Antepartum fetal Monitoring Mostafa mohammed khodry Assistant prof

- Slides: 44
Antepartum fetal Monitoring Mostafa mohammed khodry Assistant prof of obstetric and gynecology South valley university- Egypt
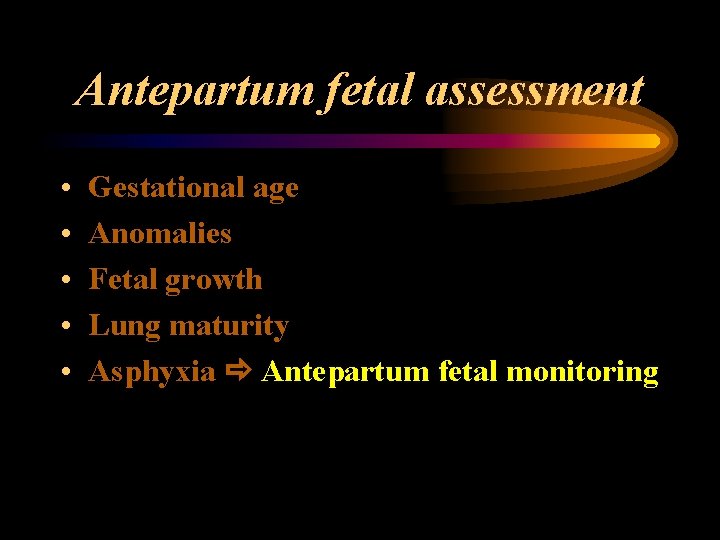
Antepartum fetal assessment • • • Gestational age Anomalies Fetal growth Lung maturity Asphyxia Antepartum fetal monitoring
Uteroplacental insufficiency Inadequate delivery of nutritive or respiratory substances to appropriate fetal tissues.
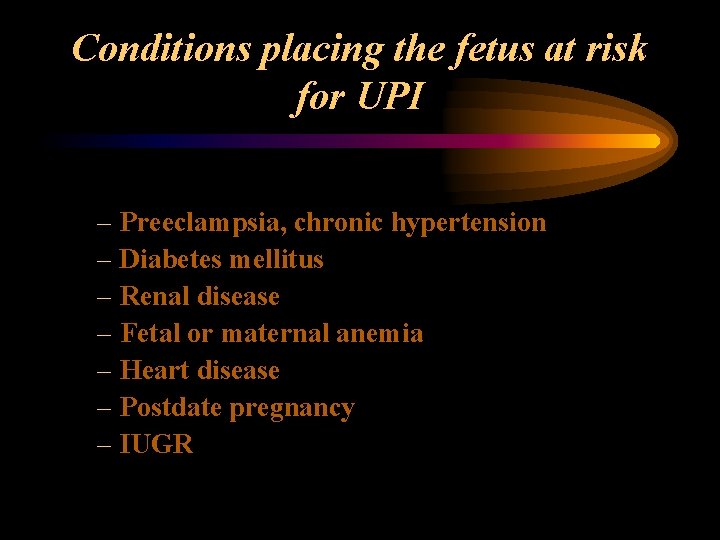
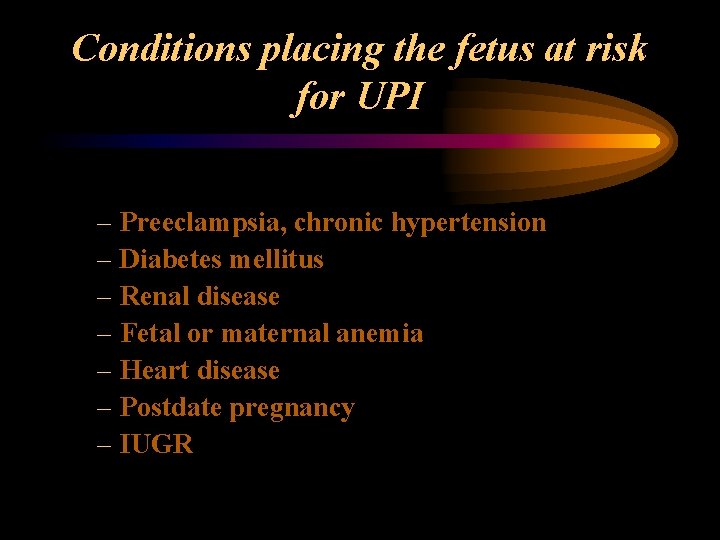
Conditions placing the fetus at risk for UPI – Preeclampsia, chronic hypertension – Diabetes mellitus – Renal disease – Fetal or maternal anemia – Heart disease – Postdate pregnancy – IUGR
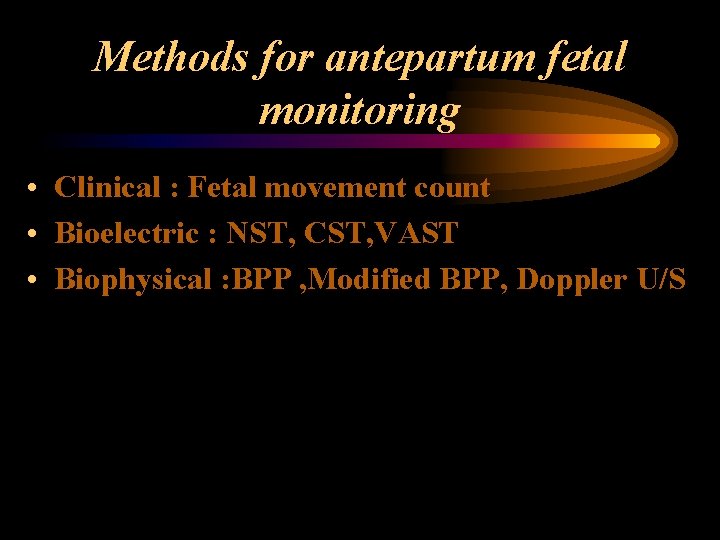
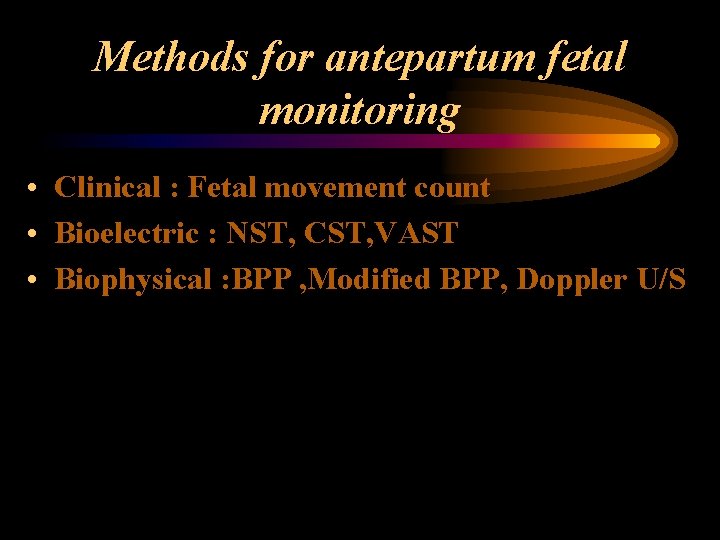
Methods for antepartum fetal monitoring • Clinical : Fetal movement count • Bioelectric : NST, CST, VAST • Biophysical : BPP , Modified BPP, Doppler U/S
