Anticoagulant Management In Ischemic Stroke Mandy Binning MD

Anticoagulant Management In Ischemic Stroke Mandy Binning, MD Nick Hopkins MD Elad Levy MD Adnan Siddiqui MD, Ph. D Dept of Neurosurgery SUNY Buffalo
DISCLOSURES L. Nelson Hopkins, MD Consulting Fees – Abbott Vascular, Bard Peripheral Vascular, Boston Scientific Corporation, Micrus Endovascular Cordis, a Johnson & Johnson company Grants/Contracted Research – Cordis, a Johnson & Johnson company, Boston Scientific Corporation, Micrus Endovascular Honoraria – Access. Closure, Inc. , Bard Peripheral Vascular, Boston Scientific Corporation, Cordis, a Johnson & Johnson company, market. Rx, Inc. , Micrus Endovascular, Medsn Ownership Interest (Stocks, Stock Options or Other Ownership Interest) – APW Holding, Inc. , Boston Scientific Corporation, Magellan Spine Tech, Inc. , Med. Focus Accelerator Fund, Micrus Endovascular
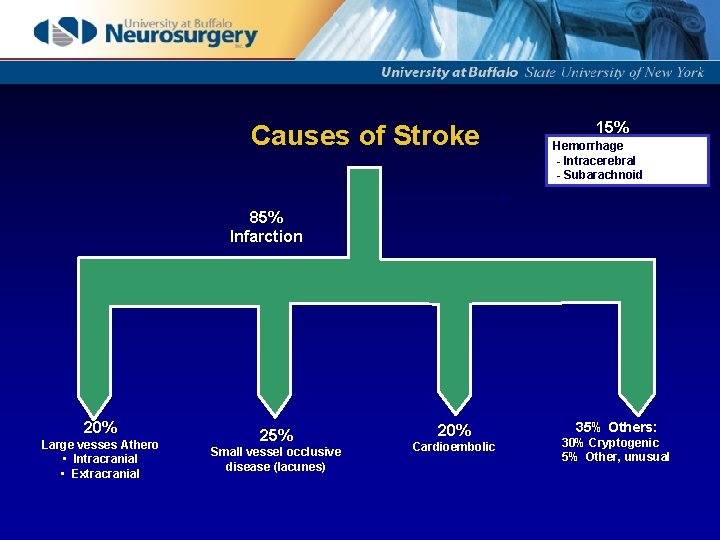
Causes of Stroke 15% Hemorrhage - Intracerebral - Subarachnoid 85% Infarction 20% Large vesses Athero • Intracranial • Extracranial 25% Small vessel occlusive disease (lacunes) 20% Cardioembolic 35% Others: 30% Cryptogenic 5% Other, unusual
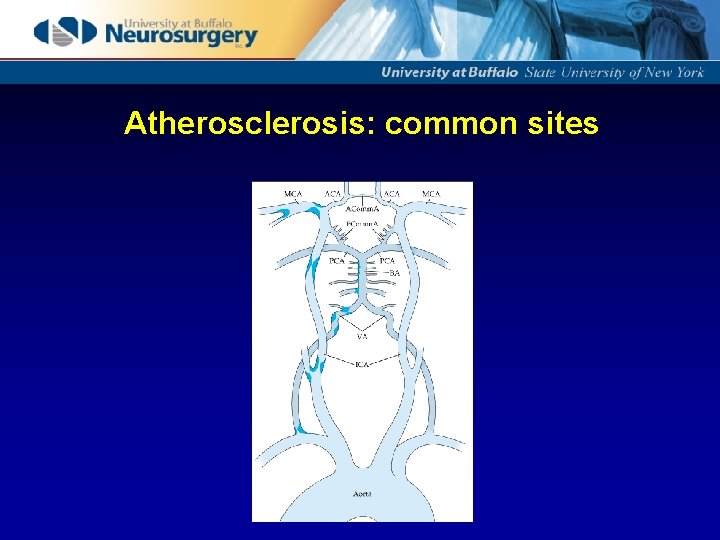
Atherosclerosis: common sites
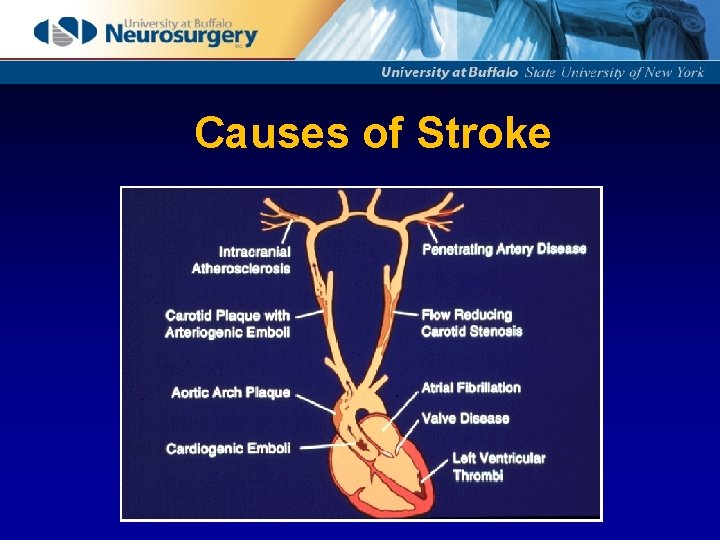
Causes of Stroke
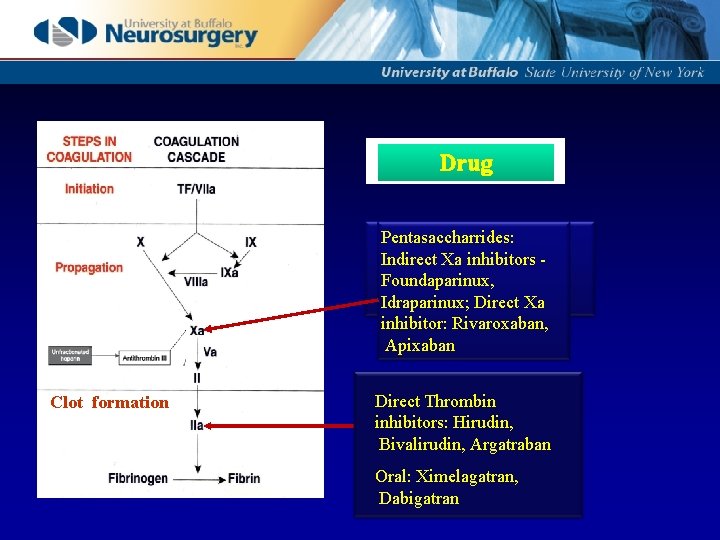
Drug Pentasaccharrides: Indirect Xa inhibitors Foundaparinux, Idraparinux; Direct Xa inhibitor: Rivaroxaban, Apixaban Clot formation Direct Thrombin inhibitors: Hirudin, Bivalirudin, Argatraban Oral: Ximelagatran, Dabigatran
Anticoagulants: Long history of use Usefulness of emergency anticoag in debate Disagreements exist about : • Best agent to administer • Route of administration • Use of a bolus dose to start treatment • Level of anticoagulation • Duration of treatment
Questions • Do antithrombotic agents reduce stroke-related morbidity and mortality? • Do antithrombotic agents reduce early stroke recurrence? • Do antithrombotic agents vary in efficacy according to stroke subtype? Risk of Early Recurrent Embolism about 12% (range 2 -22%) for cardiogenic embolic stroke within 2 weeks if untreated. • Do antithrombotic agents reduce systemic thrombotic complications such as DVT/PE? • What are the risks of hemorrhage associated with antithrombotic treatment?
