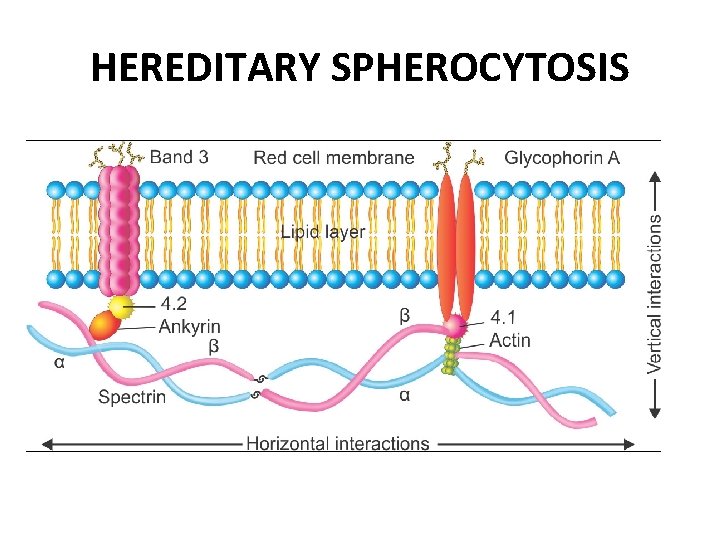
HEREDITARY SPHEROCYTOSIS • Etiopathogenesis • Autosomal dominant disorder • RBC membrane protein defect caused by various mutations. Most common mutations involve ankyrin, band 3, spectrin, or band protein 4. 2.
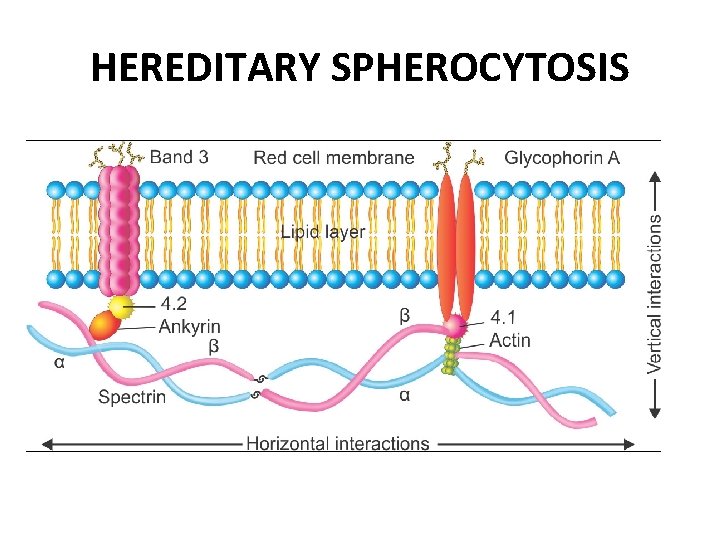
HEREDITARY SPHEROCYTOSIS
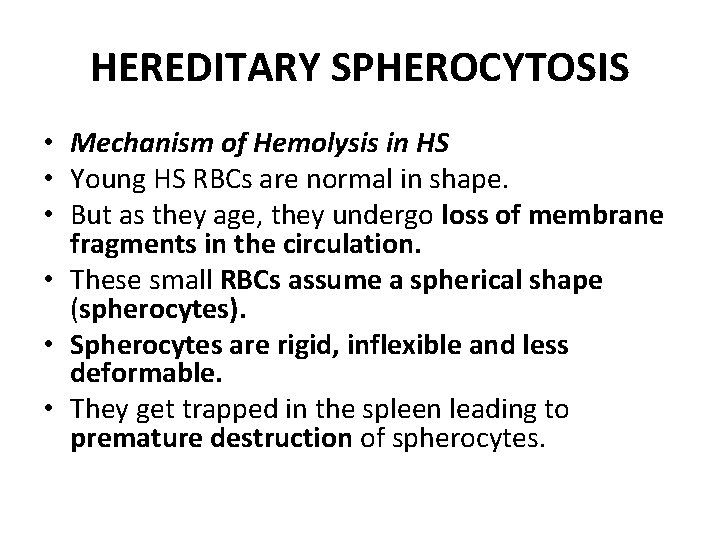
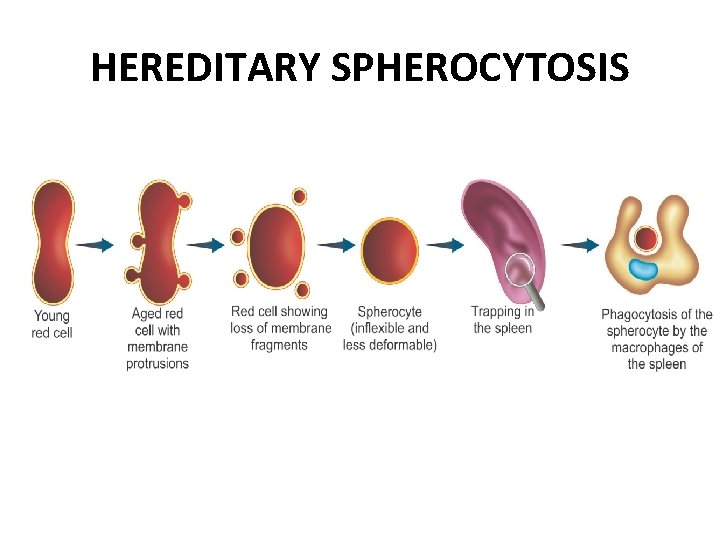
