AORN Fire Safety Tool Kit Fire Prevention in
- Slides: 32
AORN Fire Safety Tool Kit Fire Prevention in the Perioperative Practice Setting
Goals After completing this learning activity, perioperative team members will have increased knowledge of fire safety in the perioperative practice setting and of tools to promote fire prevention, plan effective responses, and develop evidence-based policies to protect perioperative patients and personnel.
Learning Outcomes After completing this activity, the participant will be able to: 1. Identify the locations where a fire may occur 2. Identify the three components of the fire triangle 3. Identify fire prevention interventions 4. Describe the fire risk assessment
Fire Facts Estimated Frequency • 200 to 240 per year in the United States o 44% head, neck, or upper chest o 26% elsewhere on the patient o 21% in the airway o 8% elsewhere in the patient
Patient Injuries Of the 200 to 240 OR fires per year, • 20 to 30 are serious and result in disfiguring or disabling injuries • 1 to 2 are fatal
Location • Ambulatory surgery centers • Hospitals • Physicians’ offices
Patients All patients 7
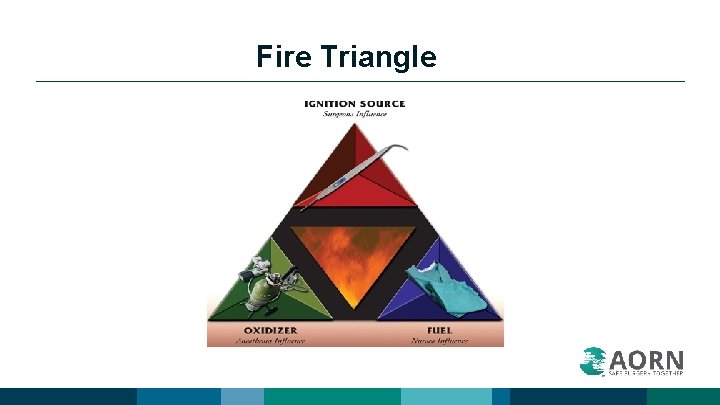
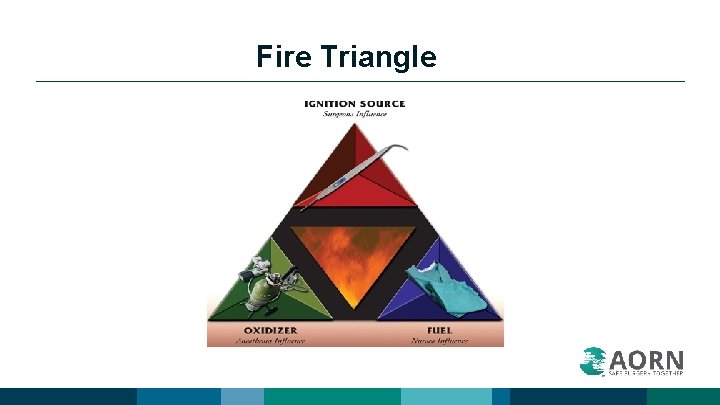
Fire Triangle
Team Effort • • Nurses Surgical technologists Surgeons Assistants Environmental Services associates Administration team members Everyone else not mentioned
Fire Prevention Assessment • • Perform before the start of the procedure. All members of the team participate. Communicate this assessment during the “time out. ” Document the assessment in the patient’s record. .
Fire Prevention Assessment • Ignition sources that are present • Fuels that are present • The potential for the presence of an oxygen-enriched environment 11
Fire Prevention Assessment Tool A. Is an alcohol-based prep agent or other volatile chemical being used preoperatively? Y or N B. Is the surgical procedure being performed above the xiphoid process? Y or N C. Is open oxygen or nitrous oxide being administered? Y or N D. Is an electrosurgical unit, laser, or fiber-optic light cord being used? Y or N E. Are there other possible contributors? Y or N
Ignition Sources • Electrosurgical unit (ESU) • Argon beam coagulator • Power tools (eg, drills, burrs) • Laser • Fiber-optic light • Defibrillator • Electrical equipment
Controlling Ignition Sources: Interventions • Place the patient return electrode on a large muscle mass close to the surgical site. • Keep active electrode cords from coiling. • Store the ESU pencil in a safety holster when not in use.
Controlling Ignition Sources: Interventions • Do not use an ignition source to enter the bowel when it is distended with gas. • Keep the ESU active electrode away from oxygen or nitrous oxide. • Keep the active electrode tip clean. • Use active electrodes or return electrodes that are manufacturer-approved for the ESU being used. • Use approved protective covers as insulators on the active electrode tip, NOT red rubber catheter or packing material. • Activate the active electrode only in close proximity to target tissue and away from other metal objects.
