Antiallergic drugs MR AYDIN MD Assoc Prof Ankara



- Slides: 39
Anti-allergic drugs ÖMÜR AYDIN, MD, Assoc. Prof. Ankara University School of Medicine Dept of Allergy and Clinical Immunology
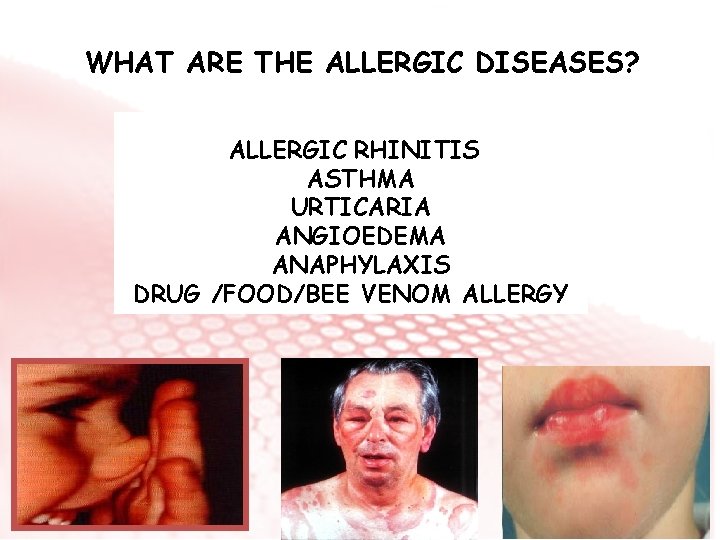
WHAT ARE THE ALLERGIC DISEASES? ALLERGIC RHINITIS ASTHMA URTICARIA ANGIOEDEMA ANAPHYLAXIS DRUG /FOOD/BEE VENOM ALLERGY
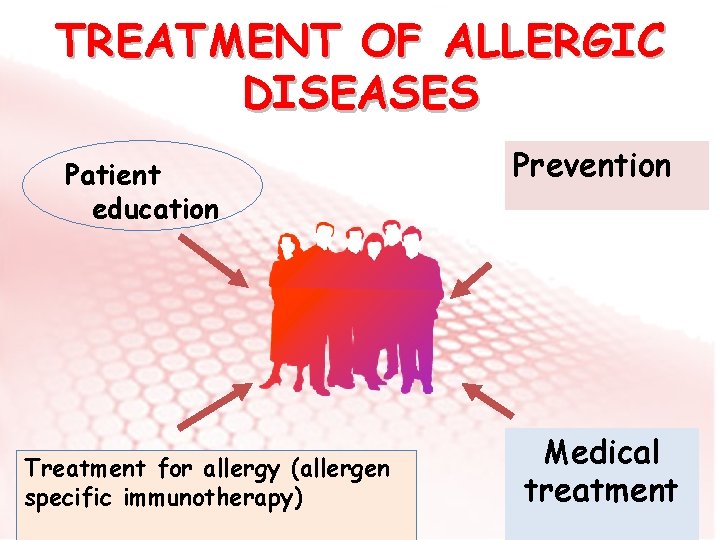
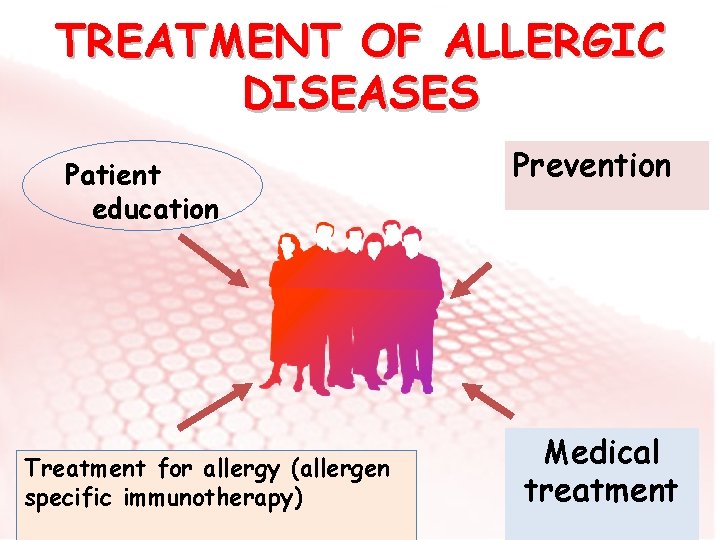
TREATMENT OF ALLERGIC DISEASES Patient education Treatment for allergy (allergen specific immunotherapy) Prevention Medical treatment
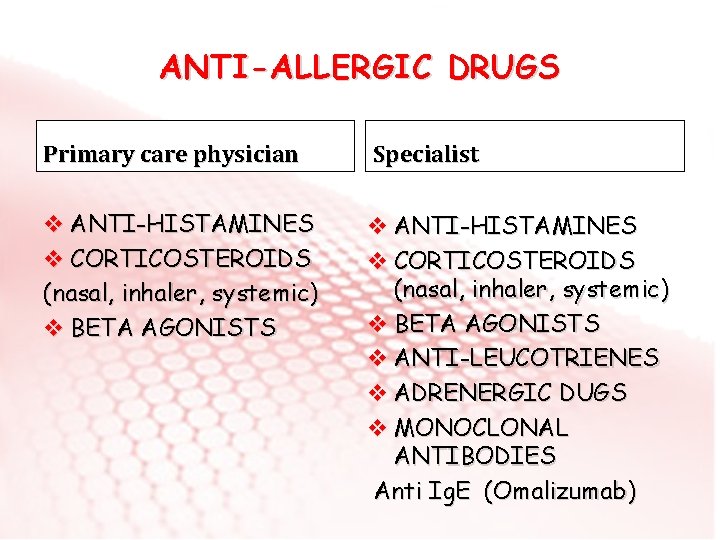
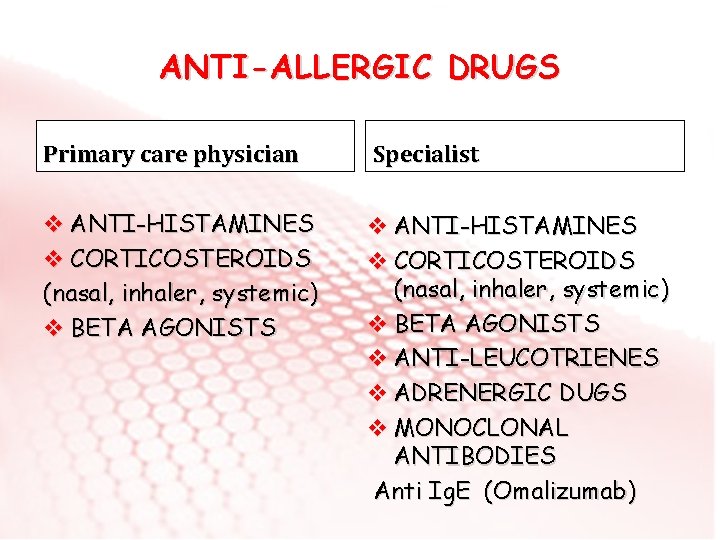
ANTI-ALLERGIC DRUGS Primary care physician Specialist v ANTI-HISTAMINES v CORTICOSTEROIDS (nasal, inhaler, systemic) v BETA AGONISTS v ANTI-LEUCOTRIENES v ADRENERGIC DUGS v MONOCLONAL ANTIBODIES Anti Ig. E (Omalizumab)
v ANTI-HISTAMINES H 1 receptor blokers are used. Bind to histamin receptor competetively and reverses the effects of histamine. Indications: v. Respiratory allergies (Rhinoconjunctivitis) v. Skin allergies (Urticaria, angioedema) v. Other allergies
