Antiepileptic Drugs By Imad M Taj Eldin Faculty
ﺑﺴﻢ ﺍﻟﻠﻪ ﺍﻟﺮﺣﻤﻦ ﺍﻟﺮﺣﻴﻢ Antiepileptic Drugs By Imad M. Taj Eldin Faculty of Pharmacy
Definitions • Epilepsy is a chronic CNS disease • It is very common disorder, affecting 0. 5 -1% of the population. • The characteristic event in epilepsy is the seizure, which is associated with the episodic high frequency discharge of impulses by a group of neurons in the brain. • In epilepsy certain neurons and group of neurons become hyperexcitable and begin firing bursts of action potentials that propagate in a synchronous manner to other brains structures. Seizure • Seizure is state produced by abnormal excessive neuronal discharge within the gray matter that is always associated with abnormal electroencephalogram (EEG) activity
Definitions Convulsion • Convulsion: is violent involuntary contraction or series of contractions of the voluntary muscles. • There are three types of involuntary movement: ØTonic movement (sustained contractions). ØClonic (alternating contractions and relaxations occurring in rapid succession) ØMyoclonus movement (brief contraction of a portion of a muscle).
Definitions Epilepsy • Epilepsy is a general term for a group of diverse CNS disorders characterized by: ØRepeated spontaneous occurrence of brief convulsive or nonconvulsive seizures. ØAbnormal and excessive EEG activity. ØPossibly loss or disturbance of consciousness. ØPossibly psychic phenomenon. ØOccasionally autonomic hyperactivity.
Etiology of Epilepsy The cause of the seizure and epilepsy disorder is not known (idiopathic epilepsy), but it may be due to: Ø Trauma during the birth process. Ø Head trauma Ø Meningitis Ø Brain tumors Ø Childhood fever Ø As a toxic manifestation of the action of CNS stimulants Ø Eclampsia Ø Uremia Ø Hypoglycemia Ø Cerebral circulation or neurological diseases
Types of Epilepsy • The agreed clinical classification of epilepsy recognizes two categories namely partial and generalized seizures. The partial seizure • The partial seizure could be simple (of localized discharge in which consciousness is unaltered), complex or partial seizures evoking to secondary generalized seizures 1. Simple Partial Seizure: its major clinical manifestations are: ØMay be limited to a single limb. Ø May show sequential involvement of body parts. ØConsciousness usually preserved. ØMay have autonomic signs and symptoms e. g. sweating and pupillary dilatation …etc.
Types of Epilepsy 2. Complex partial seizure: its major clinical manifestations are: ØImpairment of consciousness ØMay have autonomic activity e. g. urination, salivation, flushing. . . etc 3. Partial seizure evoking to secondary generalized. Its major clinical manifestations are: ØMay generalize to tonic, clonic or tonic-clonic.
Types of Epilepsy Generalized Seizure 1. Absence seizure (petitmal). Its major clinical manifestations are: ØBrief loss of consciousness (lasts 10– 45 sec) with or without motor involvement ØOccurs in childhood with a tendency to following adolescence. 2. Myoclonic seizure. Its major clinical manifestations are: ØSudden, brief, shock like contraction of musculature (myoclonic jerks). 3. Tonic-clonic (Grandmal). • Clonic: Repetitive muscle jerks. • Tonic: Rigid, violent muscular contraction with limb fixed. Characterized by: Ø Loss of consciousness, Ø Sudden sharp tonic contractions of muscles, Ø Falling to ground, Ø Following by clonic convulsive movement and autonomic symptoms.
Types of Epilepsy 5. Atonic (Astatic) • Its major clinical manifestations are: ØSudden diminution in muscle tone affecting isolated muscle groups or loss of all muscle tone. ØMay have brief loss of consciousness. 6. Status epilepticus • It is prolonged seizure (>20 min) of any of the types previously described. • Status epilepticus is a continuous seizure state that can be fatal unless the convulsions are terminated. • It is a leading cause of death in epileptic patients and must be considered a medical emergency.
