Anterior Shoulder Dislocation and The Black Lung Jerod
Anterior Shoulder Dislocation and The Black Lung Jerod Miller
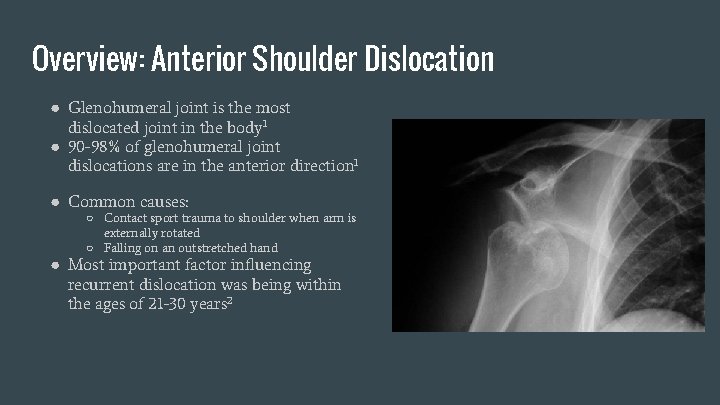
Overview: Anterior Shoulder Dislocation ● Glenohumeral joint is the most dislocated joint in the body 1 ● 90 -98% of glenohumeral joint dislocations are in the anterior direction 1 ● Common causes: ○ Contact sport trauma to shoulder when arm is externally rotated ○ Falling on an outstretched hand ● Most important factor influencing recurrent dislocation was being within the ages of 21 -30 years 2
Overview: Anterior Shoulder Dislocation ● Treatment Options ○ Non-surgical ○ Surgical Treatment ■ Indicated if patient is predisposed to recurrent dislocations ● Predisposing criteria for recurrent dislocation 3 ○ young age ○ Has a history of recurrence ○ Boney Defect ○ active lifestyle
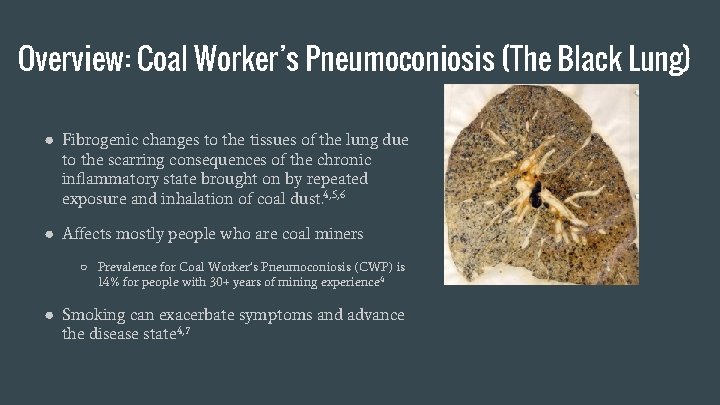
Overview: Coal Worker’s Pneumoconiosis (The Black Lung) ● Fibrogenic changes to the tissues of the lung due to the scarring consequences of the chronic inflammatory state brought on by repeated exposure and inhalation of coal dust. 4, 5, 6 ● Affects mostly people who are coal miners ○ Prevalence for Coal Worker’s Pneumoconiosis (CWP) is 14% for people with 30+ years of mining experience 4 ● Smoking can exacerbate symptoms and advance the disease state 4, 7
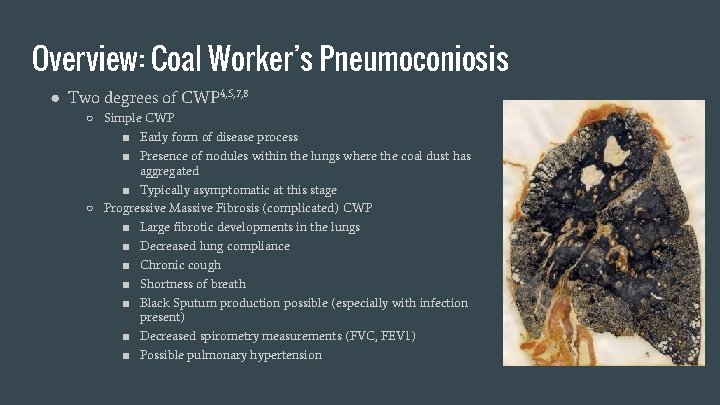
Overview: Coal Worker’s Pneumoconiosis ● Two degrees of CWP 4, 5, 7, 8 ○ Simple CWP ■ Early form of disease process ■ Presence of nodules within the lungs where the coal dust has aggregated ■ Typically asymptomatic at this stage ○ Progressive Massive Fibrosis (complicated) CWP ■ Large fibrotic developments in the lungs ■ Decreased lung compliance ■ Chronic cough ■ Shortness of breath ■ Black Sputum production possible (especially with infection present) ■ Decreased spirometry measurements (FVC, FEV 1) ■ Possible pulmonary hypertension
Overview: Coal Worker’s Pneumoconiosis ● Treatment 4, 7, 8 ○ No specific treatment for actual recovery from disease except lung transplant ○ Most treatments focus on management of symptoms ■ Prescription bronchodilators ■ Routine vaccination ■ Antibiotic therapy for infection ■ Pulmonary rehabilitation ■ Smoking cessation programs (if patients are smokers) ■ Discontinuing exposure to coal dust ■ Supplemental oxygen if needed
