Anthropometrics and assessment of energy expenditure Liz Hudson










- Slides: 40
Anthropometrics and assessment of energy expenditure Liz Hudson MPH, RD September, 26 th 2016
Anthropometric data • Height • Weight • BMI • Ideal Body Weight (BMI)
Ideal Body weight (IBW) and Usual Body Weight (UBW) • Include these measures in every assessment, % of IBW and/or UBW provides important clinical information and can be part of criteria to diagnose malnutrition • Usual body weight is more useful in those who are ill • IBW Men: 106 lbs for first 5 feet of height + 6 lbs for every inch over 5 feet; for males under 5 feet in height, start with 106 lbs and subtract 6 lbs for every inch below 5 feet • IBW Women: 100 lbs for first 5 feet of height and plus 5 lbs for every inch thereafter; for women under 5 ft, start with 100 lbs and subtract 5 lbs for every inch under 5 ft
Example • Calculate the IBW of a man that is 190. 5 cm tall (height and weight in electronic medical records are most often in the metric scale) • Step 1. Convert 190. 5 cm to inches there are 2. 54 cm per inch, 190. 5 /2. 54 = 75 inches. • Step 2: How many inches over 5 ft is that? There are 12 inches per foot. 5 x 12 = 72 inches. 75 -60 = 15 (this man is 6 ft 3 inches) • Step 3: Plug into formula 106 lbs + (6 lbs x 15 inches) = 106+90 = 196 lbs. Report in kg 196/2. 2 = 89. 1 kg • IBW for a man 6 ft, 3 inches = 89. 1 kg

Note on adjusted body weight • Use in the past was common for obese patients • Rationale is that fat is less metabolically active than lean tissue; thus using actual body weight in an obese person will overestimate energy needs • However, studies have shown that in very overweight persons, calculating HBE using the adjusted wt tends to make calculations less accurate; underestimating total energy needs
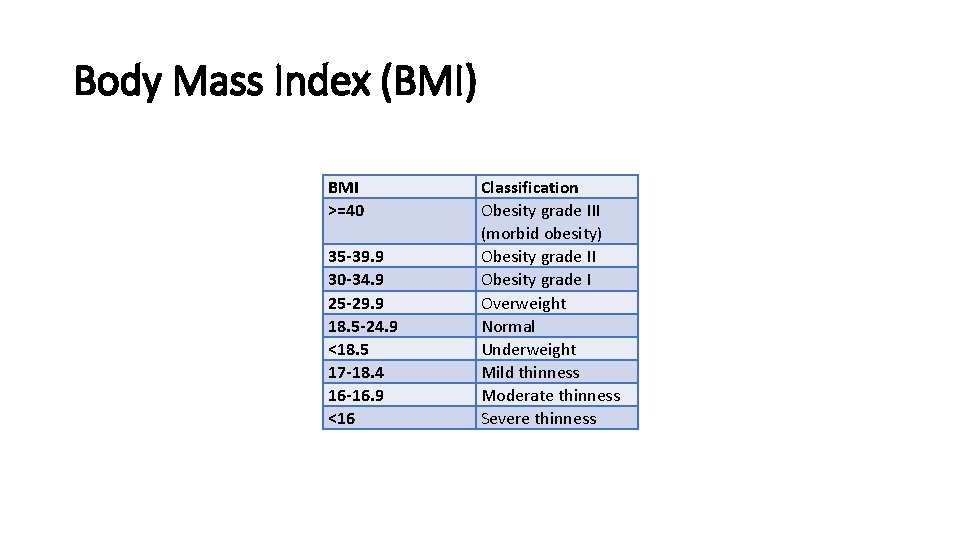
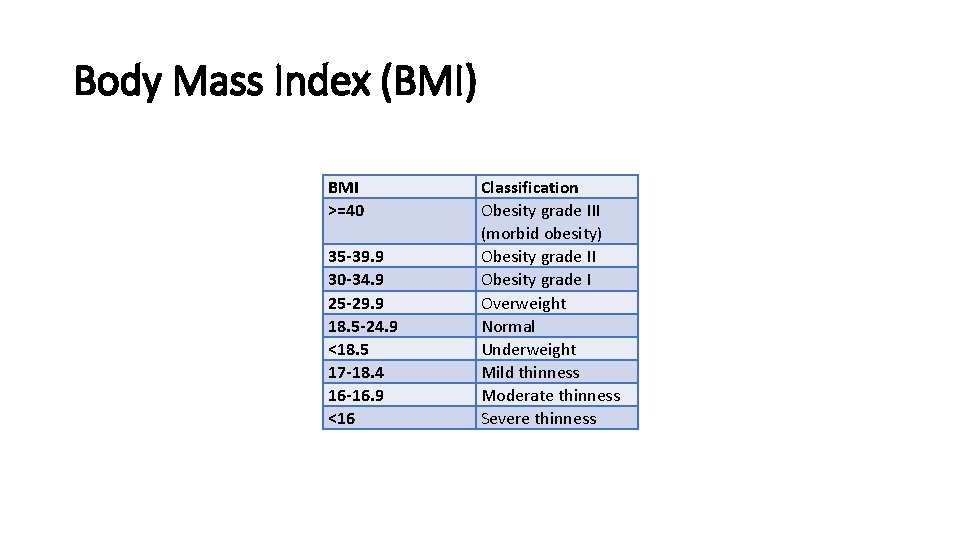
Body Mass Index (BMI) BMI >=40 35 -39. 9 30 -34. 9 25 -29. 9 18. 5 -24. 9 <18. 5 17 -18. 4 16 -16. 9 <16 Classification Obesity grade III (morbid obesity) Obesity grade II Obesity grade I Overweight Normal Underweight Mild thinness Moderate thinness Severe thinness

BMI • Metric: BMI = Weight in kg / Height in meters ^2 • English: BMI = Weight (lbs) / Height in inches^2 x 703 • Does not measure body fat directly • Most researches and health practitioners think that it provides an acceptable estimation of body fat • What do you guys think? • BMI should be measured in conjunction with other information related to the patient’s health status
Weight Status as a Predictor of Morbidity and Mortality • In young to middle aged adults, morbidity/ mortality is highest in the highest quintile of BMI • In the elderly, morbidity/mortality is highest in the lowest quintile of BMI • In most populations, there is a U-shaped relationship between mortality and BMI
