Anxiety disorders Anxiety is a normal protective psychological









- Slides: 50
Anxiety disorders
• Anxiety is a normal, protective, psychological response to an unpleasant or threatening situation. • Mild to moderate anxiety can improve performance and ensure appropriate action is taken. • However, excessive or prolonged symptoms can be disabling, lead to severe distress and cause much impairment to social functioning.
Pathophysiology Anxiety occurs when there is a disturbance of the arousal systems in the brain. Arousal is maintained by at least three interconnected systems: a general arousal system, an ‘emotional’ arousal system and an endocrine/autonomic arousal system. Excessive activity in this system, due to internal or external stresses, can lead hyperarousal as seen in anxiety. to a state of
Pathophysiology These arousal systems activate somatic responses to arousal, such as increased muscle tone, increased sympathetic activity and increased output of anterior and posterior pituitary hormones. Inappropriate increases in autonomic activity are often associated with anxiety states; the resulting symptoms (palpitations, sweating, tremor, etc. ) may initiate a vicious circle that increases the anxiety.
Pathophysiology Several neurotransmitters have been implicated in the arousal systems: • Acetylcholine is the main transmitter maintaining general arousal • noradrenergic and serotonergic are associated with emotional arousal activity. • Drugs which antagonize such activity have anxiolytic effects. • In addition, the inhibitory neurotransmitter γ-aminobutyric acid (GABA) exerts an inhibitory control on other transmitter pathways and increased GABA activity may have a protective effect against excessive stress reactions. • Many drugs which increase GABA activity, such as the benzodiazepines, are potent anxiolytics.
Etiology • Stress, appears to be linked to genetic factors. • Anxiety may also be induced by central stimulant drugs (caffeine, amphetamines). • Withdrawal from chronic use of central nervous system depressant drugs (alcohol, hypnotics, anxiolytics). • Metabolic disturbances (hyperventilation, hypoglycaemia, thyrotoxicosis). • It may be part of a depressive disorder. • Long history of high anxiety levels going back to childhood
Clinical Manifestations Somatic symptoms may be prominent in anxiety and include: • Palpitations • Chest pain • Shortness of breath • Dizziness • Dysphagia • Gastro-intestinal disturbances • Loss of libido • Headaches and tremor • Panic attacks are experienced as storms of increased autonomic activity combined with a fear of imminent death or loss of control

Treatment for anxiety disorders often requires multiple approaches: Psychotherapy Psychological therapies (talking therapies) are generally considered first-line treatments in all anxiety disorders because they may provide a longer lasting response and lower relapse rates than pharmacotherapy • the most supporting evidence in anxiety disorders is cognitive behavioral therapy (CBT)
