ANTICOAGULANT FIBRINOLYTIC AND ANTIAGGREGANT DRUGS Prof Dr zlem
ANTICOAGULANT, FIBRINOLYTIC AND ANTIAGGREGANT DRUGS Prof. Dr. Özlem Uğur
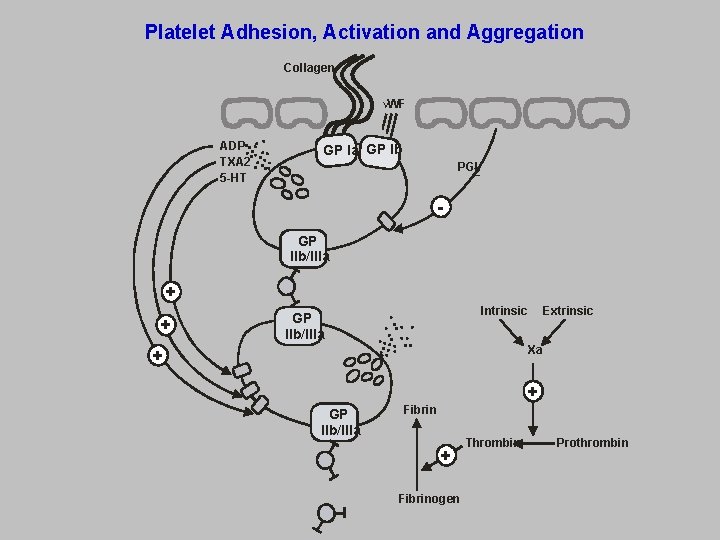
Platelet Adhesion, Activation and Aggregation Collagen VWF ADP TXA 2 5 -HT GP Ia GP Ib PGI 2 GP IIb/IIIa + + Intrinsic GP IIb/IIIa Extrinsic Xa + + GP IIb/IIIa Fibrin + Fibrinogen Thrombin Prothrombin
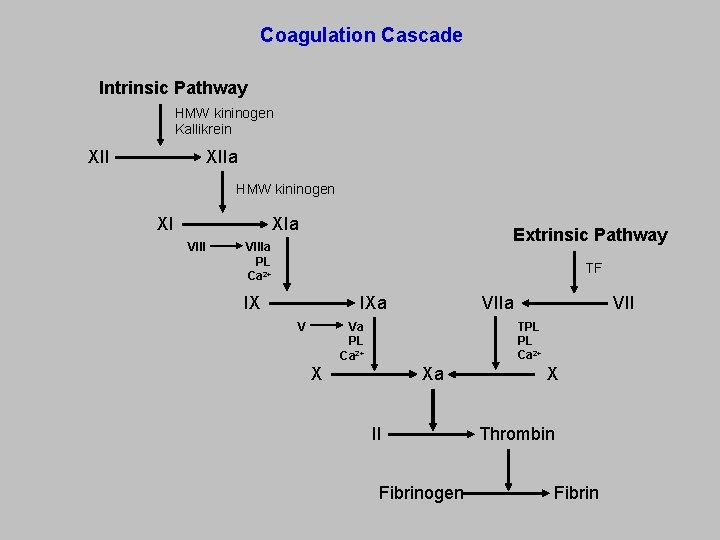
Coagulation Cascade Intrinsic Pathway HMW kininogen Kallikrein XIIa XII HMW kininogen XIa XI VIII Extrinsic Pathway VIIIa PL Ca 2+ TF IXa IX V VIIa TPL PL Ca 2+ Va PL Ca 2+ Xa X II Fibrinogen X Thrombin Fibrin
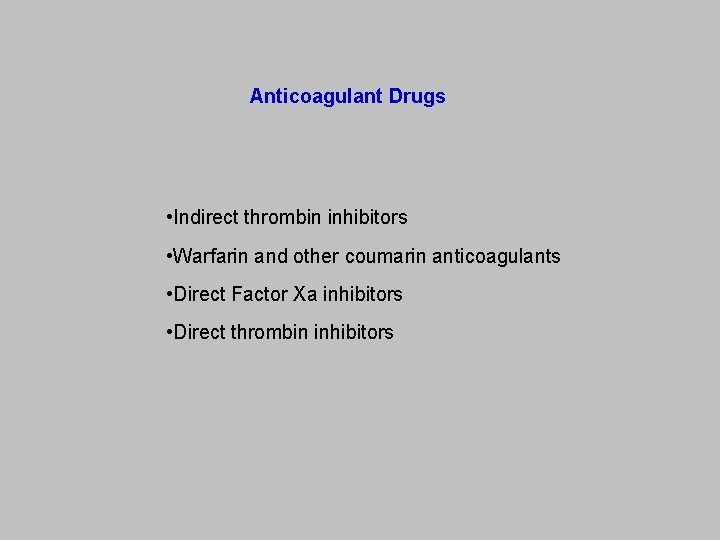
Anticoagulant Drugs • Indirect thrombin inhibitors • Warfarin and other coumarin anticoagulants • Direct Factor Xa inhibitors • Direct thrombin inhibitors
Indirect Thrombin Inhibitors • Unfractionated heparin • Low molecular weight heparin • Fondaparinux
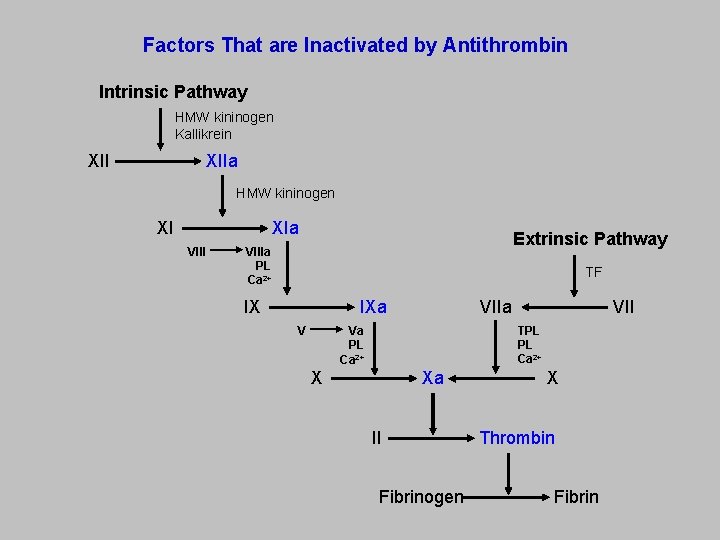
