Aortic Stenosis Errors in Echo and Hemodynamic Assessment




- Slides: 17
Aortic Stenosis: Errors in Echo and Hemodynamic Assessment Howard C. Herrmann, MD University of Pennsylvania Philadelphia
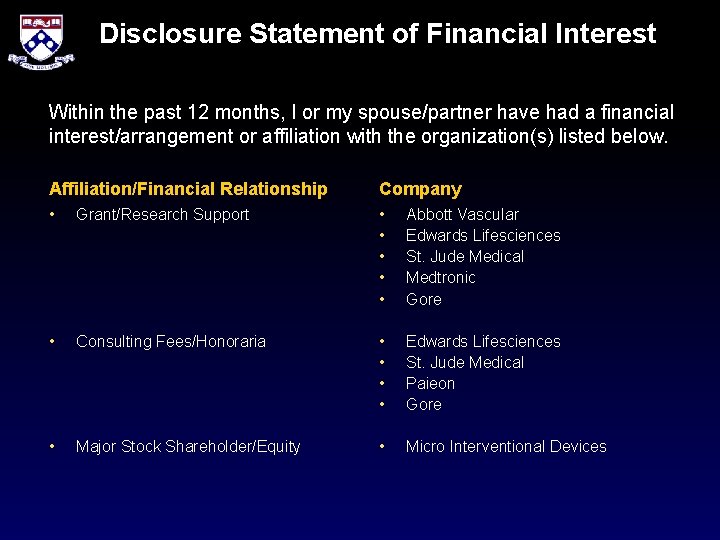
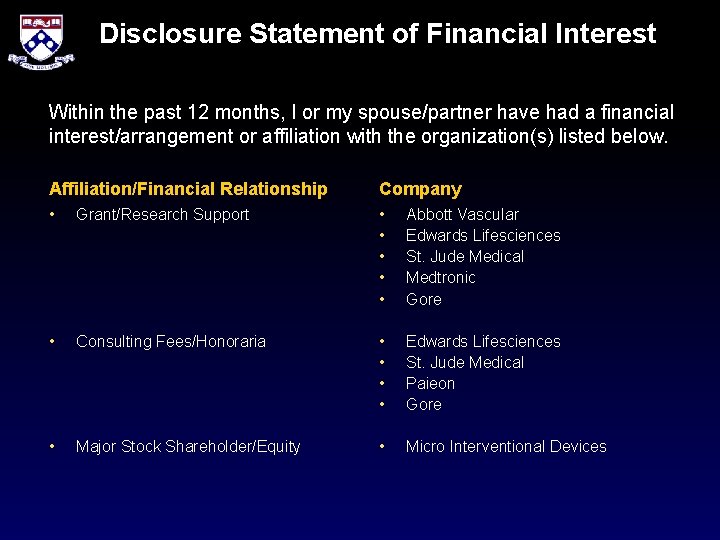
Disclosure Statement of Financial Interest Within the past 12 months, I or my spouse/partner have had a financial interest/arrangement or affiliation with the organization(s) listed below. Affiliation/Financial Relationship • Grant/Research Support Company • Abbott Vascular • Edwards Lifesciences • St. Jude Medical • Medtronic • Gore • Consulting Fees/Honoraria • • Edwards Lifesciences St. Jude Medical Paieon Gore • Major Stock Shareholder/Equity • Micro Interventional Devices
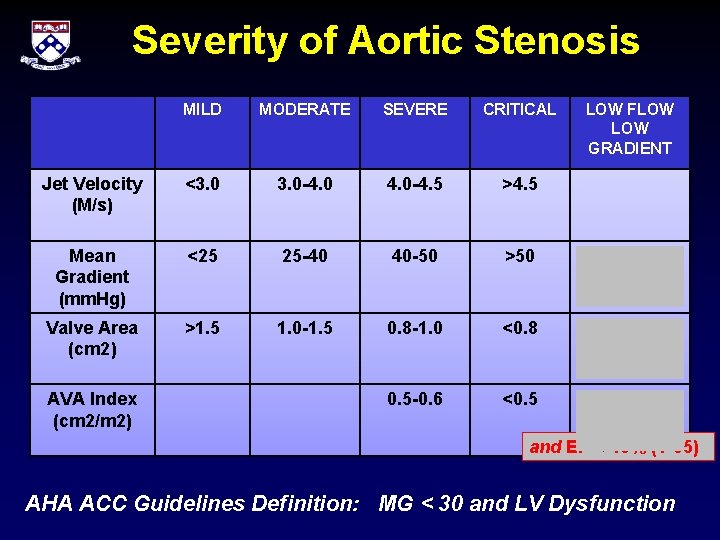
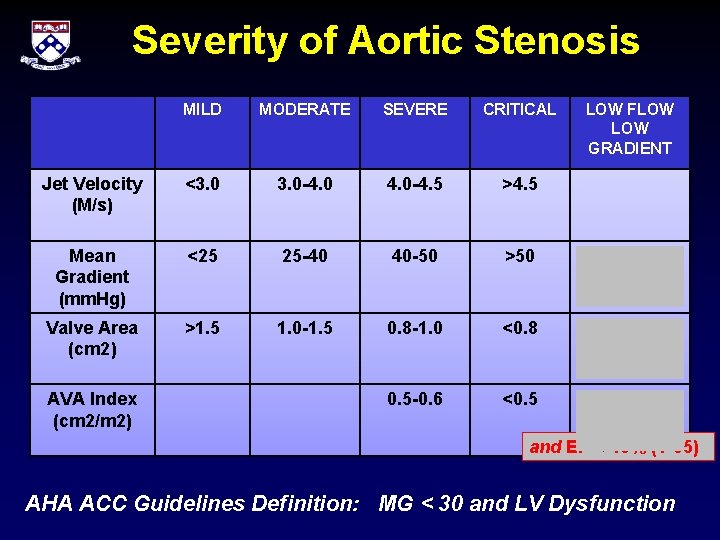