Pharmacotherapy Benzodiazepines • Benzodiazepines are commonly prescribed to provide immediate relief of the symptoms of severe anxiety. • All benzodiazepines anxiolytic, amnesic, have muscular sedative/hypnotic, relaxant and anticonvulsant actions with minor differences in the relative potency of these effects. • A number of different benzodiazepines are available
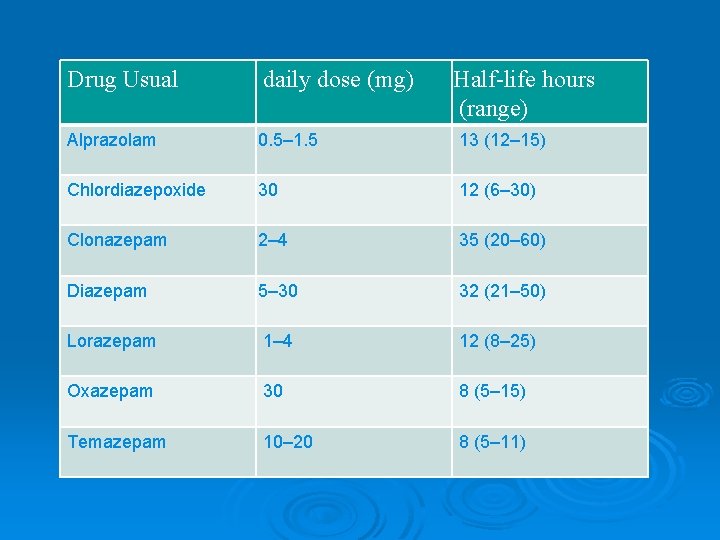
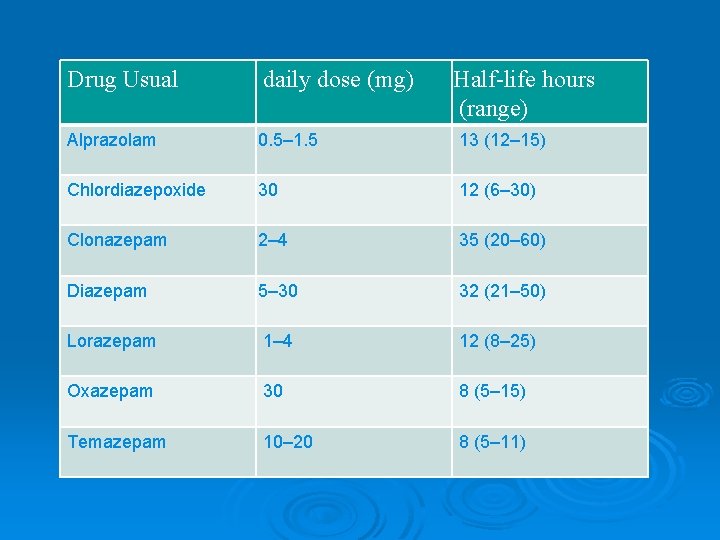
Drug Usual daily dose (mg) Half-life hours (range) Alprazolam 0. 5– 1. 5 13 (12– 15) Chlordiazepoxide 30 12 (6– 30) Clonazepam 2– 4 35 (20– 60) Diazepam 5– 30 32 (21– 50) Lorazepam 1– 4 12 (8– 25) Oxazepam 30 8 (5– 15) Temazepam 10– 20 8 (5– 11)

Mechanism of Action • Neuronal activity in the CNS is regulated by the balance between GABA inhibitory activity and excitatory neurotransmitters such as glutamate. • If the balance swings towards more GABA activity, sedation, ataxia and amnesia occur. Conversely, when GABA is reduced arousal, anxiety and restlessness occur. • All benzodiazepines bind to postsynaptic GABA-A receptors in the brain, with varying degrees of affinity, and potentiate the inhibitory actions of GABA at these sites. • GABA is the most important inhibitory neurotransmitter in the central nervous system (CNS).
Adverse effects may include: • Drowsiness, lightheadedness, confusion, ataxia, amnesia, a paradoxical increase in aggression, an increased risk of falls and fractures in the elderly and an increased risk of road traffic accidents. • They are also widely acknowledged as addictive and cause tolerance after more than 2– 4 weeks of continuous use. • Respiratory depression is rare, but possible following high oral doses or parenteral use. • Flumazenil, a benzodiazepine receptor antagonist, can reverse the effects of severe reactions but requires repeated dosing because of its short half-life.

Benzodiazepine withdrawal • Abrupt withdrawal in dependent subjects is dangerous and can induce acute anxiety, psychosis or convulsions. • Gradual withdrawal are necessary with psychological treatments, can be successful in the majority of patients. • The duration of withdrawal should be tailored to individual needs and may last many months. Dosage reductions may be of the order of 1– 2 mg of diazepam per month. • Even with slow dosage reduction, a variety of withdrawal symptoms may be experienced, including increased anxiety, insomnia, hypersensitivity to sensory stimuli, perceptual distortions, paraesthesia, muscle twitching, depression and many others.
Antidepressant drugs • Antidepressants can provide a long-term treatment option for those with an anxiety disorder. • They are recommended for those who are unable to commit to or have not responded to psychological therapies. • In addition, antidepressants are considered first-line treatment option either alone or in combination with CBT in patients suffering from Obsessive-compulsive disorder (OCD) with moderate or severe impairment. • The response rate to antidepressants in anxiety is often lower and takes longer than that seen in depression.
