Antibiotic Use in Sepsis and Stewardship Maureen Campion
Antibiotic Use in Sepsis and Stewardship Maureen Campion, Pharm. D Clinical Pharmacy Specialist- Infectious Disease UMass Memorial Medical Center
Disclosure statement I have no actual or potential conflict of interest in relation to this program/presentation.
Objectives • Identify the role of antibiotics in sepsis • Describe the challenges to timely antibiotic administrations • List 3 ways to optimize antibiotics in sepsis • Understand the importance of de-escalation of antibiotics in sepsis
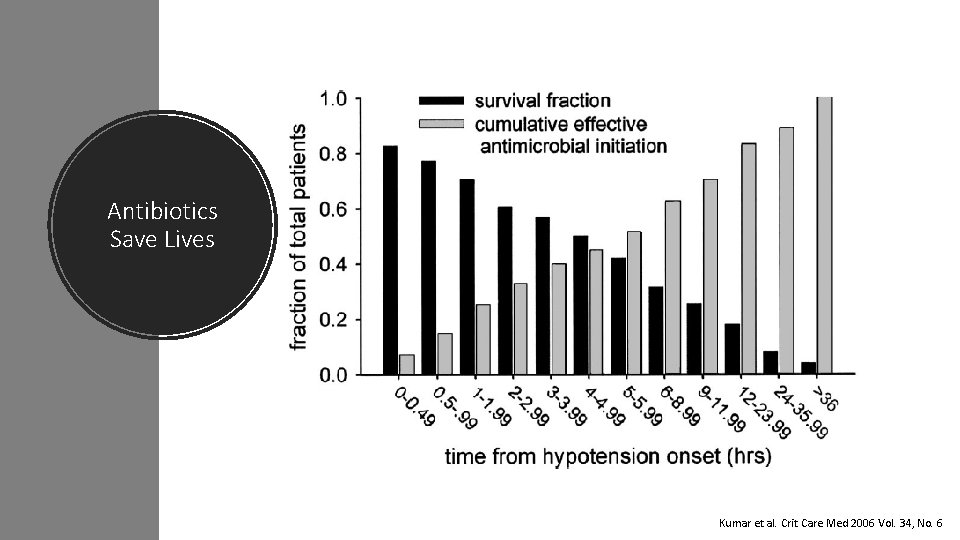
Antibiotics Save Lives Kumar et al. Crit Care Med 2006 Vol. 34, No. 6
![“Each hour of delay in antimicrobial administration [in severe sepsis] was associated with an “Each hour of delay in antimicrobial administration [in severe sepsis] was associated with an](http://slidetodoc.com/presentation_image_h2/d74d8beeea4b21958e3c49e65ca79c31/image-5.jpg)
“Each hour of delay in antimicrobial administration [in severe sepsis] was associated with an average decrease in survival of 7. 6%”
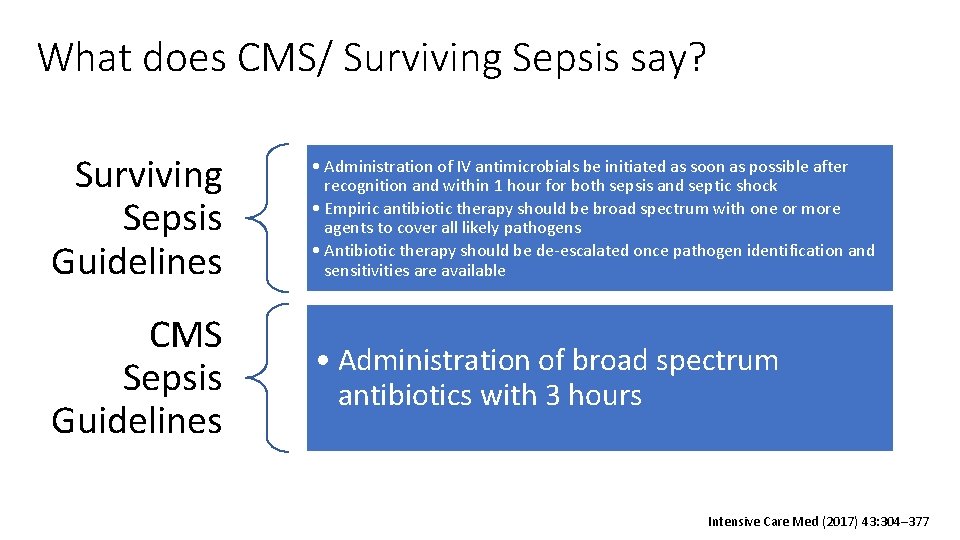
What does CMS/ Surviving Sepsis say? Surviving Sepsis Guidelines • Administration of IV antimicrobials be initiated as soon as possible after recognition and within 1 hour for both sepsis and septic shock • Empiric antibiotic therapy should be broad spectrum with one or more agents to cover all likely pathogens • Antibiotic therapy should be de-escalated once pathogen identification and sensitivities are available CMS Sepsis Guidelines • Administration of broad spectrum antibiotics with 3 hours Intensive Care Med (2017) 43: 304– 377