Factors That are Inactivated by Antithrombin Intrinsic Pathway HMW kininogen Kallikrein XIIa XII HMW kininogen XIa XI VIII Extrinsic Pathway VIIIa PL Ca 2+ TF IXa IX V VIIa TPL PL Ca 2+ Va PL Ca 2+ Xa X II Fibrinogen X Thrombin Fibrin
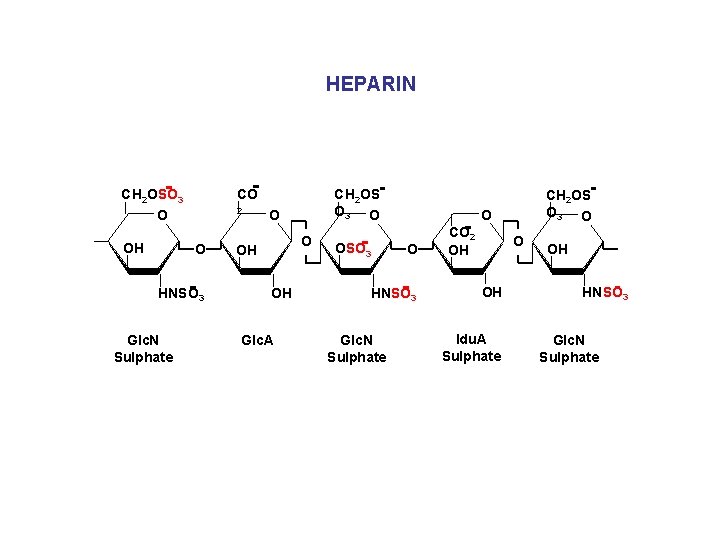
HEPARIN CO CH 2 OSO 3 2 O OH O HNSO 3 Glc. N Sulphate CH 2 OS O 3 O OH OH Glc. A OSO 3 O O HNSO 3 Glc. N Sulphate CH 2 OS O 3 O CO 2 OH O OH Idu. A Sulphate OH HNSO 3 Glc. N Sulphate
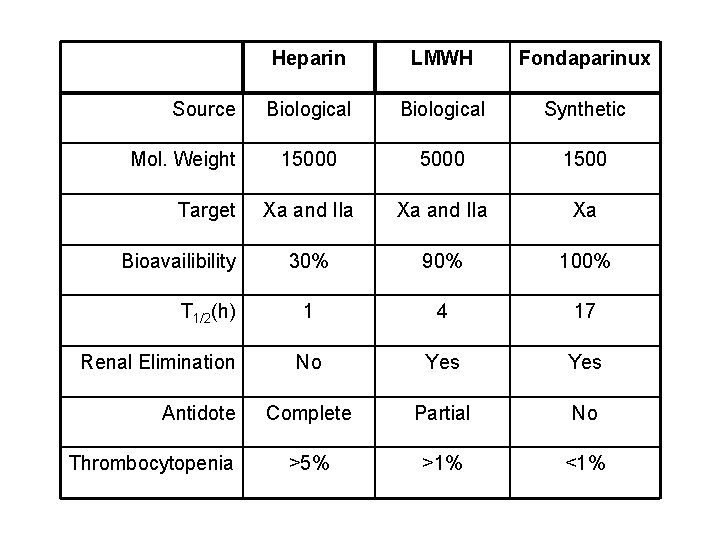
Source Mol. Weight Target Bioavailibility T 1/2(h) Renal Elimination Antidote Thrombocytopenia Heparin LMWH Fondaparinux Biological Synthetic 15000 1500 Xa and IIa Xa 30% 90% 100% 1 4 17 No Yes Complete Partial No >5% >1% <1%
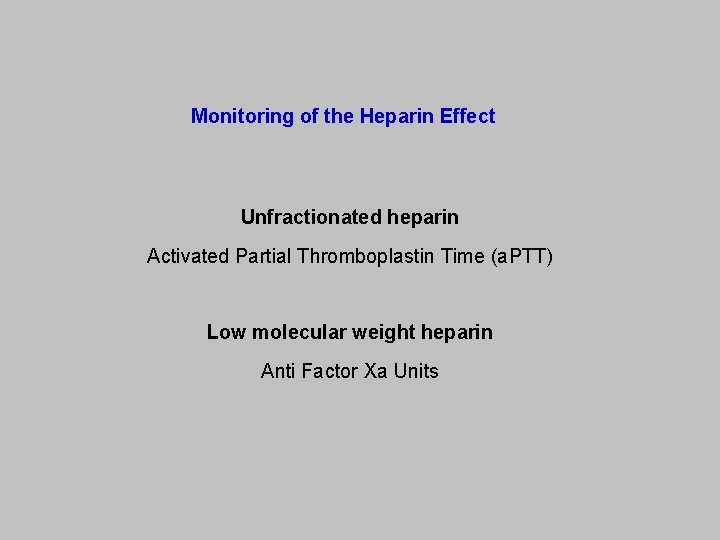
Monitoring of the Heparin Effect Unfractionated heparin Activated Partial Thromboplastin Time (a. PTT) Low molecular weight heparin Anti Factor Xa Units
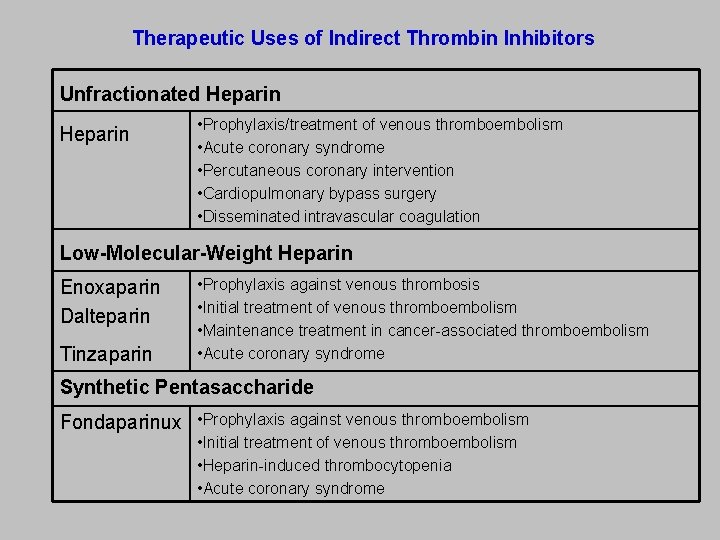
Therapeutic Uses of Indirect Thrombin Inhibitors Unfractionated Heparin • Prophylaxis/treatment of venous thromboembolism • Acute coronary syndrome • Percutaneous coronary intervention • Cardiopulmonary