Selective serotonin reuptake inhibitors • The selective serotonin reuptake inhibitors (SSRIs) have a broad anxiolytic effect and are considered the first drug options in GAD, panic disorder, social phobia, PTSD and OCD. • Initial worsening of symptoms is common when starting an SSRI in anxiety, so beginning with half the dose than that used in depression is recommended as is reassuring the patient that this is usually only experienced for the first few weeks of treatment.
Tricyclic antidepressants • Certain TCAs such as clomipramine, imipramine and amitriptyline are efficacious in some anxiety disorders. • They are, however, associated with a greater burden of adverse reactions such as anticholinergic effects, hypotension and weight gain. • Particular concern is the TCAs' cardiac toxicity in overdose which relegates their use to second line following the failure of an SSRI.
Monoamine-oxidase inhibitors • The monoamine-oxidase inhibitors (MAOIs) are rarely used in practice because of their potential interactions with other medicines and tyramine in the diet. • Moclobemide is a reversible MAOI, so causes fewer problematic interactions. • Phenelzine and moclobemide are occasionally used by specialists in social phobia following the failure of an SSRI. • Phenelzine is also recommended as a third-line treatment option in PTSD
Other antidepressants • The selective and noradrenaline reuptake inhibitor (SNRI) venlafaxine has some evidence to support its use in almost all the anxiety disorders, but it is only licensed for use in GAD and social phobia at a dose of 75 mg/day in the extended release form. • Withdrawal effects and increase blood pressure at higher doses are the major problems. • Duloxetine, another SNRI, is also licensed in GAD and can similarly increase blood pressure.
• Mirtazapine, an α 2 -adrenoreceptor antagonist, is recommended as an option for PTSD if patients do not wish to participate in trauma focused CBT. • Mirtazapine has a lower incidence of nausea, vomiting and sexual dysfunction than the SSRIs but can commonly cause weight gain and sedation.
General considerations for anxiety disorders Ø Often have an early onset- teens or early twenties Ø Show 2: 1 female predominance Ø Similar to major depression and chronic diseases such as diabetes in functional impairment and decreased quality of life
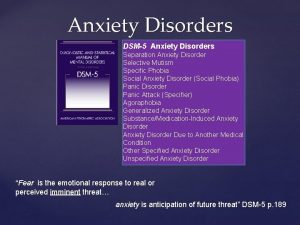
Anxiety disorders Panic disorder (PD) Ø Specific phobia Ø Social anxiety disorder (SAD) Ø Generalized anxiety disorder (GAD) Ø Obsessive. Compulsive disorder (OCD) Ø Posttraumatic Stress Disorder (PTSD) Ø Acute Stress Disorder Ø Anxiety Disorder due to a General Medical Condition Ø Substance-Induced Anxiety Disorder Ø

Comorbid diagnosis Ø Once an anxiety disorder is diagnosed, it is critical to screen for other psychiatric diagnosis since it is very common for other diagnosis to be present and this can impact both treatment and prognosis.