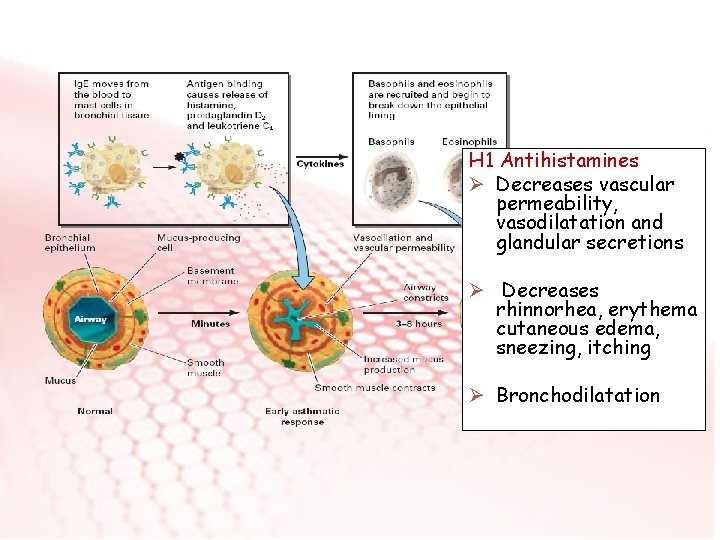
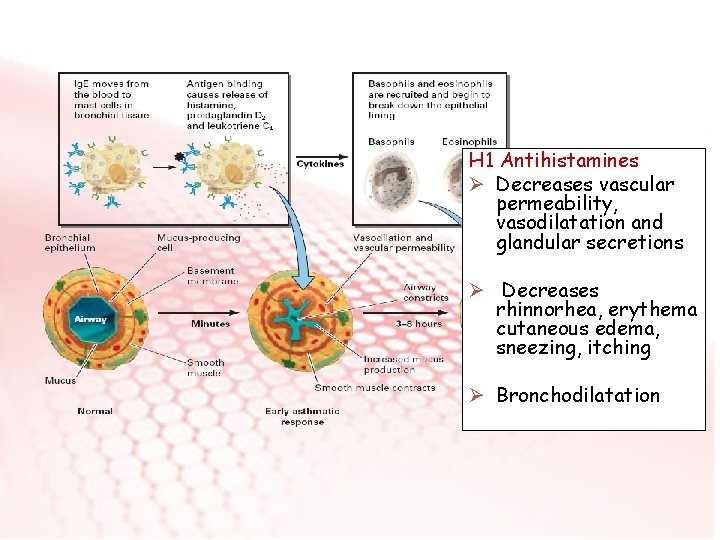
H 1 Antihistamines Ø Decreases vascular permeability, vasodilatation and glandular secretions Ø Decreases rhinnorhea, erythema cutaneous edema, sneezing, itching Ø Bronchodilatation
H 1 Antihistamines v. Oral, vtopical (nasal, ophtalmic), vparenteral forms are available
1 st generation H 1 Antihistamines Ø Azatadine Ø Brompheniramine Ø Klorpheniramine Ø Siproheptadine Ø Difenhidramine Ø Hydroxyzine Ø Tripellenamine Ø Ketotifen
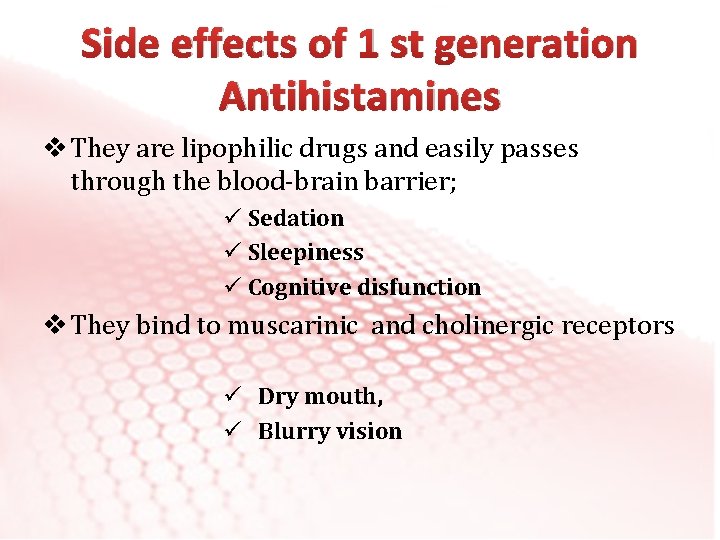
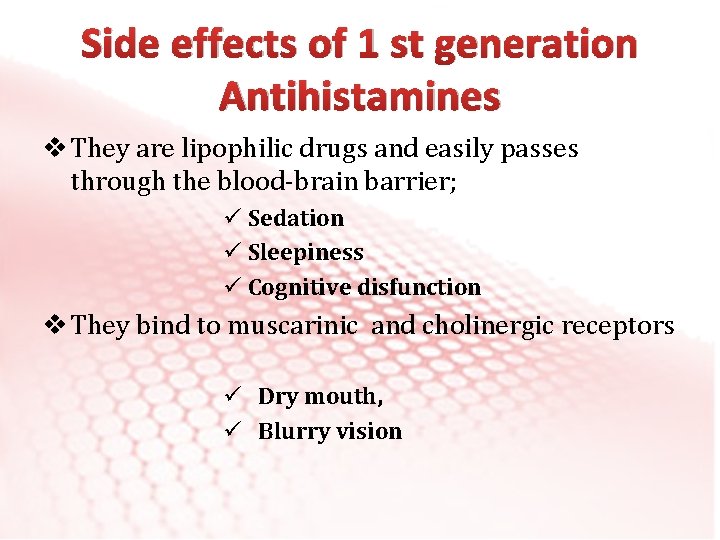
Side effects of 1 st generation Antihistamines v They are lipophilic drugs and easily passes through the blood-brain barrier; ü Sedation ü Sleepiness ü Cognitive disfunction v They bind to muscarinic and cholinergic receptors ü Dry mouth, ü Blurry vision
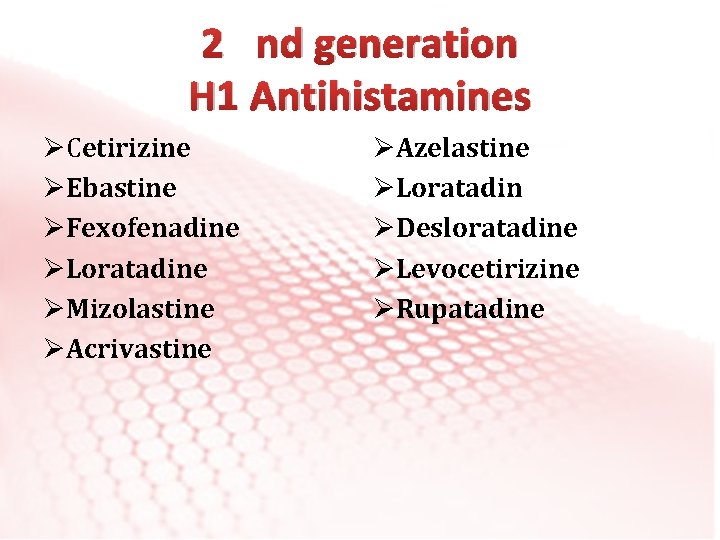
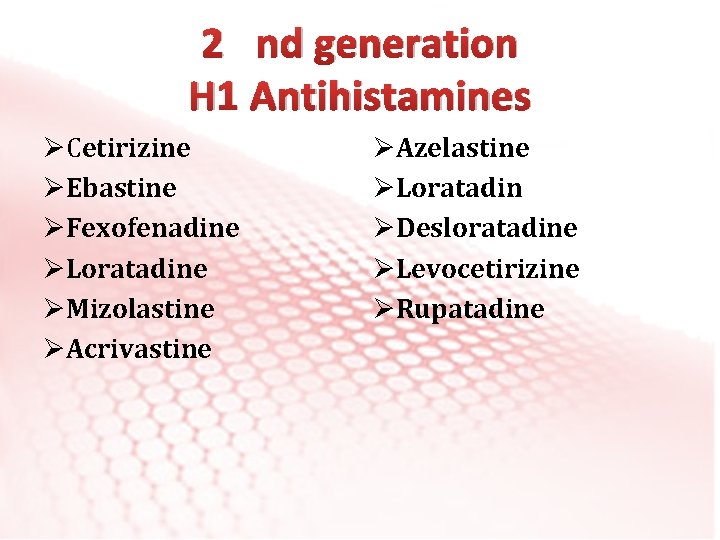