bypass surgery • Disseminated intravascular coagulation Low-Molecular-Weight Heparin Enoxaparin Dalteparin Tinzaparin • Prophylaxis against venous thrombosis • Initial treatment of venous thromboembolism • Maintenance treatment in cancer-associated thromboembolism • Acute coronary syndrome Synthetic Pentasaccharide Fondaparinux • Prophylaxis against venous thromboembolism • Initial treatment of venous thromboembolism • Heparin-induced thrombocytopenia • Acute coronary syndrome
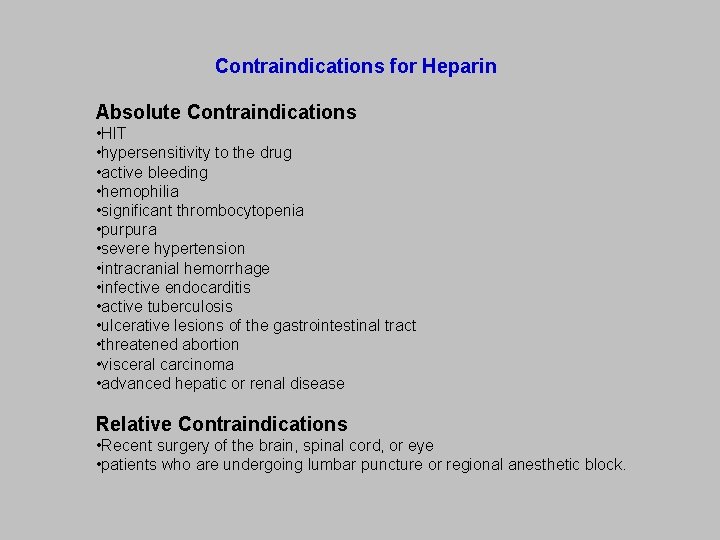
Contraindications for Heparin Absolute Contraindications • HIT • hypersensitivity to the drug • active bleeding • hemophilia • significant thrombocytopenia • purpura • severe hypertension • intracranial hemorrhage • infective endocarditis • active tuberculosis • ulcerative lesions of the gastrointestinal tract • threatened abortion • visceral carcinoma • advanced hepatic or renal disease Relative Contraindications • Recent surgery of the brain, spinal cord, or eye • patients who are undergoing lumbar puncture or regional anesthetic block.