Severity of Aortic Stenosis MILD MODERATE SEVERE CRITICAL Jet Velocity (M/s) <3. 0 -4. 5 >4. 5 Mean Gradient (mm. Hg) <25 25 -40 40 -50 >50 <40 (? <35, 30) Valve Area (cm 2) >1. 5 1. 0 -1. 5 0. 8 -1. 0 <0. 8 < 0. 8 (? <1. 2, 1. 0) 0. 5 -0. 6 <0. 5 < 0. 6 AVA Index (cm 2/m 2) LOW FLOW GRADIENT and EF < 40% (? 35) AHA ACC Guidelines Definition: MG < 30 and LV Dysfunction
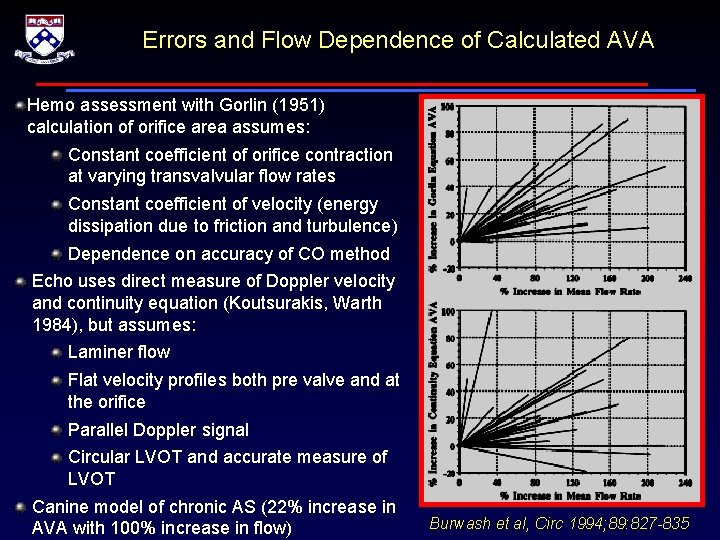
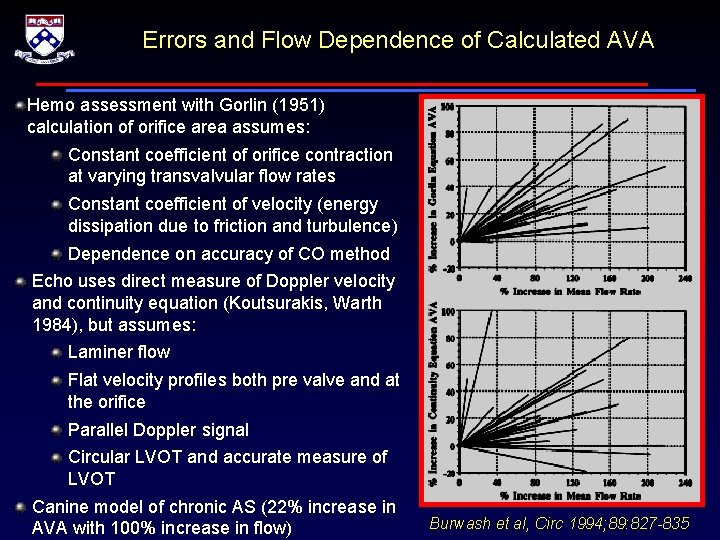
Errors and Flow Dependence of Calculated AVA Hemo assessment with Gorlin (1951) calculation of orifice area assumes: Constant coefficient of orifice contraction at varying transvalvular flow rates Constant coefficient of velocity (energy dissipation due to friction and turbulence) Dependence on accuracy of CO method Echo uses direct measure of Doppler velocity and continuity equation (Koutsurakis, Warth 