2 nd generation H 1 Antihistamines ØCetirizine ØEbastine ØFexofenadine ØLoratadine ØMizolastine ØAcrivastine ØAzelastine ØLoratadin ØDesloratadine ØLevocetirizine ØRupatadine
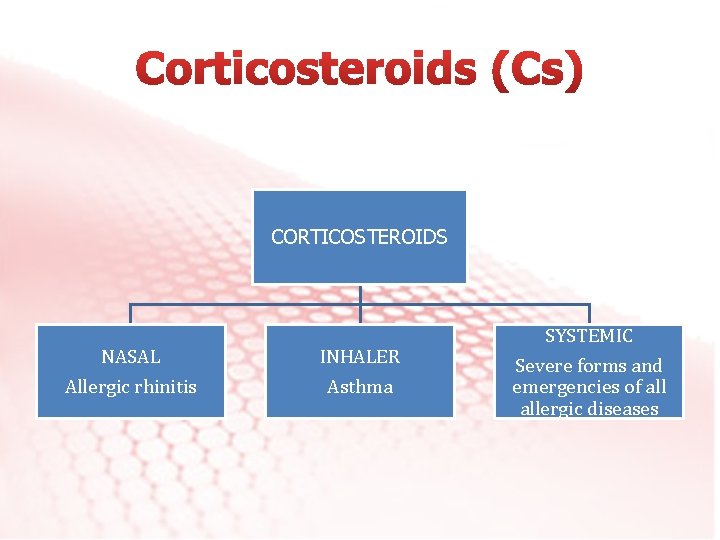
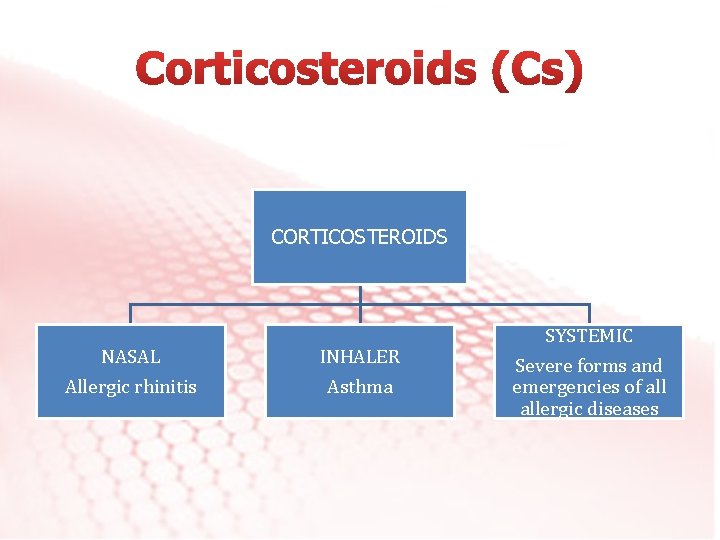
CORTICOSTEROIDS NASAL Allergic rhinitis INHALER Asthma SYSTEMIC Severe forms and emergencies of allergic diseases
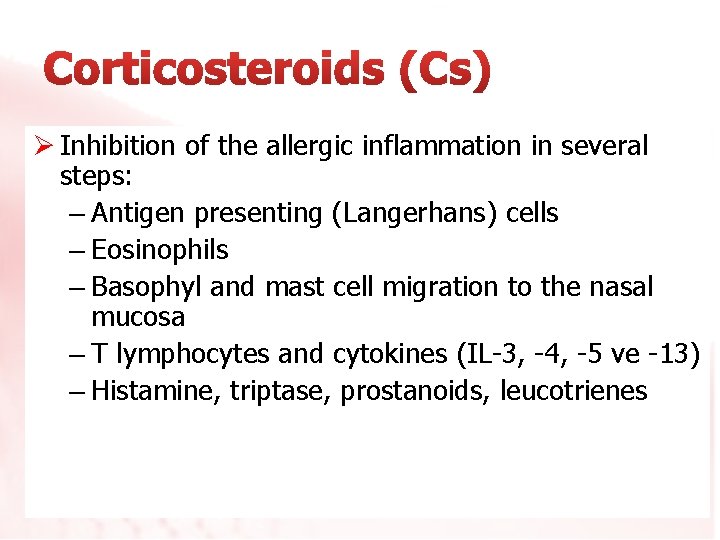
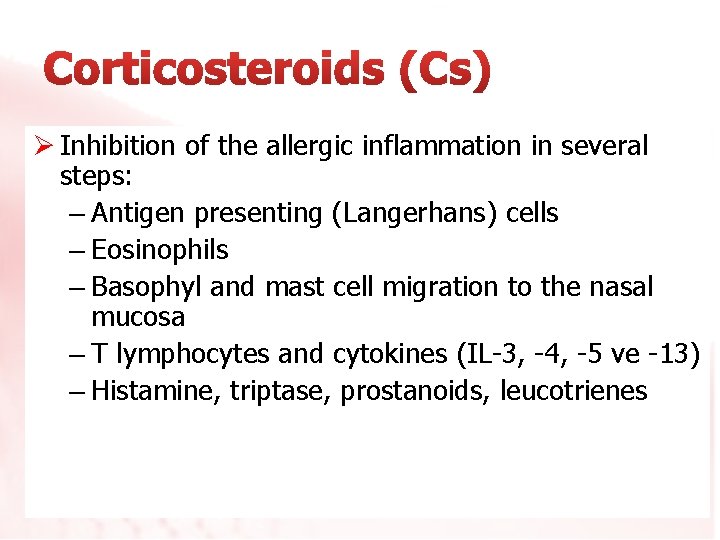
Ø Inhibition of the allergic inflammation in several steps: – Antigen presenting (Langerhans) cells – Eosinophils – Basophyl and mast cell migration to the nasal mucosa – T lymphocytes and cytokines (IL-3, -4, -5 ve -13) – Histamine, triptase, prostanoids, leucotrienes
Ø Decreases the symptoms of rhinitis (sneezing, rhinorhea, itchy nose, nasal obstruction). Ø Effect starts later than antihistamines.
Ø Beclomethasone dipropionate Ø Budesonide Ø Flunisolide Ø Fluticasone propionate Ø Fluticasone furoate Ø Mometasone furoate Ø Triamcinolone acetonide Ø Ciclesonide
• Local – Dry nose – Bleeding – Septal perforation: Rare. Must be sprayed towards the lateral wall of the nose
