Antiviral Drugs Dr Yasmine Ibrahim Assistant professor in

Antiviral Drugs Dr. Yasmine Ibrahim Assistant professor in Pharmacology Department, Minia University
Learning Objectives At the end of the lecture, students must be able to : • To classify major drug groups and specific examples of drugs for the viral infections (Herpes, HBV, HCV and influenza). • To describe the mechanism of action of antiviral drugs including their pharmacological actions, important pharmacokinetic parameters, interactions and dosing.
Introduction • A virus is an obligate intracellular organism that depends up on the host cell to maintain its metabolic function and activity. Therefore, drugs that negatively impact on a virus are also likely to negatively impact normal pathways of the host.
Lecture outlines 1. Introduction to viral replication (recall) 2. Drugs used for hepatitis B and C infection 3. Drugs used for anti-herpes therapy 4. Drugs used for influenza
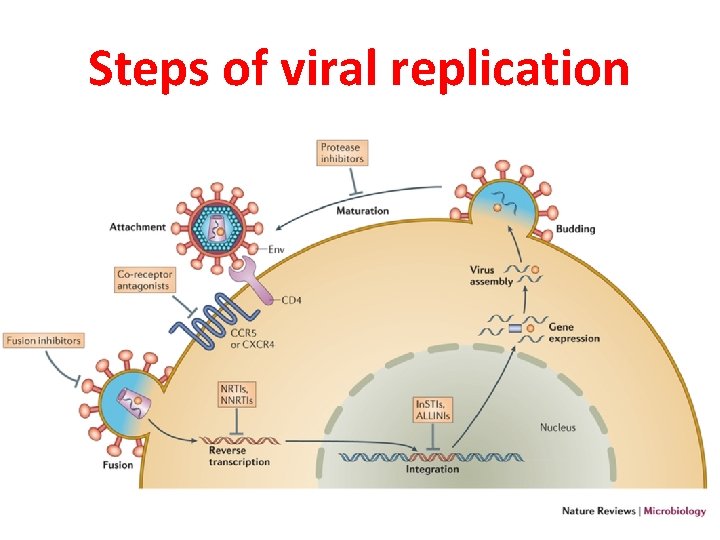
Steps of viral replication
Anti-viral agents (1) Drugs used for hepatitis infection.
The goals of chronic HBV therapy • To sustain suppression of HBV replication, resulting in slowing of progression of hepatic disease(with retardation of hepatic fibrosis and even reversal of cirrhosis), • To prevent complications (i. e, cirrhosis, hepatic failure, and hepatocellular carcinoma), and • To reduce the need for liver transplantation.
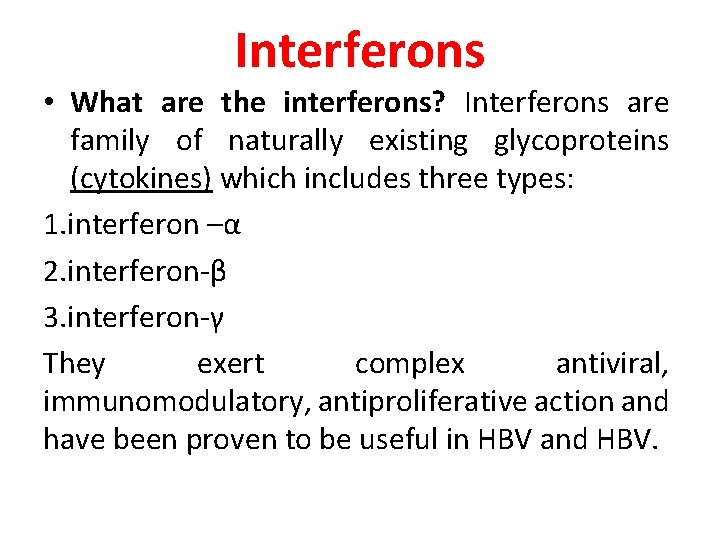
Interferons • What are the interferons? Interferons are family of naturally existing glycoproteins (cytokines) which includes three types: 1. interferon –α 2. interferon-β 3. interferon-γ They exert complex antiviral, immunomodulatory, antiproliferative action and have been proven to be useful in HBV and HBV.