Case Presentation Patient: Derek Zoolander ● History ○ 65 year old coal miner with 35 years of experience ○ Recently underwent Latarjet Stabilization surgery for his 4 th recurrent dislocation of his right shoulder ■ Initial anterior shoulder dislocation was at the age of 21 ■ Most recent dislocation happened falling in the tub at home ○ Previously diagnosed with Progressive Massive Fibrosis CWP ○ History of smoking for 30 years at 1 pack a day ○ No family history of cardiovascular disease ○ Has been prescribed medications to help manage his pain from surgery, to increase his lung function, and manage his depression. ○ Complains of dyspnea and shortness of breath with ADLs ○ Black sputum production infrequent
Medications 9 Ibuprofen ● Non-COX specific Non. Steroidal Anti Inflammatory Drug ● Goal: To manage pain and reduce swelling caused by the recent surgery ● PT considerations ○ Possibility of GI distress and ulceration Tiotropium (Spiriva) ● Anticholinergic (inhaled) ● Goal: Bronchodilation of the lungs to improve airway function ● PT considerations ○ Tachycardia, blurred vision, confusion ○ Systemic side effects occur infrequently because of route of administration
Medications 9 Budesonide (Pulmicort) ● Glucocorticoid (inhaled) ● Goal: To reduce inflammation in the lung tissue to attempt to prevent further fibrosis ● PT implications ○ Due to the inhalation route of administration, risk of the adverse effects (muscle wasting, osteoporosis, hypertension, adrenal suppression) is minimal. The physical therapist should still be on the lookout for these adverse effects though. ○ When used long term, tolerance can be an issue with glucocorticoids
Medications 9 Citalopram (Celexa) ● Selective Serotonin Reuptake Inhibitor ● Goal: To decrease depression ● PT implications ○ Possible GI symptoms such as nausea, vomiting, constipation, and diarrhea Supplemental Oxygen ● Goal: To improve oxygen saturation of the blood ● PT implications ○ Hoses from oxygen device may pose safety risk.