Panic Disorder
Panic Disorder Ø Recurrent unexpected panic attacks and for a one month period or more of: l Persistent worry about having additional attacks l Worry about the implications of the attacks l Significant change in behavior because of the attacks
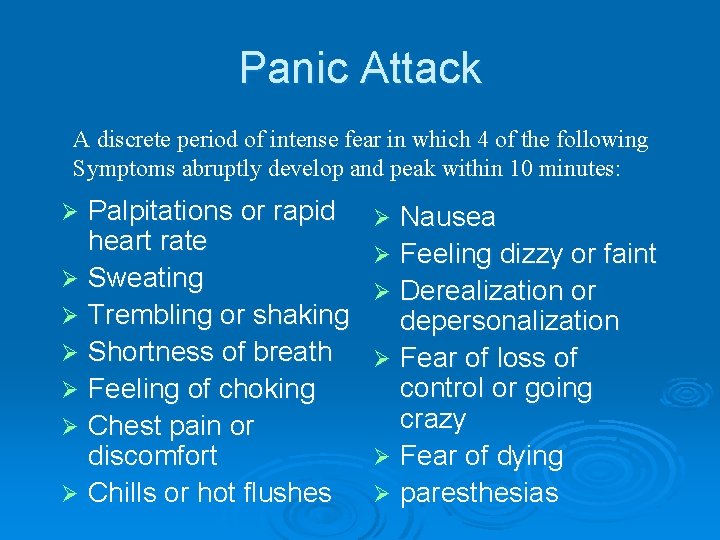
Panic Attack A discrete period of intense fear in which 4 of the following Symptoms abruptly develop and peak within 10 minutes: Palpitations or rapid heart rate Ø Sweating Ø Trembling or shaking Ø Shortness of breath Ø Feeling of choking Ø Chest pain or discomfort Ø Chills or hot flushes Ø Nausea Ø Feeling dizzy or faint Ø Derealization or depersonalization Ø Fear of loss of control or going crazy Ø Fear of dying Ø paresthesias Ø
Panic disorder epidemiology Ø -1 -3% of general population; 5 -10% of primary care patients ---Onset in teens or early 20’s Ø -Female: male 2 -3: 1
Panic disorder epidemiology Ø 30 -50% l avoidance of situations where escape would be difficult Ø 50 -60% l have agoraphobia have lifetime major depression one third with current depression Ø 20 -25% have dependence history of substance
Panic Disorder Etiology Ø Drugs/alcohol Ø Genetics Ø Social learning Ø Cognitive theories Ø Neurobiology/conditioned fear Ø Psychosocial stressors l prior separation anxiety

Treatment Ø Education, reassurance, elimination of caffeine, alcohol, drugs, OTC stimulants Ø Cognitive-behavioral therapy Ø Medications tricyclics, – SSRIs, MAOIs, valproate, gabapentin venlafaxine, benzodiazepines,
Generalized Anxiety Disorder
Generalized Anxiety Disorder Ø Excessive worry more days than not for at least 6 months about a number of events and they find it difficult to control the worry. Ø 3 or more of the following symptoms: l restlessness, easily fatigued, difficulty concentrating, irritable, muscle tension, sleep disturbanc
Generalized Anxiety Disorder Epidemiology Ø 4 -7 % of general population Ø Onset in childhood or adolescence Ø Female: male 2 to 1

GAD Treatment Ø Medications including: Ø Buspirone (does not carry the risk of physical dependence and withdrawal symptoms) Ø Benzodiazepines Ø antidepressants (SSRIs, venlafaxine, imipramine) Ø Cognitive-behavioral therapy
Obsessive-Compulsive Disorder Obsessions or compulsions defined by: l Recurrent and persistent thoughts, impulses or images that are intrusive and inappropriate and cause marked anxiety. l Impulses or images are not simply excessive worries about real-life problems. l The person attempts to ignore or suppress these things or neutralize them. l The person recognizes these thoughts or images as a products of their own mind.
OCD continued Ø At some point the person has recognized that the obsessions or compulsions are excessive. Ø The obsessions or compulsions cause marked distress, take > 1 hour/day or interfere with the person’s normal routine or function.