1984), but assumes: Laminer flow Flat velocity profiles both pre valve and at the orifice Parallel Doppler signal Circular LVOT and accurate measure of LVOT Canine model of chronic AS (22% increase in AVA with 100% increase in flow) Burwash et al, Circ 1994; 89: 827 -835
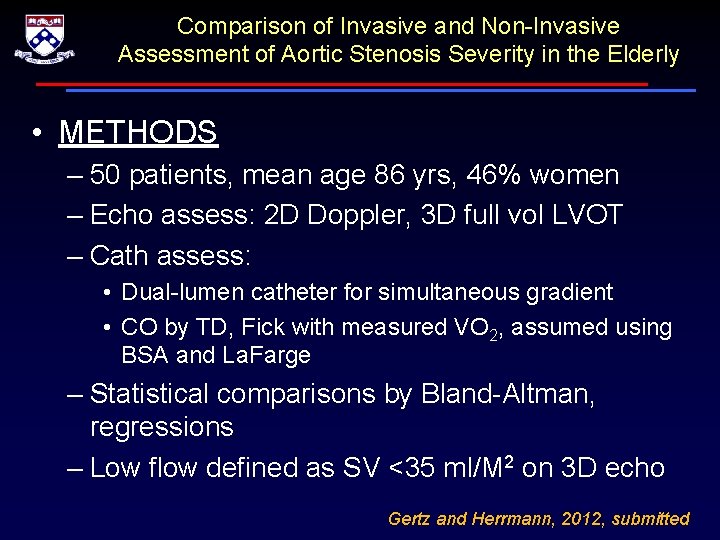
Comparison of Invasive and Non-Invasive Assessment of Aortic Stenosis Severity in the Elderly • METHODS – 50 patients, mean age 86 yrs, 46% women – Echo assess: 2 D Doppler, 3 D full vol LVOT – Cath assess: • Dual-lumen catheter for simultaneous gradient • CO by TD, Fick with measured VO 2, assumed using BSA and La. Farge – Statistical comparisons by Bland-Altman, regressions – Low flow defined as SV <35 ml/M 2 on 3 D echo Gertz and Herrmann, 2012, submitted




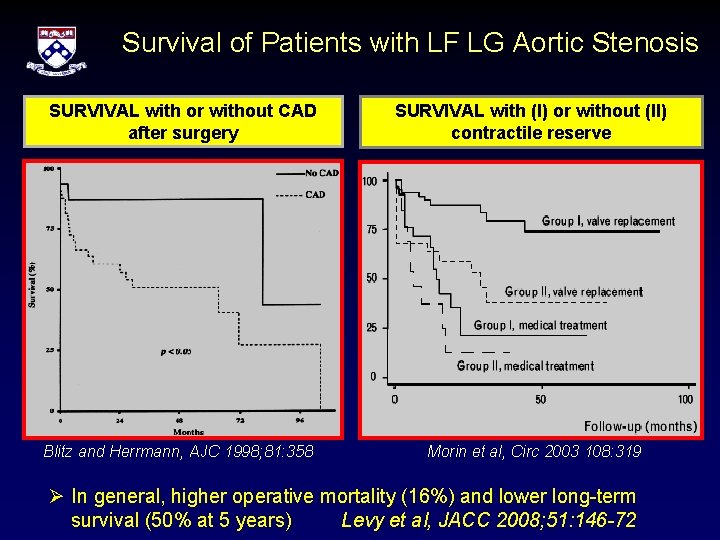
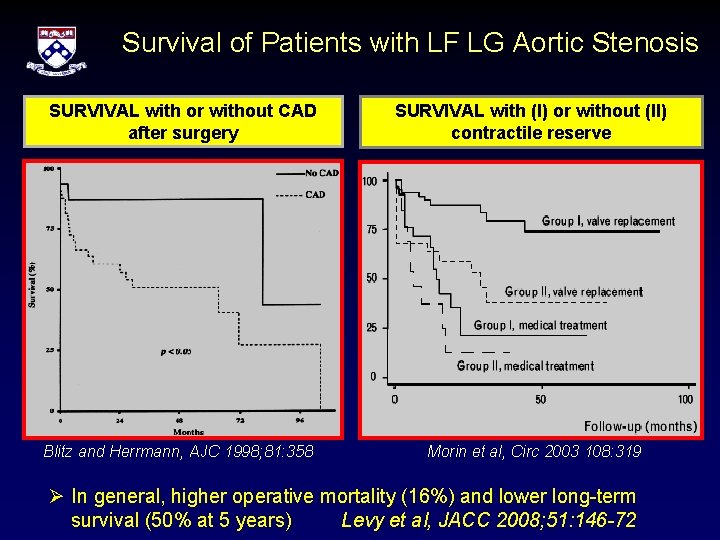