Pharmacology of interferon • MOC • The exact mechanism is unknown. • However, it binds to specific cell receptor and initiates intracellular signaling resulting in induction of host cell enzymes and cytokines leading to: • Inhibition of viral penetration, genome replication, viral maturation, and release. • It also enhances the phagocytic activity of macrophages, and augments the activity of cytotoxic T cells.
Pharmacokinetics of interferon • Interferon – α is not absorbed orally and given by I. M. or S. C. routes. • Cellular uptake and metabolism by renal and liver account for disappearance of interferon from plasma. • Renal elimination accounts for 30%.
Adverse drug reactions • Flu-like symptoms: CNS side effects: Mood disorders, depression, confusion, seizures. • Bone marrow depression • Profound fatigue • Weight loss • Cough • Alopecia • Tennitus and reversible hearing loss • Induction of autoantibodies leading to thyroid dysfunction and autoimmune disturbances. • Cardiotoxicity
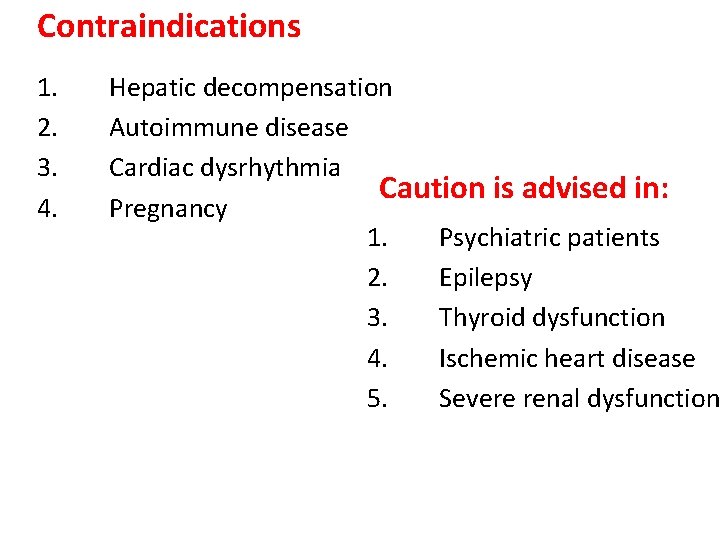
Contraindications 1. 2. 3. 4. Hepatic decompensation Autoimmune disease Cardiac dysrhythmia Caution is advised in: Pregnancy 1. Psychiatric patients 2. Epilepsy 3. Thyroid dysfunction 4. Ischemic heart disease 5. Severe renal dysfunction
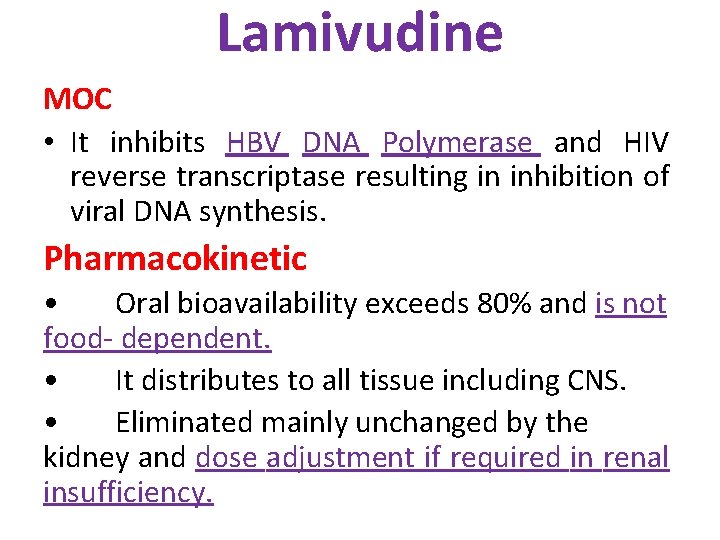
Lamivudine MOC • It inhibits HBV DNA Polymerase and HIV reverse transcriptase resulting in inhibition of viral DNA synthesis. Pharmacokinetic • Oral bioavailability exceeds 80% and is not food- dependent. • It distributes to all tissue including CNS. • Eliminated mainly unchanged by the kidney and dose adjustment if required in renal insufficiency.