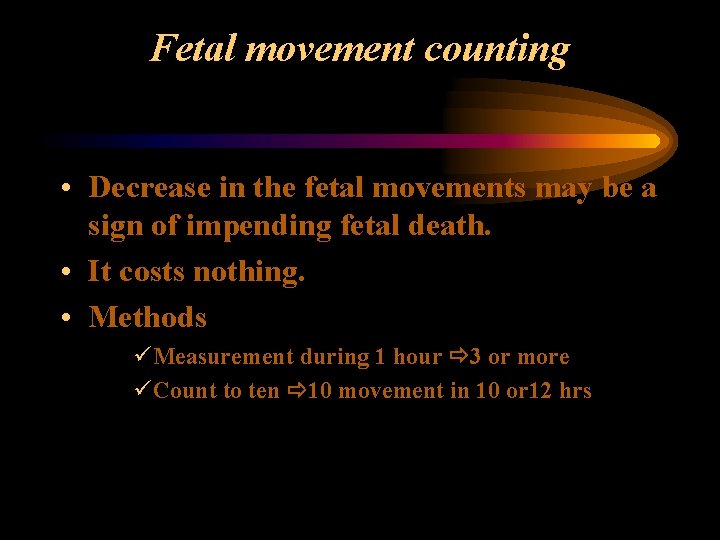
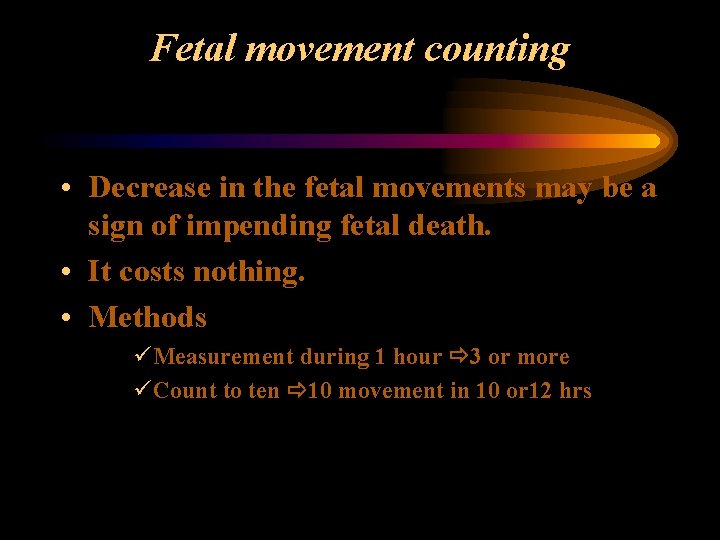
Fetal movement counting • Decrease in the fetal movements may be a sign of impending fetal death. • It costs nothing. • Methods üMeasurement during 1 hour 3 or more üCount to ten 10 movement in 10 or 12 hrs
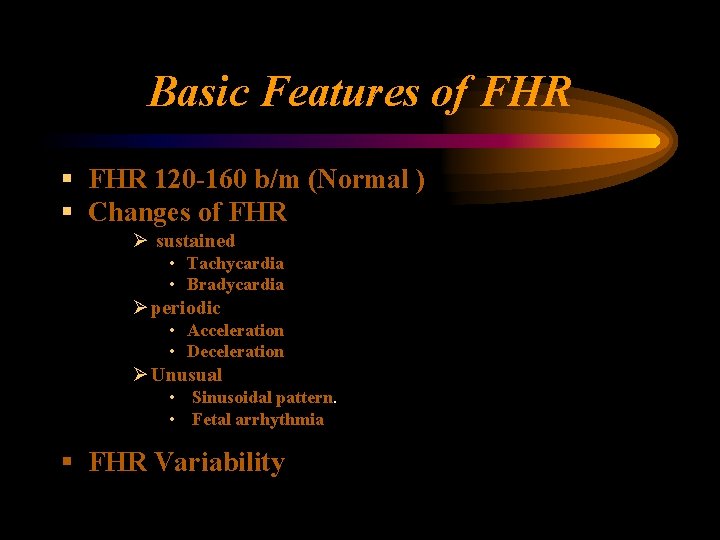
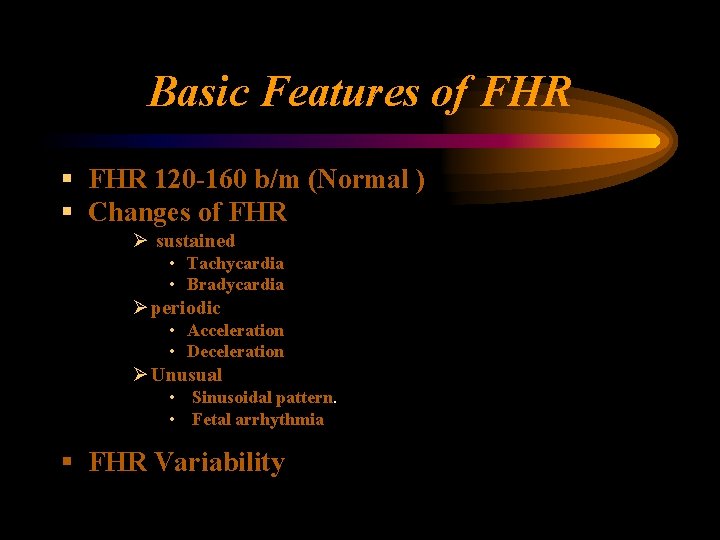
Basic Features of FHR § FHR 120 -160 b/m (Normal ) § Changes of FHR Ø sustained • Tachycardia • Bradycardia Ø periodic • Acceleration • Deceleration Ø Unusual • Sinusoidal pattern. • Fetal arrhythmia § FHR Variability
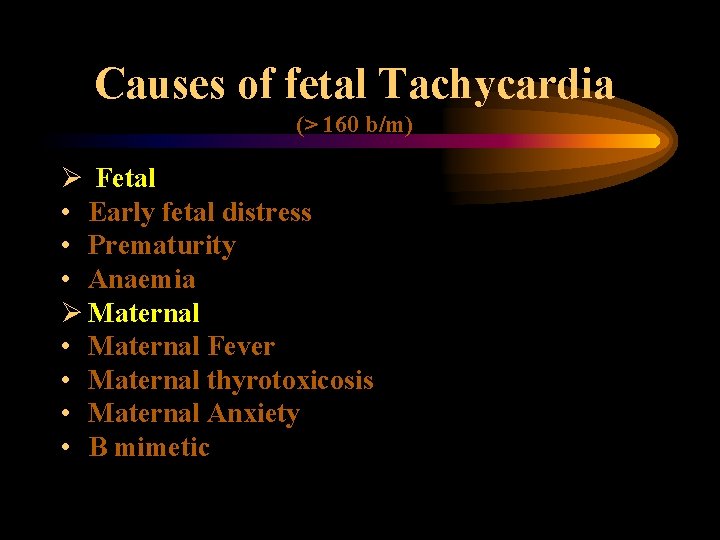
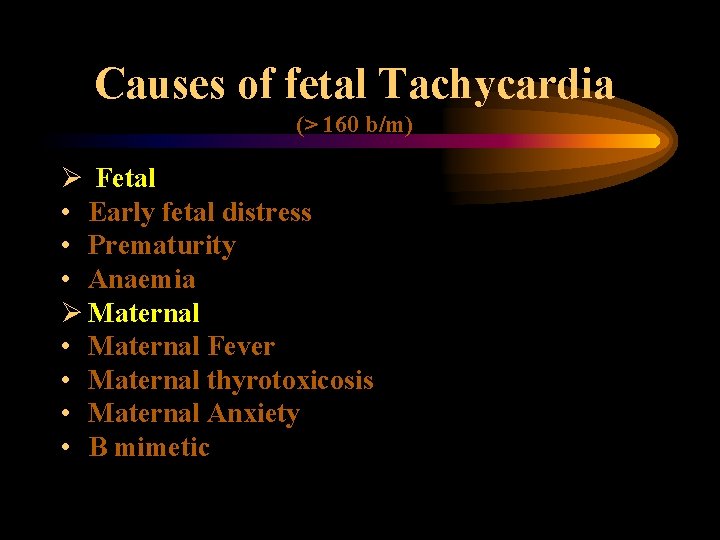
Tachycardia Causes of fetal Tachycardia (> 160 b/m) Ø Fetal • Early fetal distress • Prematurity • Anaemia Ø Maternal • Maternal Fever • Maternal thyrotoxicosis • Maternal Anxiety • B mimetic
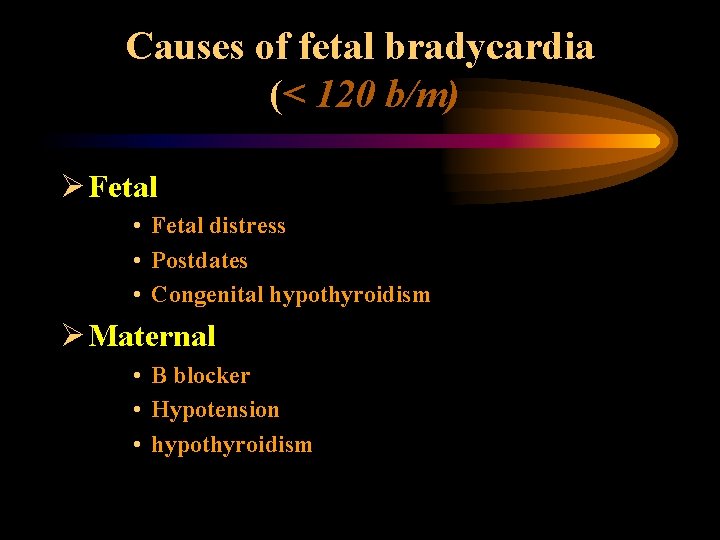