Survival of Patients with LF LG Aortic Stenosis SURVIVAL with or without CAD after surgery Blitz and Herrmann, AJC 1998; 81: 358 SURVIVAL with (I) or without (II) contractile reserve Morin et al, Circ 2003 108: 319 Ø In general, higher operative mortality (16%) and lower long-term survival (50% at 5 years) Levy et al, JACC 2008; 51: 146 -72
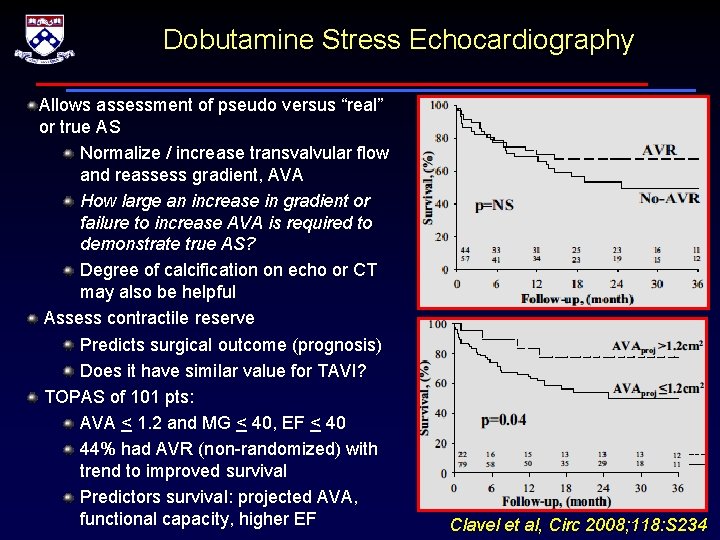
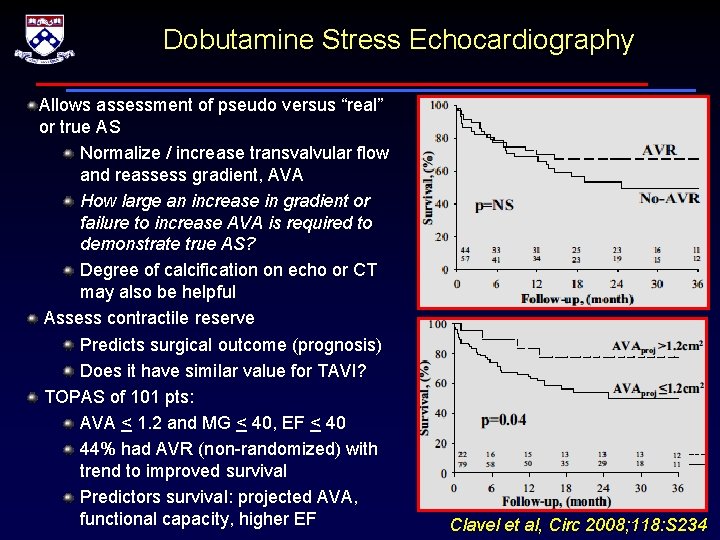
Dobutamine Stress Echocardiography Allows assessment of pseudo versus “real” or true AS Normalize / increase transvalvular flow and reassess gradient, AVA How large an increase in gradient or failure to increase AVA is required to demonstrate true AS? Degree of calcification on echo or CT may also be helpful Assess contractile reserve Predicts surgical outcome (prognosis) Does it have similar value for TAVI? TOPAS of 101 pts: AVA < 1. 