Lamivudine Adverse effects • GIT discomfort. • Headache, insomnia, fatigue.
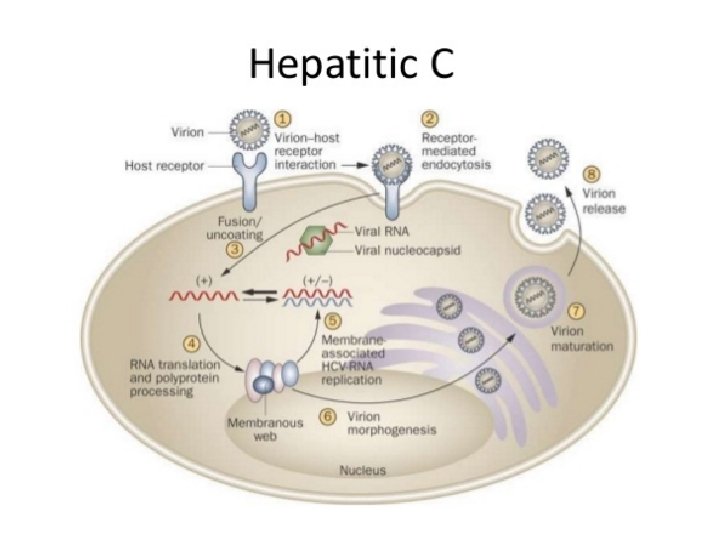
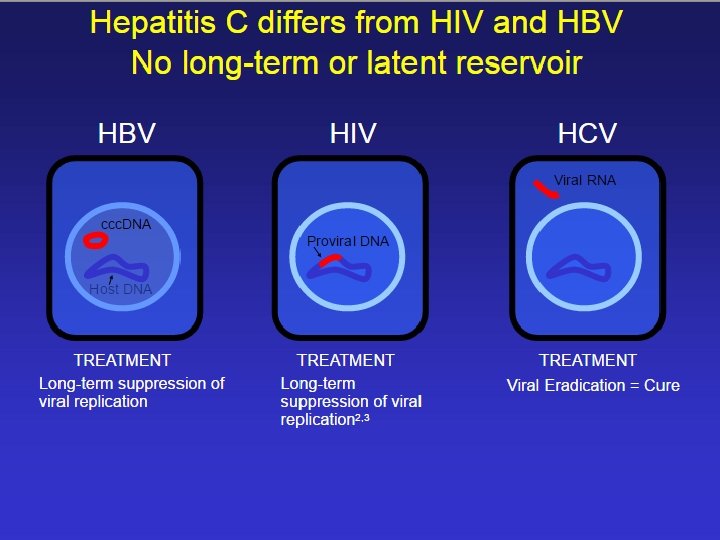
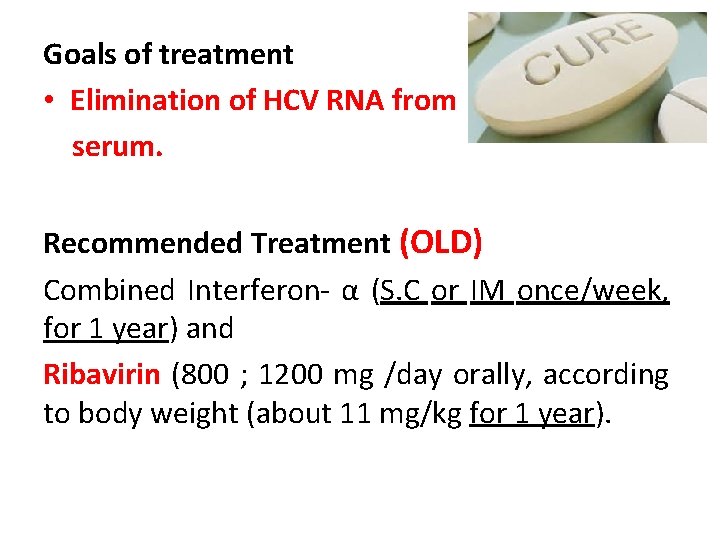
Goals of treatment • Elimination of HCV RNA from serum. Recommended Treatment (OLD) Combined Interferon- α (S. C or IM once/week, for 1 year) and Ribavirin (800 ; 1200 mg /day orally, according to body weight (about 11 mg/kg for 1 year).
