Antipartum hemorrhage APH Bleeding from or into genital
Antipartum hemorrhage (APH)
• Bleeding from or into genital tract occurring from 24 weeks of pregnancy and prior to the birth of the baby. • Affects 3 -5% of pregnancies. • It’s the leading cause of maternal morbidity and prenatal mortality ( mainly due prematurity ) • Obstetric hemorrhage remains one of the major causes of maternal death in the developing countries.
• 50% of estimated 500, 000 maternal deaths occurring globally per year. • Fifth of very preterm babies are born in association with APH. • APH has a heterogeneous pathophysiology and can’t be predicted. (70% of cases of abruptio placenta occur in low-risk pregnancies )

• There is no consistent definition of the severity of APH(often underestimated) Following definitions have been used : 1 -spotting: staining, streaking, spotting 2 -minor hemorrhage <50 ml 3 - major hemorrhage : 50 -1000 ml with no signs of clinical shock 4 - massive : more than 1000 ml and/or signs of clinical shock
Causes: 1 -placenta previa 2 -placenta abruption 3 -local causes (cervical or vaginal lesions, cancer, infections or lacerations) 4 -vasa previa 5 -uterine rupture -unexplained (high risk pregnancy SGA, RRO. M, PTL, IUGR, C/S)
• Management: in the hospital maternity unity with facilities for resuscitation such as: 1 -anesthetic support 2 -blood transfusion resources 3 -performing emergency operative delivery 4 -multi disciplinary team including: Midwifery, obstetric staff, neonatal staff, anesthetic staff, hematologist, radiologist and vascular surgeon.
• Investigations: CBC, RFT, LFT, Coagulation factors, blood grouping, Rh. ABCD : A, B AIRWAY and breathing oxygen 10 -15 L/min C: Circulation: two large bore cannulas. 14 gauge IV lines. D: asses fetus and decide delivery -Clinical Examinations -No vaginal digital examination , speculum examination should be done to rule out local causes. u/s to diagnose placenta previa
• Steroids can be given if pregnancy < 34 weeks for fetal lung maturity. • Tocolysis shouldn’t be used in (unstable patient, fetal compromise, major APH) • It’s a decision of a senior obstetrician. • Avoid nifedipine (HYPOTENSION) • Anti DIg should be given to all non sensitized RH-ve if they have APH. At least 500 IU anti. DIg followed by a test of FMH if it's more than 40 ml of RBC additional Anti D required. • Anti D Ig should be given at minimum of 6 weeks intervals(in recurrent bleeding) • Risk of PPH: pt should receive active management of 3 rd stage of labor using syntometrine (in absence of high B. P) • Senior consultant anesthetic care needed in high risk hemorrhage.
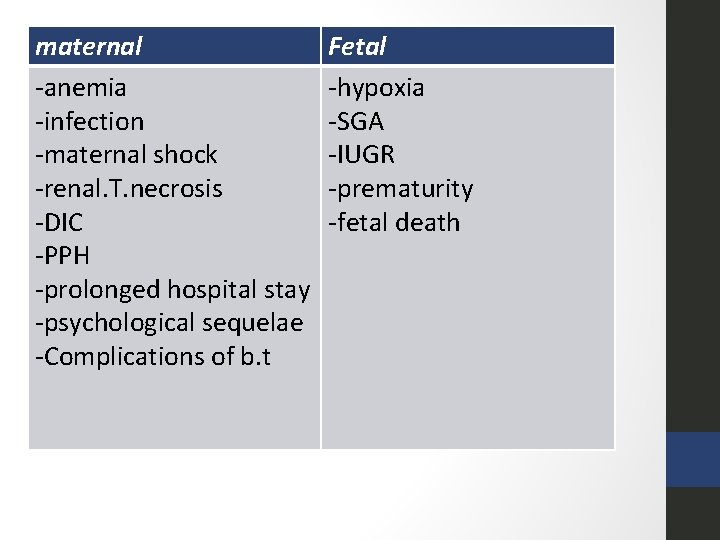
maternal -anemia -infection -maternal shock -renal. T. necrosis -DIC -PPH -prolonged hospital stay -psychological sequelae -Complications of b. t Fetal -hypoxia -SGA -IUGR -prematurity -fetal death
- Slides: 9