2 and MG < 40, EF < 40 44% had AVR (non-randomized) with trend to improved survival Predictors survival: projected AVA, functional capacity, higher EF Clavel et al, Circ 2008; 118: S 234
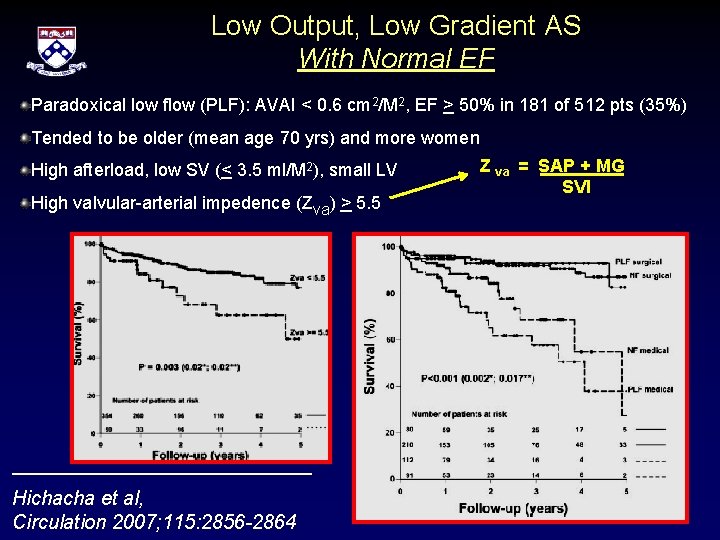
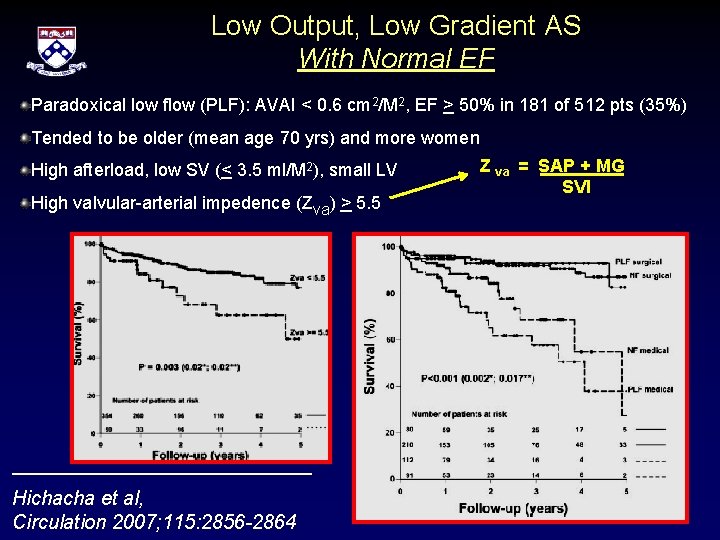
Low Output, Low Gradient AS With Normal EF Paradoxical low flow (PLF): AVAI < 0. 6 cm 2/M 2, EF > 50% in 181 of 512 pts (35%) Tended to be older (mean age 70 yrs) and more women High afterload, low SV (< 3. 5 ml/M 2), small LV High valvular-arterial impedence (Zva) > 5. 5 Hichacha et al, Circulation 2007; 115: 2856 -2864 Z va = SAP + MG SVI
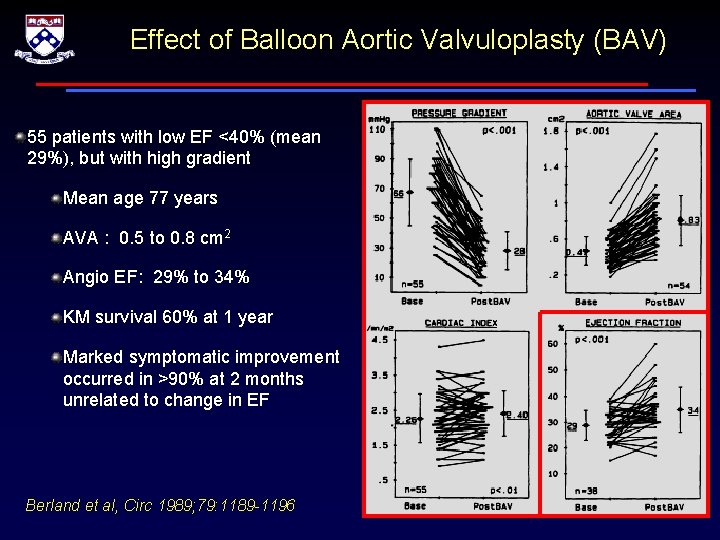
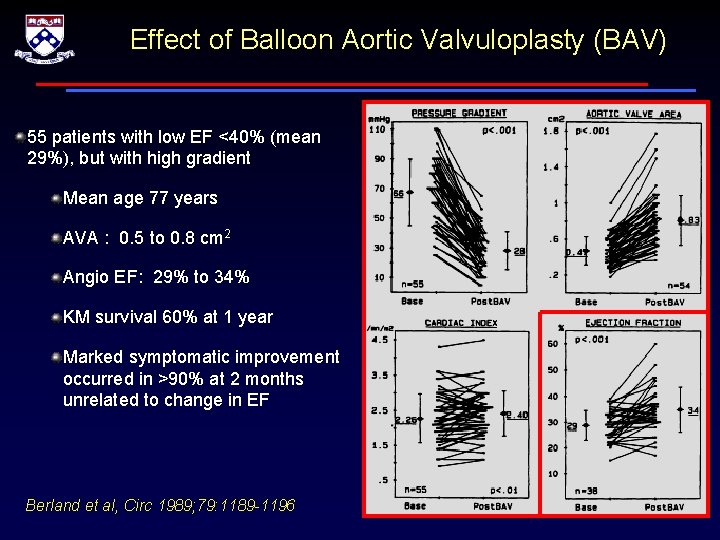
