Antibiotics vaccines for healthcare worker Key points l
Antibiotics & vaccines for healthcare worker
Key points l Introduction l Choice of the proper antibiotic l Antimicrobial combinations l Choice of the route and efficacy assessment
Sir A. Fleming: discoverer of Penicillin Noble prize 1945
Antibiotics l PCNs l Cephalosporins l Carbapenem l Monobactams l Glycopeptide l Aminoglycoside l Fluroquinolone

PCN l l l l PCN G PCN V Amoxicillin Cloxacillin Oxacillin Ampicillin Piperacillin Methicillin
Choice of the proper agent Identification of the organism 2) Antimicrobial susceptibility 3) The narrowest effective spectrum 4) Host factors (Allergy, age, renal and liver, site of infection, pregnancy, metabolic abnormalities) 1)
Identification of the organism l Gram stain (CSF, Pleural, synovial, peritoneal, urine, sputum) l ELISA / latex agglutination l PCR l CULTURE (best if before Abx) l Bacteriologic statistics (the application of knowledge of the organisms most likely to cause infection in a given clinical sitting)
Antimicrobial susceptibility l l l l Disk diffusion method Epsilometer (E-test) Minimum inhibitory conc. (MIC) Minimum bactercidal conc. (MBC) Specialized testing for: fastidious organisms (obligate anaerobes), Haemophilus spp, pneumococci, MRSA Resistance mechanism of the bacteria: eg: Staph. aureus, E. coli, Enterbacter …. .

Disk diffusion method
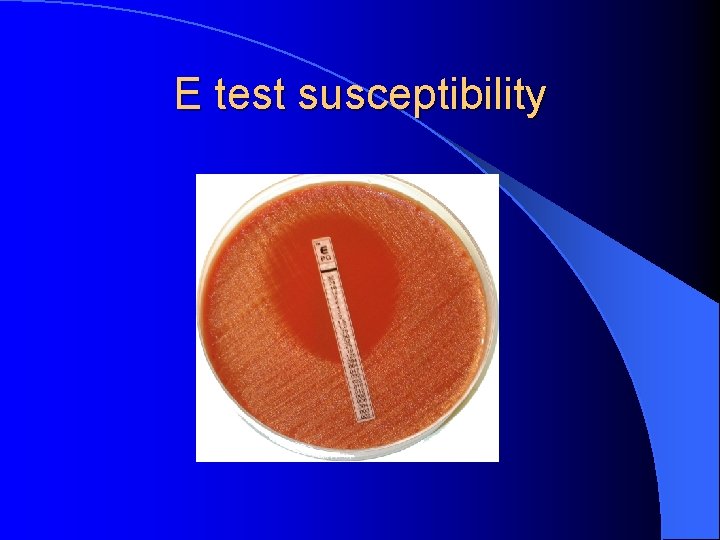
E test susceptibility
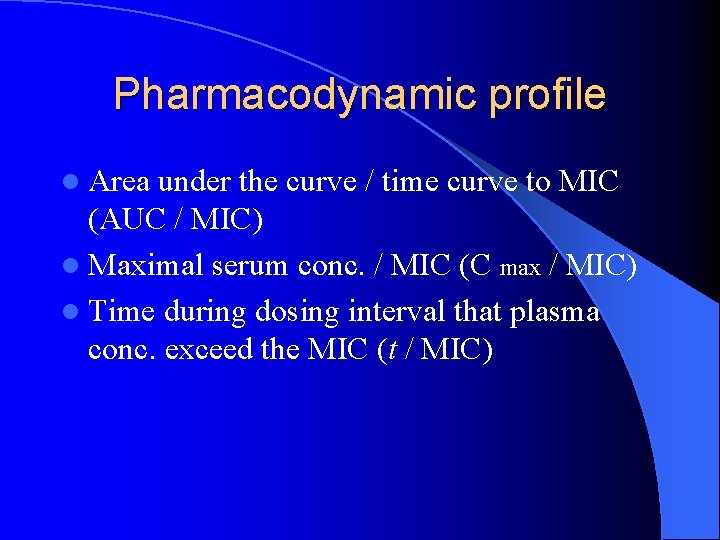