Challenges with Recommendations • No consistent definition of time “zero” • Overly broad use of broad spectrum antibiotics due to need to meet 1 hour or 3 hour metric • Appropriate labs including blood cultures should be drawn prior to the initiation of antibiotics Clinical Infectious Diseases® 2018; 66(10): 1631– 5
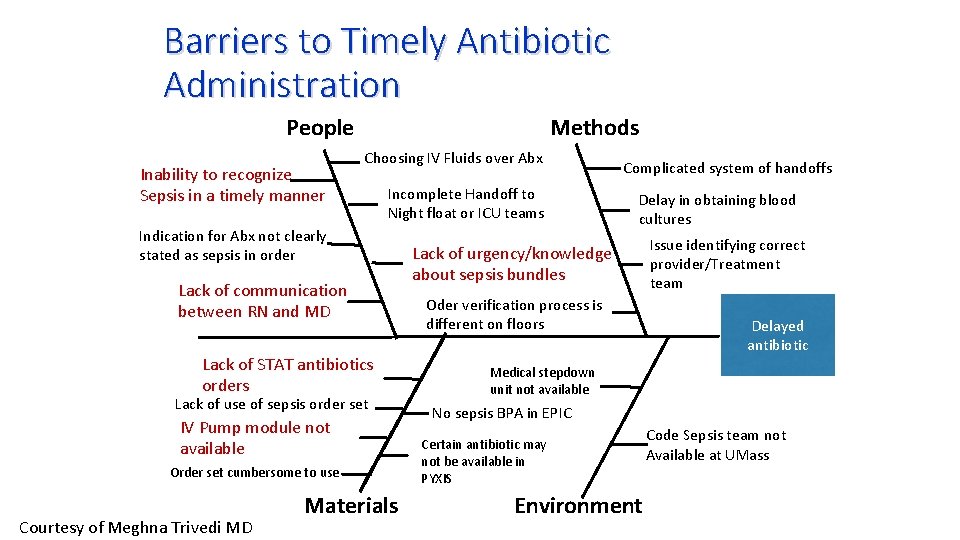
Barriers to Timely Antibiotic Administration Methods People Inability to recognize Sepsis in a timely manner Choosing IV Fluids over Abx Incomplete Handoff to Night float or ICU teams Indication for Abx not clearly stated as sepsis in order Lack of communication between RN and MD Lack of STAT antibiotics orders Lack of use of sepsis order set IV Pump module not available Order set cumbersome to use Courtesy of Meghna Trivedi MD Materials Complicated system of handoffs Delay in obtaining blood cultures Lack of urgency/knowledge about sepsis bundles Oder verification process is different on floors Issue identifying correct provider/Treatment team Delayed antibiotic Medical stepdown unit not available No sepsis BPA in EPIC Certain antibiotic may not be available in PYXIS Environment Code Sepsis team not Available at UMass
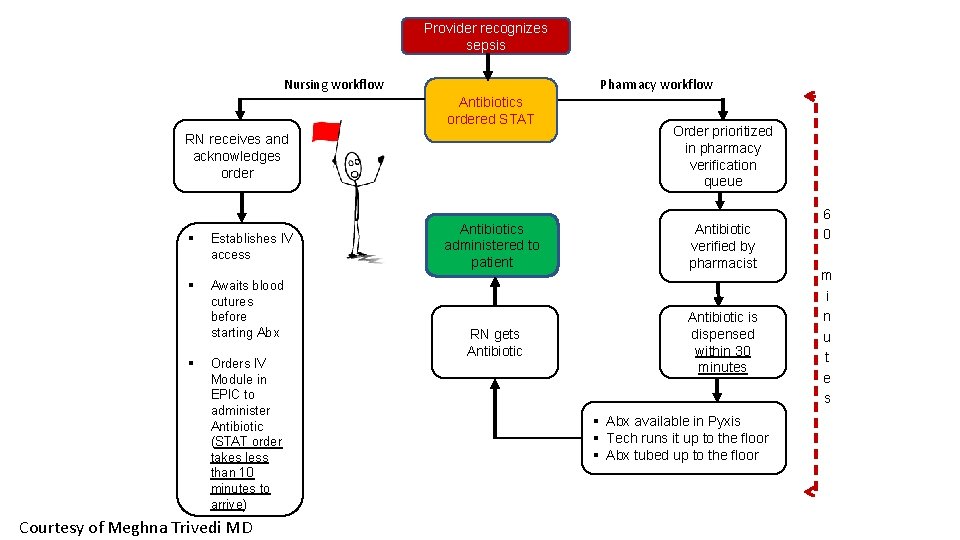