Effect of Balloon Aortic Valvuloplasty (BAV) 55 patients with low EF <40% (mean 29%), but with high gradient Mean age 77 years AVA : 0. 5 to 0. 8 cm 2 Angio EF: 29% to 34% KM survival 60% at 1 year Marked symptomatic improvement occurred in >90% at 2 months unrelated to change in EF Berland et al, Circ 1989; 79: 1189 -1196
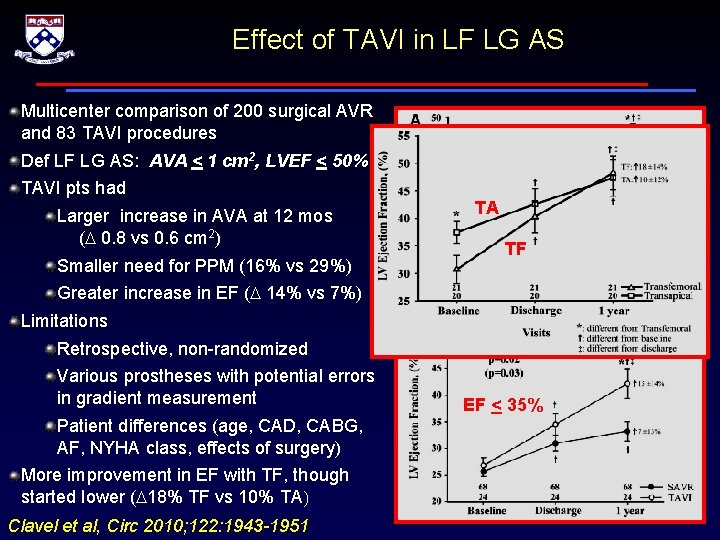
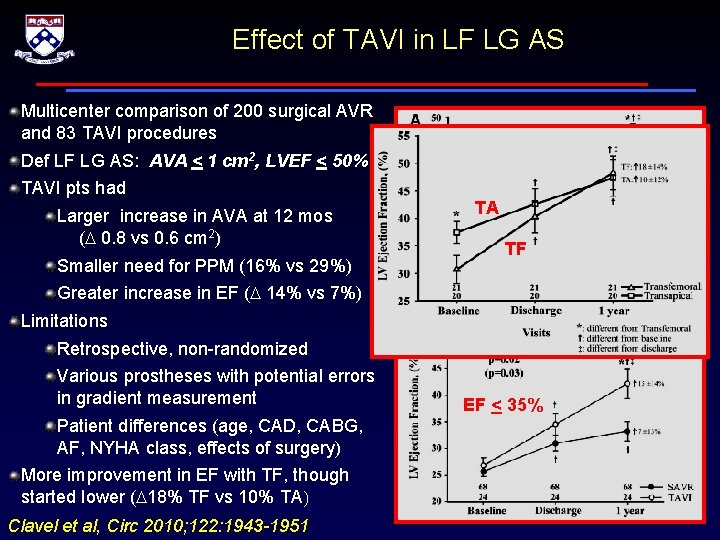
Effect of TAVI in LF LG AS Multicenter comparison of 200 surgical AVR and 83 TAVI procedures Def LF LG AS: AVA < 1 cm 2, LVEF < 50% TAVI pts had Larger increase in AVA at 12 mos (D 0. 8 vs 0. 6 cm 2) Smaller need for PPM (16% vs 29%) ALL PATIENTS TA TF Greater increase in EF (D 14% vs 7%) Limitations Retrospective, non-randomized Various prostheses with potential errors in gradient measurement Patient differences (age, CAD, CABG, AF, NYHA class, effects of surgery) More improvement in EF with TF, though started lower (D 18% TF vs 10% TA) Clavel et al, Circ 2010; 122: 1943 -1951 EF < 35%