Warfarin and Other Coumarin Drugs
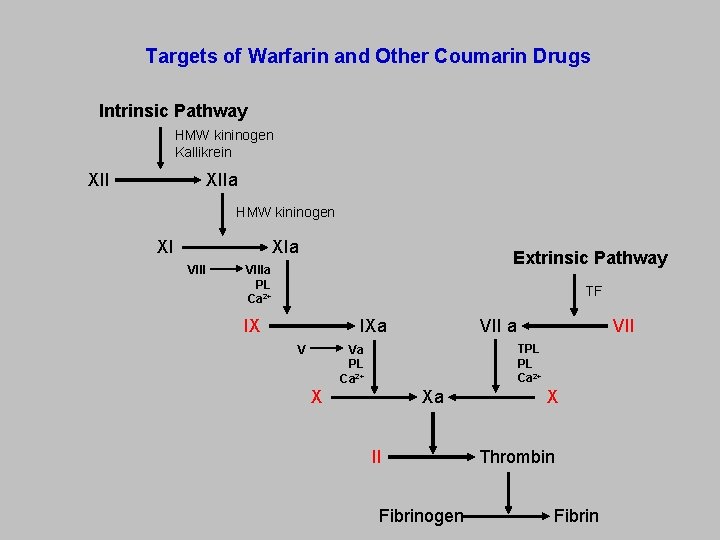
Targets of Warfarin and Other Coumarin Drugs Intrinsic Pathway HMW kininogen Kallikrein XIIa XII HMW kininogen XIa XI VIII Extrinsic Pathway VIIIa PL Ca 2+ TF IXa IX V VII a TPL PL Ca 2+ Va PL Ca 2+ Xa X II Fibrinogen X Thrombin Fibrin
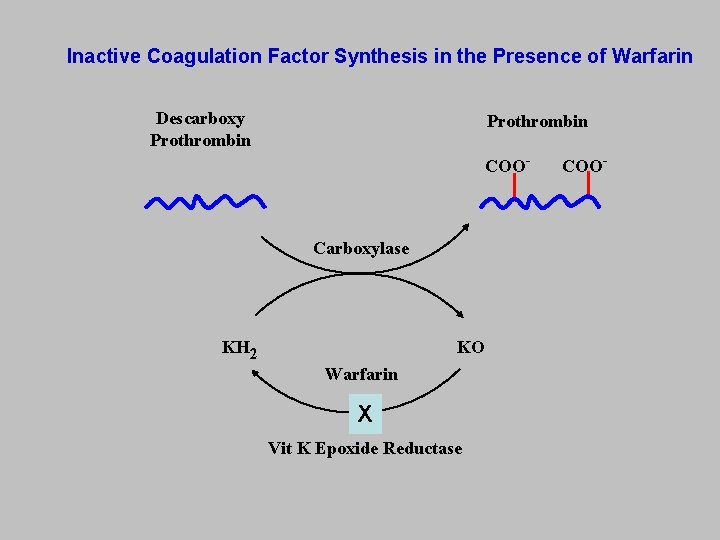
Inactive Coagulation Factor Synthesis in the Presence of Warfarin Descarboxy Prothrombin COO- Carboxylase KO KH 2 Warfarin X Vit K Epoxide Reductase COO-
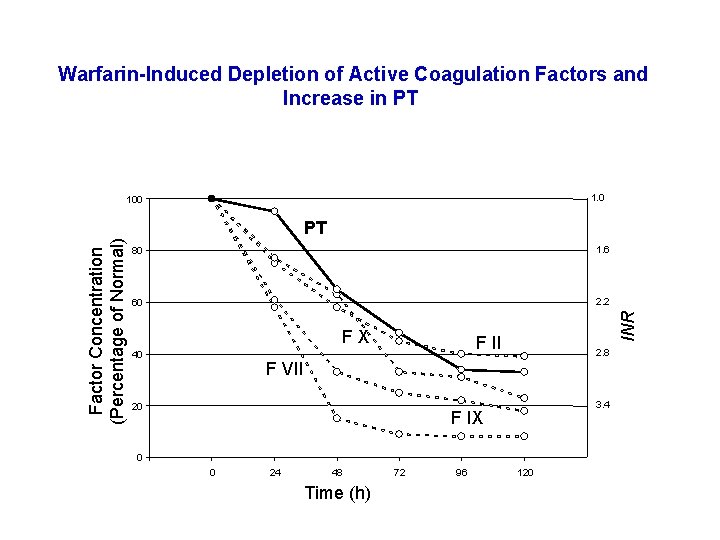
Warfarin-Induced Depletion of Active Coagulation Factors and Increase in PT 1. 0 PT 80 1. 6 60 2. 2 FX 40 INR Factor Concentration (Percentage of Normal) 100 F II 2. 8 F VII 20 3. 4 F IX 0 0 24 48 Time (h) 72 96 120
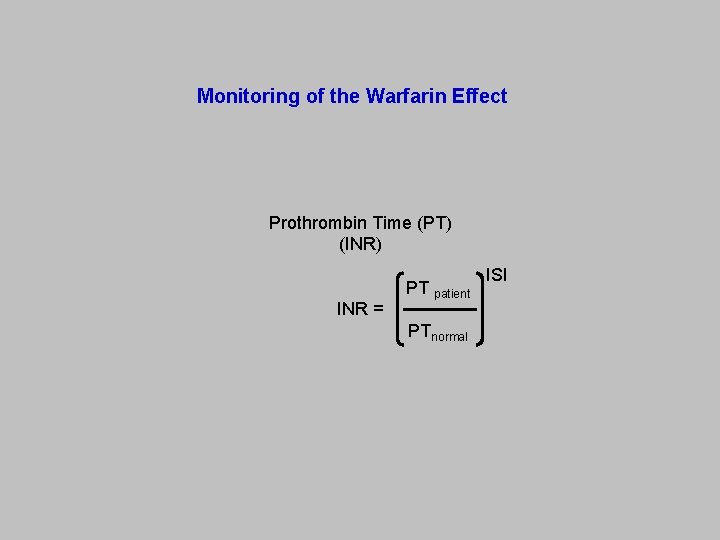
Monitoring of the Warfarin Effect Prothrombin Time (PT) (INR) PT INR = ISI patient PTnormal
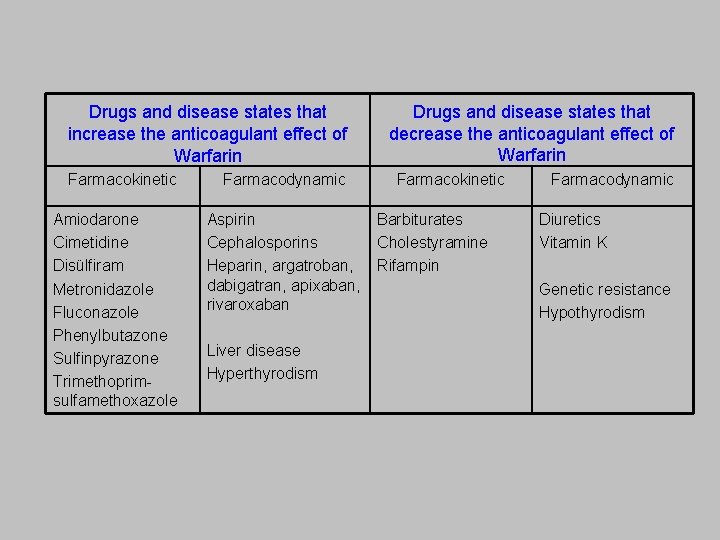