Provider recognizes sepsis Nursing workflow Pharmacy workflow Antibiotics ordered STAT RN receives and acknowledges order § Establishes IV access § Awaits blood cutures before starting Abx § Orders IV Module in EPIC to administer Antibiotic (STAT order takes less than 10 minutes to arrive) Courtesy of Meghna Trivedi MD Order prioritized in pharmacy verification queue Antibiotics administered to patient Antibiotic verified by pharmacist RN gets Antibiotic is dispensed within 30 minutes § Abx available in Pyxis § Tech runs it up to the floor § Abx tubed up to the floor 6 0 m i n u t e s
Time to Antibiotics Order sets Cultures first! STAT Orders
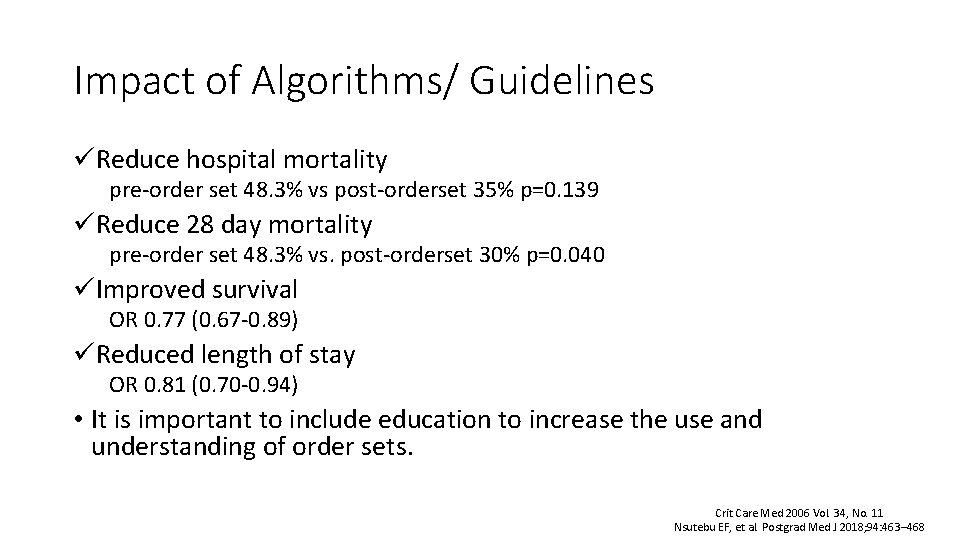
Impact of Algorithms/ Guidelines üReduce hospital mortality pre-order set 48. 3% vs post-orderset 35% p=0. 139 üReduce 28 day mortality pre-order set 48. 3% vs. post-orderset 30% p=0. 040 üImproved survival OR 0. 77 (0. 67 -0. 89) üReduced length of stay OR 0. 81 (0. 70 -0. 94) • It is important to include education to increase the use and understanding of order sets. Crit Care Med 2006 Vol. 34, No. 11 Nsutebu EF, et al. Postgrad Med J 2018; 94: 463– 468
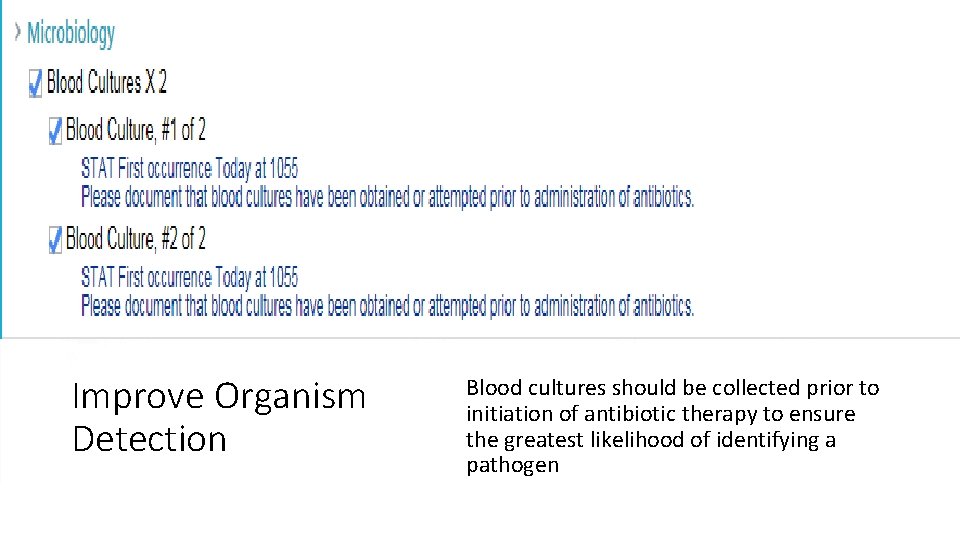
Improve Organism Detection Blood cultures should be collected prior to initiation of antibiotic therapy to ensure the greatest likelihood of identifying a pathogen
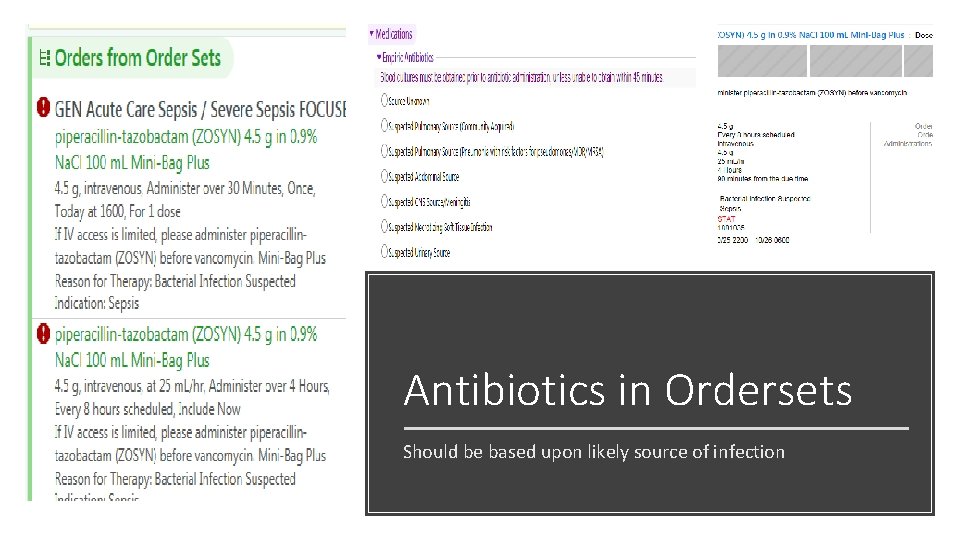
Antibiotics in Ordersets Should be based upon likely source of infection
Antibiotic Choice Base upon location of suspected infection Local susceptibilities Risk factors for multi-drug resistant organisms (MDRO)