Causes of fetal bradycardia (< 120 b/m) Ø Fetal • Fetal distress • Postdates • Congenital hypothyroidism Ø Maternal • B blocker • Hypotension • hypothyroidism
Accelerations Acceleration is an abrupt increase in FHR 15 b/m last for > 15 second
Decelerations Deceleration is an abrupt decrease in FHR 15 b/m last for > 15 second
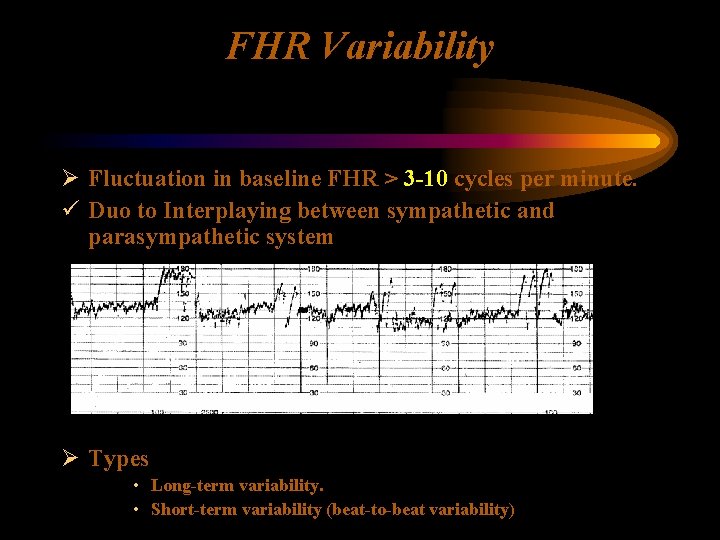
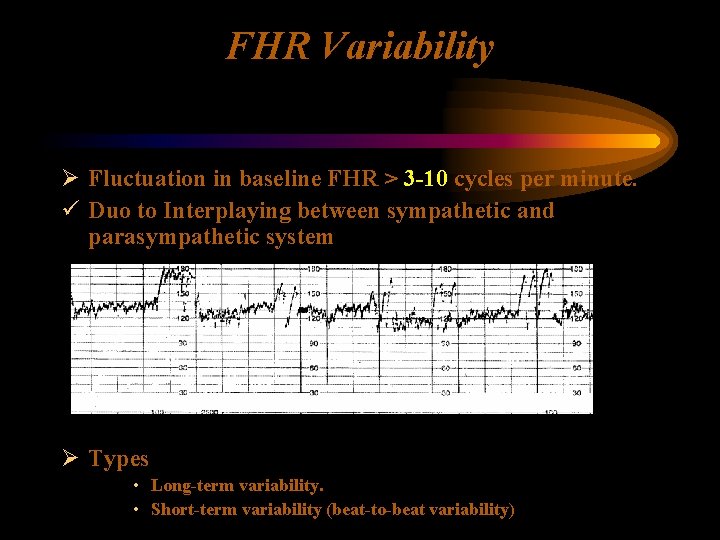
FHR Variability Ø Fluctuation in baseline FHR > 3 -10 cycles per minute. ü Duo to Interplaying between sympathetic and parasympathetic system Ø Types • Long-term variability. • Short-term variability (beat-to-beat variability)
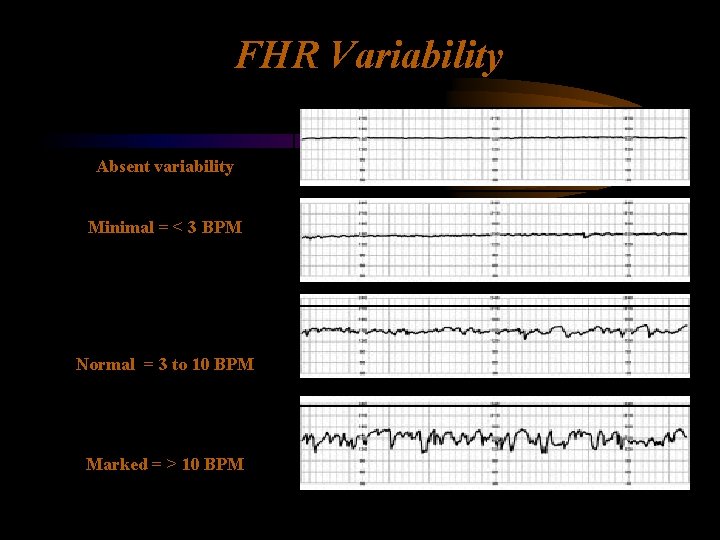
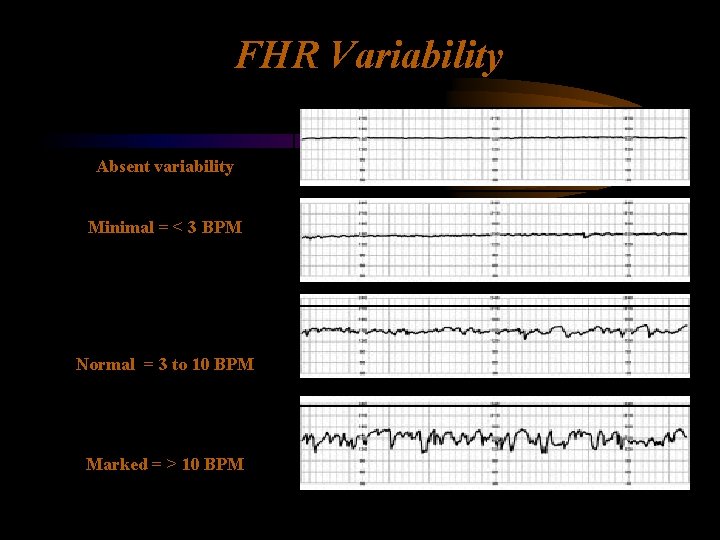
FHR Variability Absent variability Minimal = < 3 BPM Normal = 3 to 10 BPM Marked = > 10 BPM
FHR Variability Persistently minimal or absent FHR variability appears to be the most significant sign of fetal compromise.