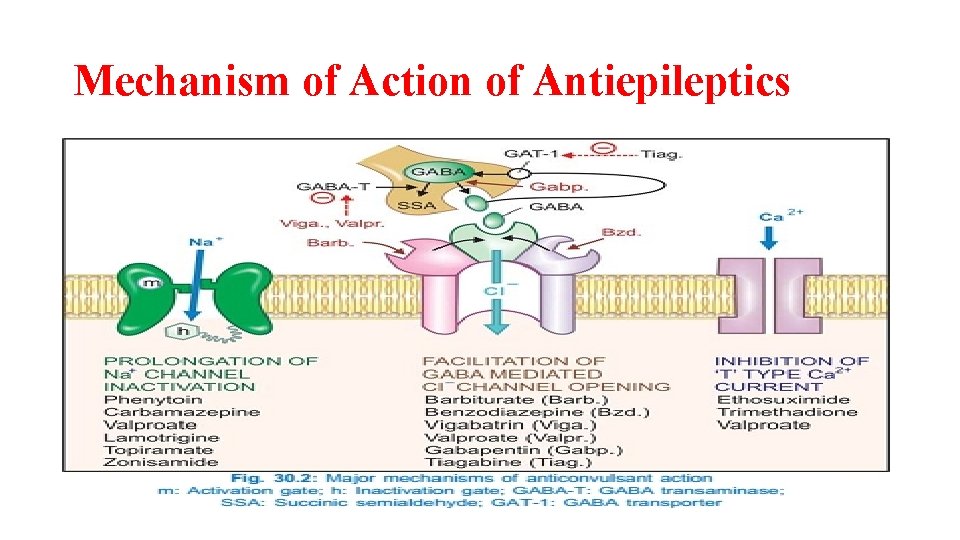
Mechanism of Action of Antiepileptics There are several mechanisms for antiepileptic drugs to exert their anticonvulsant effects: ØInhibition of sodium channel function. ØInhibition of T-type calcium channels. ØEnhancement of GABA action. ØReduction of excitatory glutamatergic neurotransmission.
Mechanism of Action of Antiepileptics
Classification of Antiepileptics The anticonvulsants are categorized by their mechanism of action into the following groups: • Type I: Sodium channels blocking agents e. g. phenytoin , carbamazepine, oxycarbamazepine, lamotrigine, and felbamate. ØTheir mechanism of action depends on blocking sodium channels and inhibit the generation of action potentials. • Type II: Drugs with multiple actions e. g. are valproic acid (sodium valproate), benzodiazepines, barbiturates, and primidone. • Their mechanism of action depends on: Ø Enhancement of GABAergic inhibition Ø Reduces T-type calcium currents and Ø Possibly blocks sodium channels.
Classification of Antiepileptics • Type III: Drugs that block the T-type of calcium channels only. Examples are ethosuximide and trimethadione. • Type IV: Drugs that enhance GABAergic inhibition only, e. g. vigabatrin and Tiagabine. • Miscellaneous drugs: e. g. , levetiracetam and lacosamide are anticonvulsant agents, which are not categorized because their mechanism of action is unknown.
Sodium Channel Blocking Agents • These are phenytoin, carbamazepine, lamotrigine, and felbamate. • These agents are similar to each other in pharmacological properties, clinical indications for epilepsy treatment and their presumed mechanism of action. • They differ from each other in, one drug cannot routinely be substituted for another, pharmacokinetic properties, adverse effects, their interaction with other drugs and their chemical structures. Mechanism of Action • They block sodium channels and inhibit the generation of action potentials • Their effect is “use dependent, ” that is, related to their selective binding and prolongation of the inactivated state of the sodium channel. • They also decrease neurotransmission by actions on presynaptic neurons.
Sodium Channel Blocking Agents Phenytoin is a valuable agent for treatment of: ØGeneralized tonic-clonic seizures and for the treatment of partial seizures with complex symptomatology. ØDisturbed psychotic patients without epilepsy. ØTrigeminal neuralgia. ØUseful as an antiarrhythmic agent, particularly in the treatment of digitalis induce arrhythmia. ØStatus epilepticus
Pharmacokinetics of Phenytoin • The absorption of phenytoin is slow and takes place primarily in the duodenum. • Simultaneous ingestion of antacid significantly decreases the absorption of phenytoin. • About 80%-90 bound to albumin. • Other drugs such as salicylates, valproic acid, thyroxin and phenylbutazone inhibit this binding to plasma proteins competitively. • Thus increases the free phenytoin concentration. • Phenytoin is metabolized by hepatic mixed function oxidase system and excreted mainly as glucuronide. • It causes induction of the liver metabolizing enzymes, and thus increases the rate of metabolism of other drugs (e. g. oral anticoagulants).