Drugs and disease states that increase the anticoagulant effect of Warfarin Farmacokinetic Amiodarone Cimetidine Disülfiram Metronidazole Fluconazole Phenylbutazone Sulfinpyrazone Trimethoprimsulfamethoxazole Farmacodynamic Aspirin Cephalosporins Heparin, argatroban, dabigatran, apixaban, rivaroxaban Liver disease Hyperthyrodism Drugs and disease states that decrease the anticoagulant effect of Warfarin Farmacokinetic Barbiturates Cholestyramine Rifampin Farmacodynamic Diuretics Vitamin K Genetic resistance Hypothyrodism
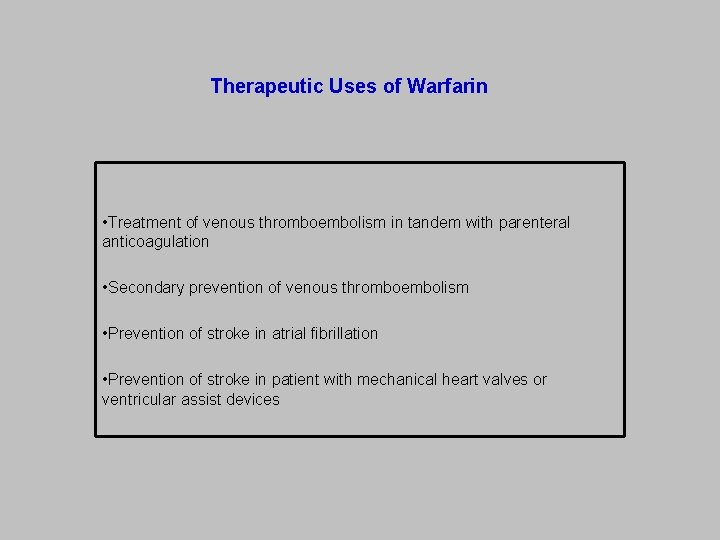
Therapeutic Uses of Warfarin • Treatment of venous thromboembolism in tandem with parenteral anticoagulation • Secondary prevention of venous thromboembolism • Prevention of stroke in atrial fibrillation • Prevention of stroke in patient with mechanical heart valves or ventricular assist devices
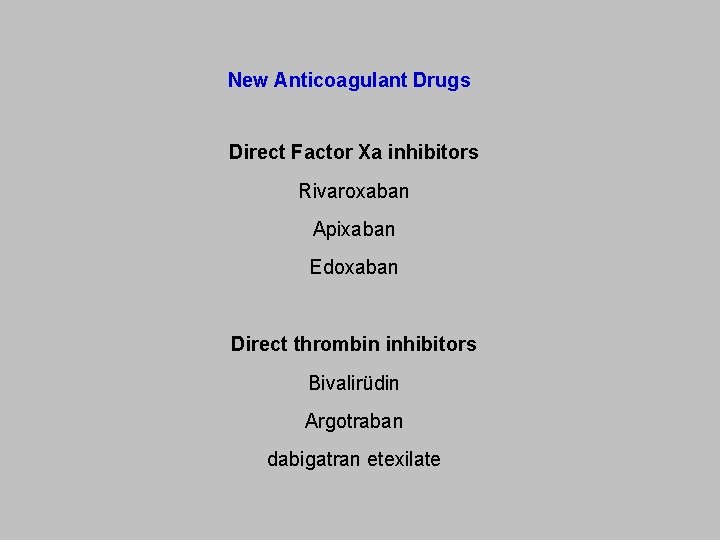
New Anticoagulant Drugs Direct Factor Xa inhibitors Rivaroxaban Apixaban Edoxaban Direct thrombin inhibitors Bivalirüdin Argotraban dabigatran etexilate
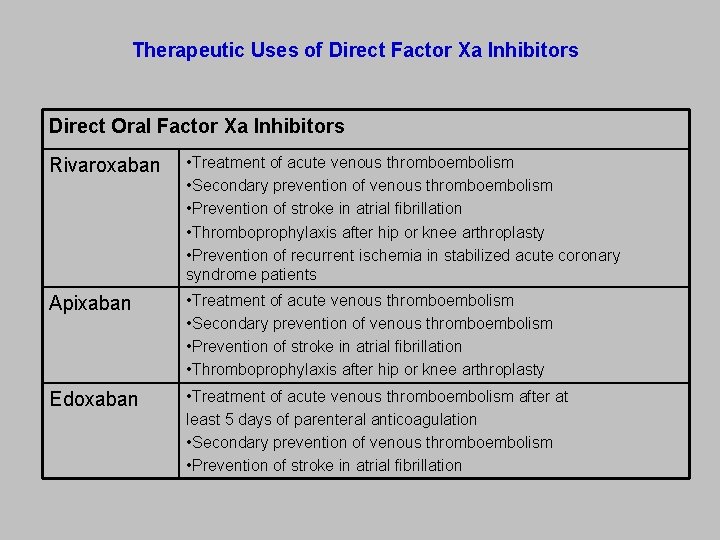