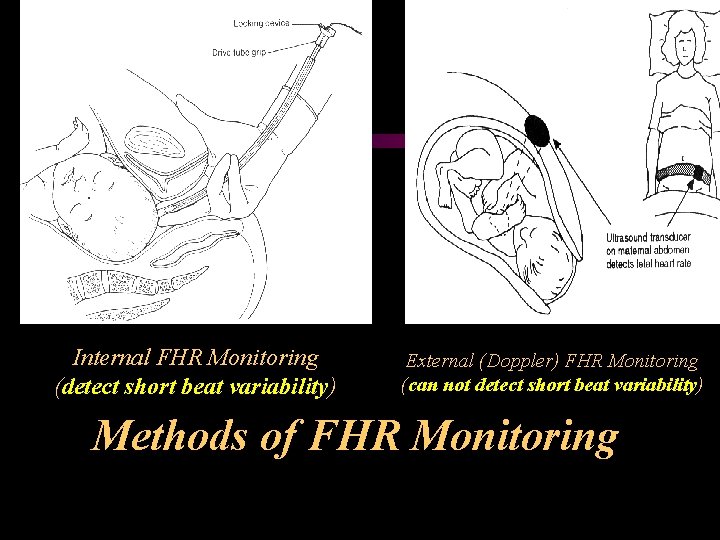
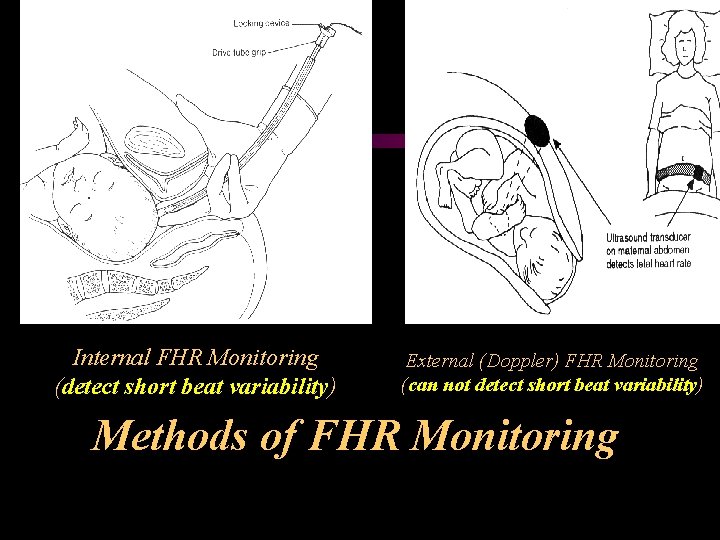
Internal FHR Monitoring (detect short beat variability) External (Doppler) FHR Monitoring (can not detect short beat variability) Methods of FHR Monitoring
Nonstress test (NST) Ø Definition The nonstress test (NST) is bioelectric test monitors FHR changes in relation to FM
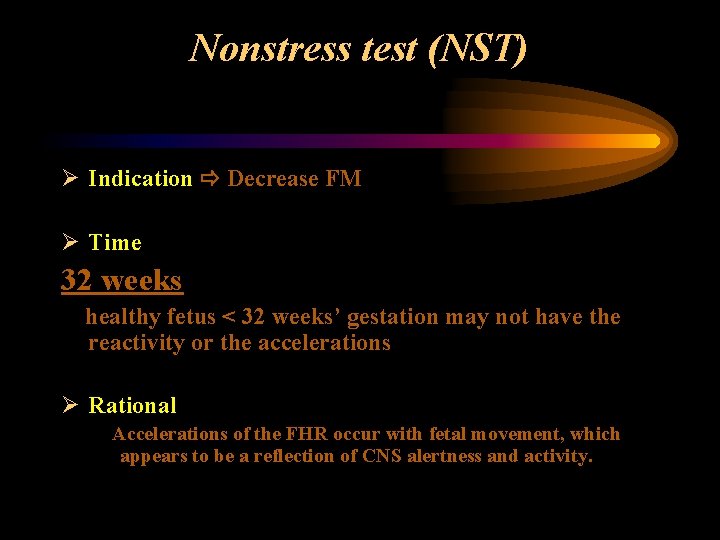
Nonstress test (NST) Ø Indication Decrease FM Ø Time 32 weeks healthy fetus < 32 weeks’ gestation may not have the reactivity or the accelerations Ø Rational Accelerations of the FHR occur with fetal movement, which appears to be a reflection of CNS alertness and activity.
Nonstress test (NST) Ø Technique – External monitors for contraction and FHR measurement applied. – Patient in left lateral tilt (to minimize supine hypotension). – Fetal movement is recorded.