Body Composition: Skinfold thickness (subcutaneous fat) • Validity depends on measurement technique and repetition over time • Changes take 3 to 4 weeks • Accuracy decreases with increasing obesity • Skinfold sites most reflective of body fatness are over the triceps and the biceps, below the scapula, suprailiac, and upper thigh
Body Composition: circumference measurements • Waist circumference: smallest area below the ribcage and above the umbilicus; measurements >40 for men and >35 for women are risk factors for disease • Mid arm circumference (MAC) in combination with TSF can determine arm muscle area (lean body mass)
Body Composition: Other measurements – refer to book • Underwater weighing • Total body potassium • Neutron activation analysis • BIA: fat free mass and fat mass • CT: subcutaneous and intra-abdominal fat • MRI: size of skeleton and internal organs; abdominal fat • DEXA: dual-energy x-ray absorptiometry; bone mineral density and fat and boneless lean tissue

Nutrition focused physical exam • Four basic physical examination techniques utilized • Inspection • Palpation • Percussion • Auscultation • Recommend refer to appendix 29 for further detail

Energy Expenditure: Predictive Equations • Objectives: • Compare/contrast predictive equations used to calculate energy requirements • Discuss the strengths and limitations of various predictive equations used in clinical practice • BRIEFLY Describe the role of indirect calorimetry (IC) in assessing energy expenditure
Review of Terminology Use This! • Basal metabolic rate (BMR), may also be presented as Basal energy expenditure (BEE): minimum amount of energy expended that is compatible with life • Resting metabolic rate (RMR) or Resting Energy Expenditure (REE): energy expended in the activities necessary to sustain normal body functions now used in place of BEE, tends to be 10 -20% higher than BEE • Estimated energy expenditure (EEE): Often used interchangeably with REE • Thermic Effect of Food (TEF): increase in energy expenditure associated with consumption, digestion, and absorption of food • Total energy expenditure (TEE): REE + TEF + activity expenditure = TEE
Factors affecting REE • Age: REE highly affected by proportion of lean body mass, which often decreases with increased age • Body composition: people with higher percentage of lean body mass will have higher resting metabolism • Body size • Climate: REE can be affected by living in extreme temps • Gender • Hormonal Status: hormones affect metabolic rate • Body temperature: fever increases REE • Other: i. e caffeine, nicotine, alcohol can stimulate REE
Thermic Effect of Food • Presence, magnitude, duration influenced by: • • • Size of the meal Ratio of protein, carbohydrate, and fat Fiber content Time of day the meal is eaten Degree of psychological stress Age
Thermic Effect of Food • Thermic effect of digestion results in a 5 -10% increase in RMR • • Greater with larger meal Peaks at 60 -180 minutes Longer in obese patients Longer in older patients
Predictive Equations • So many choices….