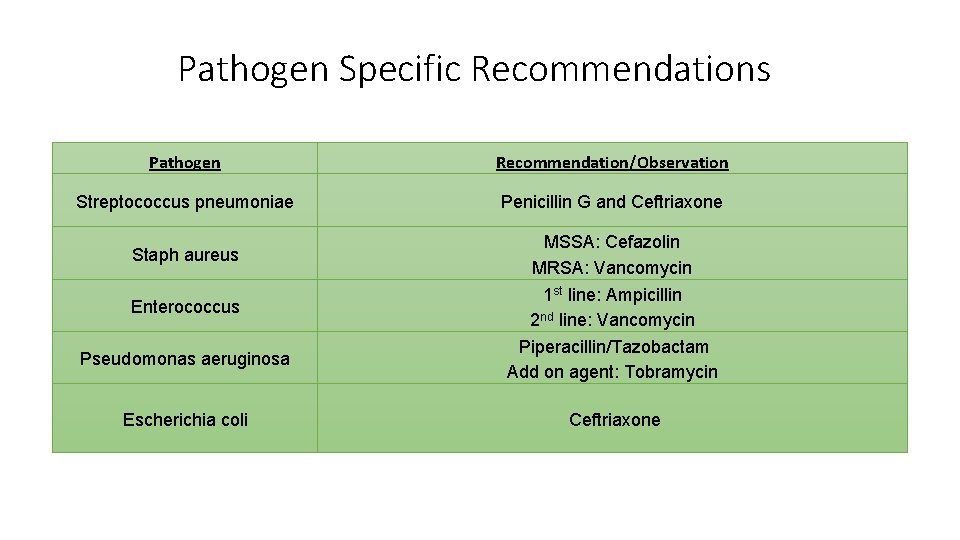
Pathogen Specific Recommendations Pathogen Recommendation/Observation Streptococcus pneumoniae Penicillin G and Ceftriaxone Staph aureus Enterococcus Pseudomonas aeruginosa Escherichia coli MSSA: Cefazolin MRSA: Vancomycin 1 st line: Ampicillin 2 nd line: Vancomycin Piperacillin/Tazobactam Add on agent: Tobramycin Ceftriaxone
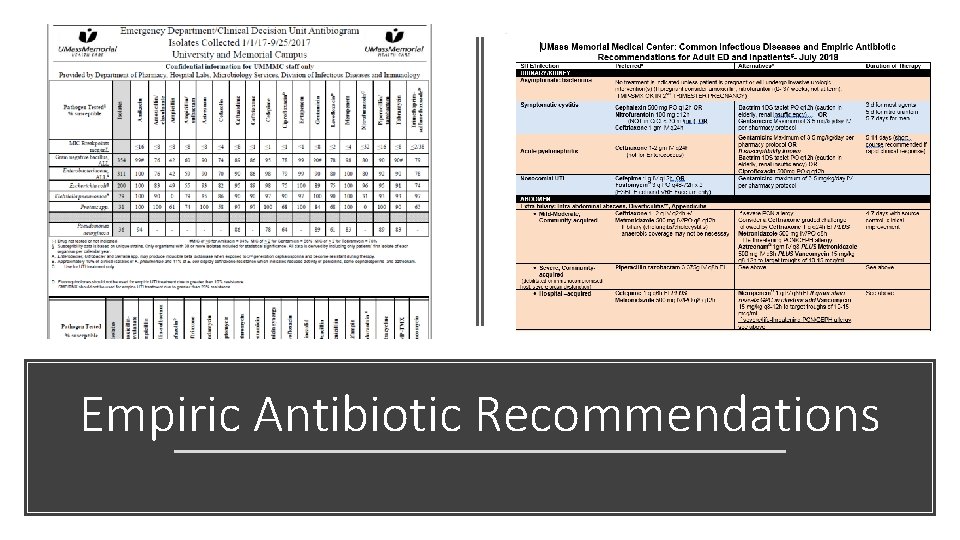
Empiric Antibiotic Recommendations

Risk Factors for MDRO/Health Care Associated Pathogens IV broad spectrum antibiotics within 90 days History of MDRO Local high antibiotic resistance rates Chronic dialysis within 30 days Renal replacement therapy with last 30 days Home wound care Mechanical ventilation greater than 5 days Immunosuppression (HIV/AIDS, hematologic cancer, solid cancers on chemotherapy, corticosteroids, treatment with immunosuppressive drugs, etc. ). • Central venous catheter • Hospitalization greater than 5 days • Residence in a LTAC • • Clinical Infectious Diseases, 2016; 63: 61–e 111, Clinical Infectious Diseases 2017; 65: 1607 -1614 Infect Control Hosp Epidemiol 2017; 38: 266– 272
How do you optimize it? Pharmacokinetic/ pharmacodynamic optimization Rapid diagnostics
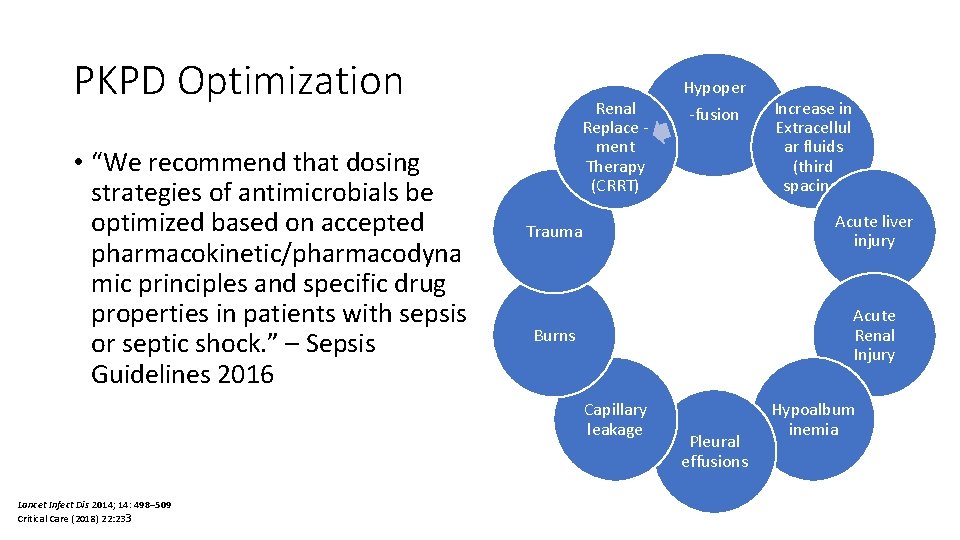