Do antithrombotic agents reduce stroke -related Morbidity and mortality?
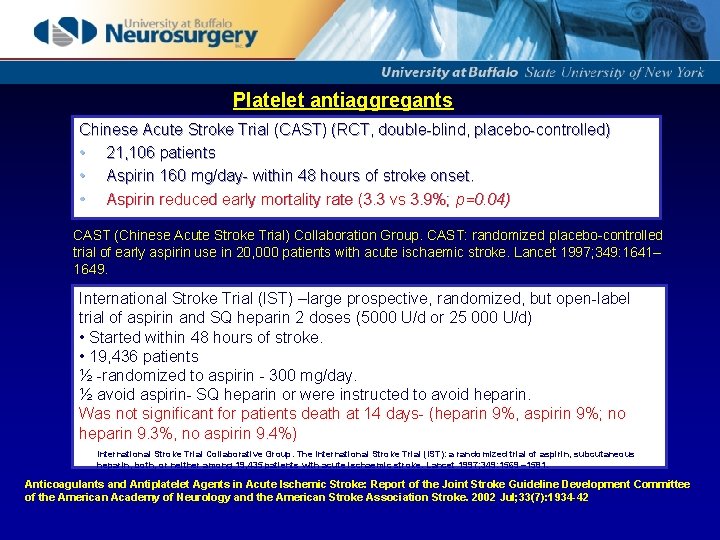
Platelet antiaggregants Chinese Acute Stroke Trial (CAST) (RCT, double-blind, placebo-controlled) • 21, 106 patients • Aspirin 160 mg/day- within 48 hours of stroke onset. • Aspirin reduced early mortality rate (3. 3 vs 3. 9%; p=0. 04) CAST (Chinese Acute Stroke Trial) Collaboration Group. CAST: randomized placebo-controlled trial of early aspirin use in 20, 000 patients with acute ischaemic stroke. Lancet 1997; 349: 1641– 1649. International Stroke Trial (IST) –large prospective, randomized, but open-label trial of aspirin and SQ heparin 2 doses (5000 U/d or 25 000 U/d) • Started within 48 hours of stroke. • 19, 436 patients ½ -randomized to aspirin - 300 mg/day. ½ avoid aspirin- SQ heparin or were instructed to avoid heparin. Was not significant for patients death at 14 days- (heparin 9%, aspirin 9%; no heparin 9. 3%, no aspirin 9. 4%) International Stroke Trial Collaborative Group. The International Stroke Trial (IST): a randomized trial of aspirin, subcutaneous heparin, both, or neither among 19, 435 patients with acute ischaemic stroke. Lancet 1997; 349: 1569 – 1581. Anticoagulants and Antiplatelet Agents in Acute Ischemic Stroke: Report of the Joint Stroke Guideline Development Committee of the American Academy of Neurology and the American Stroke Association Stroke. 2002 Jul; 33(7): 1934 -42
In patients within 48 hours of acute ischemic stroke onset Abciximab, unfractionated heparin LMW heparins Heparinoids Have not been shown to reduce mortality or morbidity. • Most trials have not demonstrated the efficacy of anticoagulation in improving outcomes. • One relatively small trial -IV heparin shoed improve outcomes, when administered within 3 hours of stroke onset in nonlacunar stroke. • In light of the generally negative data, the results of this trial may need to be replicated.
Overall, for aspirin there is a slight but statistically significant benefit in reducing recurrent stroke.