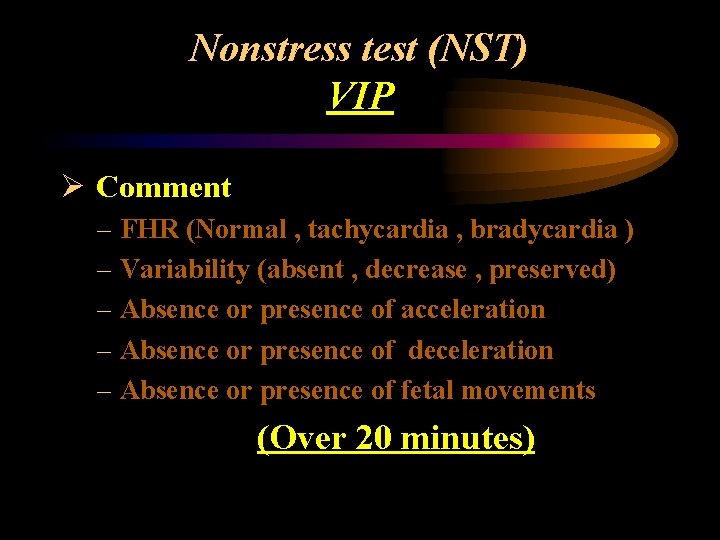
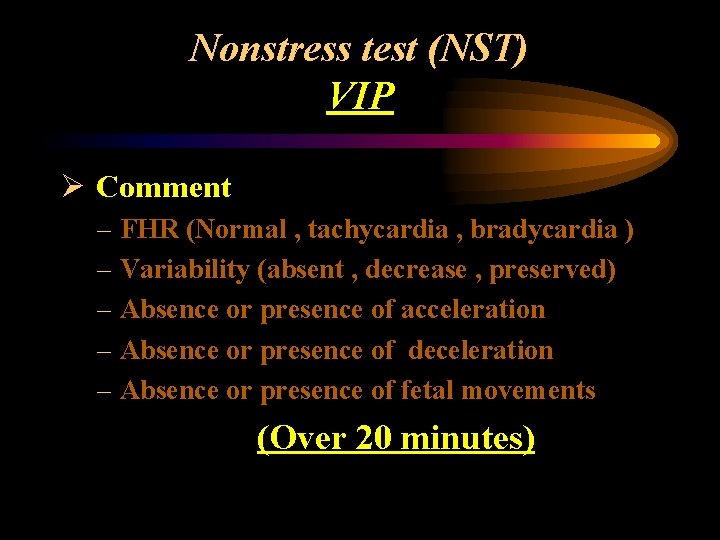
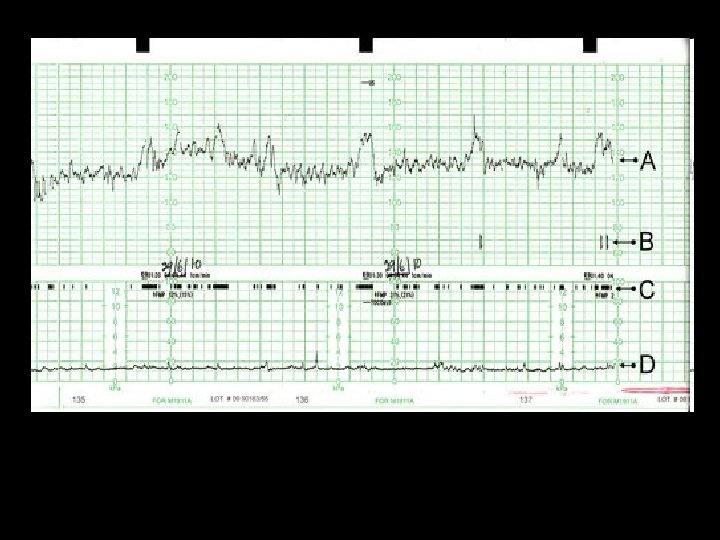
Nonstress test (NST) VIP Ø Comment – FHR (Normal , tachycardia , bradycardia ) – Variability (absent , decrease , preserved) – Absence or presence of acceleration – Absence or presence of deceleration – Absence or presence of fetal movements (Over 20 minutes)
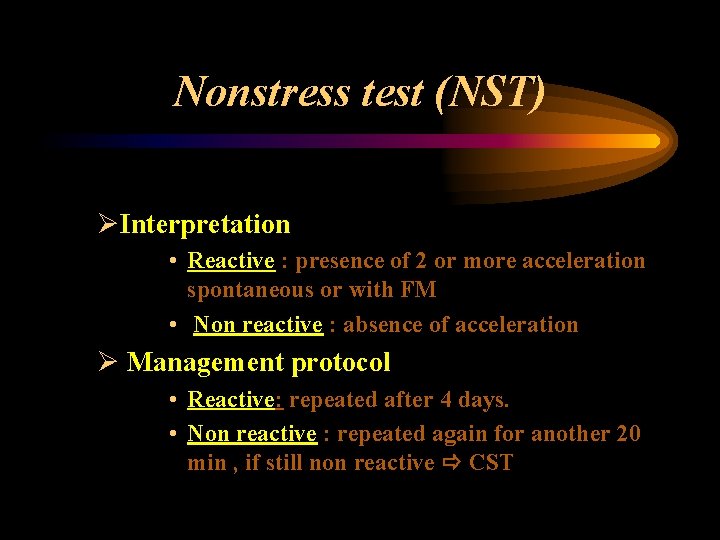
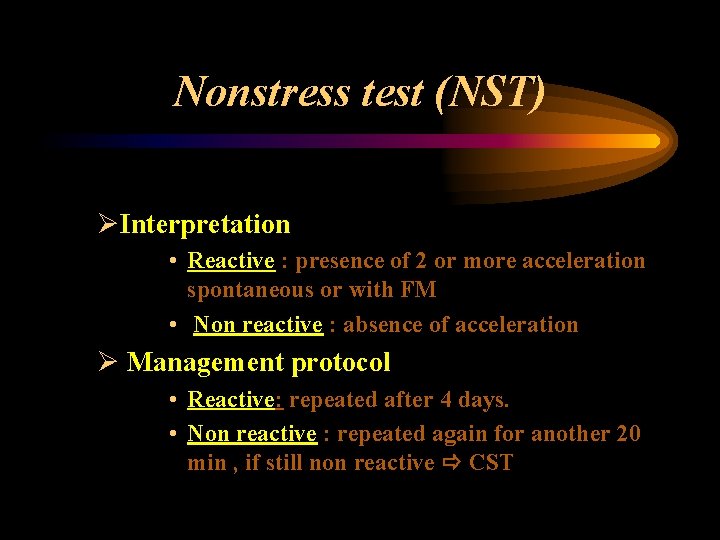
Nonstress test (NST) ØInterpretation • Reactive : presence of 2 or more acceleration spontaneous or with FM • Non reactive : absence of acceleration Ø Management protocol • Reactive: repeated after 4 days. • Non reactive : repeated again for another 20 min , if still non reactive CST
Nonstress test (NST) Ø Contraindications Absent
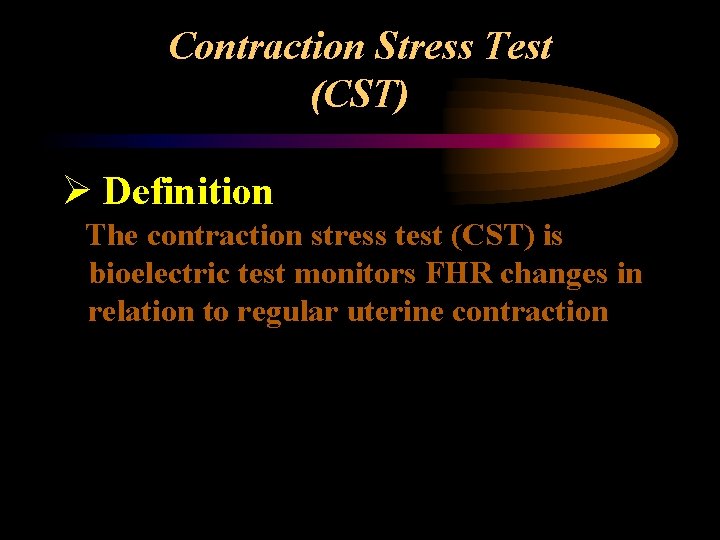
Contraction Stress Test (CST) Ø Definition The contraction stress test (CST) is bioelectric test monitors FHR changes in relation to regular uterine contraction
Contraction Stress Test (CST) Ø Indication Non reactive NST Ø Rational Uterine contraction Hypoxia (Normal fetus can tolerate)
Contraction Stress Test (CST) Ø Technique – External monitors for contraction and FHR measurement applied. – Patient in left lateral tilt. – Protocol for oxytocin infusion(o. 5 MIU/min) or breast stimulation(5 min). – Goal: three to five contractions in ten minutes.