PKPD Optimization • “We recommend that dosing strategies of antimicrobials be optimized based on accepted pharmacokinetic/pharmacodyna mic principles and specific drug properties in patients with sepsis or septic shock. ” – Sepsis Guidelines 2016 Renal Replace ment Therapy (CRRT) Increase in Extracellul ar fluids (third spacing) Trauma Acute liver injury Burns Acute Renal Injury Capillary leakage Lancet Infect Dis 2014; 14: 498– 509 Critical Care (2018) 22: 233 Hypoper -fusion Pleural effusions Hypoalbum inemia
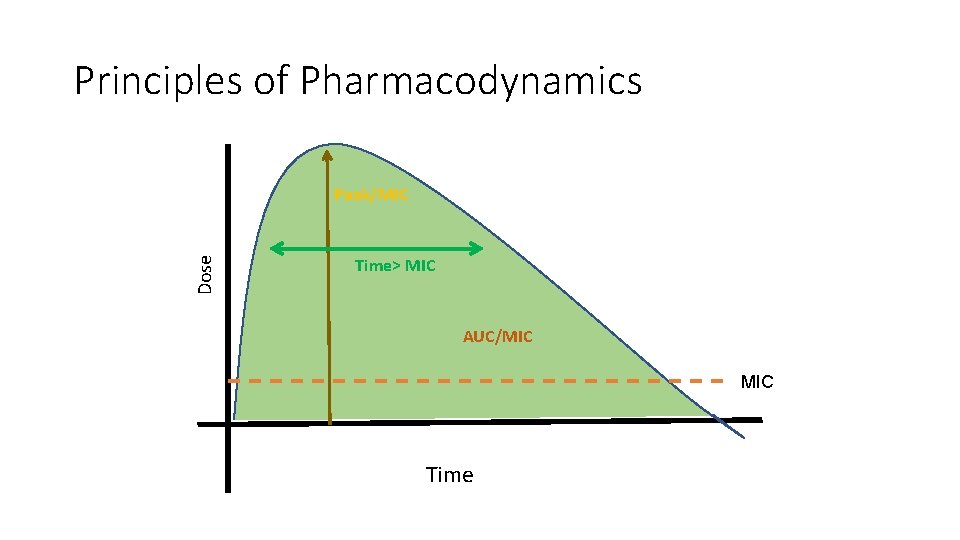
Principles of Pharmacodynamics Dose Peak/MIC Time> MIC AUC/MIC Time

Pharmacokinetics/Pharmacodynamics • MIC- Minimum Inhibitory Concentration • The lowest required concentration to inhibit growth • Specific to each antibiotic and organism Susceptible Intermediate Resistant Organism can be eradicated Requires higher doses or concentration to achieve efficacy Less than optimal results
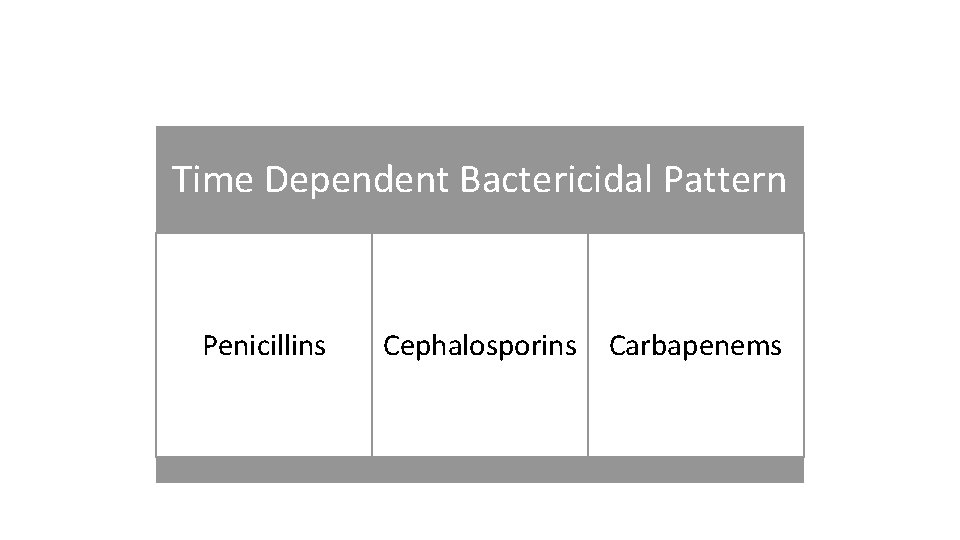
Time Dependent Bactericidal Pattern Penicillins Cephalosporins Carbapenems
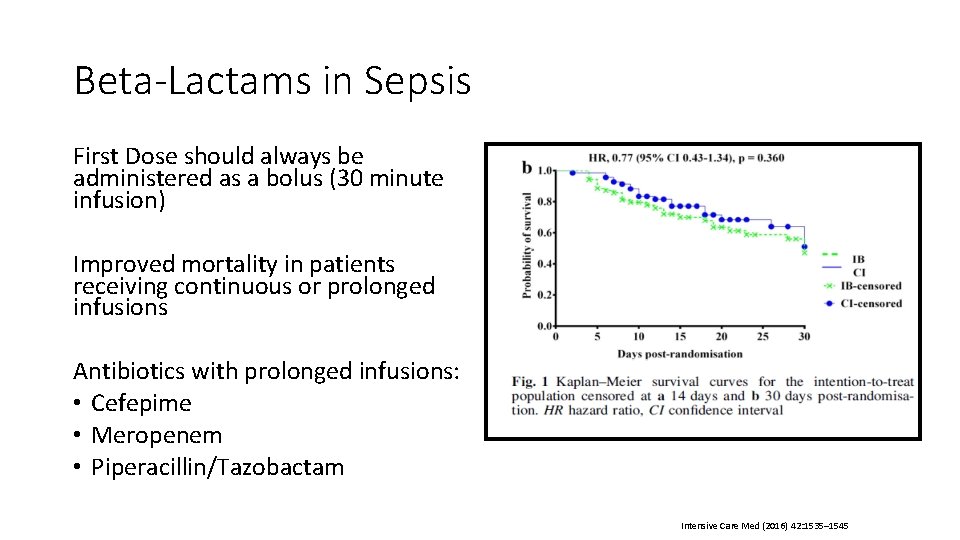
Beta-Lactams in Sepsis First Dose should always be administered as a bolus (30 minute infusion) Improved mortality in patients receiving continuous or prolonged infusions Antibiotics with prolonged infusions: • Cefepime • Meropenem • Piperacillin/Tazobactam Intensive Care Med (2016) 42: 1535– 1545
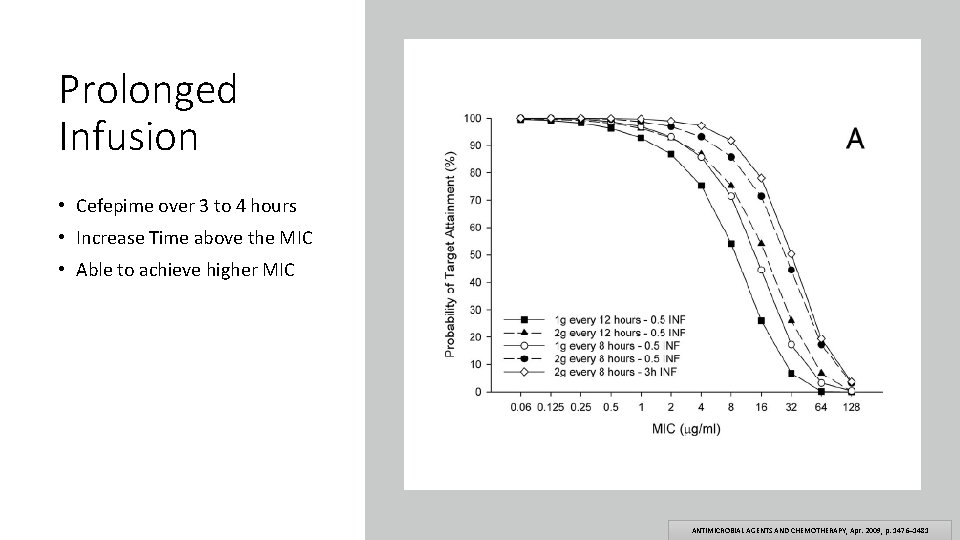
Prolonged Infusion • Cefepime over 3 to 4 hours • Increase Time above the MIC • Able to achieve higher MIC ANTIMICROBIAL AGENTS AND CHEMOTHERAPY, Apr. 2009, p. 1476– 1481