Used for asthma treatment Decreases airway inflammation Qo. L Symptoms Pulmonary functions BHR Asthma exacerbations, hospitalizations improvement
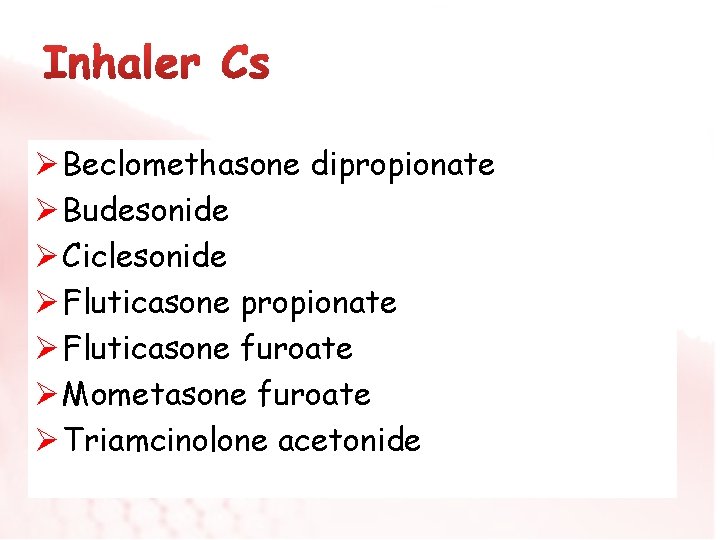
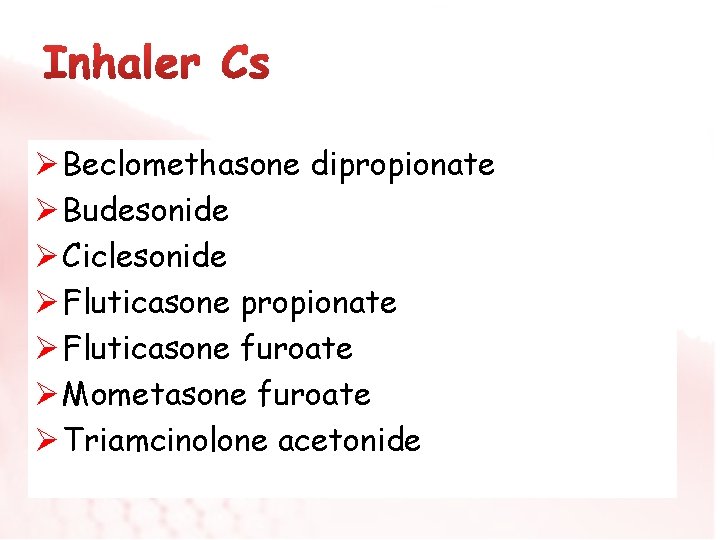
Ø Beclomethasone dipropionate Ø Budesonide Ø Ciclesonide Ø Fluticasone propionate Ø Fluticasone furoate Ø Mometasone furoate Ø Triamcinolone acetonide
• Local (common side effects) Hoarseness Cough Oral candida • Systemic (rare) Adrenal supression Cataract Glaucoma
Systemic Cs ü Most effective anti-inflammatory drugs that supresses chemokines and citokines ü Daily dose (40 -60 mg/day methyl prednisolon or equivalent)
When to use Systemic Cs Used when we plan a short term but fast treatment ü Asthma attack: short course ü Step 5 severe asthma: short/long corse ü Severe persistant allergic rhinitis when not responded to drugs: short course ü Anaphylaxis: short course ü Urticaria- angioedema: short/long corse
Systemic Cs Side effects; ü Diabetes ü ü Osteopozis Myopathy Cushing Cataract