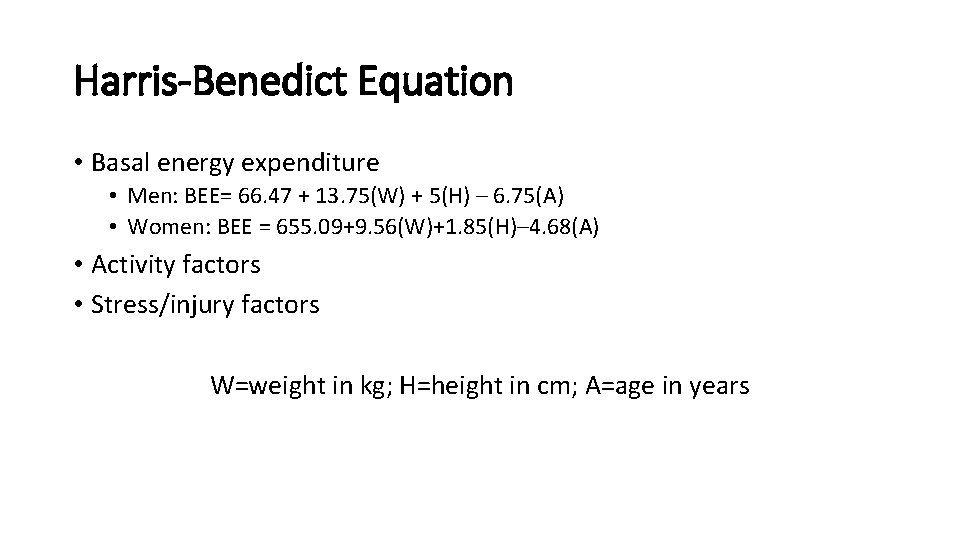
Harris-Benedict Equation • Basal energy expenditure • Men: BEE= 66. 47 + 13. 75(W) + 5(H) – 6. 75(A) • Women: BEE = 655. 09+9. 56(W)+1. 85(H)– 4. 68(A) • Activity factors • Stress/injury factors W=weight in kg; H=height in cm; A=age in years
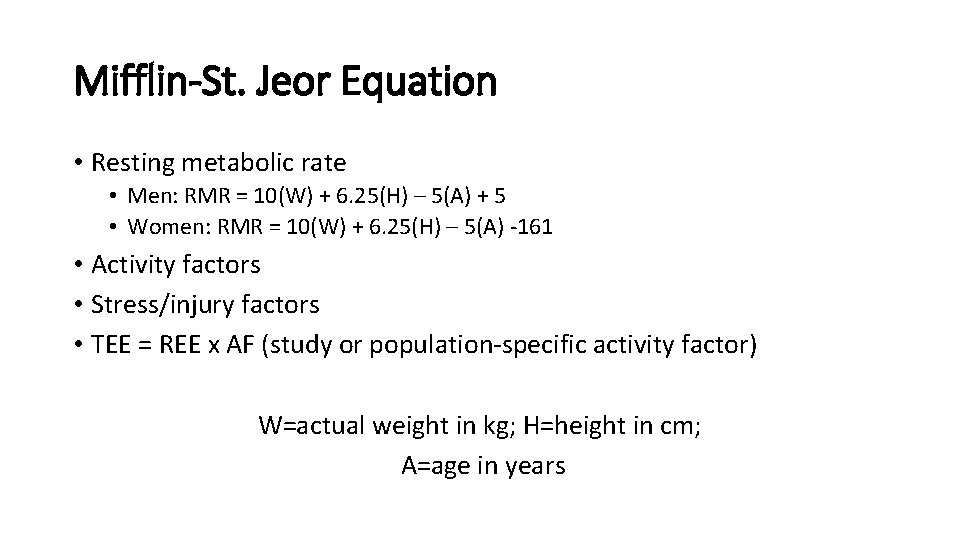
Mifflin-St. Jeor Equation • Resting metabolic rate • Men: RMR = 10(W) + 6. 25(H) – 5(A) + 5 • Women: RMR = 10(W) + 6. 25(H) – 5(A) -161 • Activity factors • Stress/injury factors • TEE = REE x AF (study or population-specific activity factor) W=actual weight in kg; H=height in cm; A=age in years
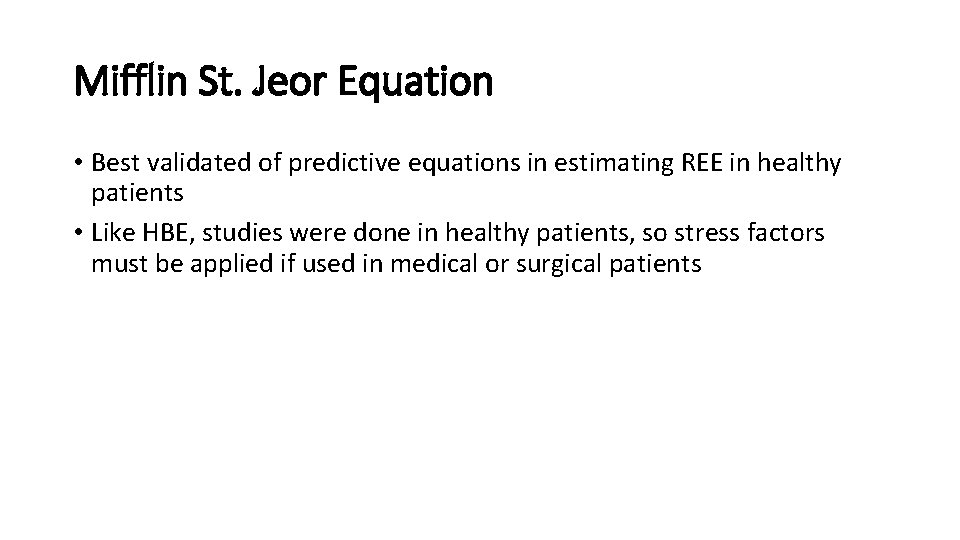
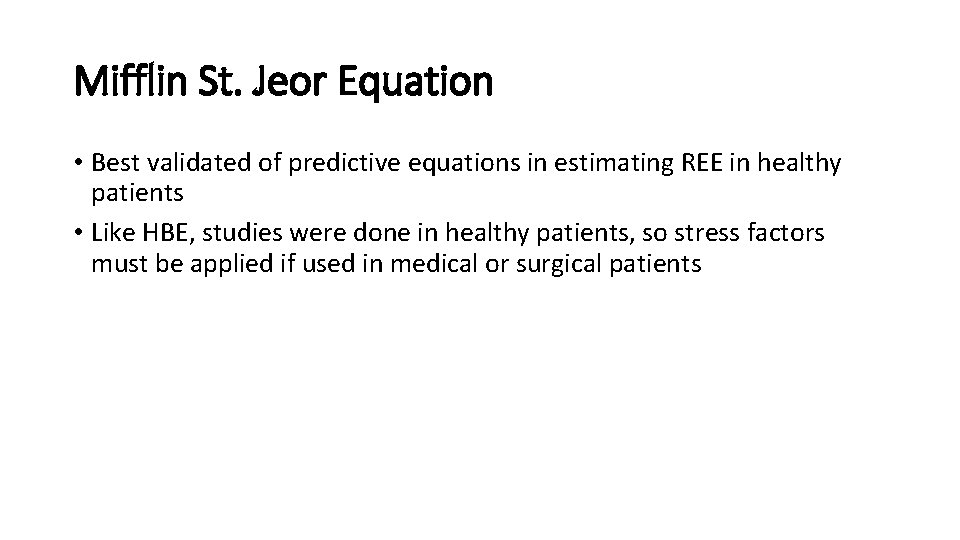
Mifflin St. Jeor Equation • Best validated of predictive equations in estimating REE in healthy patients • Like HBE, studies were done in healthy patients, so stress factors must be applied if used in medical or surgical patients