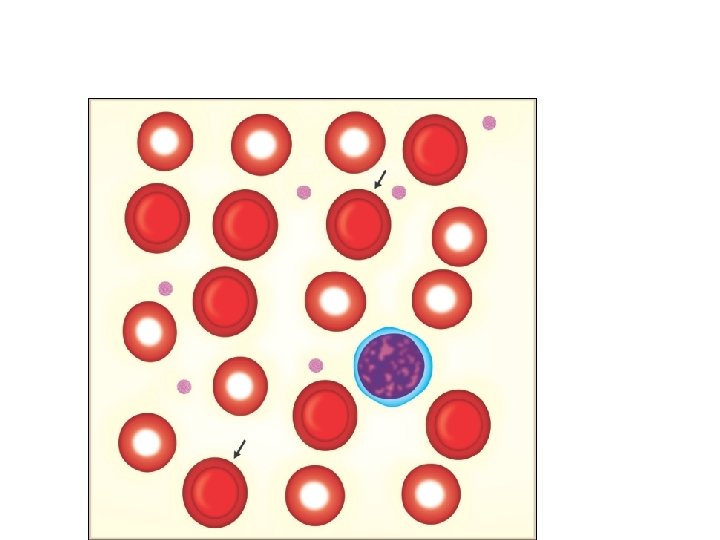
HEREDITARY SPHEROCYTOSIS • Mechanism of Hemolysis in HS • Young HS RBCs are normal in shape. • But as they age, they undergo loss of membrane fragments in the circulation. • These small RBCs assume a spherical shape (spherocytes). • Spherocytes are rigid, inflexible and less deformable. • They get trapped in the spleen leading to premature destruction of spherocytes.