Epinephrine (Adrenalin) v. Stimulates alfa and beta adrenergic reseptors directly v. First choice drug in anaphylaxis treatment v Main therapeutic effect: bronchodilatation, cardiac stimulation, skeletal muscle relaxation
v. CNS; tremor, agitation, headache, disorientation, serebral hemorhage v. CVS; palpitation, tachycardia, hipertension, ven tricular fibrilation, angina, arithmia v Methabolic; Hyperglycemia, lactic acidosis v. Skin; urticaria, local pain at injection-site
v 1 -adrenergic agonist: Phenylephrin v 2 -adrenergic agonist: Oximethasoline, Xsilomethasoline v. Noradrenalin secreting agents: Ephedrin, pseudoephedrin
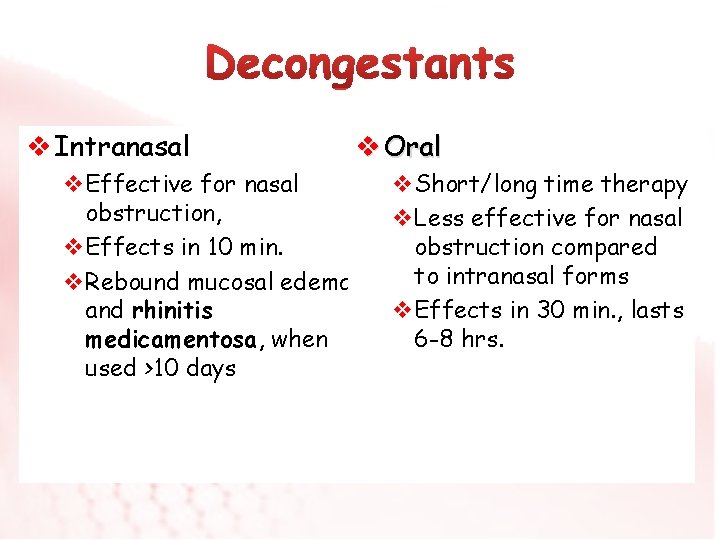
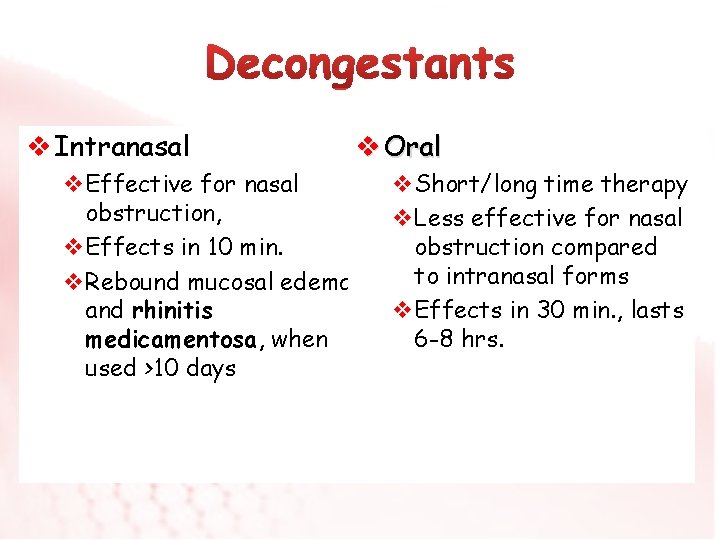
v Intranasal v. Effective for nasal obstruction, v. Effects in 10 min. v. Rebound mucosal edema and rhinitis medicamentosa, when used >10 days v Oral v. Short/long time therapy v. Less effective for nasal obstruction compared to intranasal forms v. Effects in 30 min. , lasts 6 -8 hrs.
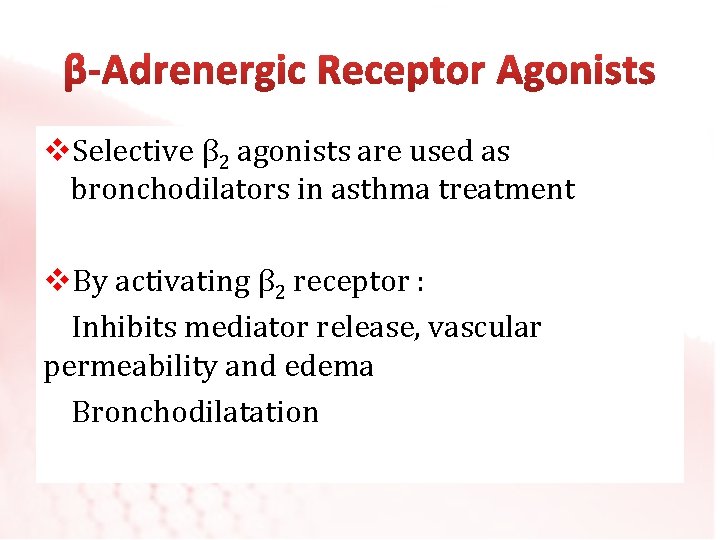