Pharmacodynamic profile l Area under the curve / time curve to MIC (AUC / MIC) l Maximal serum conc. / MIC (C max / MIC) l Time during dosing interval that plasma conc. exceed the MIC (t / MIC)
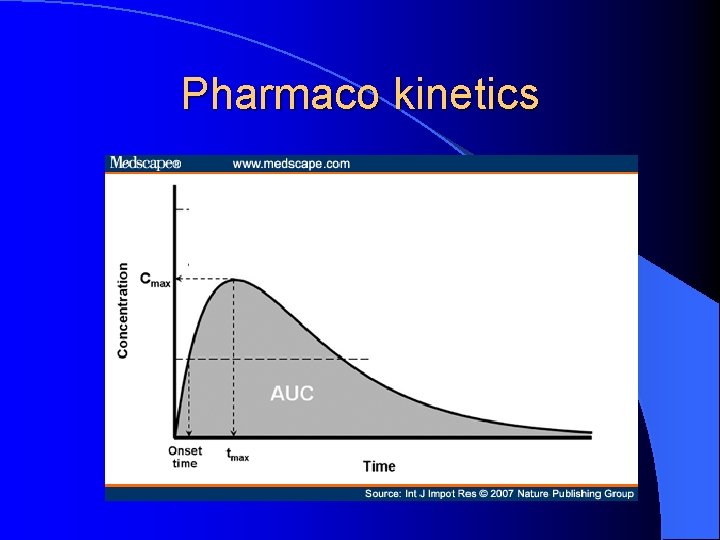
Pharmaco kinetics
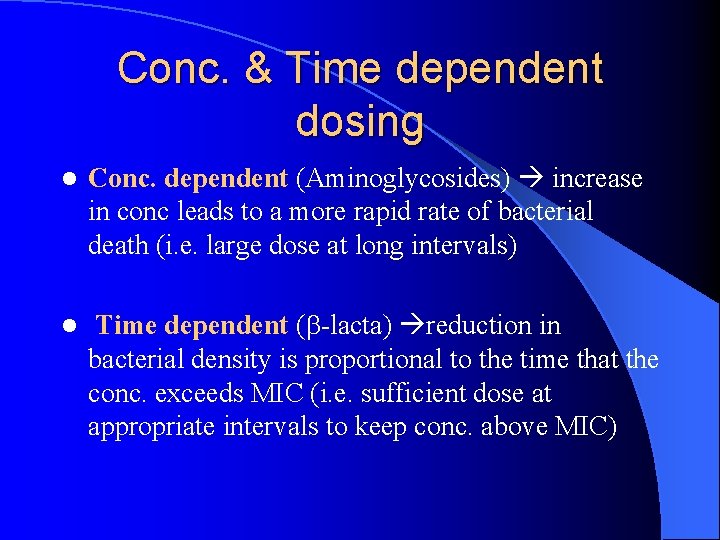
Conc. & Time dependent dosing l Conc. dependent (Aminoglycosides) increase in conc leads to a more rapid rate of bacterial death (i. e. large dose at long intervals) l Time dependent ( -lacta) reduction in bacterial density is proportional to the time that the conc. exceeds MIC (i. e. sufficient dose at appropriate intervals to keep conc. above MIC)
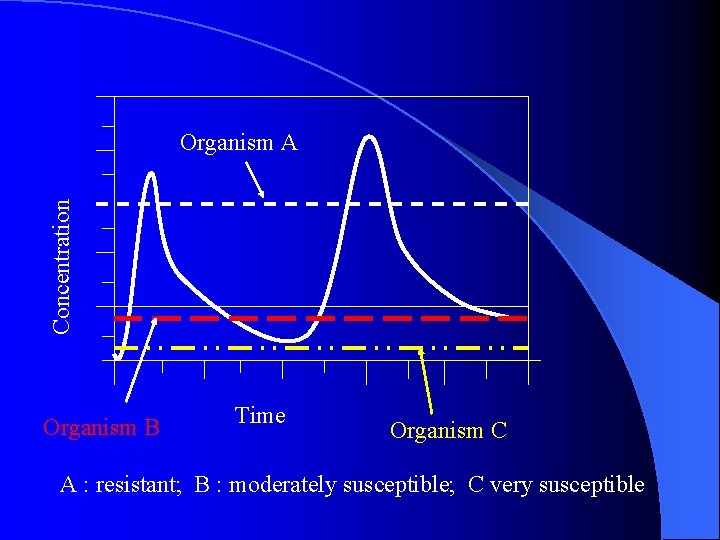
Concentration Organism A Organism B Time Organism C A : resistant; B : moderately susceptible; C very susceptible
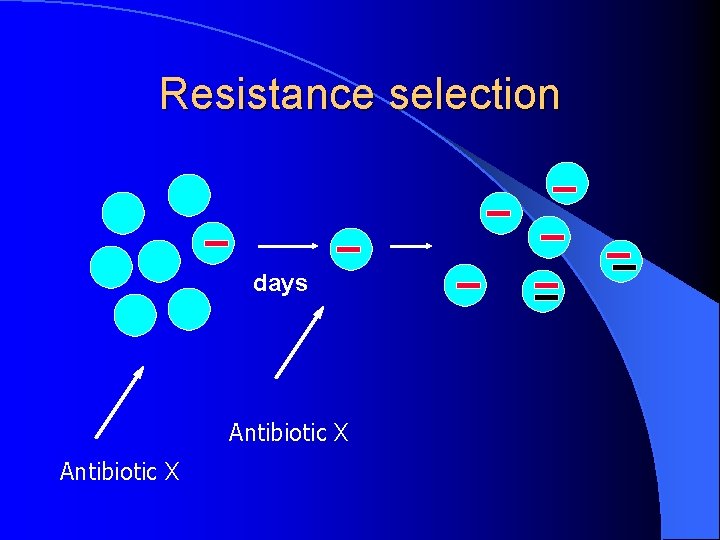
Resistance selection days Antibiotic X
Published data l Manuals l l l eg: Sanford’s Medical letter on drugs and therapeutics (nb: use this information within its context)
Host factors l Previous history of adverse reactions l Neutrophil function neutropenic are treated aggressively l CLL, Multiple Myeloma, asplenia treated empirically
Age l Renal function (impaired physiologic function) l Absorption l Tetracyclines l INH hepatotoxicity l Nephrotoxicity l Aminoglycosides and cochlear toxicity
Genetic / metabolic l Hemolysis in G 6 PD deficiency l DM : sulfa drugs can potentiate the sulfonylurea hypoglycemic agents l - Dextrose load
Pregnancy Safe : PCN, cephalosporin, erythromycin l Dangerous: tetracyclines (hepatic toxicity, dental discoloration) l ? metronidazole l l FQ Contrindicated l ? ? rifampin, Ag, azithromyccin, clindamycin, imipenem, vancomycin, TMP l Abx dose needs to be increased?