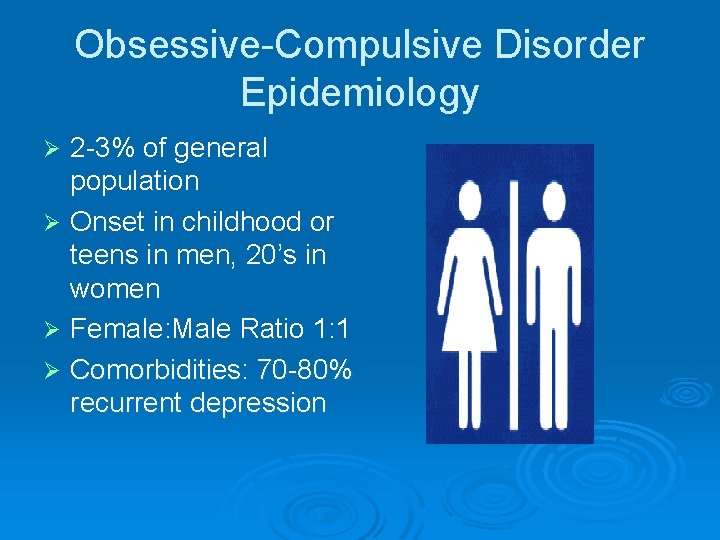
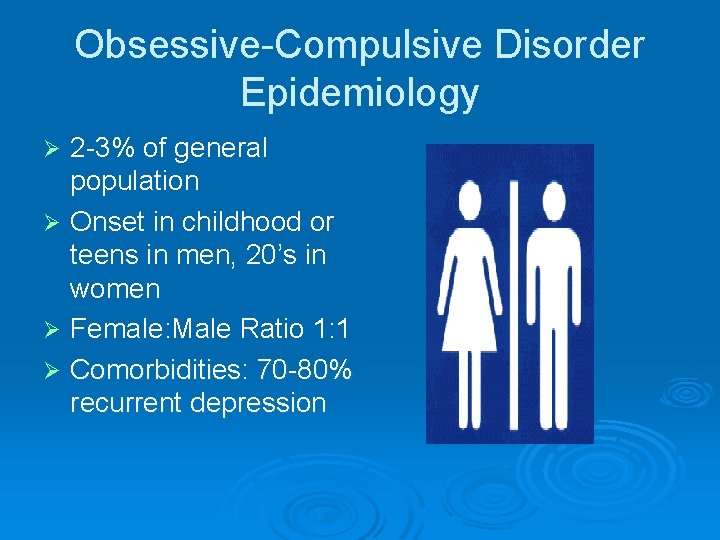
Obsessive-Compulsive Disorder Epidemiology 2 -3% of general population Ø Onset in childhood or teens in men, 20’s in women Ø Female: Male Ratio 1: 1 Ø Comorbidities: 70 -80% recurrent depression Ø

Treatment Ø 40 -60% treatment response Ø Serotonergic antidepressants Ø Behavior therapy Ø Adjunctive antipsychotics, psychosurgery
Post Traumatic Stress Disorder
Posttraumatic Stress Disorder Ø The person was exposed to a traumatic event and both of the following were present: l l The event involved actual or threatened death or serious injury to self or others The person’s response involved intense fear, helplessness or horror Ø Duration of symptoms is >1 month and cause significant distress or impairment in functioning.
PTSD continued Ø The traumatic event is re-experienced via: Ø recurrent recollections of the event, nightmares, flashbacks, intense physiologic distress or physiological reactivity at exposure to cues of the event. Ø Persistent symptoms of increased arousal marked by two or more of the following: Ø sleep difficulty, irritability or anger, difficulty concentrating and hypervigilance.
PTSD Epidemiology Ø 7 -9% of general population Ø 60 -80% of trauma victims Ø 50 -80% of sexual assault victims Ø Increased risk in women, younger people Ø Risk increases with “dose” of trauma, lack of social support, pre-existing psychiatric disorder.

Comorbidities Ø Depression Ø Other anxiety disorders Ø Substance use disorders Ø Somatization Ø Dissociative disorders
Post-traumatic Stress Disorder Etiology Ø Conditioned fear Ø Genetic/familial vulnerability Ø Stress-induced release l norepinephrine, cortisol Ø Autonomic arousal immediately after trauma predicts PTSD

PTSD Treatment Ø Cognitive-behavioral therapy Ø Group therapy Ø Medications stabilizers, – antidepressants, mood beta-blockers, prazosin and gabapentin clonidine,
Social Anxiety Disorder
Social Anxiety Disorder (SAD) Ø Marked fear of one or more social or performance situations. Ø Exposure to the feared situation almost invariably provokes anxiety. Ø The person recognizes the fear is excessive. Ø The avoidance, fear or distress significantly interferes with their routine or function.