Controlling Ignition Sources: Interventions • Inspect minimally invasive electrosurgical electrodes for impaired insulation; remove electrode from service if not intact. • Use “cut” or “blend” settings instead of coagulation. • Use the lowest power setting for the ESU. • Only the person controlling the active electrode activates the ESU. • Remove the active electrode from the electrosurgical or electrocautery unit before discarding.
Controlling Ignition Sources: Interventions • • • Use a laser-resistant endotracheal tube when using a laser during upper airway procedures. Place wet sponges around the endotracheal tube cuff if the surgeon is operating in close proximity to the endotracheal tube. Use wet sponges or towels around the surgical site. Only the person controlling the laser beam activates the laser. Have water or saline and the appropriate type of fire extinguisher available.
Controlling Ignition Sources: Interventions • • • Place the light source in standby mode or turn it off when not in use. Inspect light cables before use and remove them from service if broken light bundles are visible. Select defibrillator paddles that are the correct size for the patient. Use only manufacturer-recommended defibrillator paddle lubricant. Place defibrillator paddles appropriately.
Controlling Ignition Sources: Interventions • • • Inspect electrical cords and plugs for integrity and remove from service if broken. Check biomedical inspection stickers on equipment for a current inspection date and remove the equipment from service if not current. Do not bypass or disable equipment safety features. Follow manufacturer’s recommendations for use. Keep fluids off of electrical equipment.
Oxidizers • Oxygen-enriched environment • Nitrous oxide 20
Controlling the Oxidizer: Interventions • Tent drapes to allow for free air flow. • Keep the oxygen percentage as low as possible. • Use an adhesive incise drape.
Controlling the Oxidizer: Interventions • Inflate the endotracheal tube cuff with tinted saline. • Evacuate the surgical smoke from small or enclosed spaces. • Pack wet sponges around the back of the patient’s throat. • If oxygen is being used, suction the patient’s oropharynx deeply before using the ignition source.
Controlling the Oxidizer: Interventions • Inform the surgeon that an open oxygen source is being used. • Stop supplemental oxygen or nitrous oxide before and during the use of an ignition source. • Check the anesthesia circuits for possible leaks. • Turn off the oxygen at end of each procedure.
Controlling the Oxidizer: Interventions • Oxygen delivery during head, face, neck, and upper chest surgery: o o o Do not use open delivery of 100% oxygen. Intubate or use a laryngeal mask airway if supplemental oxygen needed. If oxygen is greater than 30% via open delivery, use 5 L to 10 L of air/minute under the drapes. • Exceptions: o o Patient verbal response required during surgery (eg, carotid artery surgery, neurosurgery, pacemaker insertion) Open oxygen delivery required to keep the patient safe
Fuels • • Patient Personnel Drapes Gowns Towels Sponges Dressings Tapes • • • Linens Head coverings Shoe covers Collodion Alcohol-based skin preparations • Human hair • Endotracheal tubes
Controlling Fuels: Interventions • Use moist towels around the surgical site when using a laser. • During throat surgery, use moist sponges as packing in the throat. • Use water-based ointment and not oil-based ointment in facial hair and other hair near the surgical site.
Controlling Fuels: Interventions • Prevent pooling of skin prep solutions. • Remove prep-soaked linen and disposable prepping drapes. • Allow skin-prep agents to dry and fumes to dissipate before draping. • Allow chemicals (eg, alcohol, collodion, tinctures) to dry. • Conduct a skin prep “time out. ”
CMS Regulations: Alcohol-Based Skin Preps • • • Policies and procedures must be in place to reduce risk of fire. Personnel must be aware of these policies. Products are packaged for controlled delivery with clear directions that must be followed. Documentation of implementation of fire prevention practices must be present in the patient’s medical record. Personnel must demonstrate practice of the policies and procedures.
CMS Regulations: Alcohol-Based Skin Preps • The CMS inspector approaches you and asks, “What is your facility doing to reduce the risk of fires related to alcohol-based skin preps? ”
Summary Steps for surgical fire prevention 1. Know the components a) Ignition sources b) Oxidizers c) Fuels 2. Communicate a) Fire risk assessment
References Centers for Medicare & Medicaid Services. State Operations Manual. Appendix A—Survey Protocol, Regulations and Interpretive Guidelines for Hospitals. http: //cms. gov/manuals/Downloads/som 107 ap_a_hospitals. pdf. Accessed October 28, 2018. Clarke JR, Bruley ME. Surgical fires: trends associated with prevention efforts. Pa Patient Saf Advis. 2012; 9(2): 130 -135. ECRI Institute. New clinical guide to surgical fire prevention. Patients can catch fire—here’s how to keep them safer. Health Devices. 2009; 38(10): 314 -332. Guideline for a safe environment of care. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc. Guideline for safe use of energy-generating devices. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc.
The End