Renal and liver fx l Vancomycin & Aminoglycosides
Site of infection l Optimal therapy requires concentrations > MIC at the site of infection l l l l Meningitis Endocarditis Osteomylitis Chronic prostatitis Intraocular infections Abscesses Foreign body UTI
Immune system l Abx can cause immune suppression esp. in the immunosuppressed patients l Suppress monocyte transformation, phagocytosis, chemotaxis, antibody production
Combinations l Some physicians use combinations for the sense of security deleterious effects l Indications: 1) prevention of emergence of resistant bacteria : TB, staph endocarditis l 2) polymicrobial infections : abd. sepsis l 3) initial therapy: eg: Ag + piperacillin l 4)Synergism: …
Synergism l For resistant organisms l Limited data to support their benefit l e. g. : PCN + Ag Enterococcal endocarditis l Oxacillin + Ag Staph. endocarditis l Anti-pseudomonal - lactam + Ag Pseudomonas bacteremia l Impaired host
Antagonism l Too many in vitro reports l Clinically was seen in : PCN + tetracyclines l 2 -lactams induce lactamases l More important in immunosuppressed pts
Adverse effects l 5% of pts will have a side effect l Combinations more cost, more adverse effects
Anaphylaxis l Beta lactams are the most common ABx to cause anaphylaxis l PCN risk of anaphylaxis: 0. 01% l Death occurs in 1 / 100, 000 courses l 10 - 20% of pts who claim to have an allergy to PCN are truly allergic l 50% of pts with a positive skin test: reaction