In 48 hours of onset of acute ischemic stroke Heparin, LMW, heparinoids Have not been shown to reduce the rate of stroke recurrence.
Do antithrombotic agents vary in efficacy by stroke subtype? Platelet antiaggregants. • CAST & IST studies • Used Oxfordshire Classification of ischemic stroke subtypes: 4 categories: total anterior circulation infarction, partial anterior circulation infarction, posterior infarction, lacunar infarction. • Aspirin did not reduce death or nonfatal stroke. CAST (Chinese Acute Stroke Trial) Collaboration Group. CAST: randomized placebo-controlled trial of early aspirin use in 20, 000 patients with acute ischaemic stroke. Lancet 1997; 349: 1641– 1649. International Stroke Trial Collaborative Group. The International Stroke Trial (IST): a randomized trial of aspirin, subcutaneous heparin, both, or neither among 19, 435 patients with acute ischaemic stroke. Lancet 1997; 349: 1569 – 1581.
Heparin Patients with atrial fibrillation do benefit from long-term anticoagulation for secondary stroke prevention EAFT Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. Lancet 1993; 342: 1255– 1262. limited data addressing the optimal time for beginning anticoagulation after an acute ischemic stroke. IST trial -SQ heparin reduced acute recurrent cardioembolic stroke, but increased ICH rate to a similar degree. However, the level of anticoagulation was not measured during follow-up. The study did not address the use of IV, dose-adjusted heparin
Do antithrombotic agents reduce systemic thrombotic complications such as deep vein thrombosis and pulmonary emboli? Pulmonary Emboli • Detected in 1% of stroke patients • Accounts for 10% of deaths after stroke, • Slows recovery & rehabilitation after stroke
SQ heparin • Reduces the risk of PE and DVT. • In IST study- Pt on 12, 500 IU SQ heparin fewer PE within 14 days VS aspirin (0. 5% vs 0. 8%; p=0. 02) • 5000 IU SQ heparin was not more effective than aspirin in preventing PE. International Stroke Trial Collaborative Group. The International Stroke Trial (IST): a randomized trial of aspirin, subcutaneous heparin, both, or neither among 19, 435 patients with acute ischaemic stroke. Lancet 1997; 349: 1569 – 1581.