Therapeutic Uses of Direct Factor Xa Inhibitors Direct Oral Factor Xa Inhibitors Rivaroxaban • Treatment of acute venous thromboembolism • Secondary prevention of venous thromboembolism • Prevention of stroke in atrial fibrillation • Thromboprophylaxis after hip or knee arthroplasty • Prevention of recurrent ischemia in stabilized acute coronary syndrome patients Apixaban • Treatment of acute venous thromboembolism • Secondary prevention of venous thromboembolism • Prevention of stroke in atrial fibrillation • Thromboprophylaxis after hip or knee arthroplasty Edoxaban • Treatment of acute venous thromboembolism after at least 5 days of parenteral anticoagulation • Secondary prevention of venous thromboembolism • Prevention of stroke in atrial fibrillation
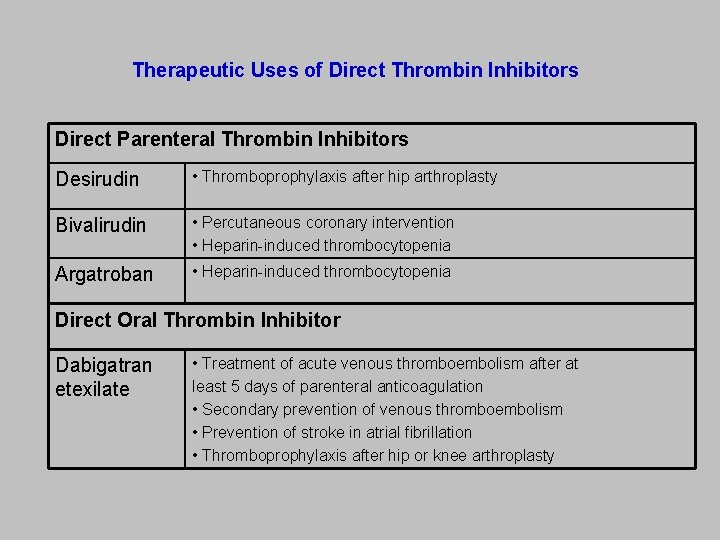
Therapeutic Uses of Direct Thrombin Inhibitors Direct Parenteral Thrombin Inhibitors Desirudin • Thromboprophylaxis after hip arthroplasty Bivalirudin • Percutaneous coronary intervention • Heparin-induced thrombocytopenia Argatroban • Heparin-induced thrombocytopenia Direct Oral Thrombin Inhibitor Dabigatran etexilate • Treatment of acute