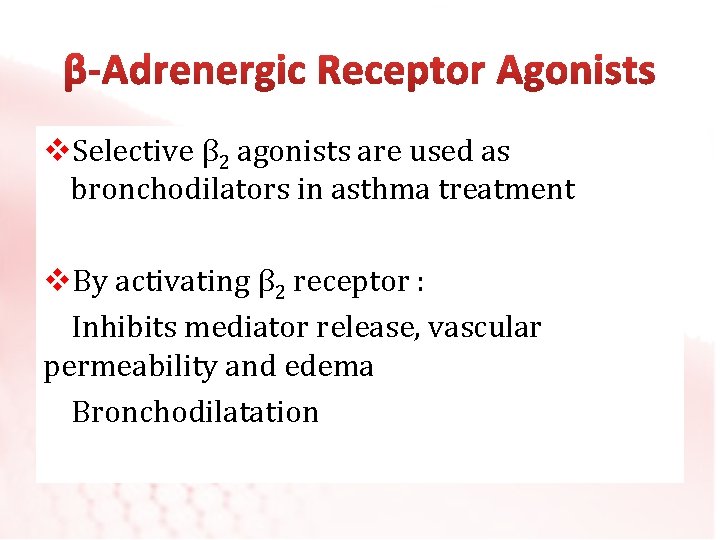
v. Selective β 2 agonists are used as bronchodilators in asthma treatment v. By activating β 2 receptor : Inhibits mediator release, vascular permeability and edema Bronchodilatation
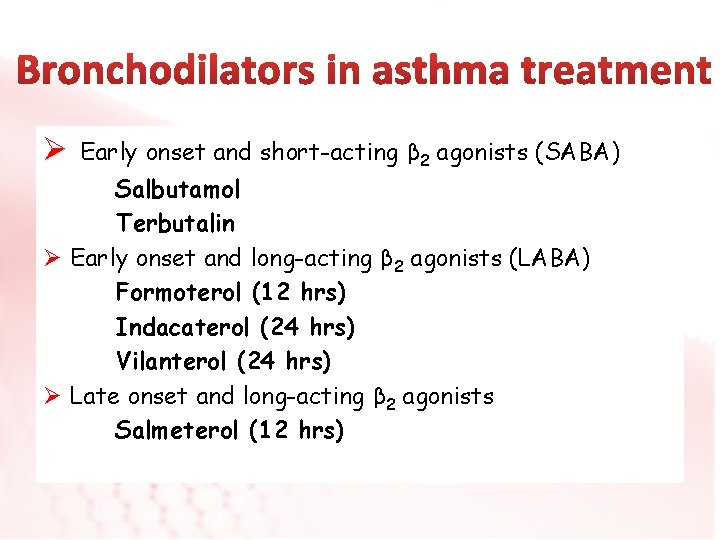
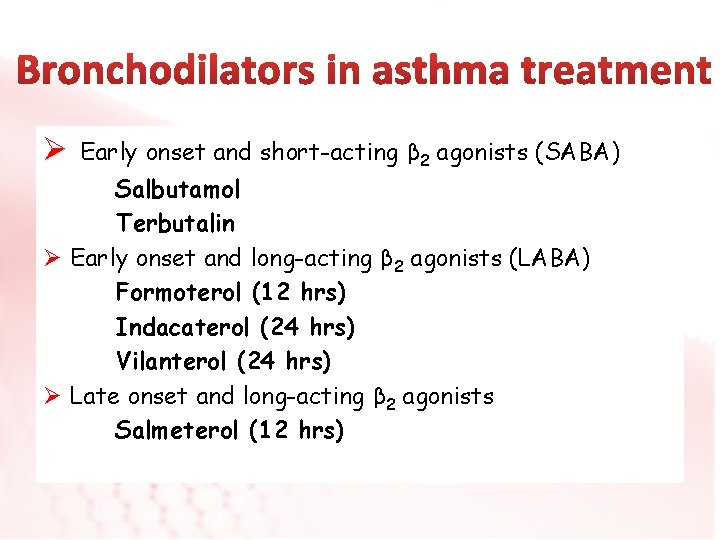
Ø Early onset and short-acting β 2 agonists (SABA) Salbutamol Terbutalin Ø Early onset and long-acting β 2 agonists (LABA) Formoterol (12 hrs) Indacaterol (24 hrs) Vilanterol (24 hrs) Ø Late onset and long-acting β 2 agonists Salmeterol (12 hrs)
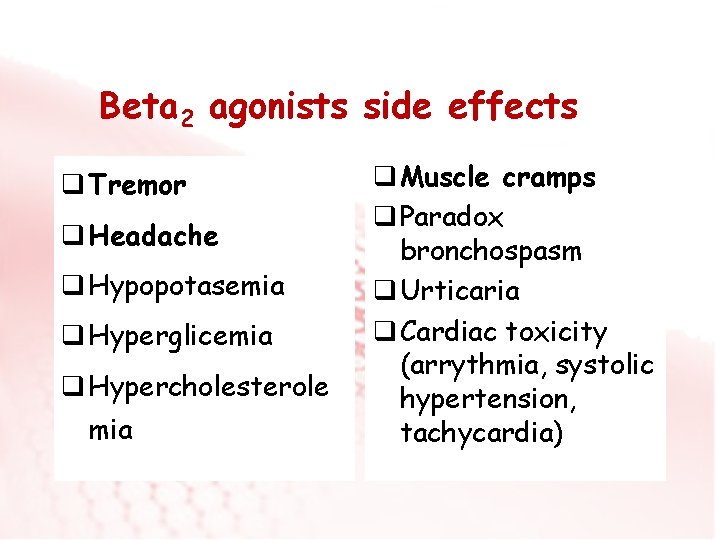
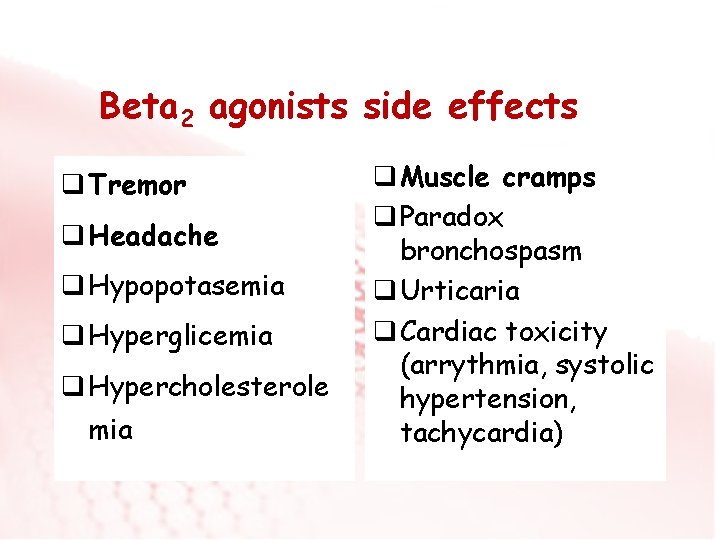
Beta 2 agonists side effects q Tremor q Headache q Hypopotasemia q Hyperglicemia q Hypercholesterole mia q Muscle cramps q Paradox bronchospasm q Urticaria q Cardiac toxicity (arrythmia, systolic hypertension, tachycardia)
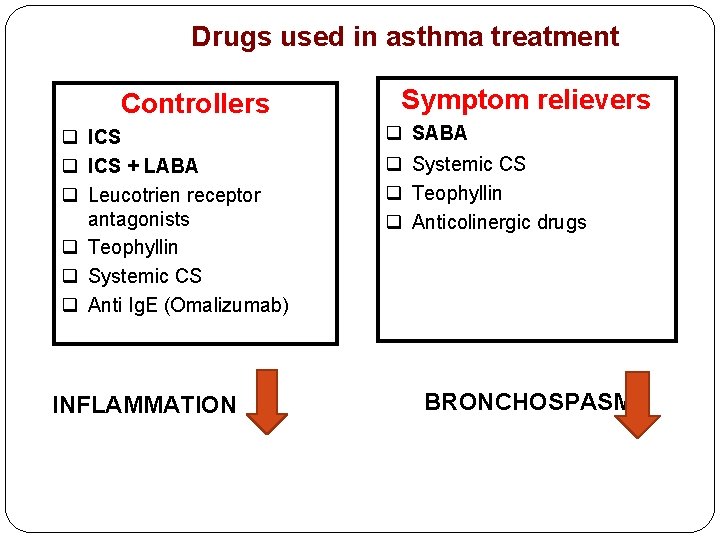
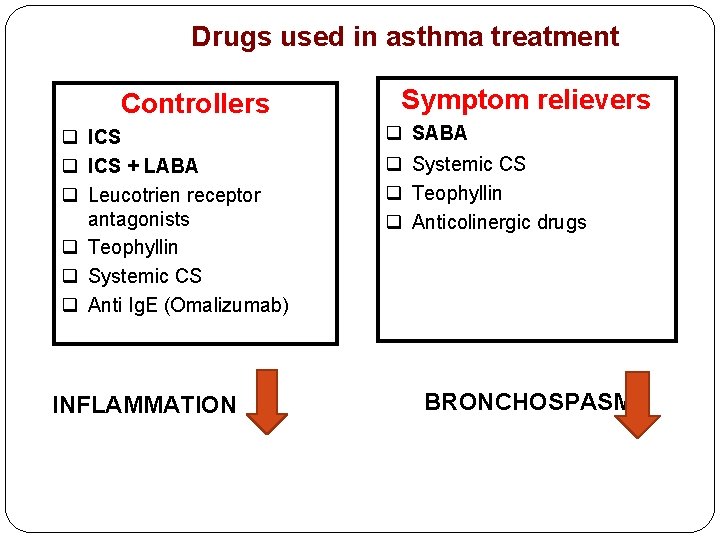
Drugs used in asthma treatment Controllers q ICS + LABA q Leucotrien receptor antagonists q Teophyllin q Systemic CS q Anti Ig. E (Omalizumab) INFLAMMATION Symptom relievers q SABA q Systemic CS q Teophyllin q Anticolinergic drugs BRONCHOSPASM