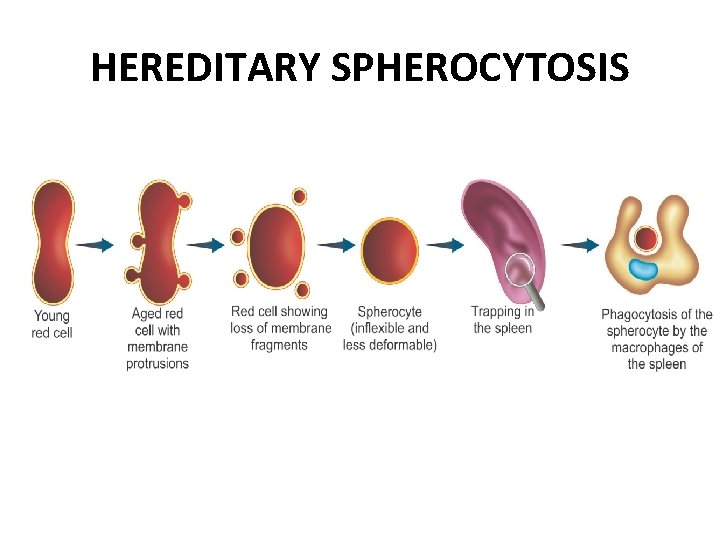
HEREDITARY SPHEROCYTOSIS
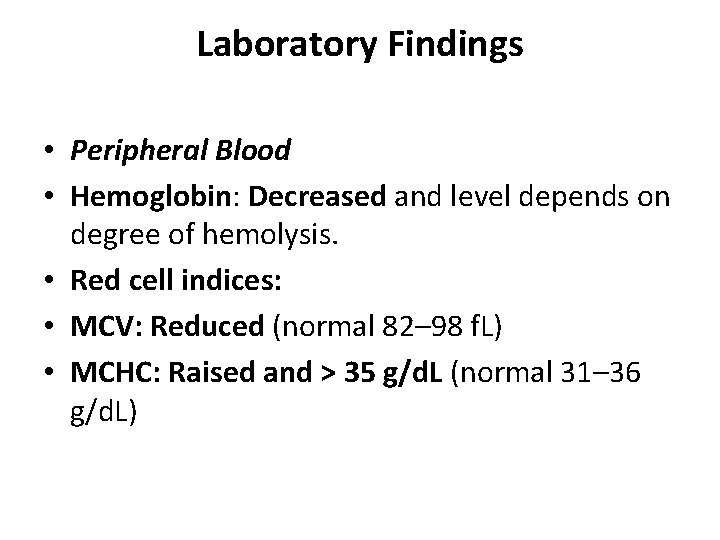
Laboratory Findings • Peripheral Blood • Hemoglobin: Decreased and level depends on degree of hemolysis. • Red cell indices: • MCV: Reduced (normal 82– 98 f. L) • MCHC: Raised and > 35 g/d. L (normal 31– 36 g/d. L)
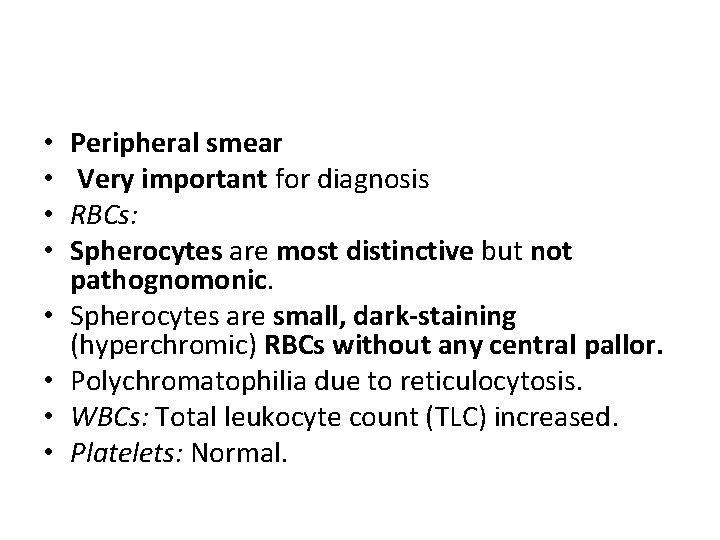
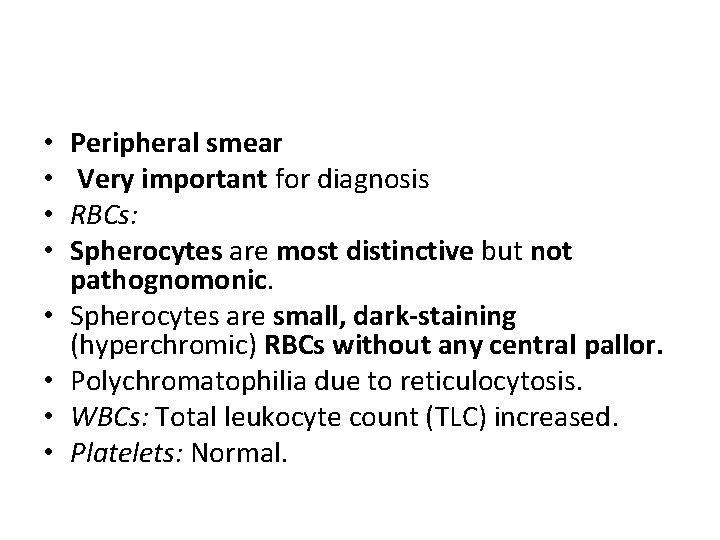