venous thromboembolism after at least 5 days of parenteral anticoagulation • Secondary prevention of venous thromboembolism • Prevention of stroke in atrial fibrillation • Thromboprophylaxis after hip or knee arthroplasty
Fibrinolytic Drugs Streptokinase Urokinase Tissue Plasminogen Activator (t-PA)
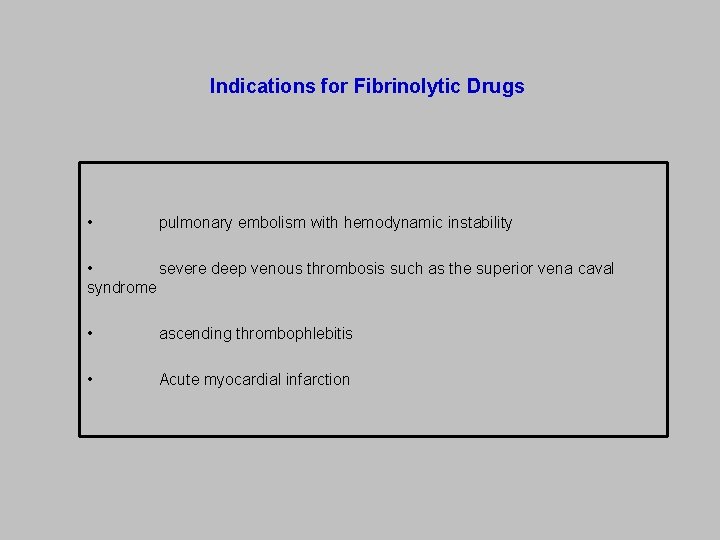
Indications for Fibrinolytic Drugs • pulmonary embolism with hemodynamic instability • severe deep venous thrombosis such as the superior vena caval syndrome • ascending thrombophlebitis • Acute myocardial infarction

Contraindications for Fibrinolytic Drugs Absolute Contraindications • İntracranial hemorrhage • Structural lesions in cerebral blood vessels • Malignant intracranial tumors • Ischemic attack in the last three months • Suspected aortic dissection • Active bleeding or bleeding diathesis • Closed cranial or facial trauma in the last three months Relative Contraindications • Uncontrolled hypertension • Major surgical operation in the last three weeks • Internal bleeding in the last two weeks • Known streptokinase hypersensitivity (for streptokinase) • Pregnancy • Peptic ulcer • Warfarin use (INR>1. 7)