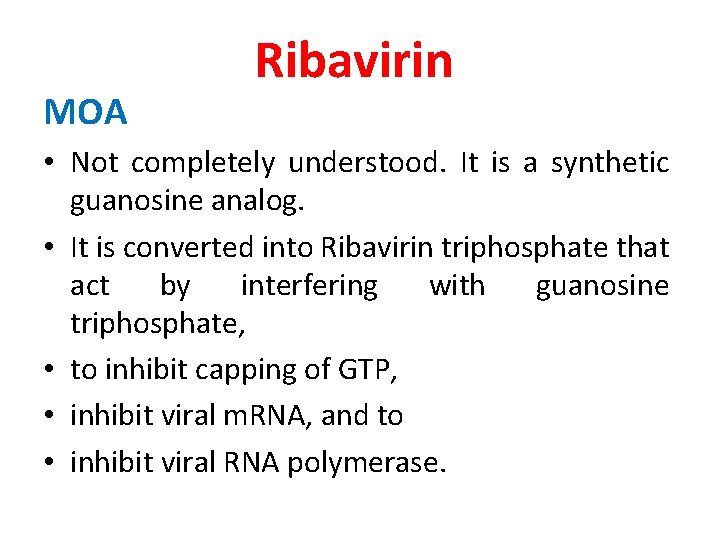
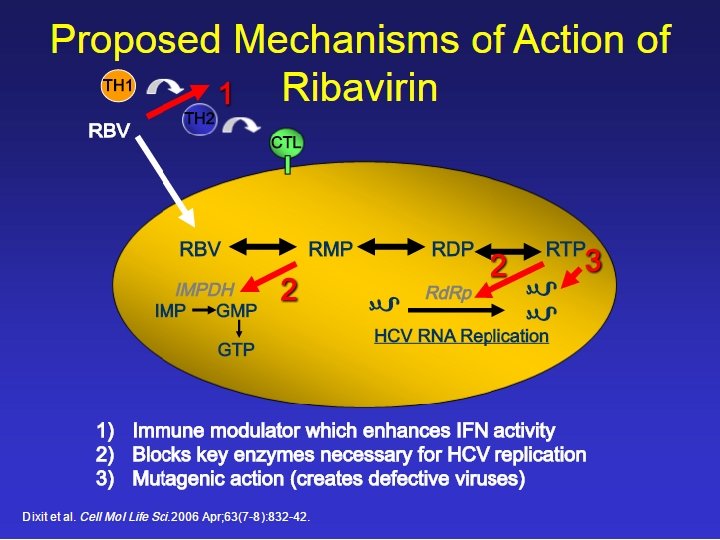
MOA Ribavirin • Not completely understood. It is a synthetic guanosine analog. • It is converted into Ribavirin triphosphate that act by interfering with guanosine triphosphate, • to inhibit capping of GTP, • inhibit viral m. RNA, and to • inhibit viral RNA polymerase.