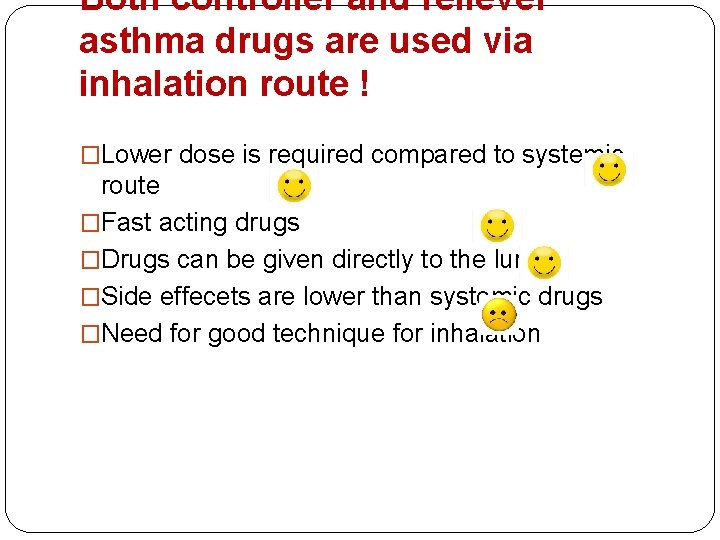
Both controller and reliever asthma drugs are used via inhalation route ! �Lower dose is required compared to systemic route �Fast acting drugs �Drugs can be given directly to the lungs �Side effecets are lower than systemic drugs �Need for good technique for inhalation

INHALER DEVICES Metered dose inhalers (MDI) Dry powder inhalers (DPI) Space rs
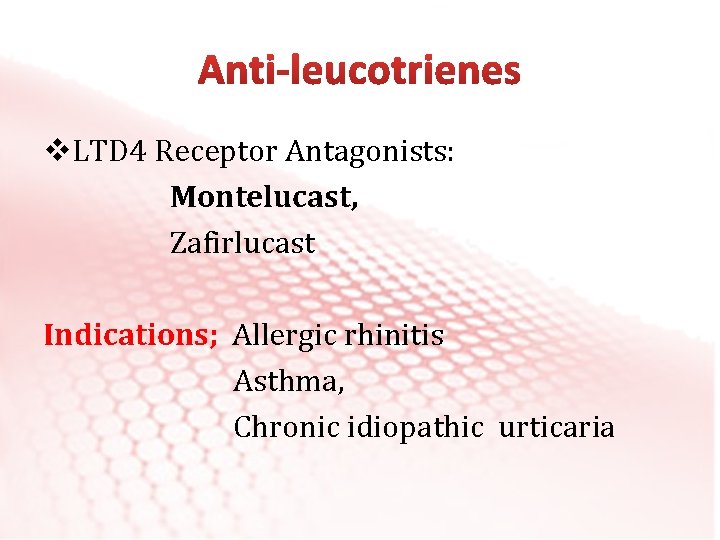
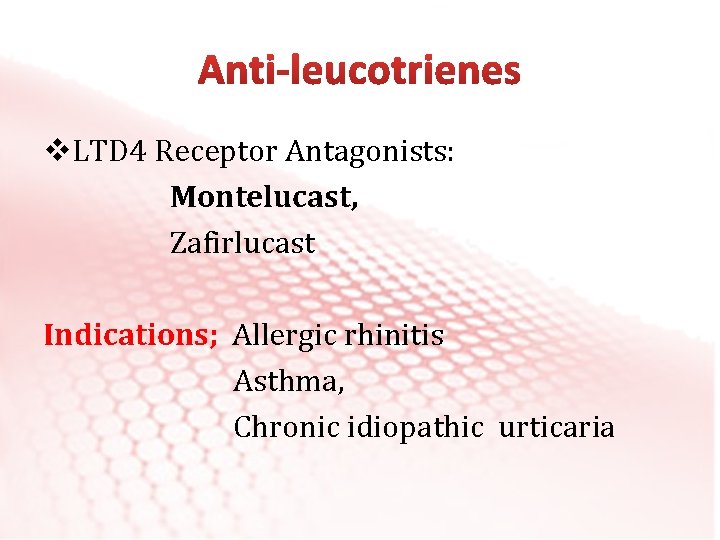
v. LTD 4 Receptor Antagonists: Montelucast, Zafirlucast Indications; Allergic rhinitis Asthma, Chronic idiopathic urticaria
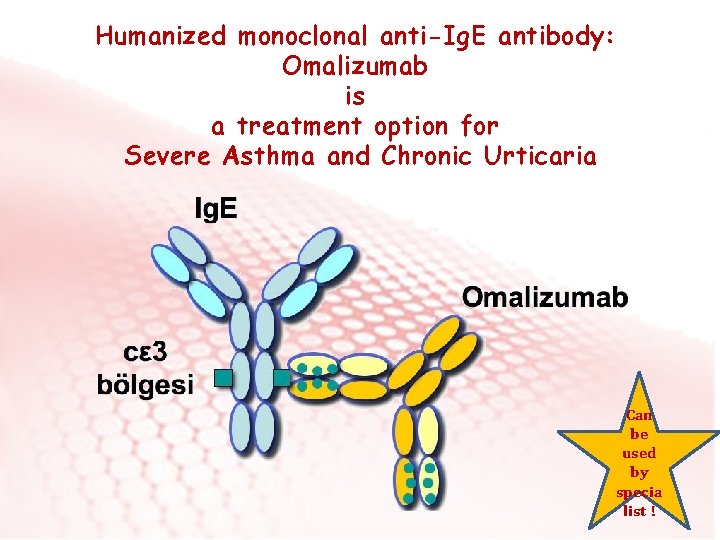
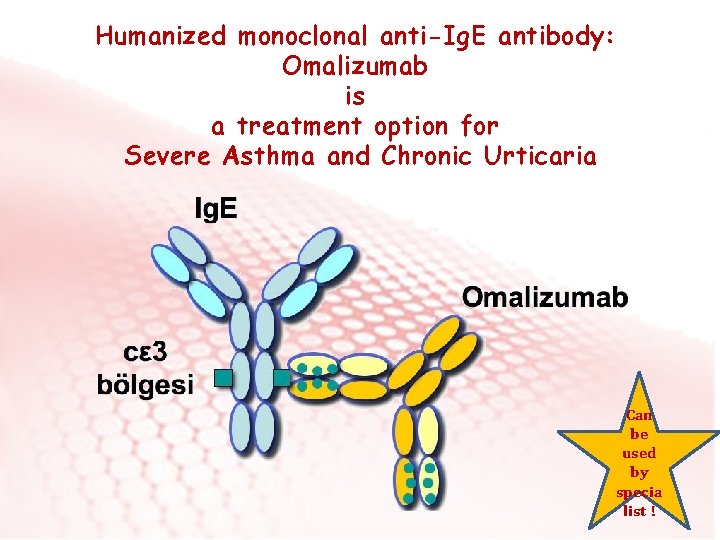
Humanized monoclonal anti-Ig. E antibody: Omalizumab is a treatment option for Severe Asthma and Chronic Urticaria Can be used by specia list !