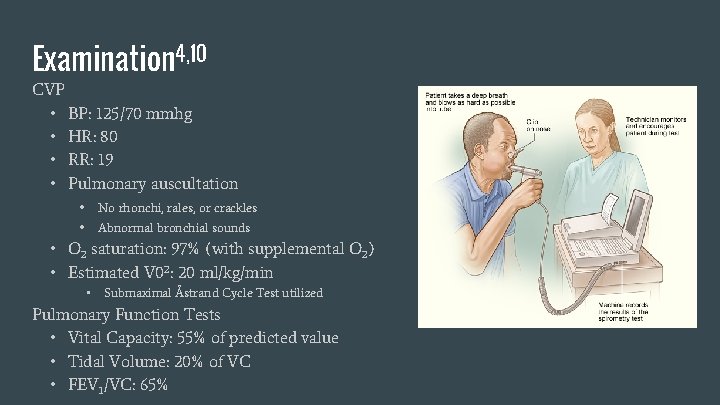
Examination 4, 10 CVP • BP: 125/70 mmhg • HR: 80 • RR: 19 • Pulmonary auscultation No rhonchi, rales, or crackles Abnormal bronchial sounds • O 2 saturation: 97% (with supplemental O 2) • Estimated V 02: 20 ml/kg/min • Submaximal Åstrand Cycle Test utilized Pulmonary Function Tests • Vital Capacity: 55% of predicted value • Tidal Volume: 20% of VC • FEV 1/VC: 65%
Examination 10 Temperature: 98. 6° F Musculoskeletal: ● Barrel chest ○ Slight abdominal paradoxical breathing ● Decreased ROM in right shoulder due to surgery ● MMT contraindicated because of acute tissue repair ● Forward head posture
Examination Integumentary ● Slight swelling of the right upper extremity from lack of use during immobilization ● Local inflammation of surgical site on right shoulder ● Surgical scar is slightly red but no infection present and has no restrictions Outcome Measure 11 ● Disability of the Arm, Shoulder, and Hand (DASH) ○ DASH score: 85 (100 is the highest level of disability) ● Chronic Respiratory Disease Questionnaire (CRQ) ○ CRQ score: 55 (20 is max impairment, 140 no impairment)
Assessment Clinical Assessment Patient reports depression over current inability to function due to the immobilization of his shoulder compounded by his relatively severe pulmonary restrictions but also reports that depression has improved significantly since he started drug therapy. Post-surgical stabilization presentation is normal with obvious motion and strength restrictions and local inflammation and pain. Coal Worker’s Pneumoconiosis disability is severe and characterized by dyspnea at rest and activity, thoracic breathing dysfunction, and decreased aerobic capacity. Condition is exacerbated by smoking habits Prognosis ● Shoulder impairment: good ● CWP: poor
Plan of Care ● Educate patient on shoulder repair and supplement previous education for CWP ● Teach bed mobility ● Use physical agents to treat both conditions ● Optimize breathing techniques ● Improve aerobic performance as much as CWP allows ● Increase shoulder function through adequate uses of therapeutic exercise ● Provide information on resources to facilitate smoking cessation
Physical Therapy Goals ● Facilitate adequate healing of surgical incision ● Enable more efficient breathing pattern ● Return shoulder to level of prior function ● Decrease DASH score ● Increase CRQ score ● Increase estimated VO 2 max
Physical Agents 13 ● Intermittent Pneumatic Compression Pump & Compression Wrap ○ Use: to reduce and then maintain low levels of edema and swelling in the right upper extremity ○ Settings: Patient’s blood pressure should be taken and the compression force should not exceed diastolic pressure. Inflation time: 80 seconds. Deflation time: 40 seconds. Total treatment duration 1 hour. ○ Limb wrapped with compression wrap after IPCP. ● Cryotherapy ○ Use: to reduce pain and swelling in right shoulder ○ Settings: apply ice pack to the right shoulder for 15 minutes ● Ultrasound ○ Use: to aid the healing of the surgical incision of the right shoulder. ○ Settings: Frequency: 3 MHz, intensity: . 5 W/cm 2, 20% duty cycle, 5 minutes
Transfer Training ● Independent left roll from supine to sidelying and independent side-lying to sitting on edge of bed. ○ Taught to patient to facilitate his ease of getting out of bed while his right arm is immobilized and cannot be used. ○ Previously got out of bed on the right side using his right arm to push himself up.