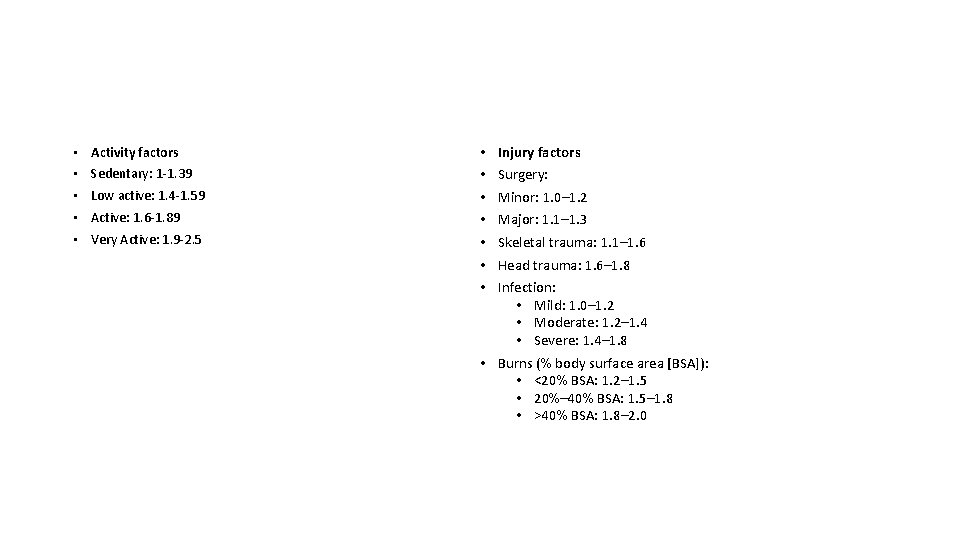
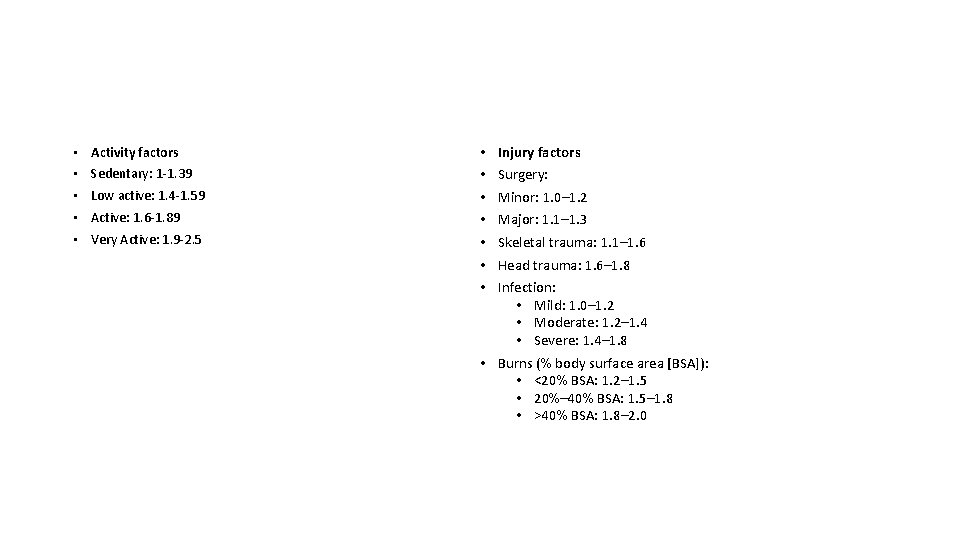
• Activity factors • Sedentary: 1 -1. 39 • Low active: 1. 4 -1. 59 • Active: 1. 6 -1. 89 • Very Active: 1. 9 -2. 5 • • Injury factors Surgery: Minor: 1. 0– 1. 2 Major: 1. 1– 1. 3 Skeletal trauma: 1. 1– 1. 6 Head trauma: 1. 6– 1. 8 Infection: • Mild: 1. 0– 1. 2 • Moderate: 1. 2– 1. 4 • Severe: 1. 4– 1. 8 • Burns (% body surface area [BSA]): • <20% BSA: 1. 2– 1. 5 • 20%– 40% BSA: 1. 5– 1. 8 • >40% BSA: 1. 8– 2. 0

Simplistic Weight-Based Equations • 11 -14 kcal/kg (morbid obesity) • 15 -18 kcal/kg (obese/overweight) • 22 -25 kcal/kg (normal, healthy weight) • 25 -30 kcal/kg (underweight, or have increased needs) • 30 -35 kcal/kg (underweight, higher degree of increased needs, hematologic malignancy) • 40+ kcal/kg (increased needs, weight gain)