Omalizumab for severe asthma Ø Patients ≥ 12 yrs old Ø Body weight <200 kg Ø Serum Total Ig. E level: 30 -1500 IU /ml • If there is no response to treatment in 16 weeks, treatment should be discontinued. • After administration of Omalizumab, the patient should remain under surveillance for 2 hours. • Injections should be done in an allergy clinic. The patient should be informed about anaphylaxis.

Allergen Specific Immunotherapy • It is the only treatment that changes the natural course of allergic diseases. • It should be given in a long period of up to 3 -5 years. Can be used by specia list !

Allergen Specific Immunotherapy Ig. E related allergic diseases proven by allergy tests and patient history: ü Severe Persistant. Allergic Rhinitis, ü Mild-Moderate Allergic Asthma (FEV 1 >70%) ü Bee-venom allergy (anaphylaxis)
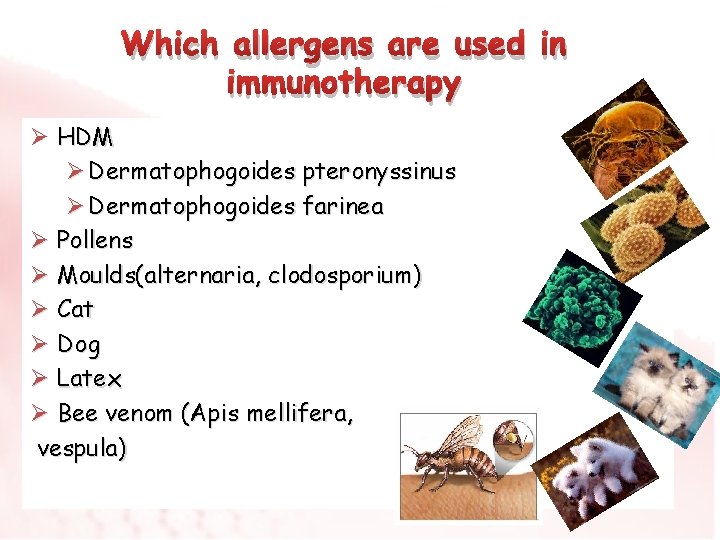
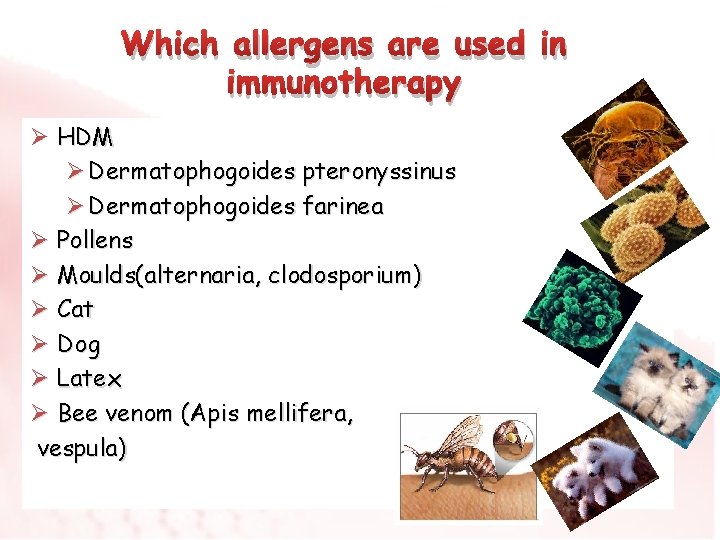
Which allergens are used in immunotherapy Ø HDM Ø Dermatophogoides pteronyssinus Ø Dermatophogoides farinea Ø Pollens Ø Moulds(alternaria, clodosporium) Ø Cat Ø Dog Ø Latex Ø Bee venom (Apis mellifera, vespula)
v. Subcutaneous v. Sublingual v. Oral
Thank you …