Concentration Dependent Bactericidal Pattern Daptomycin Quinolones Aminoglycosides Metronidazole
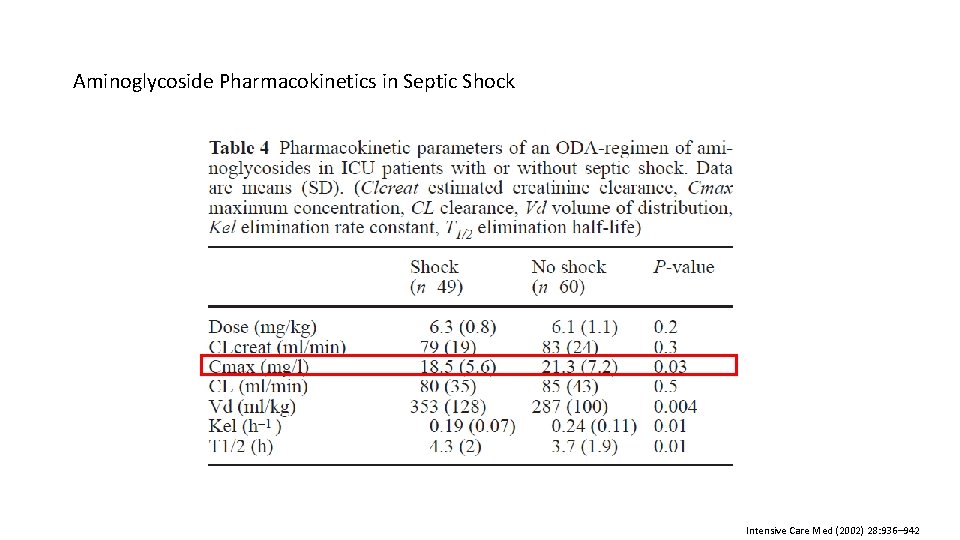
Aminoglycoside Pharmacokinetics in Septic Shock Intensive Care Med (2002) 28: 936– 942
AUC/MIC Tetracyclines Vancomycin Azithromycin Clindamycin
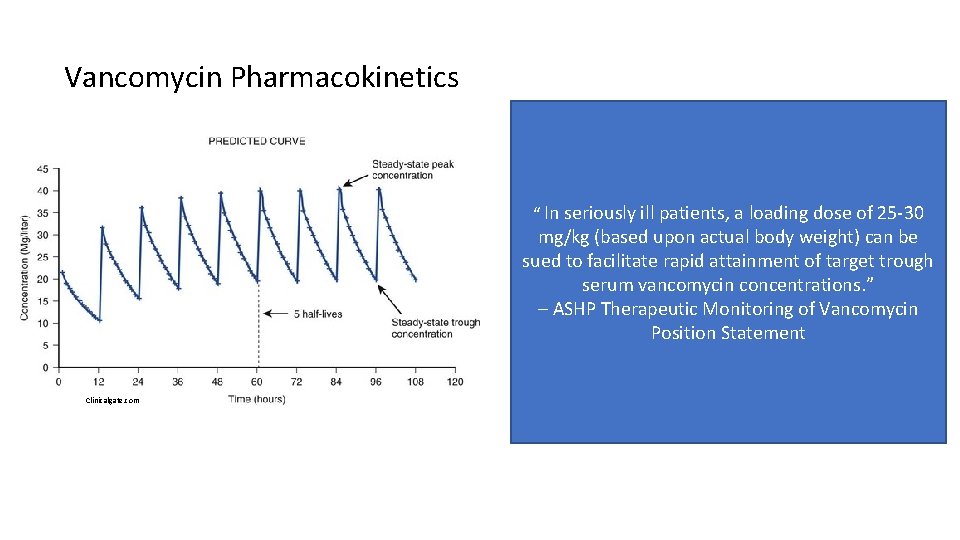
Vancomycin Pharmacokinetics “ In seriously ill patients, a loading dose of 25 -30 mg/kg (based upon actual body weight) can be sued to facilitate rapid attainment of target trough serum vancomycin concentrations. ” – ASHP Therapeutic Monitoring of Vancomycin Position Statement Clinicalgate. com
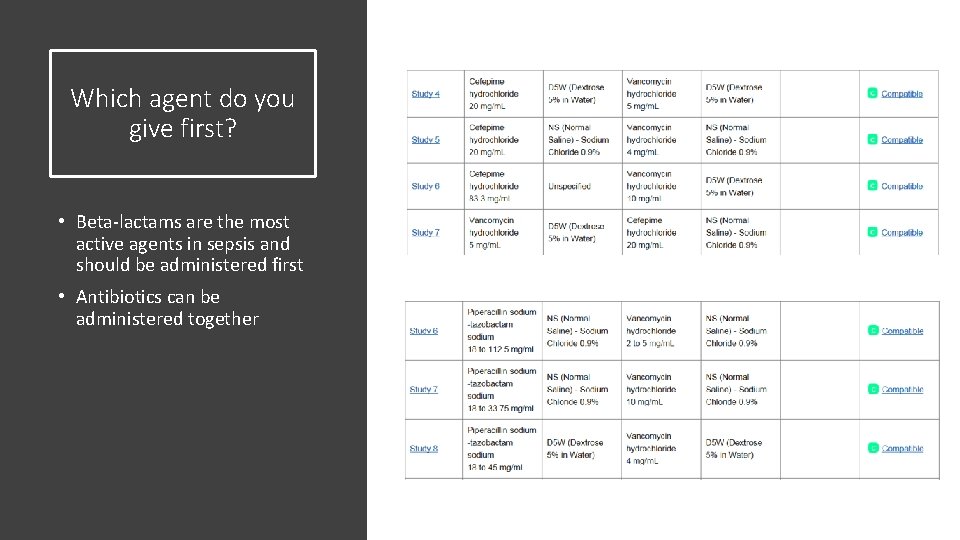
Which agent do you give first? • Beta-lactams are the most active agents in sepsis and should be administered first • Antibiotics can be administered together
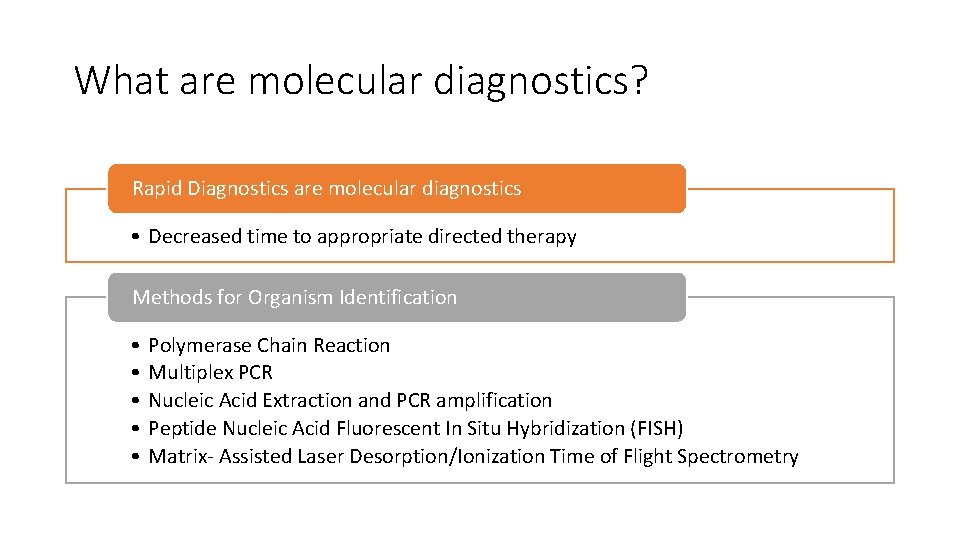
What are molecular diagnostics? Rapid Diagnostics are molecular diagnostics • Decreased time to appropriate directed therapy Methods for Organism Identification • • • Polymerase Chain Reaction Multiplex PCR Nucleic Acid Extraction and PCR amplification Peptide Nucleic Acid Fluorescent In Situ Hybridization (FISH) Matrix- Assisted Laser Desorption/Ionization Time of Flight Spectrometry
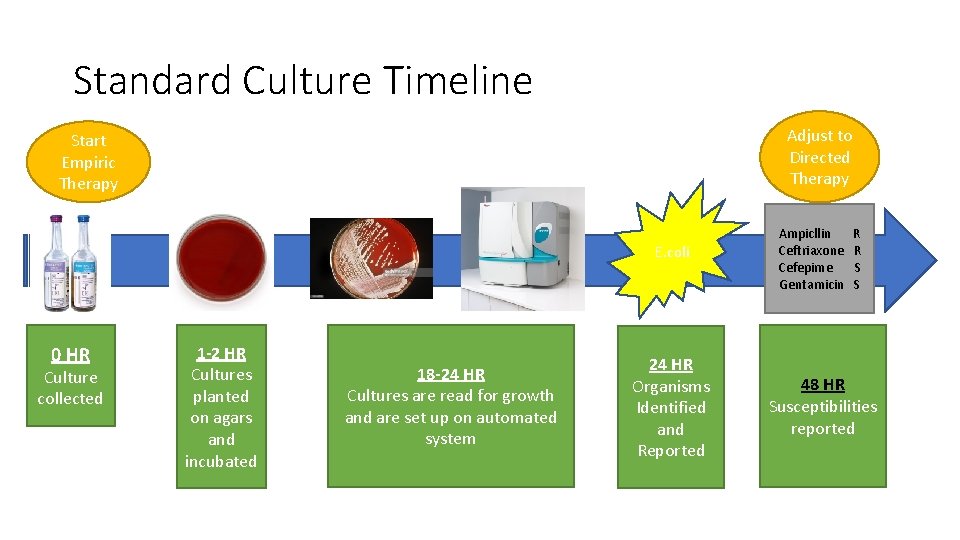
Standard Culture Timeline Adjust to Directed Therapy Start Empiric Therapy E. coli 0 HR Culture collected 1 -2 HR Cultures planted on agars and incubated 18 -24 HR Cultures are read for growth and are set up on automated system 24 HR Organisms Identified and Reported Ampicllin Ceftriaxone Cefepime Gentamicin R R S S 48 HR Susceptibilities reported