Using Predictive Equations to Estimate Energy Requirements Is the patient Critically Ill? Yes. Is the patient obese? Is a hypocaloric regimen appropriate? Yes 22 -25 kcal/kg IBW or 11 -14 kcal/kg actual body weight No. Is the patient <60? No Use Penn State 2003 b No Yes Penn State 2003(b) No Penn State 2010 Use Mifflin St. Jeor using actual body weight
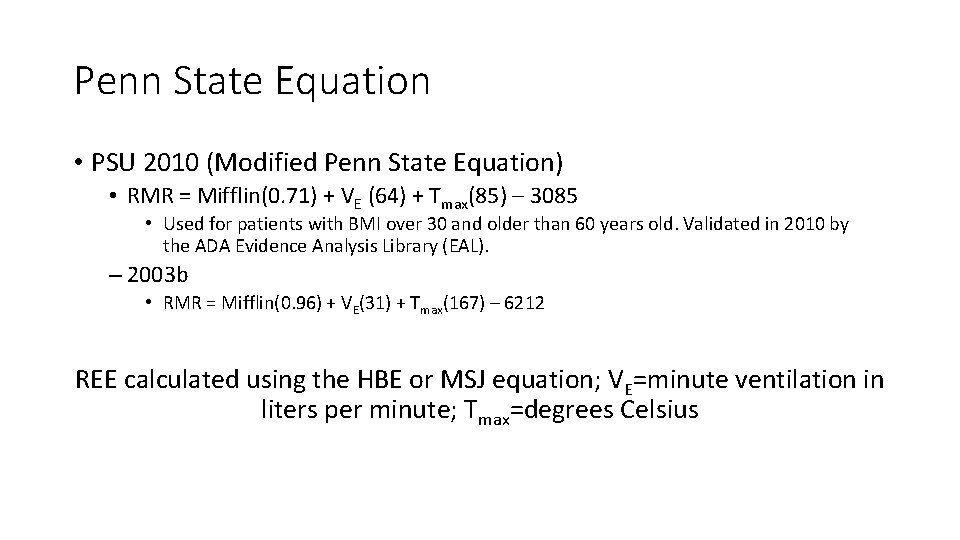
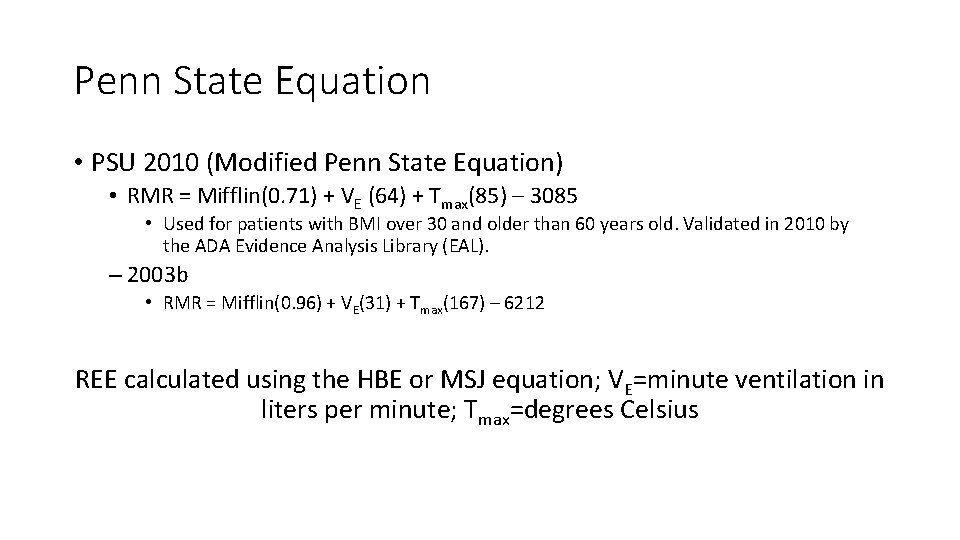
Penn State Equation • PSU 2010 (Modified Penn State Equation) • RMR = Mifflin(0. 71) + VE (64) + Tmax(85) – 3085 • Used for patients with BMI over 30 and older than 60 years old. Validated in 2010 by the ADA Evidence Analysis Library (EAL). – 2003 b • RMR = Mifflin(0. 