Antibiotics Biotechnology II Antibiotics Disrupt Cell Wall Synthesis

Antibiotics Biotechnology II
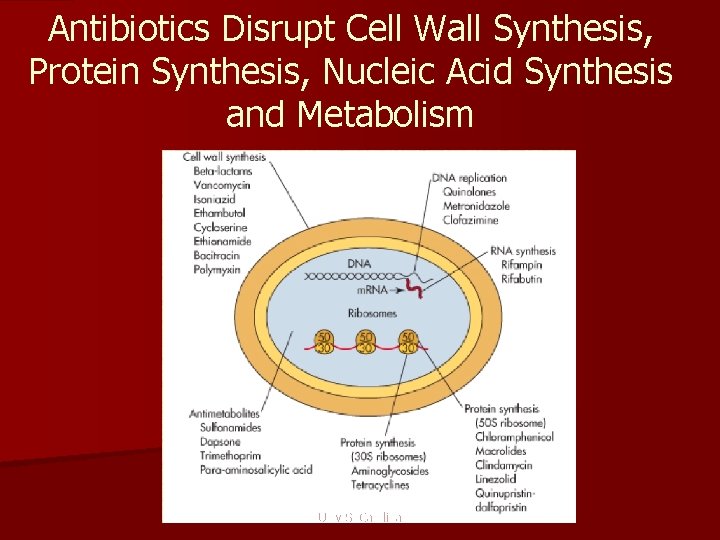
Antibiotics Disrupt Cell Wall Synthesis, Protein Synthesis, Nucleic Acid Synthesis and Metabolism Univ S. Carolina

Principles and Definitions n Selectivity – Selectivity vs toxicity n Therapeutic index – Toxic dose/ Effective dose n Categories of antibiotics – Bacteriostatic § Reversibly inhibit growth § Duration of treatment sufficient for host defenses to eradicate infection – Bactericidal§ Kill bacteria § Usually antibiotic of choice for infections in sites such as endocardium or the meninges where host defenses are ineffective.
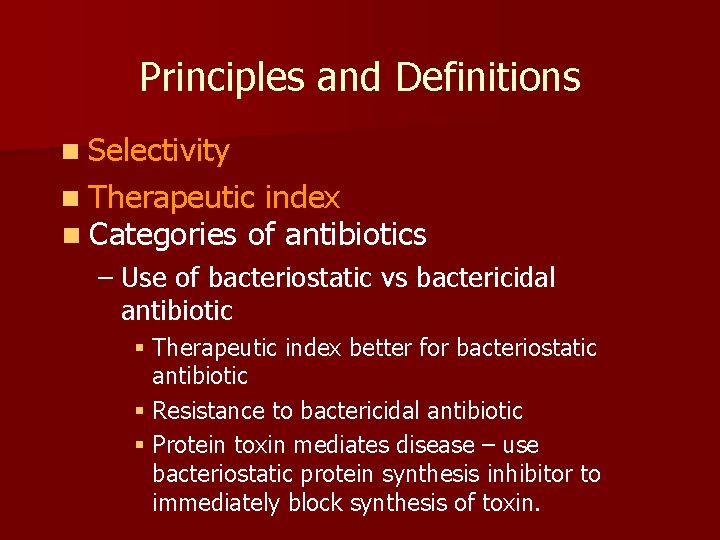
Principles and Definitions n Selectivity n Therapeutic index n Categories of antibiotics – Use of bacteriostatic vs bactericidal antibiotic § Therapeutic index better for bacteriostatic antibiotic § Resistance to bactericidal antibiotic § Protein toxin mediates disease – use bacteriostatic protein synthesis inhibitor to immediately block synthesis of toxin.
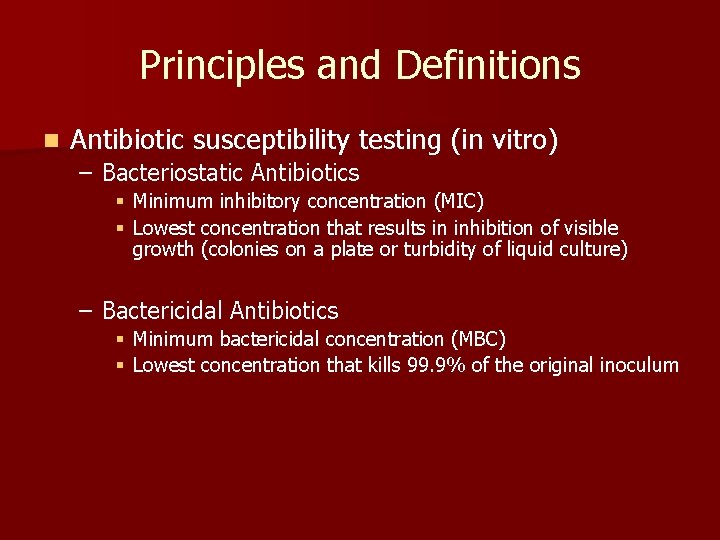
Principles and Definitions n Antibiotic susceptibility testing (in vitro) – Bacteriostatic Antibiotics § Minimum inhibitory concentration (MIC) § Lowest concentration that results in inhibition of visible growth (colonies on a plate or turbidity of liquid culture) – Bactericidal Antibiotics § Minimum bactericidal concentration (MBC) § Lowest concentration that kills 99. 9% of the original inoculum

Antibiotic Susceptibility Testing-MIC Disk Diffusion Test Determination of MIC Str Tet 8 4 2 1 0 Tetracycline ( g/ml) MIC = 2 g/ml Ery Chl Amp Size of zone of inhibition depends on sensitivity, solubility, rate of diffusion. Compare results to MIC tables generated using standards.