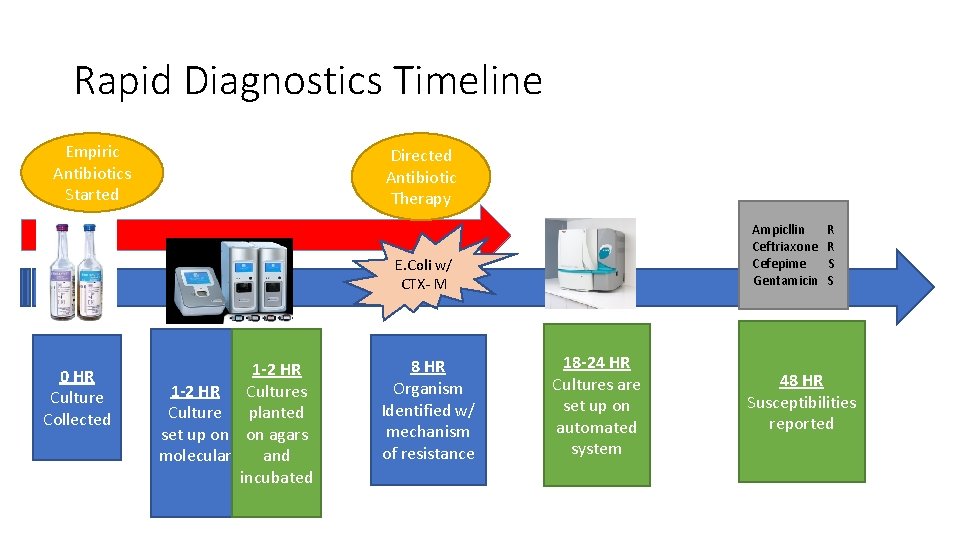
Rapid Diagnostics Timeline Empiric Antibiotics Started Directed Antibiotic Therapy Ampicllin Ceftriaxone Cefepime Gentamicin E. Coli w/ CTX- M 0 HR Culture Collected 1 -2 HR Cultures Culture planted set up on on agars molecular and incubated 8 HR Organism Identified w/ mechanism of resistance 18 -24 HR Cultures are set up on automated system R R S S 48 HR Susceptibilities reported
Minimize Adverse Events De-escalation of therapy Narrowing therapy
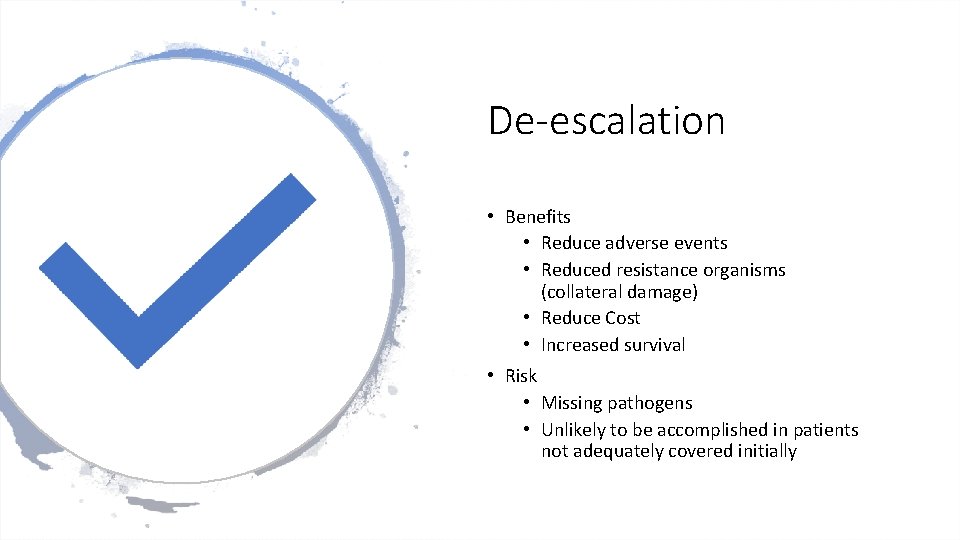
De-escalation • Benefits • Reduce adverse events • Reduced resistance organisms (collateral damage) • Reduce Cost • Increased survival • Risk • Missing pathogens • Unlikely to be accomplished in patients not adequately covered initially
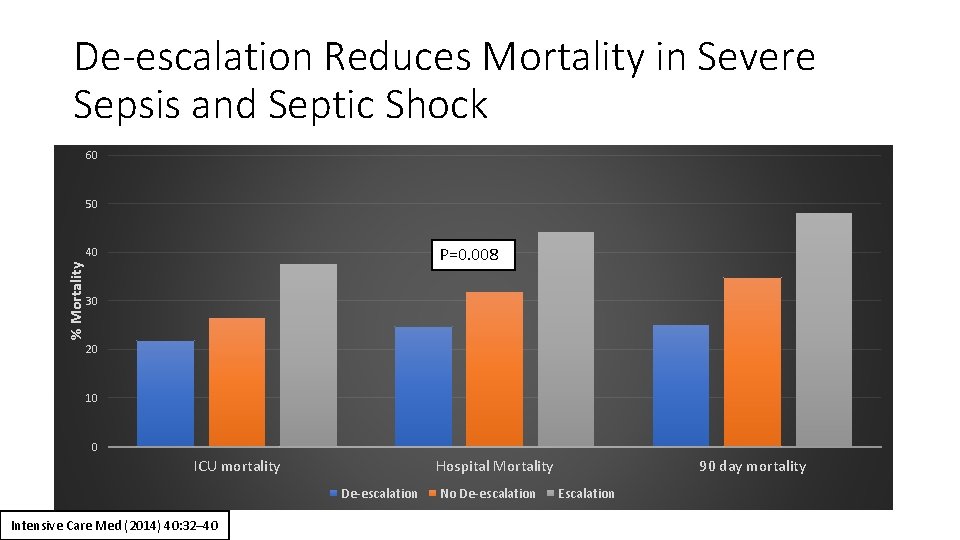
De-escalation Reduces Mortality in Severe Sepsis and Septic Shock 60 50 P=0. 008 % Mortality 40 30 20 10 0 ICU mortality Hospital Mortality De-escalation Intensive Care Med (2014) 40: 32– 40 No De-escalation 90 day mortality Escalation
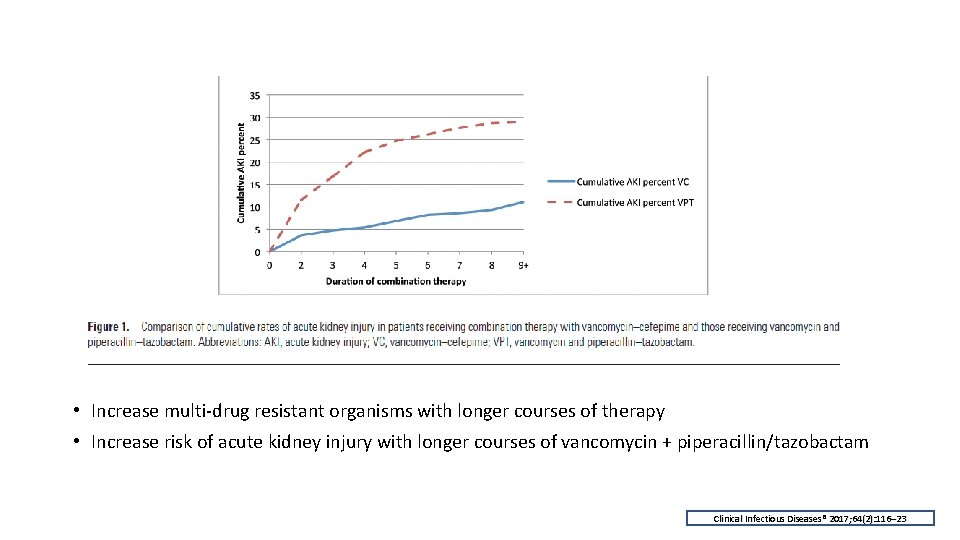
Adverse Events • Increase multi-drug resistant organisms with longer courses of therapy • Increase risk of acute kidney injury with longer courses of vancomycin + piperacillin/tazobactam Clinical Infectious Diseases® 2017; 64(2): 116– 23