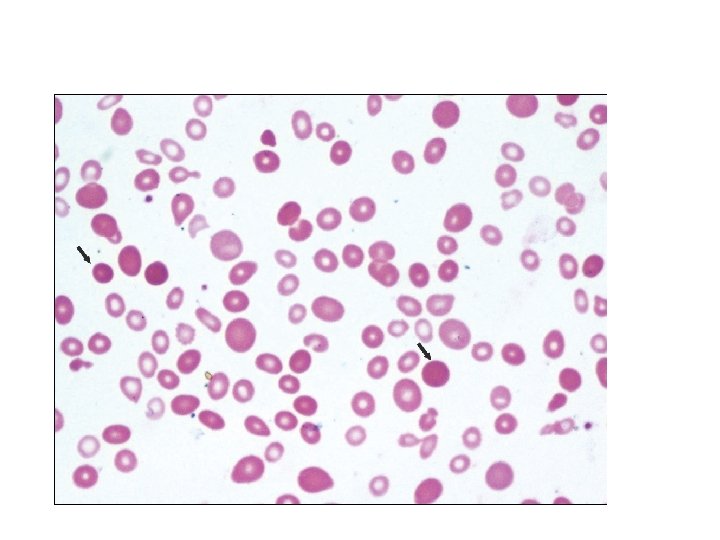
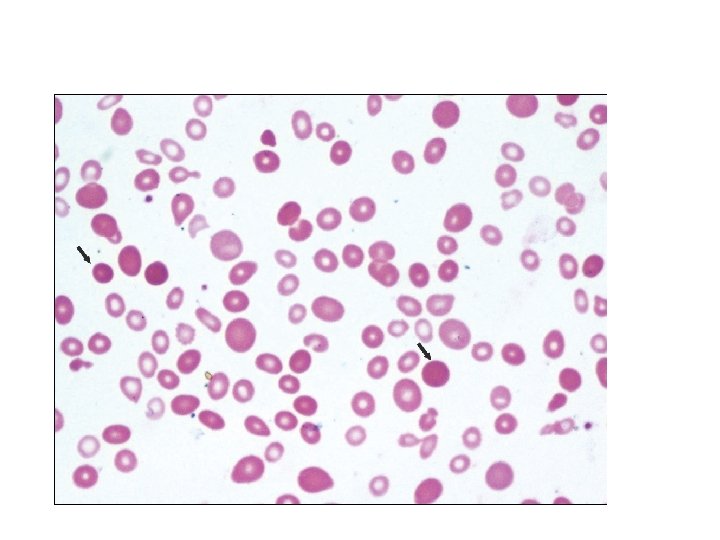
• • Peripheral smear Very important for diagnosis RBCs: Spherocytes are most distinctive but not pathognomonic. Spherocytes are small, dark-staining (hyperchromic) RBCs without any central pallor. Polychromatophilia due to reticulocytosis. WBCs: Total leukocyte count (TLC) increased. Platelets: Normal.