Pharmacokinetics • Absorbed orally, F = 64%, increase with fatty meal and decrease with antacids. • Eliminated mainly through renal route and dose adjustment is required in renal insufficiency. Adverse effects 1 - Dose-dependent hemolytic anemia (10 -20%). 2 - Other side effects: depression , fatigue, insomnia, dry cough, pruritus, 3. It has teratogenic effect
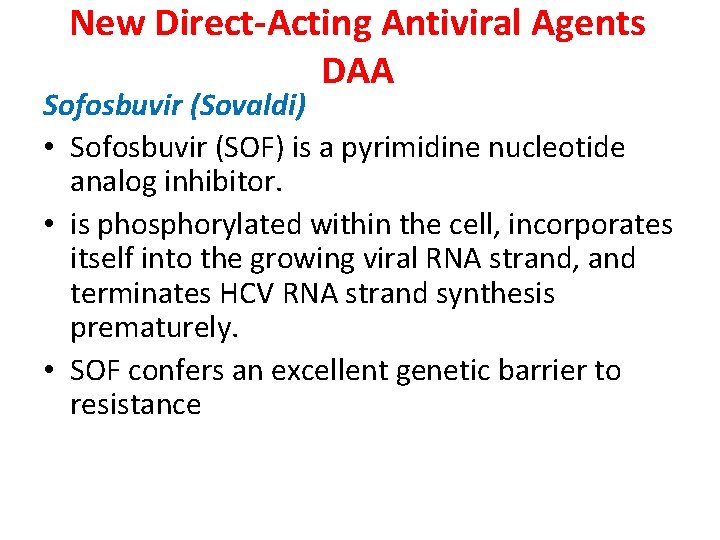
New Direct-Acting Antiviral Agents DAA Sofosbuvir (Sovaldi) • Sofosbuvir (SOF) is a pyrimidine nucleotide analog inhibitor. • is phosphorylated within the cell, incorporates itself into the growing viral RNA strand, and terminates HCV RNA strand synthesis prematurely. • SOF confers an excellent genetic barrier to resistance
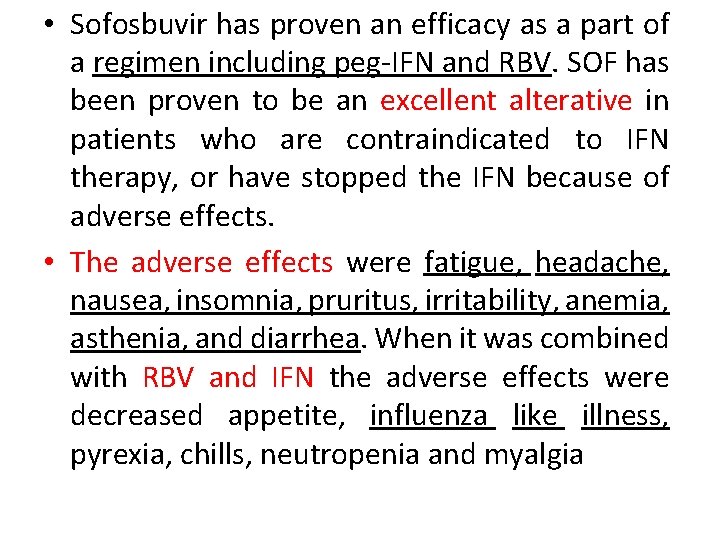
• Sofosbuvir has proven an efficacy as a part of a regimen including peg-IFN and RBV. SOF has been proven to be an excellent alterative in patients who are contraindicated to IFN therapy, or have stopped the IFN because of adverse effects. • The adverse effects were fatigue, headache, nausea, insomnia, pruritus, irritability, anemia, asthenia, and diarrhea. When it was combined with RBV and IFN the adverse effects were decreased appetite, influenza like illness, pyrexia, chills, neutropenia and myalgia
Anti-viral agents 2) Anti-herpes agents

Drugs used as anti-herpes (simplex and zoster)& varicella -zoster virus agent • Acyclovir • Valacyclovir • Famciclovir • Foscarnet • Idoxuridine
Acyclovir • MOA – Activation – Inhibition of viral DNA synthesis • Activation • Acyclovir requires three phosphorylation steps for activation. • It is converted first to the monophosphate derivative by the virus specific thymidine kinase and then to the di- and triphosphate compounds by host cell enzymes.