Anaphylaxis PCN cross reaction with Cephalosporins l Minimum cross reaction with carbapenem 1% l
Route stable , mild infection (reliable pts) l IV serious infections (sepsis) l Oral
Monitoring the response l Clinically l Drug levels l Lab tests
Cost l If all other factors are equal, the least expensive drug should be chosen
Needle stick l Risk l- of transmission Hepatitis B virus 30% l - Hepatitis C virus 3% l - HIV 0. 3%
HBV Vaccine recommendations l HB vaccine offered for all HCW – Required in US (1991) – Human rights issues (what if they refused ? ? ) l Check response after 1 month – Responders: …. . 10 IU/l – Non responders………. < 10 IU/l
HBV vaccine l Does not transmit the virus l 3 shots at 0, 1, 6 months l The series is administered once l A booster shot can be given in times of outbreak conditions l If you are exposed to HBV immediate vaccination is extremely helpful
HBV vaccine (cont) You do not need to accept the vaccine l You can decline it and sign a declination form l If you are exposed to HBV or changed your mind, you can still receive it l l Your employer might not offer you the vaccine if: – You are vaccinated – Have Antibodies – Contraindicated in your case
HBV (cont)
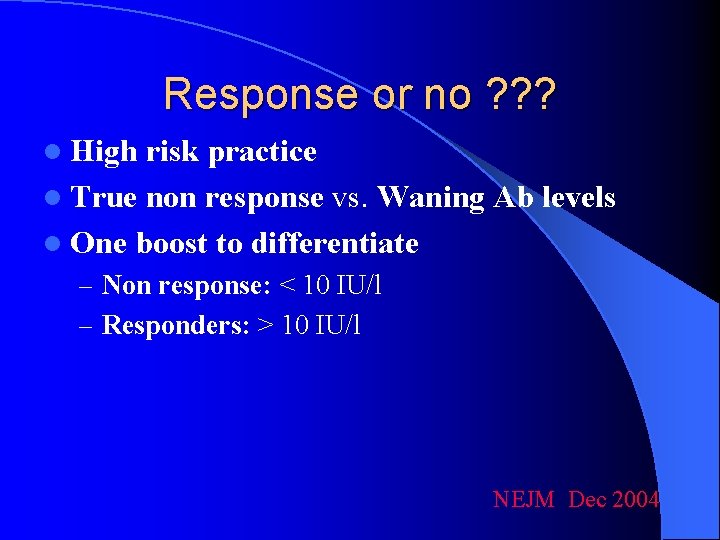
Response or no ? ? ? l High risk practice l True non response vs. Waning Ab levels l One boost to differentiate – Non response: < 10 IU/l – Responders: > 10 IU/l NEJM Dec 2004
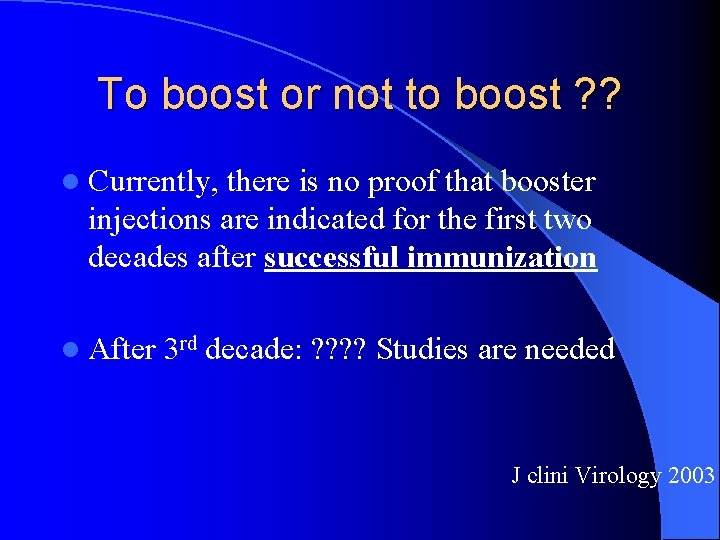