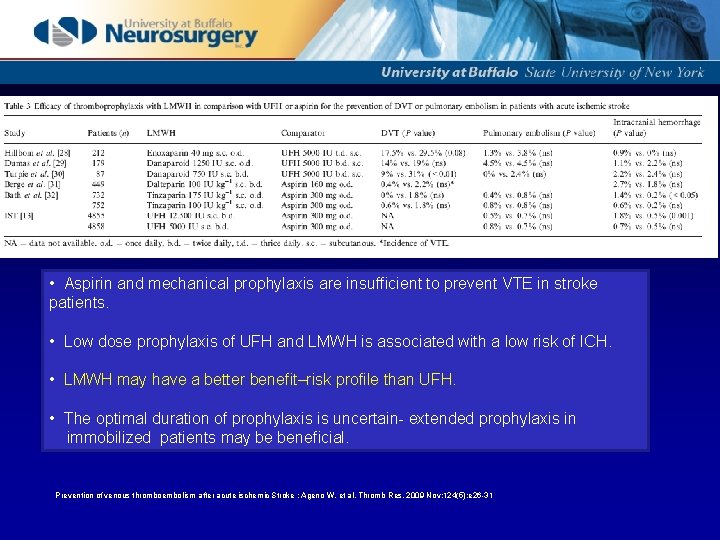
• Aspirin and mechanical prophylaxis are insufficient to prevent VTE in stroke patients. • Low dose prophylaxis of UFH and LMWH is associated with a low risk of ICH. • LMWH may have a better benefit–risk profile than UFH. • The optimal duration of prophylaxis is uncertain- extended prophylaxis in immobilized patients may be beneficial. Prevention of venous thromboembolism after acute ischemic Stroke : Ageno W, et al. Thromb Res. 2009 Nov; 124(5): e 26 -31
What are the risks of hemorrhage associated with antithrombotic agents? • 5% of embolic stroke patients will have Sx ICH • In large infarcts, ICH may reach 20%, exceeding the risk of early recurrent embolism (about 12%). • In large infarcts- with risk for delayed hemorrhagic transformation, postponing anticoagulation for 5 -7 days may be prudent.
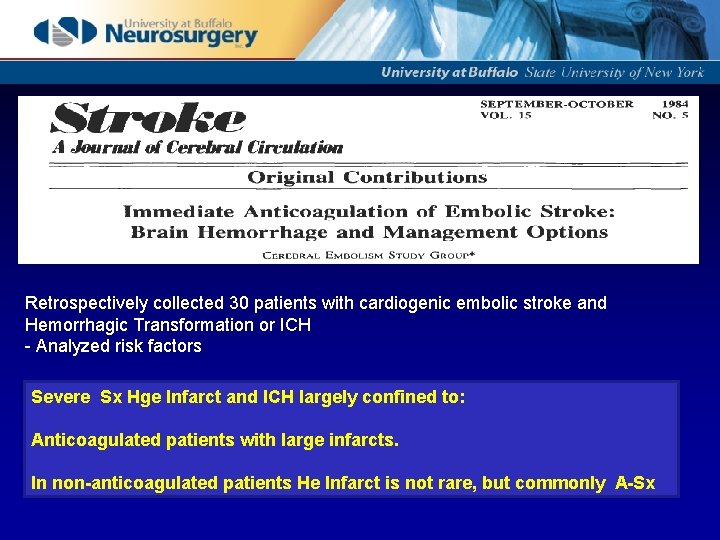
Retrospectively collected 30 patients with cardiogenic embolic stroke and Hemorrhagic Transformation or ICH - Analyzed risk factors Severe Sx Hge Infarct and ICH largely confined to: Anticoagulated patients with large infarcts. In non-anticoagulated patients He Infarct is not rare, but commonly A-Sx
• Increased risk- both systemic and ICH in patients treated with: Aspirin SQ heparin LMW heparin / heparinoids
Recommendations • Patients within 24 - 48 hours of stroke onset should be given aspirin (325 mg/day) to reduce stroke mortality and decrease morbidity (Grade A). • SQ heparin, LMW heparins, and heparinoids may be considered for DVT prophylaxis acute ischemic stroke, (Grade A). • SQ heparin -is not recommended for decreasing the risk of death, morbidity or recurrence (Grade A). The benefit in reducing early recurrent ischemic stroke, negated by an increase in hemorrhage.
• Dose-adjusted, IV heparin is not recommended for reducing morbidity, mortality, or early recurrent stroke in patients with acute stroke (not efficacious) may be associated with increased bleeding complications (Grade B). • High-dose LMW heparin/heparinoids have not been associated with either benefit or harm in reducing morbidity, mortality, or early recurrent stroke (Grade A). • IV heparin or high-dose LMW heparin/heparinoids are not recommended for any specific subgroup of patients with acute ischemic stroke that is based on any presumed stroke mechanism or location (e. g. , cardioembolic, large vessel atherosclerotic, vertebrobasilar, or “progressing” stroke) insufficient data (Grade U). • Although the LMW heparin, dalteparin, at high doses may be efficacious in patients with atrial fibrillation, it is not more efficacious than aspirin in this setting. Because aspirin is easier to administer, it, rather than dalteparin, is recommended for the various stroke subgroups (Grade A).
IV heparin • Urgent anticoagulation is not recommended for acute ischemic stroke (Class III, Level of Evidence A). • This may change if additional data demonstrate the usefulness of very early Tx of to large-artery thrombosis or cardioembolism. • Urgent anticoagulation is not recommended for patients with moderate to severe strokes because of an increased risk of serious ICH (Class III, Level of Evidence A). • Initiation of anticoagulant therapy within 24 hours of IV rt. PA is not recommended (Class III, Level of Evidence B). (Stroke. 2007; 38: 1655 -1711. )

- Slides: 27