96) + VE(31) + Tmax(167) – 6212 REE calculated using the HBE or MSJ equation; VE=minute ventilation in liters per minute; Tmax=degrees Celsius
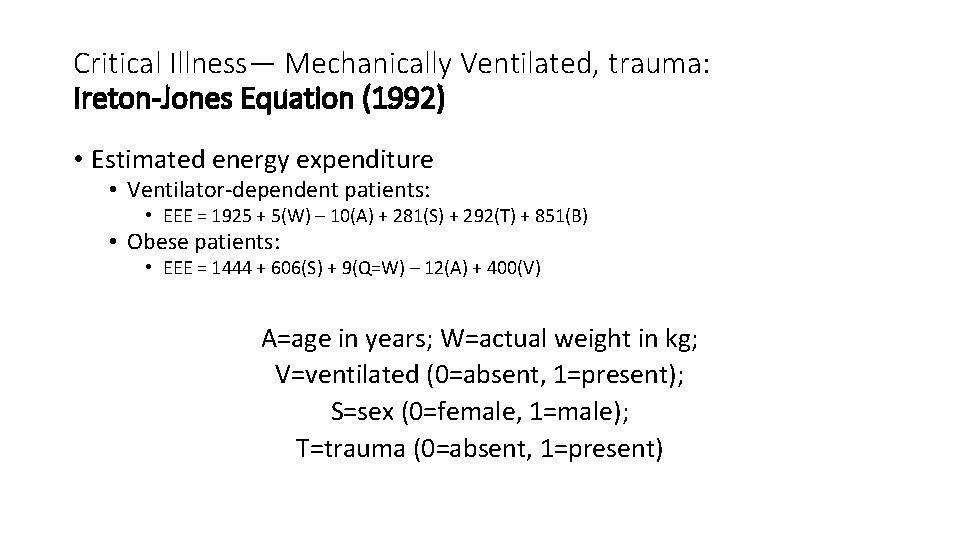
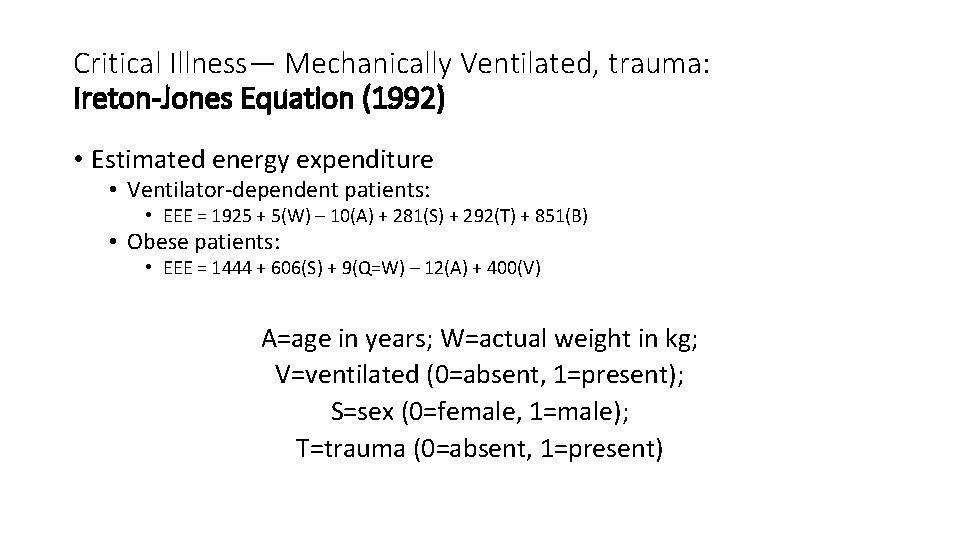
Critical Illness— Mechanically Ventilated, trauma: Ireton-Jones Equation (1992) • Estimated energy expenditure • Ventilator-dependent patients: • EEE = 1925 + 5(W) – 10(A) + 281(S) + 292(T) + 851(B) • Obese patients: • EEE = 1444 + 606(S) + 9(Q=W) – 12(A) + 400(V) A=age in years; W=actual weight in kg; V=ventilated (0=absent, 1=present); S=sex (0=female, 1=male); T=trauma (0=absent, 1=present)
Indirect Calorimetry IC measures the volume of inspired oxygen and expired carbon dioxide to determine VO 2 and VCO 2 to calculate resting energy expenditure (REE) and respiratory quotient (RQ).