Objectives • Identify the role of antibiotics in sepsis • Antibiotics reduce mortality when given early in sepsis • Describe the challenges to timely antibiotic administrations • Hard to identify time zero • Not using STAT on antibiotics orders • Lack of communication between team members • List 3 ways to optimize antibiotics in sepsis • Administer beta-lactams as prolonged infusions • Administer aminoglycosides at higher doses • Administer compatible antibiotics at the same time if line access allows • Understand the importance of de-escalation of antibiotics in sepsis • Reduce adverse events (AKI) • Improved survival • Reduce length of hospital stay
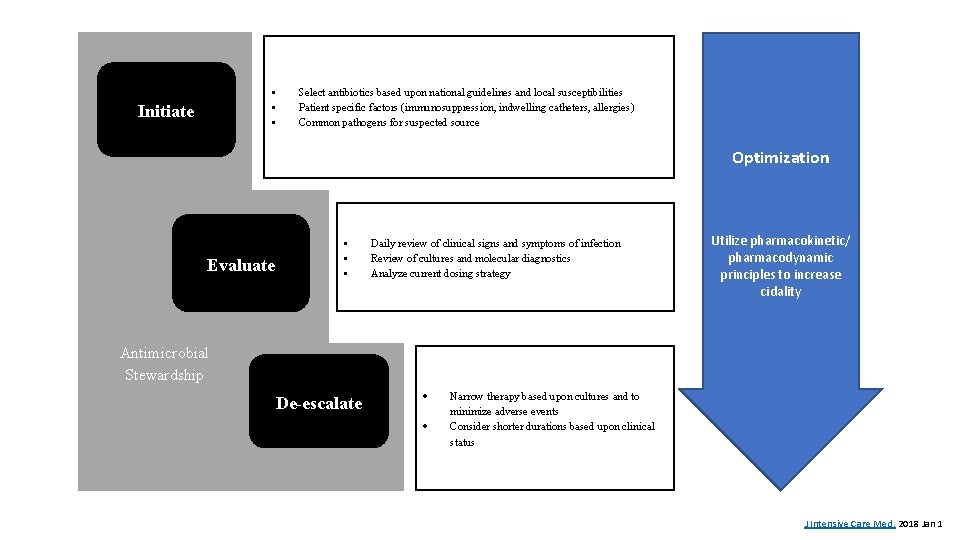
• • • Initiate Select antibiotics based upon national guidelines and local susceptibilities Patient specific factors (immunosuppression, indwelling catheters, allergies) Common pathogens for suspected source Optimization Evaluate • • • Daily review of clinical signs and symptoms of infection Review of cultures and molecular diagnostics Analyze current dosing strategy Utilize pharmacokinetic/ pharmacodynamic principles to increase cidality Antimicrobial Stewardship De-escalate Narrow therapy based upon cultures and to minimize adverse events Consider shorter durations based upon clinical status J Intensive Care Med. 2018 Jan 1
Antibiotic Use in Sepsis and Stewardship Maureen Campion, Pharm. D Clinical Pharmacy Specialist- Infectious Disease UMass Memorial Medical Center
- Slides: 39