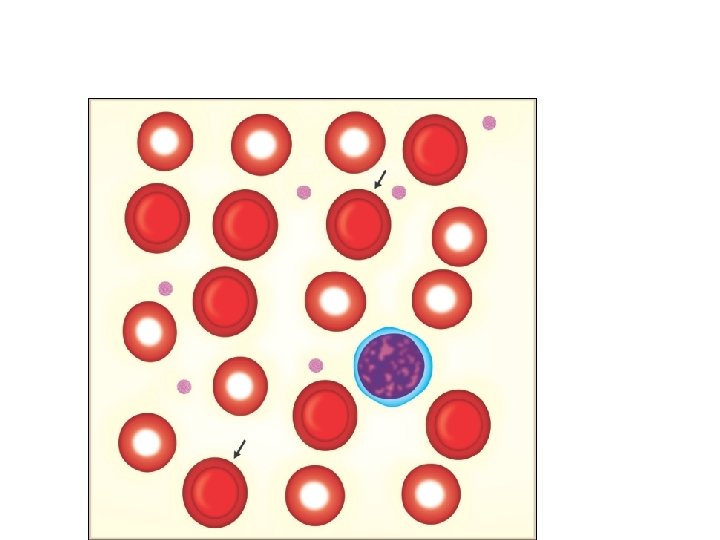
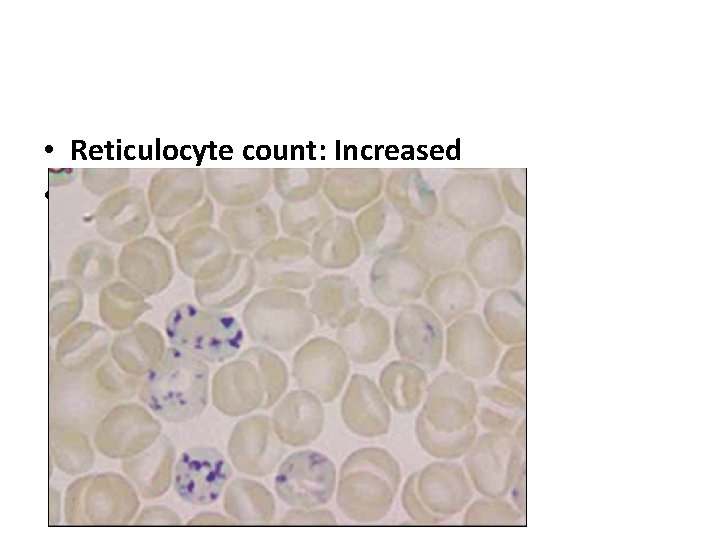
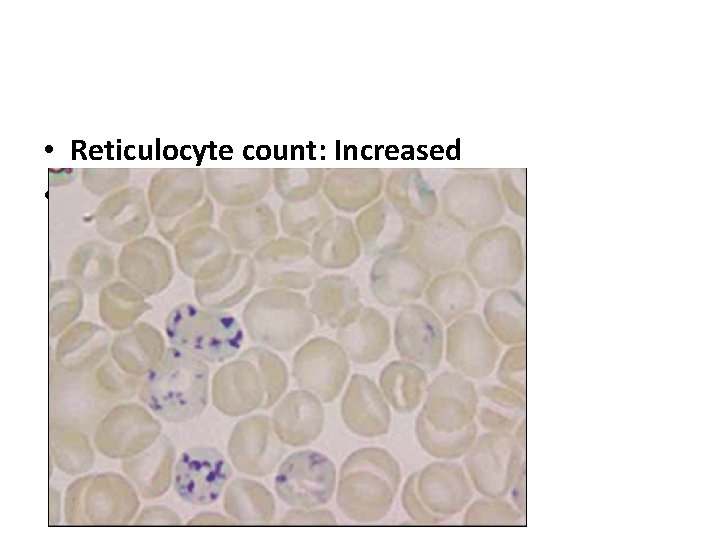
• Reticulocyte count: Increased •
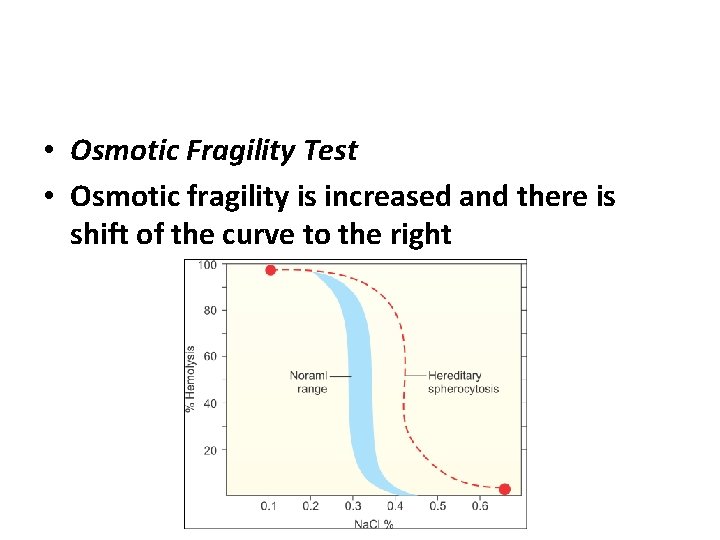
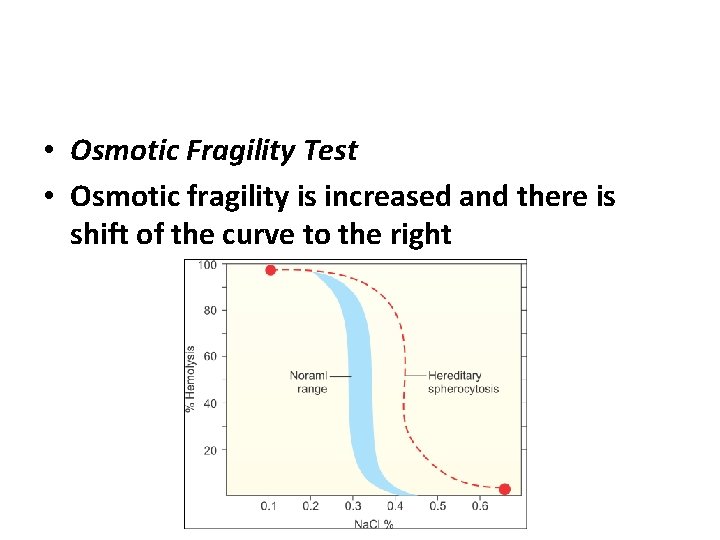
• Osmotic Fragility Test • Osmotic fragility is increased and there is shift of the curve to the right
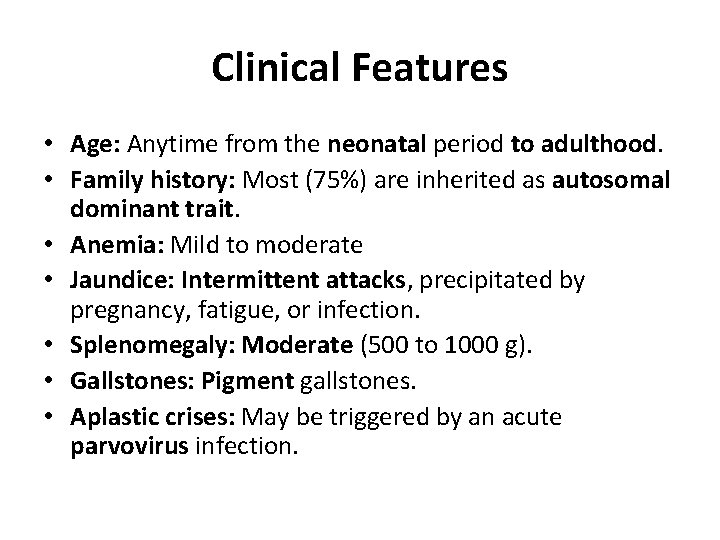
Clinical Features • Age: Anytime from the neonatal period to adulthood. • Family history: Most (75%) are inherited as autosomal dominant trait. • Anemia: Mild to moderate • Jaundice: Intermittent attacks, precipitated by pregnancy, fatigue, or infection. • Splenomegaly: Moderate (500 to 1000 g). • Gallstones: Pigment gallstones. • Aplastic crises: May be triggered by an acute parvovirus infection.