Side Effects of Phenytoin • Side effects include vertigo, ataxia, headache, nystagmus, but not sedation. • The most common chronic side effects of phenytoin in children are gingival hyperplasia, or overgrowth of the gums. • Hirsutism is a side effect in young females. • Hirsutism, result from increased androgen secretion. • Enlargement of lips and nose. • Megaloblastic anemia, due to a disorder of folate (folic acid) metabolism, and can be corrected by giving folic acid. • Phenytoin has idiosyncratic and teratogenic effects. • Idiosyncratic reactions include hypersensitivity, hepatitis and skin reactions. • Phenytoin also can cause an increased incidence of fetal malformations in children born to epileptic mothers, particularly the cleft palate and abnormal growth and development
Drug Interactions of Phenytoin • Phenytoin affected by either induction or inhibition of microsomal drug-metabolizing enzymes or alteration in drug plasma binding. • Plasma levels of phenytoin can be elevated by cimetidine, chloramphenicol, disulfiram, and isoniazid (liver enzymes inhibitors). • Phenytoin stimulates hepatic metabolism, by liver enzyme induction. • This often causes a decline in plasma concentration of carbamazepine and quinidine if they are given concomitantly. • Antacids should not be given close to the time that phenytoin is ingested, since they decrease the absorption of phenytoin. • Fosphenytoin is a new related drug, used only parenterally for status epilepticus.
Sodium Channel Blocking Agents Carbamazepine Clinical uses of Carbamazepine • Carbamazepine is an effective drug for the treatment of: ØPartial seizures and generalized tonic-clonic seizures. ØTrigeminal neuralgia. ØBipolar depression. • Pharmacokinetics: Carbamazepine is slowly absorbed. • Carbamazepine is a liver enzyme inducer and can induce its own metabolism (autoinduction) after prolonged administration. • Carbamazepine also can induce the enzymes that metabolize other anticonvulsant drugs including phenytoin, ethosuximide, primidone, phenobarbitone, clonazepine and valproic acid, as well as metabolism of other drugs that the patient may be taken.
Pharmacokinetics &Interactions of Carbamazepine • Similarly, other drugs may induce the metabolism of carbamazepine and the dose of carbamazepine must be adjusted. Interactions of Carbamazepine • A common drug-drug interaction, between carbamazepine and macrolide antibiotic (e. g. erythromycin). • After a few days of antibiotic therapy, symptoms of carbamazepine toxicity develop? ? ? • Erythromycin is a liver enzyme inhibitor • Cimetidine, propoxyphene and isoniazid also have been reported to inhibit the metabolism of carbamazepine
Adverse Effects of Carbamazepine • Drowsiness is the most common side effect, followed by nausea, headache, dizziness, incoordination, vertigo and diplopia. • It causes a variety of rashes and other allergic reactions including fever, hepatosplenomegaly and lymphadenopathy. • Agranulocytosis can occur in some patients. • It is important to note that the severe adverse reactions occur less commonly than phenytoin.
Sodium Channel Blocking Agents Lamotrigine • Lamotrigine will not inhibit or induce cytochrome P 450 isoenzymes, in contrast to most antiepileptic drugs ØIt is proved effective in treatment of: ØPartial seizures, and ØIn generalized tonic-clonic epilepsy. • The adverse effects are similar to that of other drugs with the same mechanism of action (dizziness, diplopia, headache, ataxia, and rash) Felbamate and Zonisamide • Felbamate use is very limited due to development of aplastic anemia (1: 3, 000) and severe hepatitis with liver failure (1: 10, 000). • Zonisamide acts at the sodium channel and possibly the voltagedependent calcium channel. • Adverse effects include drowsiness, confusion, and rashes.
Drugs with Multiple Actions Primidone and Phenobarbitone Mechanism of action • The anticonvulsant activity of primidone is due to its conversion in the body to phenobarbitone. • The mechanism of action of phenobarbitone is related to: ØIts effect on facilitating GABA inhibition. Phenobarbitone enhances GABA’s inhibitory activity by prolonging the opening of chloride channels. ØAt somewhat higher concentrations, phenobarbitone can block sodium channels and may block excitatory glutamate response.