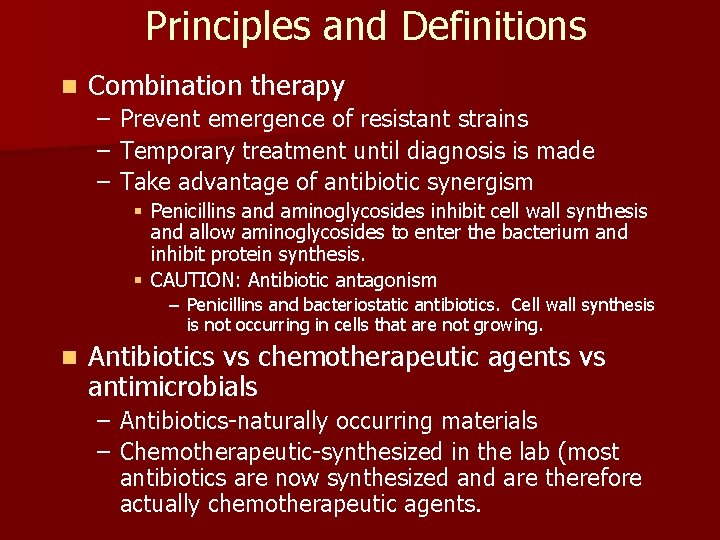
Principles and Definitions n Combination therapy – – – Prevent emergence of resistant strains Temporary treatment until diagnosis is made Take advantage of antibiotic synergism § Penicillins and aminoglycosides inhibit cell wall synthesis and allow aminoglycosides to enter the bacterium and inhibit protein synthesis. § CAUTION: Antibiotic antagonism – Penicillins and bacteriostatic antibiotics. Cell wall synthesis is not occurring in cells that are not growing. n Antibiotics vs chemotherapeutic agents vs antimicrobials – Antibiotics-naturally occurring materials – Chemotherapeutic-synthesized in the lab (most antibiotics are now synthesized and are therefore actually chemotherapeutic agents.
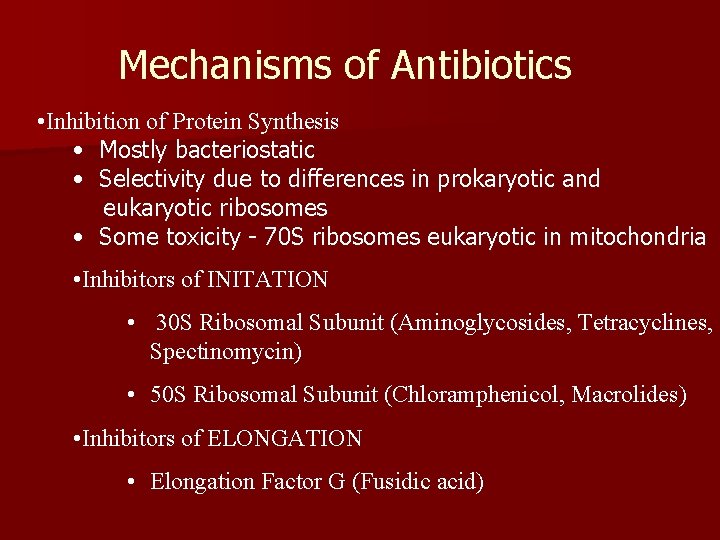
Mechanisms of Antibiotics • Inhibition of Protein Synthesis • Mostly bacteriostatic • Selectivity due to differences in prokaryotic and eukaryotic ribosomes • Some toxicity - 70 S ribosomes eukaryotic in mitochondria • Inhibitors of INITATION • 30 S Ribosomal Subunit (Aminoglycosides, Tetracyclines, Spectinomycin) • 50 S Ribosomal Subunit (Chloramphenicol, Macrolides) • Inhibitors of ELONGATION • Elongation Factor G (Fusidic acid)
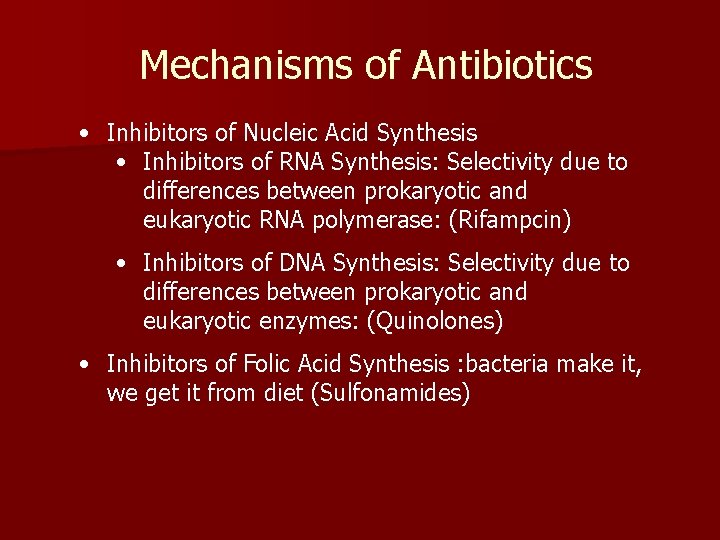