To boost or not to boost ? ? l Currently, there is no proof that booster injections are indicated for the first two decades after successful immunization l After 3 rd decade: ? ? Studies are needed J clini Virology 2003
Influenza vaccine l Annually l In the fall season – even if late l 2 strains of A + 1 strain of B l No protection against other Flu like illnesses like – RSV – Para influenza – Adenovirus
Influenza vaccine l Weak or no association with Guillain Barre syndrome – 1 / million l Contraindication – Previous GB syndrome – ? Egg allergy – Allergic reaction to any component
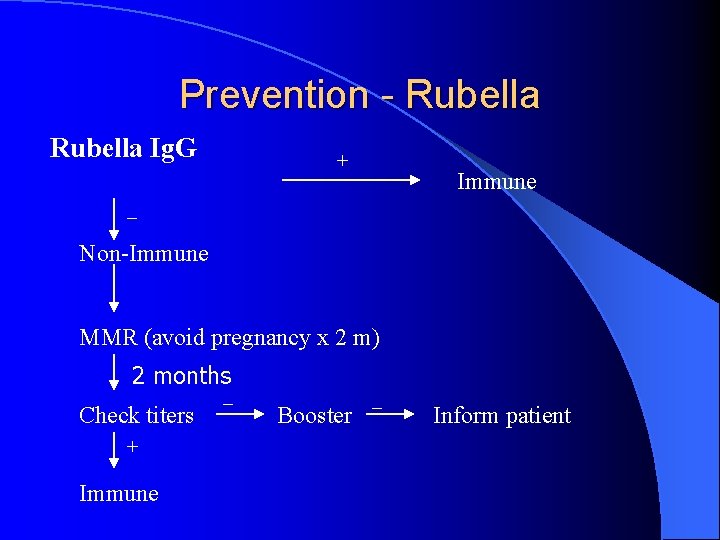
Prevention - Rubella Ig. G + Immune _ Non-Immune MMR (avoid pregnancy x 2 m) 2 months Check titers + Immune _ Booster _ Inform patient
Rubella-risk l Risk of congenital infection q 1 + 2 month: 90% q 3 rd month 50% q Termination of pregnancy is usually recommended in Western countries q > 16 weeks negligible q 12 – 16 weeks: deafness can occur
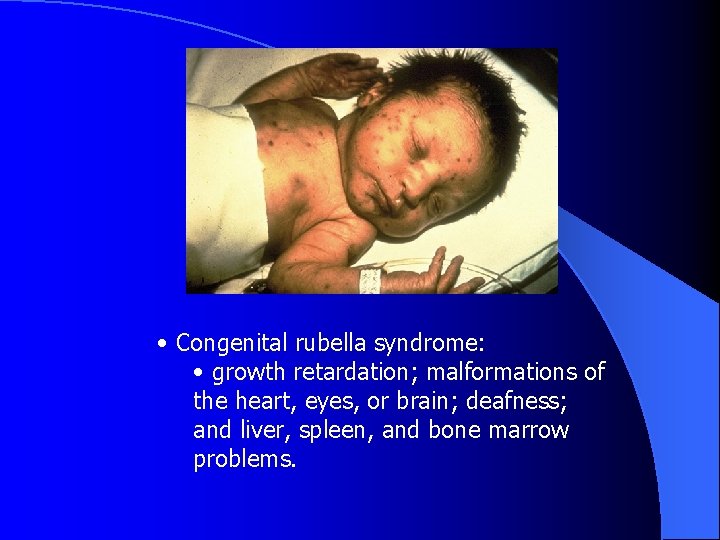
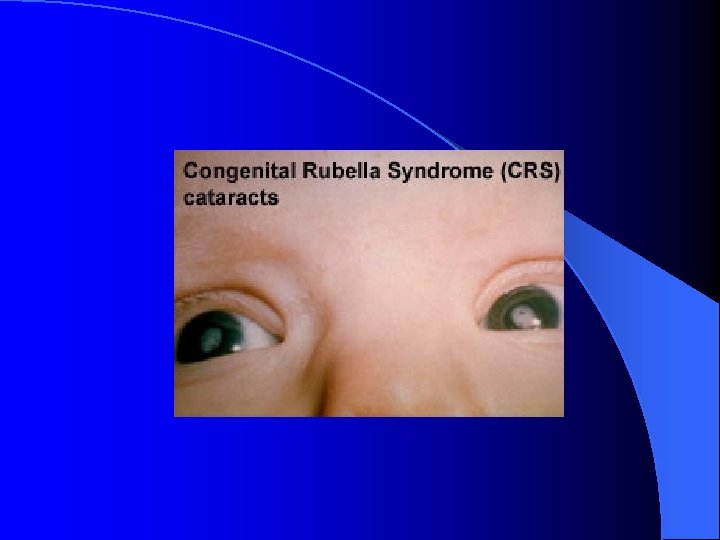
• Congenital rubella syndrome: • growth retardation; malformations of the heart, eyes, or brain; deafness; and liver, spleen, and bone marrow problems.
Prevention - Varicella l Varicella – History of chicken pox: … immune – Positive titers …. . . . immune – Absent titers: not immune l Give vaccine: 2 doses, 2 months apart – Postpone pregnancy 2 m after the second dose
Tetanus - Diphtheria vaccine l Once every ten years l Toxoid vaccine
Peneumococcal vaccine l Indicated for all immunocompromised adults l > 65 years l 1 or 2 doses
- Slides: 49