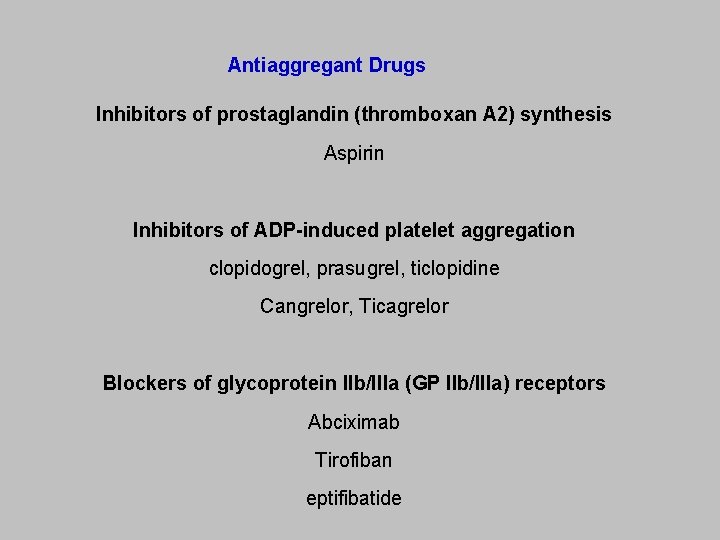
Antiaggregant Drugs Inhibitors of prostaglandin (thromboxan A 2) synthesis Aspirin Inhibitors of ADP-induced platelet aggregation clopidogrel, prasugrel, ticlopidine Cangrelor, Ticagrelor Blockers of glycoprotein IIb/IIIa (GP IIb/IIIa) receptors Abciximab Tirofiban eptifibatide
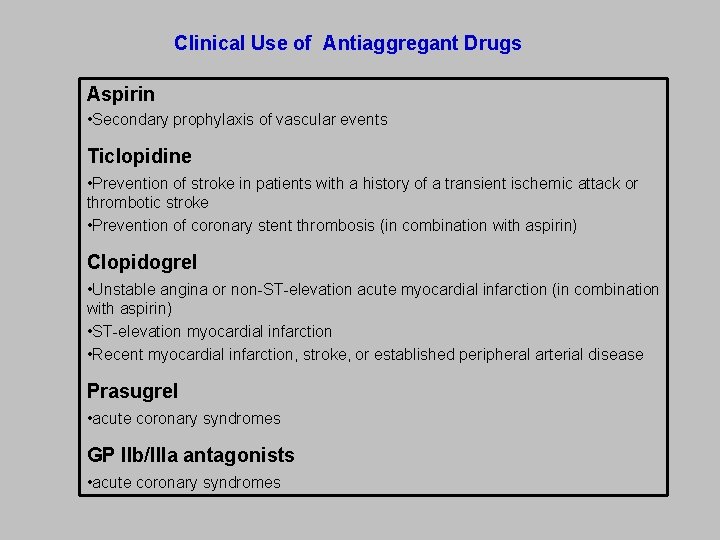
Clinical Use of Antiaggregant Drugs Aspirin • Secondary prophylaxis of vascular events Ticlopidine • Prevention of stroke in patients with a history of a transient ischemic attack or thrombotic stroke • Prevention of coronary stent thrombosis (in combination with aspirin) Clopidogrel • Unstable angina or non-ST-elevation acute myocardial infarction (in combination with aspirin) • ST-elevation myocardial infarction • Recent myocardial infarction, stroke, or established peripheral arterial disease Prasugrel • acute coronary syndromes GP IIb/IIIa antagonists • acute coronary syndromes
- Slides: 26