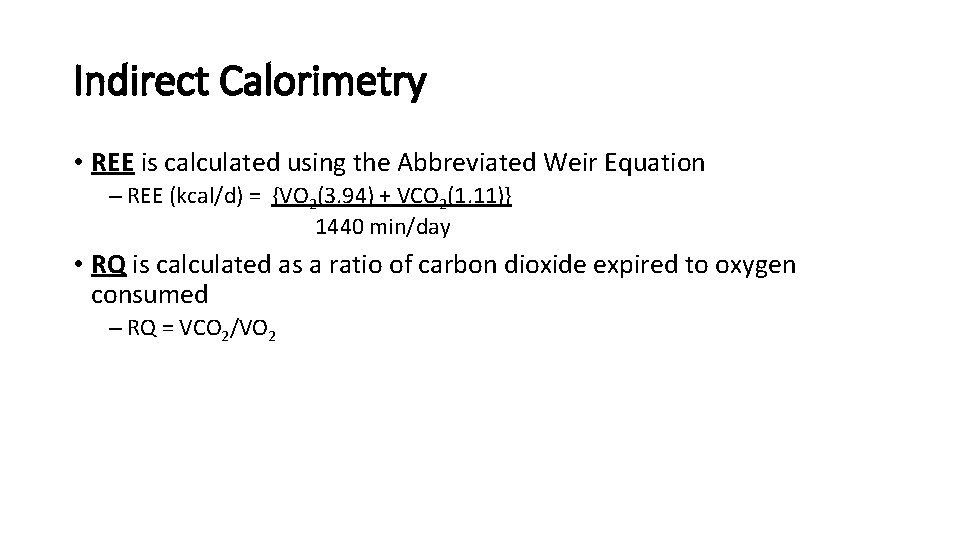
Indirect Calorimetry • REE is calculated using the Abbreviated Weir Equation – REE (kcal/d) = {VO 2(3. 94) + VCO 2(1. 11)} 1440 min/day • RQ is calculated as a ratio of carbon dioxide expired to oxygen consumed – RQ = VCO 2/VO 2

Indications for IC • Inability to accurately estimate energy requirements • Inadequate clinical response to nutrition therapy
Inability to Accurately Estimate Energy Requirements • • Trauma SIRS/fever MODS ARDS COPD Paralysis Altered body composition: – Underweight – Obesity – Alterations in fluid balance • Wounds • Paralytics • Sedation

Inadequate Clinical Response to Nutrition Therapy • Malnutrition despite “adequate” nutrition support • Poor wound healing • Failure to wean from mechanical ventilation • Underfeeding vs. overfeeding
Protein Requirements Not often done… • Can be determined through calculation of nitrogen balance • Compares nitrogen (protein) intake to nitrogen (protein) output • Limitations inaccurate urine collection and presence of renal dysfunction

Protein Requirements Condition Descriptor Adult Maintenance Older Adults Renal disease: pre-dialysis Renal disease: hemodialysis Renal disease: peritoneal dialysis Renal Disease: CRRT Hepatitis (acute or chronic) Liver disease/cirrhosis Cancer cachexia Bone Marrow Transplant (BMT) IBD Short bowel syndrome Solid organ transplant: (Acute posttransplant) Solid organ transplant (long-term) Pulmonary Disease Pregnancy Critical Illness (burns, sepsis, TBI) Stroke Protein Requirement 0. 8 -1. 0 g/kg 1. 0 -1. 2 g/kg 0. 6 -0. 8 g/kg 1. 2 -1. 3 g/kg >1. 5 -2. 5 g/kg 1 -1. 5 g/kg 1. 2 -1. 6 g/kg 1 -1. 5 g/kg 1. 5 -2. 5 g/kg 1. 0 -1. 5 g/kg 1. 5 -2. 0 g/kg 1. 2 -1. 5 g/kg +25 g/day 1. 5 -2. 0 g/kg 1 -1. 25 g/kg
Protein requirements: Older adults • Evidence suggests that older adults need more dietary protein than younger adults to support good health, promote recovery from illness, and maintain functionality. • Older adults need to make-up for age-related changes in protein metabolism • Need more protein to offset inflammatory and catabolic conditions associated with chronic and acute diseases that occur commonly with aging • Persons older than 65 years of age need at least 1. 0 -1. 2 g of protein per kg body weight to maintain and regain lean body mass and function
Protein Requirements: Wounds • For patients at risk for pressure ulcers, the recommendation for protein intake may be as high as 1. 5 g/kg to 2. 0 g/kg per day • The European Pressure Ulcer Advisory Panel recommends. 1. 0 g per kg to 1. 5 g per kg per day • Excess dietary protein in amounts greater than 1. 5 g per kg to 2 g per kg body weight per day can be a risk factor for dehydration, especially in the elderly
Fluid requirements • Goals of fluid management include maintenance of adequate hydration, tissue perfusion, and electrolyte balance • Depends on many factors • Insensible losses: fluid lost on a daily basis from the lungs, skin, respiratory tract • Measured losses: stool, urine, wound and/or ostomy drainage • Alterations in fluid balance due to • Metabolic changes: fever and hyperthyroidism • Medical therapy: diuretics