Contraction Stress Test (CST) Ø Comment – FHR (Normal , tachycardia , bradycardia ) – Variability (absent , decrease , preserved) – Absence or presence of acceleration – Absence or presence of deceleration – Uterine contraction (adequate or not ) (≥ 10 minutes)
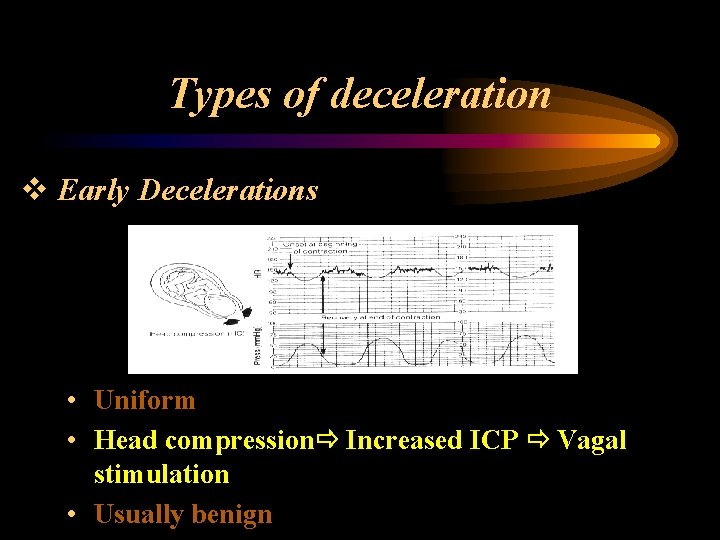
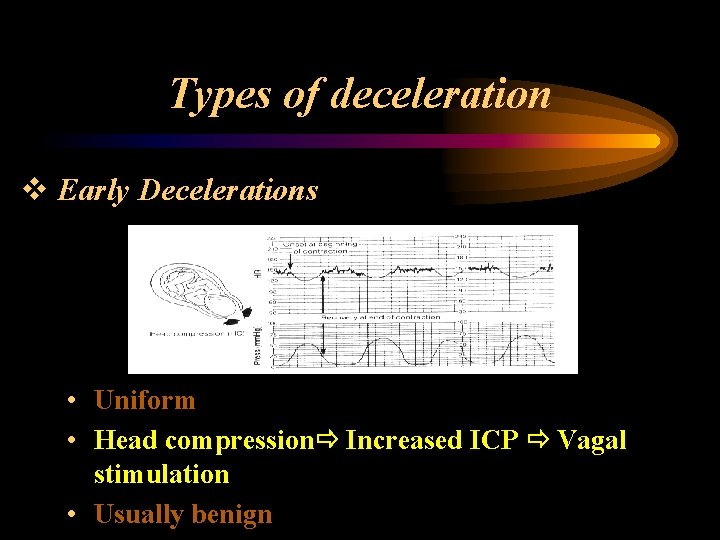
Types of deceleration v Early Decelerations • Uniform • Head compression Increased ICP Vagal stimulation • Usually benign
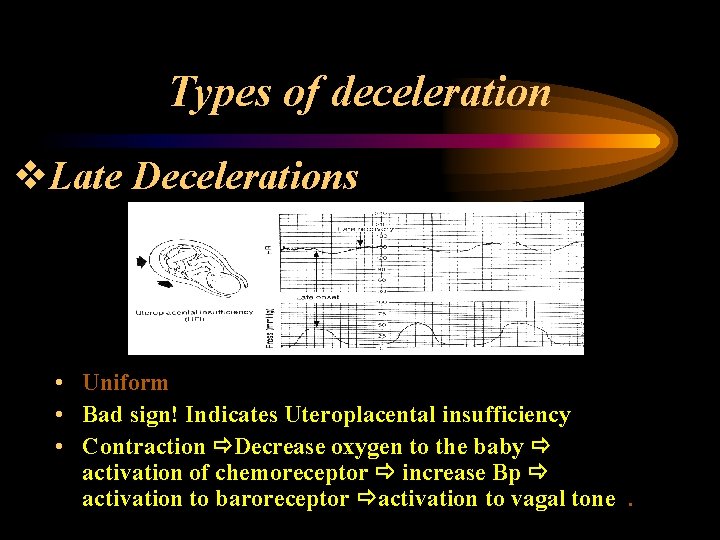
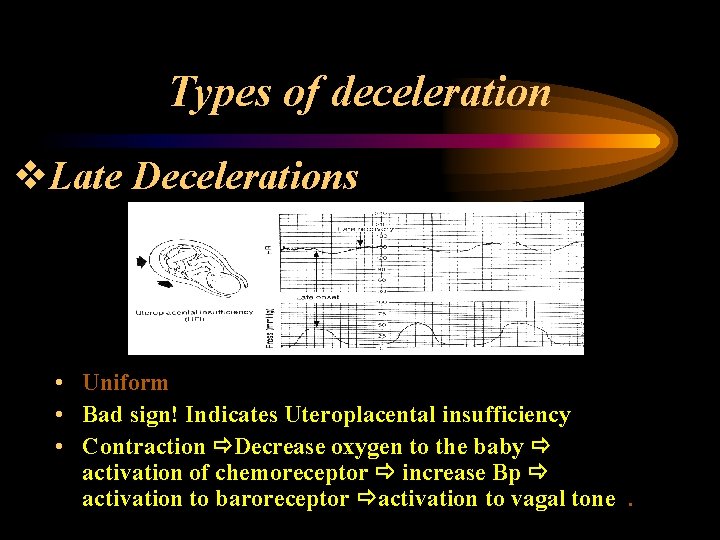
Types of deceleration v. Late Decelerations • Uniform • Bad sign! Indicates Uteroplacental insufficiency • Contraction Decrease oxygen to the baby activation of chemoreceptor increase Bp activation to baroreceptor activation to vagal tone.