SAD epidemiology Ø 12% of general population Ø Age of onset teens; more common in women. Ø Causes significant disability Ø Increased depressive disorders
Social Anxiety Disorder treatment Ø Social skills training, behavior therapy, cognitive therapy. Ø Medication – SSRIs, venlafaxine, MAOIs, benzodiazepines and gabapentin.
Take home points Ø Ø Ø Anxiety disorders are common, common! There are significant comorbid psychiatric conditions associated with anxiety disorders! Screening questions can help identify or rule out diagnoses There are many effective treatments including psychotherapy and psychopharmacology There is a huge amount of suffering associated with anxiety disorders!
 Anxiety disorders def
Anxiety disorders def Icd x anxiety disorders
Icd x anxiety disorders Multipath model of anxiety disorders
Multipath model of anxiety disorders Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Chapter 14 psychological disorders
Chapter 14 psychological disorders Group c personality disorders
Group c personality disorders Chapter 14 psychological disorders
Chapter 14 psychological disorders Psychiatric disorders
Psychiatric disorders Schizoid personality disorder
Schizoid personality disorder Chapter 18 psychological disorders
Chapter 18 psychological disorders Ap psychology chapter 15
Ap psychology chapter 15 Chapter 18 psychological disorders
Chapter 18 psychological disorders It's normal to be normal
It's normal to be normal Who is responsible for providing specialized work footwear?
Who is responsible for providing specialized work footwear? First aid kitchen
First aid kitchen Personal protective equipment in smaw
Personal protective equipment in smaw Sacramento county aps
Sacramento county aps Protective earthing conductor
Protective earthing conductor Safety continuum protective behaviours
Safety continuum protective behaviours Which part of the neuron serves as the protective coating?
Which part of the neuron serves as the protective coating? Personal protective equipment in chemistry laboratory
Personal protective equipment in chemistry laboratory In georgia mandated reporters include
In georgia mandated reporters include Cutin
Cutin Ultimate protection security services
Ultimate protection security services Topical agent definition
Topical agent definition Protective tariff
Protective tariff Meaning of colloidal suspension
Meaning of colloidal suspension Asbestos personal protective equipment
Asbestos personal protective equipment Ppe for plumbers
Ppe for plumbers Tissue is a group of cells having
Tissue is a group of cells having Arti protective regulatory policy
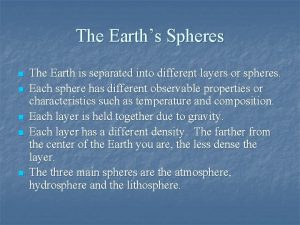
Arti protective regulatory policy Protective ozone layer
Protective ozone layer Maturation stage of amelogenesis
Maturation stage of amelogenesis Integrated protective services
Integrated protective services Effect of electrolytes on colloidal dispersion
Effect of electrolytes on colloidal dispersion Protective do brasil
Protective do brasil Protective ozone layer
Protective ozone layer Maintain your assigned protective mask
Maintain your assigned protective mask Packing learning objectives
Packing learning objectives Personal protective equipment pictograms
Personal protective equipment pictograms Personal protective factor
Personal protective factor Protective packaging and materials handling
Protective packaging and materials handling Personal protective equipment vocabulary
Personal protective equipment vocabulary Rowan county dss
Rowan county dss Larimer county child protective services
Larimer county child protective services V
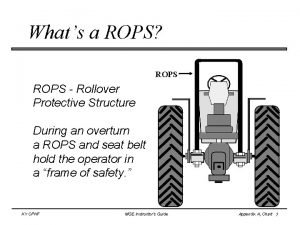
V Roll over protective structure (rops)
Roll over protective structure (rops) Wv adult protective services
Wv adult protective services Protective custom choice
Protective custom choice Protective tariff
Protective tariff Caldwell county dss
Caldwell county dss