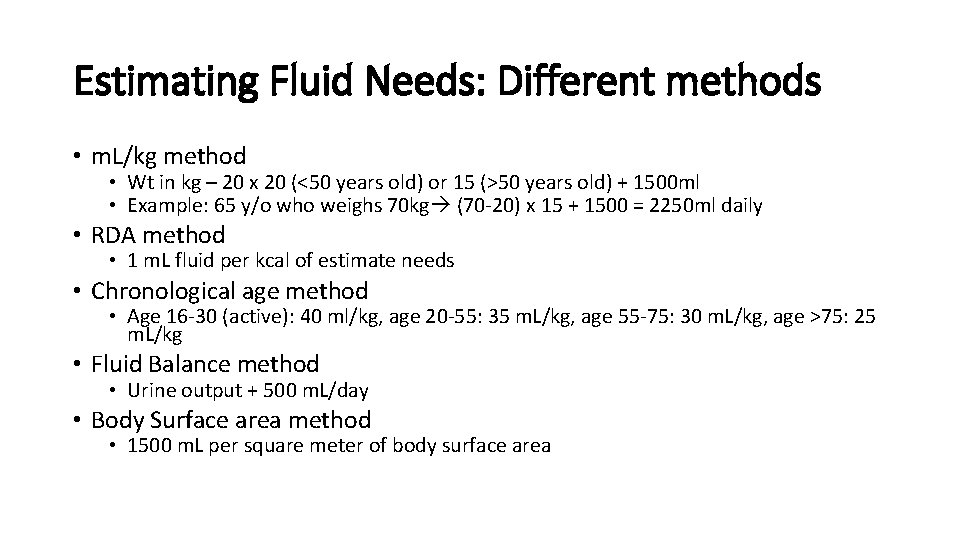
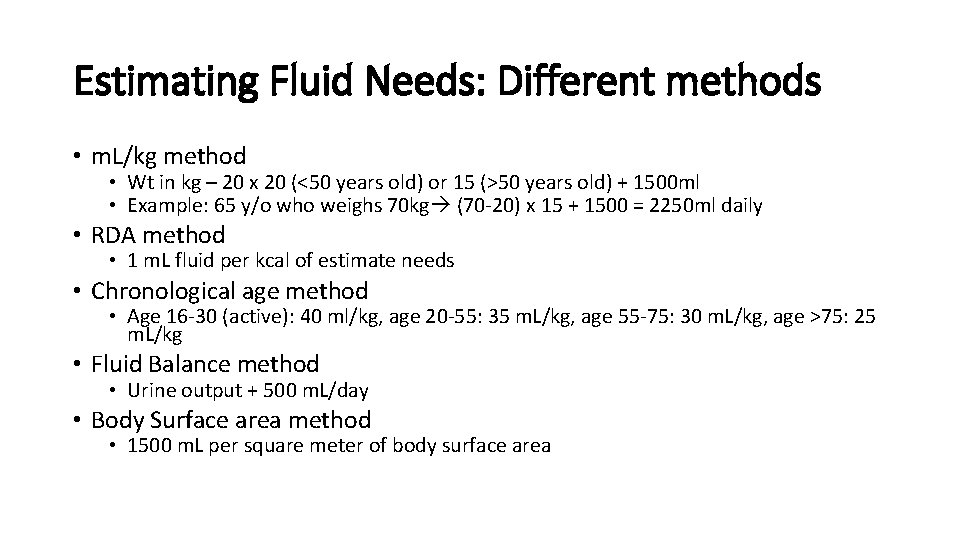
Estimating Fluid Needs: Different methods • m. L/kg method • Wt in kg – 20 x 20 (<50 years old) or 15 (>50 years old) + 1500 ml • Example: 65 y/o who weighs 70 kg (70 -20) x 15 + 1500 = 2250 ml daily • RDA method • 1 m. L fluid per kcal of estimate needs • Chronological age method • Age 16 -30 (active): 40 ml/kg, age 20 -55: 35 m. L/kg, age 55 -75: 30 m. L/kg, age >75: 25 m. L/kg • Fluid Balance method • Urine output + 500 m. L/day • Body Surface area method • 1500 m. L per square meter of body surface area
Let’s practice!
 Ergonomics and anthropometrics
Ergonomics and anthropometrics Revenue expenditure
Revenue expenditure Revenue expenditure examples
Revenue expenditure examples Capital expenditure vs revenue expenditure
Capital expenditure vs revenue expenditure Capital and revenue
Capital and revenue Henry hudson lifespan
Henry hudson lifespan Energy expenditure and fatigue
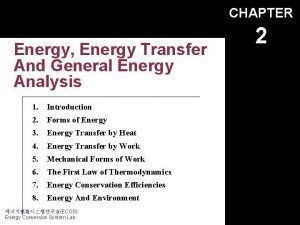
Energy expenditure and fatigue Energy energy transfer and general energy analysis
Energy energy transfer and general energy analysis Energy energy transfer and general energy analysis
Energy energy transfer and general energy analysis Stock market vocabulary worksheet
Stock market vocabulary worksheet Ann plays handball very well
Ann plays handball very well Ann handball very well
Ann handball very well Put each verb in brackets into a suitable verb form
Put each verb in brackets into a suitable verb form Income statement for small business example
Income statement for small business example Example of income and expenditure account
Example of income and expenditure account Recording income and expenditure
Recording income and expenditure 4 basic expenditure cycle activities
4 basic expenditure cycle activities Fruitless and wasteful expenditure
Fruitless and wasteful expenditure Aggregate expenditure and equilibrium output
Aggregate expenditure and equilibrium output Capital and revenue expenditure
Capital and revenue expenditure Henry hudson birth and death
Henry hudson birth and death Juan ponce de leon obstacles
Juan ponce de leon obstacles Describe henry hudson's crew
Describe henry hudson's crew Liz welch mississippi
Liz welch mississippi Liz loxley
Liz loxley Liz quintero
Liz quintero Liz pellicano
Liz pellicano Liz lochhead last supper
Liz lochhead last supper Liz whetham
Liz whetham Liz ice age
Liz ice age Box room liz lochhead
Box room liz lochhead Liz lochhead view of scotland/love poem
Liz lochhead view of scotland/love poem Liz sneddon bivariate
Liz sneddon bivariate Liz nichols art
Liz nichols art Senq tracking
Senq tracking Liz bratsky
Liz bratsky Liz hays
Liz hays Revelation liz lochhead analysis
Revelation liz lochhead analysis Workplace violence continuum
Workplace violence continuum Dr liz price
Dr liz price Erg root word
Erg root word