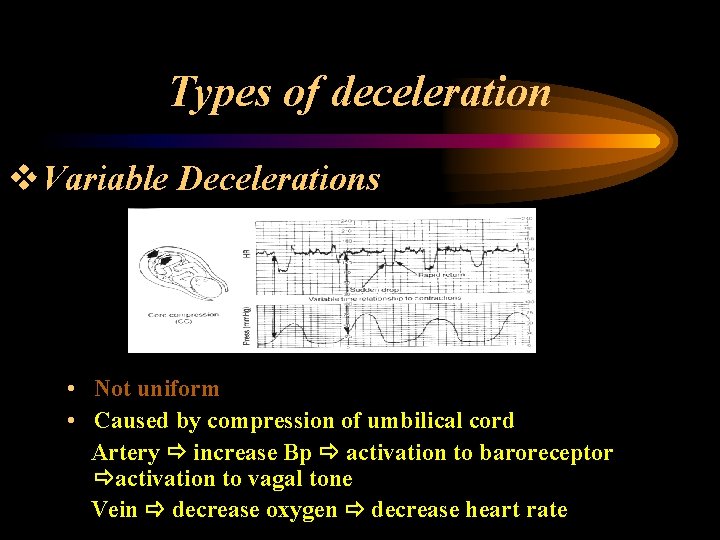
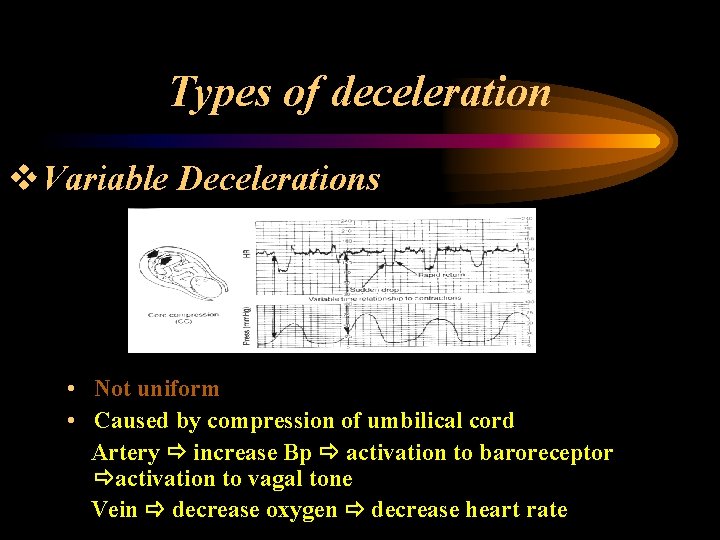
Types of deceleration v. Variable Decelerations • Not uniform • Caused by compression of umbilical cord Artery increase Bp activation to baroreceptor activation to vagal tone Vein decrease oxygen decrease heart rate
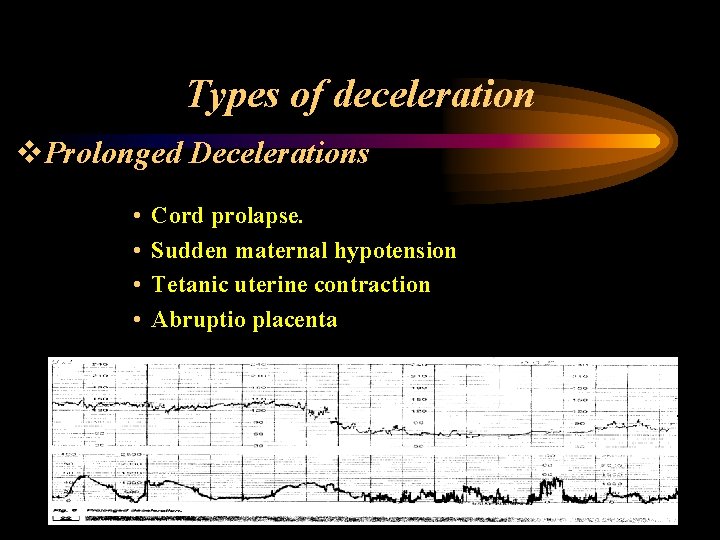
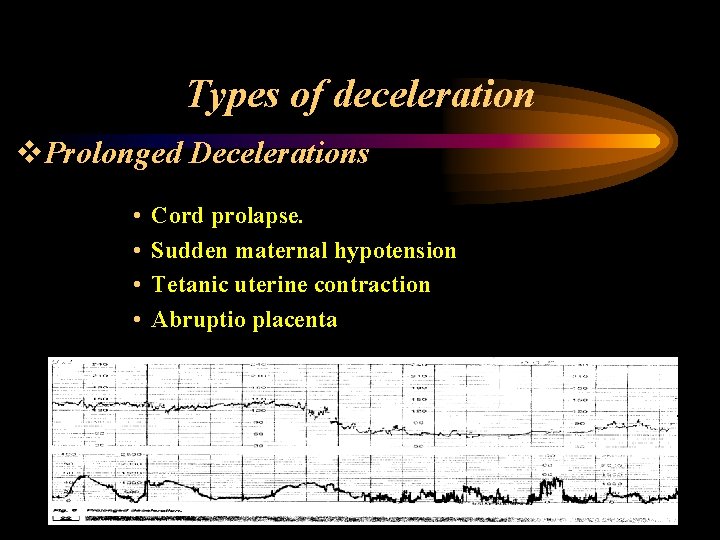
Types of deceleration v. Prolonged Decelerations • • Cord prolapse. Sudden maternal hypotension Tetanic uterine contraction Abruptio placenta
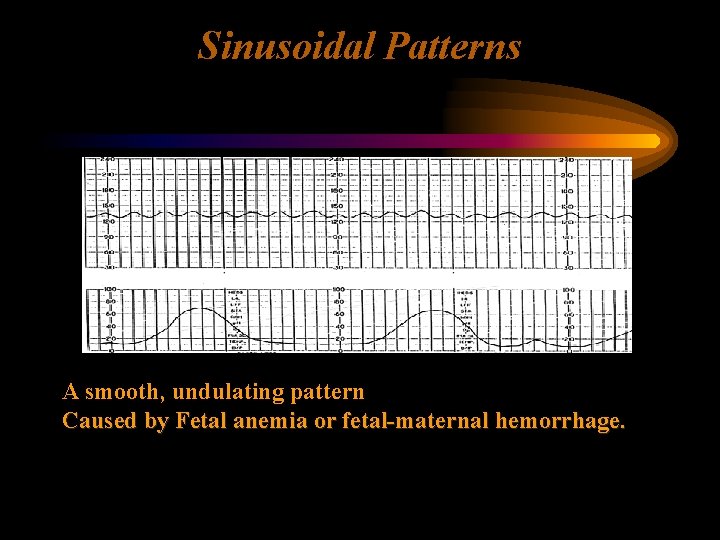
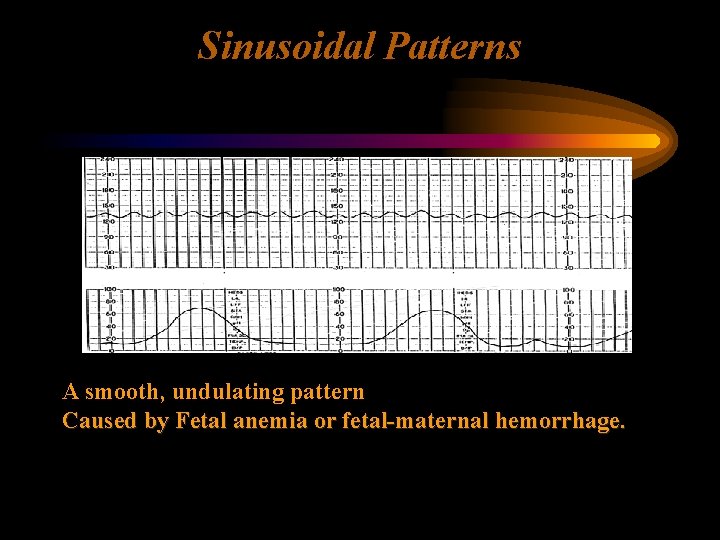
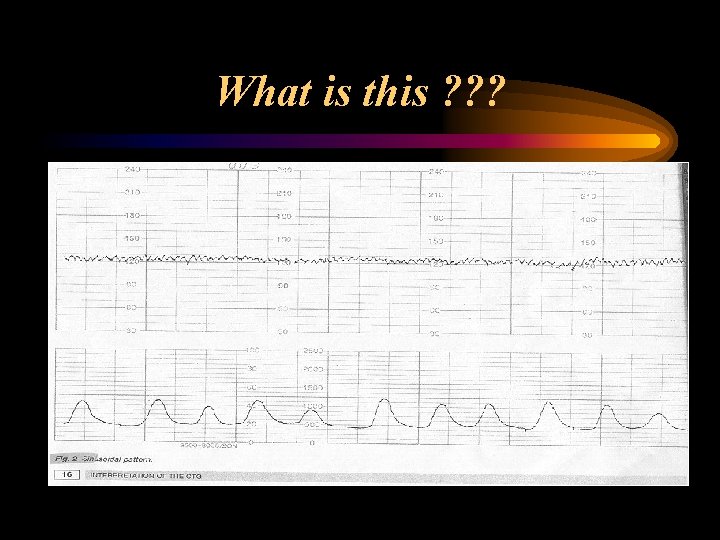
Sinusoidal Patterns A smooth, undulating pattern Caused by Fetal anemia or fetal-maternal hemorrhage.