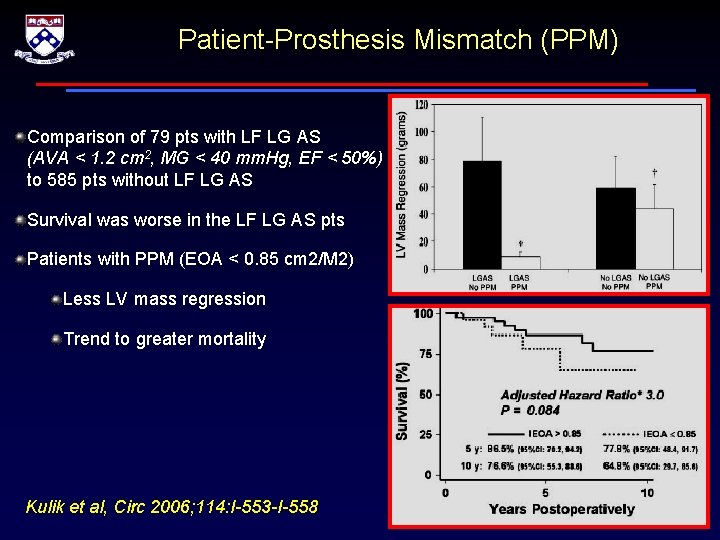
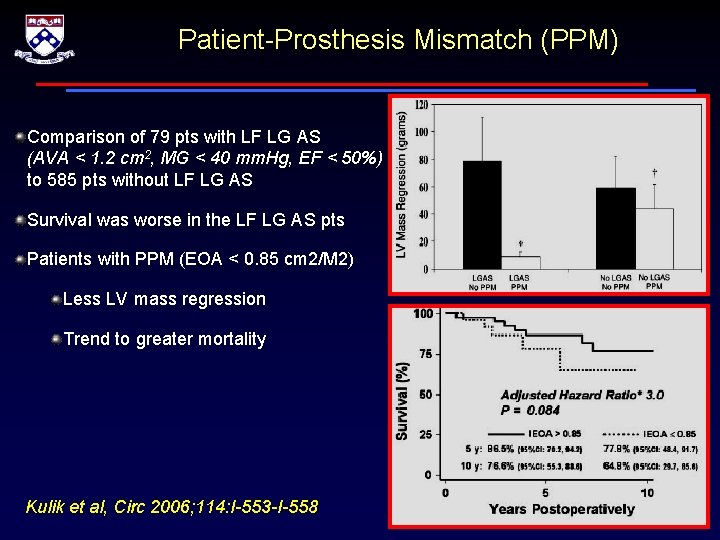
Patient-Prosthesis Mismatch (PPM) Comparison of 79 pts with LF LG AS (AVA < 1. 2 cm 2, MG < 40 mm. Hg, EF < 50%) to 585 pts without LF LG AS Survival was worse in the LF LG AS pts Patients with PPM (EOA < 0. 85 cm 2/M 2) Less LV mass regression Trend to greater mortality Kulik et al, Circ 2006; 114: I-553 -I-558
Conclusions (1): AS Assessment in General • In elderly patients, traditional measures of AS severity correlate poorly and using different measures frequently misclassifies critical AS • Current guidelines rec invasive assessment only when there is discrepancy between clinical symptoms and noninvasive findings – Common in the elderly with diastolic dysfunction, low SV, AF, multiple co-morbidities • We recommend 3 D-echo