CVP Interventions Breathing Training ● Coordinate breathing with motion ○ Trunk extension with inspiration, trunk flexion with expiration ● Try to elicit diaphragmic contribution to breathing ○ Sniffing technique ○ Using tactile cues of hand or other object on belly for visual input of lower rib cage expansion ● Stacking breaths Gradual aerobic exercise program
Other Interventions Shoulder Rehabilitation ● Ranging of right upper extremity during immobilization phase ● Progressive stretching of tight muscles ● Progressive strengthening of weakened musculature ● ADL training once strength and ROM is sufficient CWP ● Posture adjustment forward head posture ○ Stretching of anterior neck musculature ○ Strengthening of posterior neck musculature
Outcomes ● Patient’s right shoulder function returned to near previous levels and is comparable to the function of the left shoulder ● Surgical incision healed completely with mobile scar tissue ● DASH score: 30 (was 85) ● Estimated VO 2 max increased to 24 (increase of 20%) ○ Submaximal Åstrand cycling test used ● CRQ score: 70 (was 55) ● CWP complications are irreversible but some ADL function was restored ● Patient joined smoking cessation support group and has gradually reduced his smoking to half of his pre-therapy levels and has plans to quit completely.
References 1. 2. 3. 4. Emedicine. medscape. com. Shoulder Dislocation Surgery: Background, Epidemiology, Etiology. 2015. Available at: http: //emedicine. medscape. com/article/1261802 -overview#. Accessed July 29, 2015. Kralinger F, Golser K, Wischatta R, Wambacher M, Sperner G. Predicting recurrence after primary anterior shoulder dislocation. The American Journal Of Sports Medicine [serial online]. 2002; (1): 116. Available from: General One. File, Ipswich, MA. Accessed July 29, 2015. Dumont G, Fogerty S, Rosso C, Lafosse L. The arthroscopic latarjet procedure for anterior shoulder instability: 5 -year minimum follow -up. The American Journal Of Sports Medicine [serial online]. 2014; (11): 2560. Available from: General One. File, Ipswich, MA. Accessed July 29, 2015. Emedmd. com. Coal Workers’ Pneumoconiosis | e. Med. MD. com. 2015. Available at: http: //www. emedmd. com/content/coalworkers%E 2%80%99 -pneumoconiosis. Accessed November 11, 2015. Pneumoconiosis. Coal Workers Pneumoconiosis. 2011. Available at: http: //www. pneumoconiosis. org. uk/coal-workers-pneumoconiosis. Accessed November 11, 2015. 6. Vanhee, D. , et al. "Cytokines and cytokine network in silicosis and coal workers' pneumoconiosis. " European Respiratory Journal 8. 5 (1995): 834 -842. 7. Coal Worker's Pneumoconiosis Clinical Presentation: History, Physical, Causes. 2014. Available at: http: //emedicine. medscape. com/article/297887 -clinical. Accessed November 2015.
References 8. Hopkinsmedicine. org. Pneumoconiosis | Johns Hopkins Medicine Health Library. 2015. Available at: http: //www. hopkinsmedicine. org/healthlibrary/conditions/respiratory_disorders/pneumoconiosis_134, 162/. Accessed November 11, 2015. 9. 1. Ciccone, CD. Pharmacology in Rehabilitation (4 th Ed. ). Philidelphia: F. A. Davis Company; 2007. 10. De. Turk W, Cahalin L. Cardiovascular And Pulmonary Physical Therapy. New York: Mc. Graw-Hill Medical; 2011. Physio-pedia. com. DASH Outcome Measure - Physiopedia, universal access to physiotherapy knowledge. 2015. Available at: http: //www. physio-pedia. com/index. php? title=DASH_Outcome_Measure. Accessed November 13, 2015. 12. Schünemann, Holger J. , et al. "Measurement properties and interpretability of the Chronic respiratory disease questionnaire (CRQ). " COPD: Journal of Chronic Obstructive Pulmonary Disease 2. 1 (2005): 81 -89. 13. Cameron M. Physical Agents In Rehabilitation. St. Louis, Mo. : Elsevier/Saunders; 2013.
- Slides: 23