Pharmacokinetics of Primidone • Primidone is metabolized by microsomal drug metabolizing enzymes and is excreted unchanged by the kidney. • It is metabolized to phenobarbitone and phenylethylmalonamide (PEMA). • The phenylethylmalonamide has anticonvulsant activity, but most of the anticonvulsant of primidone is due to the phenobarbitone that is produced. • Phenobarbitone may initially inhibit the metabolism of other drugs, presumably by competitive inhibition of microsomal enzymes. • This may be followed by an enhanced metabolism as a result of enzyme induction.
Clinical Uses Primidone and phenobarbitone • Phenobarbitone and primidone are alternative drugs for: ØThe treatment of partial seizures and generalized tonic-clonic epilepsy. ØPhenobarbitone is also used to treat febrile convulsions in children (considered by some physicians to be the drug of choice). ØThey are less effective than carbamazepine and phenytoin.
Drugs with Multiple Actions Valproic Acid Mechanism of action This compound has broad anticonvulsant activity: ØValproic acid has been shown to block voltage-dependent sodium channels. ØIt may cause an increase in brain GABA. ØIt increases the concentration of GABA within the brain by stimulating glutamic acid decarboxylase activity (increase GABA synthesis) and inhibiting GABA aminotransaminase (decrease GABA breakdown). ØIt may activate calcium-dependent potassium conductance (not clear mechanism).
Pharmacokinetics of Valproic Acid • Valproic acid inhibits the metabolism of several drugs, including, phenobarbitone, primidone, carbamazepine and phenytoin. • It can also enhance its own metabolism at higher doses. • Valproic acid also can displace phenytoin from binding sites on plasma proteins resulting in free phenytoin and toxicity. • It is metabolized to several metabolites (these metabolites are toxic to the liver).
Clinical Uses of Valproic Acid Valproic acid has been used against several seizure types: ØIt is highly effective against absence seizure and myoclonic seizures. ØCan be used either alone or in combination with other drugs for the treatment of generalized tonic-clonic epilepsy and for partial seizures with complex symptomatology. ØIn treatment of mania and ØAs a prophylactic agent for migraine headaches.
Adverse Effects of Valproic Acid • The most serious adverse effect is hepatic failure resulting in fatality. • Fatal hepatotoxicity is much more likely to occur in children under the age of 2 years. • Patients taking valproate may develop clotting abnormalities due to inhibition of vitamin K. • Valproic acid causes reversible hair loss (alopecia). • Hyperglycemia, hyperglycinuria, and hyperammonemia. • An increase in body weight. • G. I. T disturbances (nausea, vomiting and anorexia) • Sedation, ataxia and dizziness,
Drugs with Multiple Actions Benzodiazepines • They interact with the GABAA receptors at the benzodiazepines binding site (BZ receptors) to enhance inhibition. • Also they block voltage-dependent sodium channels. • Their major use in the treatment of absence, myoclonic, and atonic seizures and in the emergency treatment of status epilepticus. • Clonazepam is a very potent anticonvulsant activity. • Side effects: Sedation and tolerance tend to limit its usefulness. • Drooling and hypersalivation may be troublesome in children and infants.
Drugs with Multiple Actions Benzodiazepines • Diazepam is the drug of choice for the emergency treatment of status epilepticus • Also used for serial seizures, prolonged seizures, and the prophylaxis of febrile seizures. • There are other benzodiazepines that have been used as antiepileptics e. g. lorazepam, nitrazepam
Drugs That Block T-type Calcium Channel Ethosuximide • The mechanism of action may be due to its ability, to reduce the lowthreshold calcium current (LTCC or T-current). • Clinical uses: The only clinical use for ethosuximide is in the treatment of absence epilepsy. • Adverse effects: Ethosuximide is a safe drug. • Most of the side effects are dose-related and consist of nausea, gastrointestinal irritation, drowsiness and anorexia. Trimethadione • Because of its toxicity its use is restricted to patients who are inadequately controlled by or do not tolerate other agents. • The mechanism of action is similar to that of ethosuximide. • The most common adverse effects are sedation and severe teratogenic effects.