as the gold standard for noninvasive assessment – TD CO when invasive assessment is undertaken – In patients with LF, a less flow dependent measure (eg. resistance) should be considered
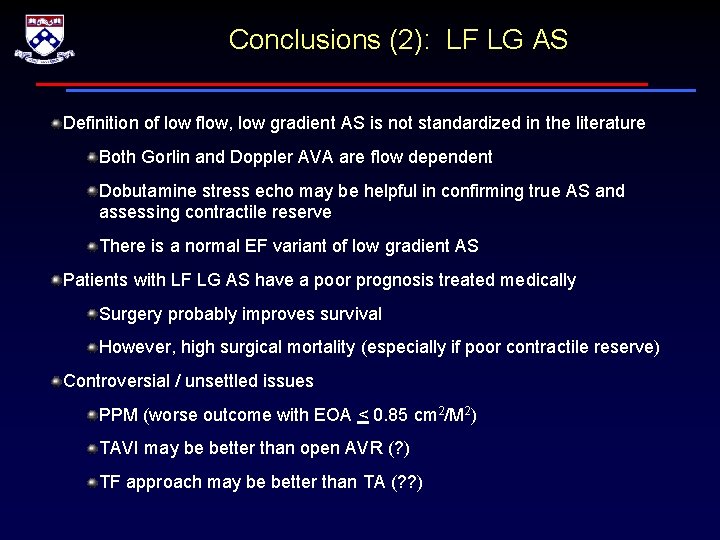
Conclusions (2): LF LG AS Definition of low flow, low gradient AS is not standardized in the literature Both Gorlin and Doppler AVA are flow dependent Dobutamine stress echo may be helpful in confirming true AS and assessing contractile reserve There is a normal EF variant of low gradient AS Patients with LF LG AS have a poor prognosis treated medically Surgery probably improves survival However, high surgical mortality (especially if poor contractile reserve) Controversial / unsettled issues PPM (worse outcome with EOA < 0. 85 cm 2/M 2) TAVI may be better than open AVR (? ) TF approach may be better than TA (? ? )