Mechanisms of Antibiotics • Inhibitors of Nucleic Acid Synthesis • Inhibitors of RNA Synthesis: Selectivity due to differences between prokaryotic and eukaryotic RNA polymerase: (Rifampcin) • Inhibitors of DNA Synthesis: Selectivity due to differences between prokaryotic and eukaryotic enzymes: (Quinolones) • Inhibitors of Folic Acid Synthesis : bacteria make it, we get it from diet (Sulfonamides)
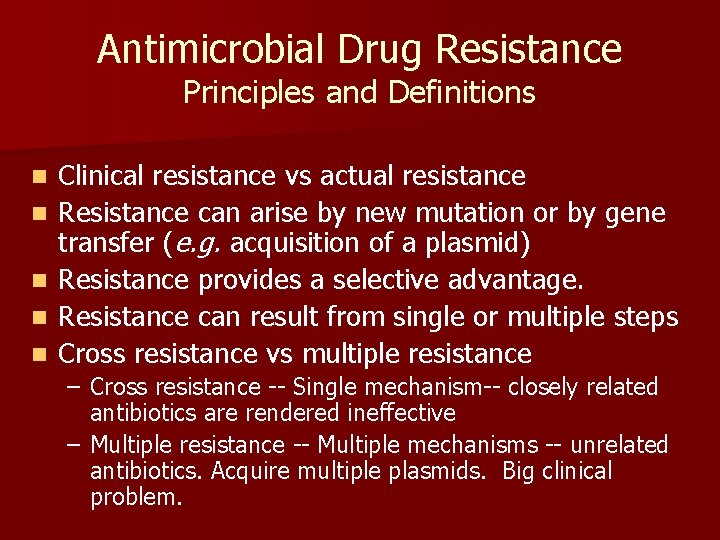
Antimicrobial Drug Resistance Principles and Definitions n n n Clinical resistance vs actual resistance Resistance can arise by new mutation or by gene transfer (e. g. acquisition of a plasmid) Resistance provides a selective advantage. Resistance can result from single or multiple steps Cross resistance vs multiple resistance – Cross resistance -- Single mechanism-- closely related antibiotics are rendered ineffective – Multiple resistance -- Multiple mechanisms -- unrelated antibiotics. Acquire multiple plasmids. Big clinical problem.
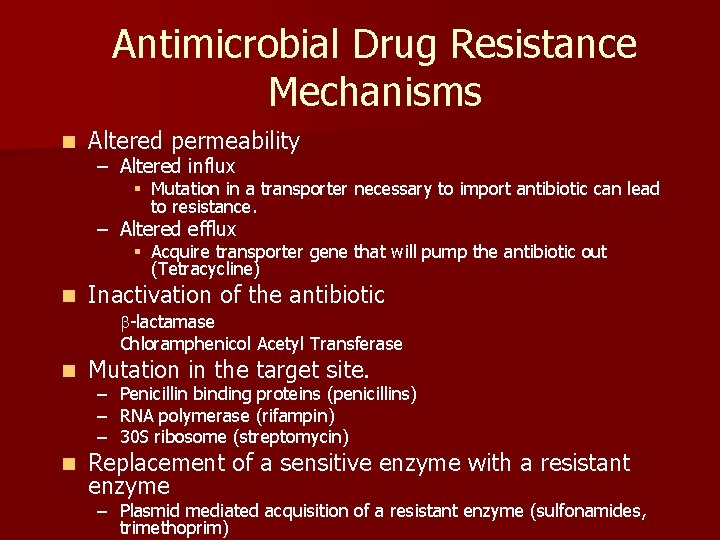
Antimicrobial Drug Resistance Mechanisms n Altered permeability – Altered influx § Mutation in a transporter necessary to import antibiotic can lead to resistance. – Altered efflux § Acquire transporter gene that will pump the antibiotic out (Tetracycline) n Inactivation of the antibiotic b-lactamase Chloramphenicol Acetyl Transferase n Mutation in the target site. n Replacement of a sensitive enzyme with a resistant enzyme – – – Penicillin binding proteins (penicillins) RNA polymerase (rifampin) 30 S ribosome (streptomycin) – Plasmid mediated acquisition of a resistant enzyme (sulfonamides, trimethoprim)
- Slides: 11