Drugs That Enhance GABAergic Action • These are Vigabatrin, Tiagabine and Topiramate Vigabatrin • Vigabatrin is an irreversible inhibitor of GABA-transaminase; the major enzyme responsible for the metabolism of GABA in the CNS, so increases GABA in the brain • The primary indication for vigabatrin is in patients with partial seizures. • The adverse effects are mild: include drowsiness, irritability, nervousness, dizziness, headache. • The most serious is visual field defects. • There is no metabolism of vigabatrin in the liver.
Drugs That Enhance GABAergic Action Tiagabine • Tiagabine, an analogue of GABA ØMechanism of action: It is able to penetrate the blood-brain barrier, acts by inhibiting GABA reuptake ØIt enhances the extracellular GABA concentration, and also potentiates and prolongs GABA-mediated synaptic responses in the brain. • The main side effects are drowsiness and confusion. • It is metabolized in the liver to inactive metabolites • Uses: Tiagabine is mainly indicated for partial seizures.
Drugs That Enhance GABAergic Action Topiramate • Topiramate is a recently introduced drug, which, mechanistically, appears to do a little of every thing, blocking sodium channels, enhancing the action of GABA, blocking AMPA receptors and inhibiting carbonic anhydrase. • Its main drawback is that, it is teratogenic and should not be used in women of child-bearing age. ØUses: Currently, it is recommended for use as add-on therapy in refractory cases of epilepsy. ØTopiramate is used in partial seizures and generalized tonicclonic seizures.
Drugs That Enhance GABAergic Action Gabapentin • Gabapentin was initially designed to be a rigid analogue of GABA. • The exact mechanism is not yet known. • Gabapentin, among other activities, increases GABA levels in the brain. • Gabapentin is absorbed satisfactorily orally. • Gabapentin is not protein bound. • Gabapentin does not appear to be metabolized. • It has short-half life and may require three times per day dosing. • Gabapentin is recommended as adjunctive therapy in the treatment of partial seizures in adults.
Pregabalin • Pregabalin, an analog of gabapentin, is used as adjunctive therapy for partial seizures. • Mechanism of action: It binds to voltage-gated calcium channels and reduces release of excitatory neurotransmitters. • Its major adverse effects are dizziness, dry mouth, blurred vision, and weight gain. • Gabapentin and pregabalin are also used to treat postherpeutic neuralgia, and diabetic peripheral neuropathy. • Pregabalin is used to treat fibromyalgia.
Levetiracetam and Lacosamide • Levetiracetam acts by an unknown mechanism. • It is used as adjunctive therapy to treat partial and generalized tonic–clonic seizures and for myoclonic seizures. • Its adverse actions include dizziness. It may cause behavioral changes. • Lacosamide acts by an undetermined mechanism. • It is used as adjunctive therapy to treat partial seizures. • Adverse effects include diplopia, dizziness, GI disturbances, and headache.
Ezogabine and Rufinamide • Ezogabine increases potassium channel opening. • It is used as adjunctive therapy to treat partial seizures. • Its adverse effects include blurred vision, confusion, and bladder dysfunction. • Rufinamide acts like phenytoin and carbamazepine. ? ? ? • It is used as adjunctive therapy to treat Lennox-Gastaut syndrome. • Its adverse effects include vomiting, diarrhea, and sedation.
Antiepileptics and Pregnancy • Most anticonvulsant drugs can cause developmental fetal abnormalities in human e. g. cleft palate. • Trimethadione should not be given to women who are pregnant, since it is clearly teratogenic. • Most of antiepileptic drugs cause some degree of folic acid deficiency, and this is associated with abnormal growth and development. • Serious hemorrhagic disorders can occur, since many antiepileptic drugs can act as competitive inhibitors of vitamin K-dependent clotting factors.
Treatment of Febrile Seizure • Convulsion associated with fever generally occurs in children between 3 months to 5 years and later can develop in some of them to epilepsy. • Phenobarbitone is the drug usually employed, although diazepam is also effective. • Phenytoin and carbamazepine are effective and valproic acid may cause hepatotoxicity in very young patients.
Treatment of Status Epilepticus • The pharmacological treatment of choice at present consists of the intravenous infusion of either diazepam or lorazepam, followed by the I. V. administration of phenytoin or general anesthesia • The drug should be administered slowly to avoid respiratory depression and the development of apnea. • After seizures are controlled, appropriate longer-term oral antiepileptic therapy should be initiated.
- Slides: 42