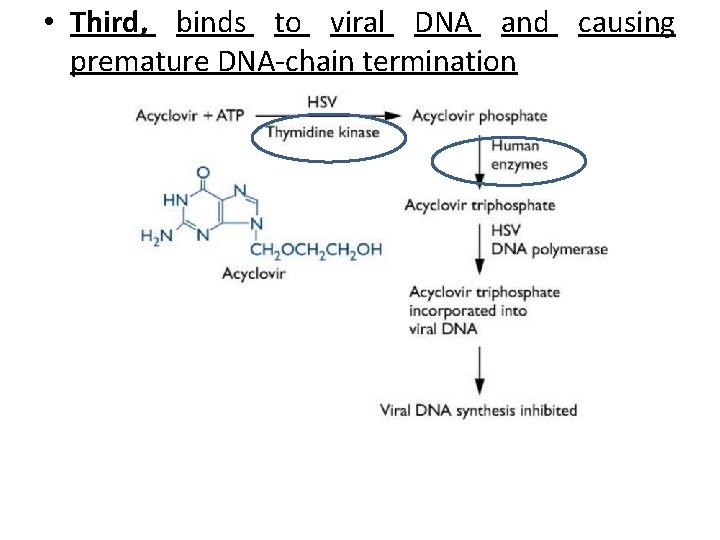
• Third, binds to viral DNA and causing premature DNA-chain termination
Selective toxicity • Because it requires the viral kinase for initial phosphorylation, acyclovir is selectively activated—and the active metabolite accumulates only in infected cells. • Absorbed orally, distributed widely including CSF. Adverse effect • Topically: local irritation • Oral: diarrhea, headache • I. V: Phelebitis, renal toxicity; neruotoxicity
Treatment of Respiratory Virus infection • The first line therapy of influenza A in immunization using Influenza A vaccine. • Drugs used in treatment of respiratory virus are: 1 - Inhibitors of Uncoating (Amantadine and rimantadine) 2 - Neuroaminidase inhibitors (Zanamivir and oseltamivir(Tamiflu)) 3 - Ribavirin (see before)

Amantadine and rimantadine Mechanism of action Interfere with viral uncoating and release of genetic material inside the host cell
Pharmacokinetics • Both are almost completely absorbed orally. • Amantadine distributes to CSF while rimantadine is not. Clinical uses § Prophylactic and treatment of influenza A virus § Amantadine is used in parkinsonism? ? ? Adverse effects § CNS (insomnia, nervousness, confusion, convulsions). This side effect is more common with amantidine. Why? ? ?
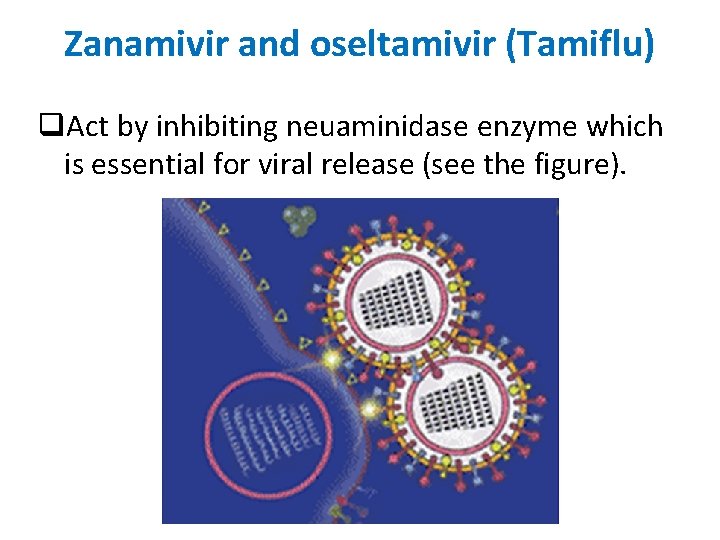
Zanamivir and oseltamivir (Tamiflu) q. Act by inhibiting neuaminidase enzyme which is essential for viral release (see the figure).
q. They do not interfere with the immune response to influenza vaccine. q. They are active against type A and B viruses. q. They prevent the infection if administered before infection. Administration within 48 hours of infection moderately affect the course of infection. q. Both drugs are eliminated unchanged in urine. q. Zanamivir is given intranasal and may cause respiratory irritation. q. Oseltamivir is a prodrug and is given orally and can cause GIT irritation.
Lecture outlines 1. Introduction to viral replication (recall) 2. Drugs used for hepatitis B and C infection 3. Drugs used for anti-herpes therapy 4. Drugs used for influenza

THANK YOU
- Slides: 37