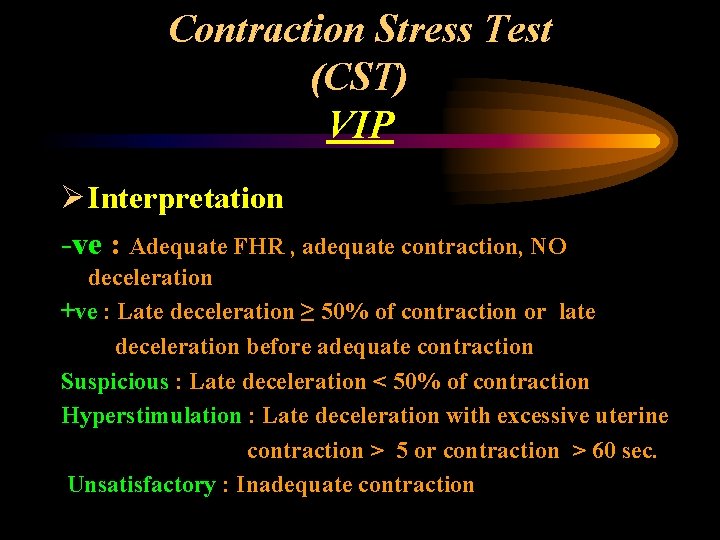
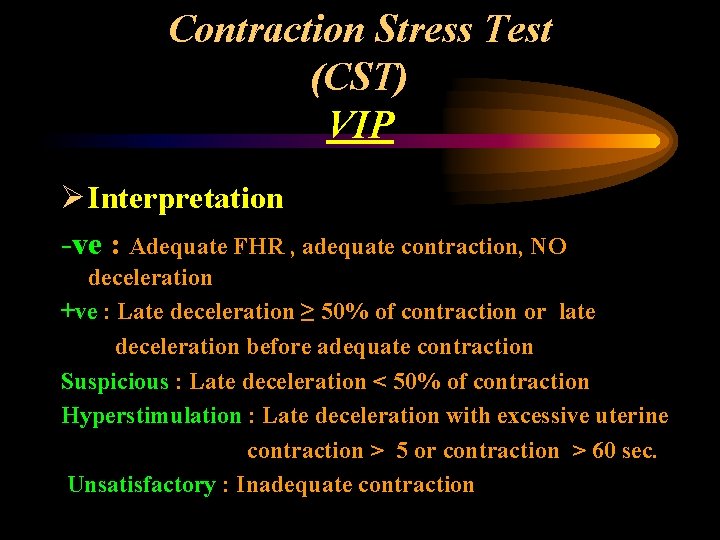
Contraction Stress Test (CST) VIP Ø Interpretation -ve : Adequate FHR , adequate contraction, NO deceleration +ve : Late deceleration ≥ 50% of contraction or late deceleration before adequate contraction Suspicious : Late deceleration < 50% of contraction Hyperstimulation : Late deceleration with excessive uterine contraction > 5 or contraction > 60 sec. Unsatisfactory : Inadequate contraction
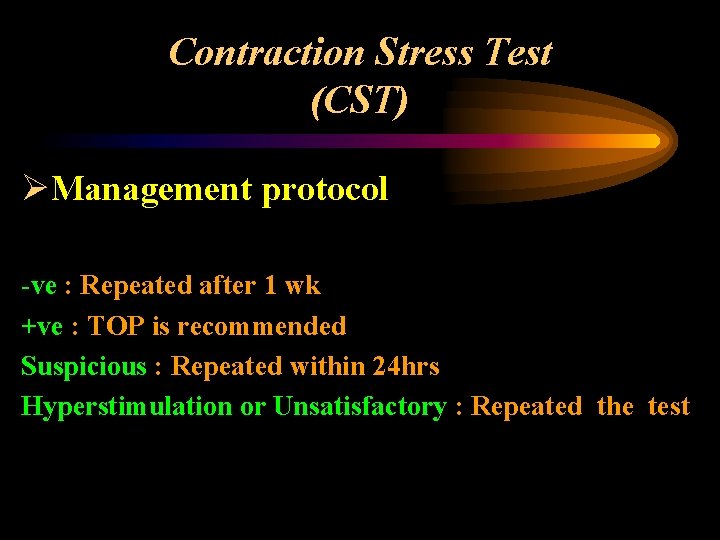
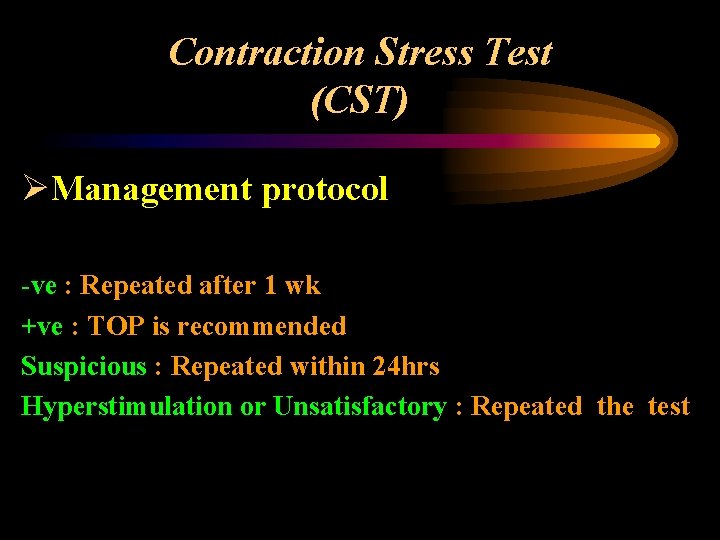
Contraction Stress Test (CST) ØManagement protocol -ve : Repeated after 1 wk +ve : TOP is recommended Suspicious : Repeated within 24 hrs Hyperstimulation or Unsatisfactory : Repeated the test
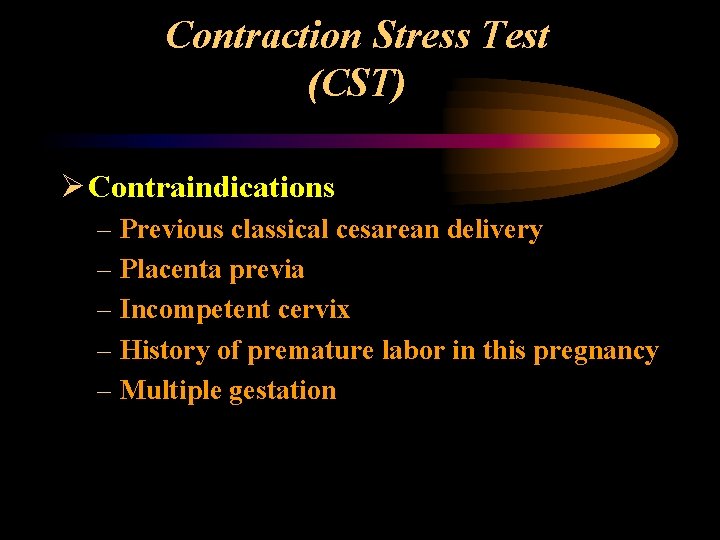
Contraction Stress Test (CST) Ø Contraindications – Previous classical cesarean delivery – Placenta previa – Incompetent cervix – History of premature labor in this pregnancy – Multiple gestation
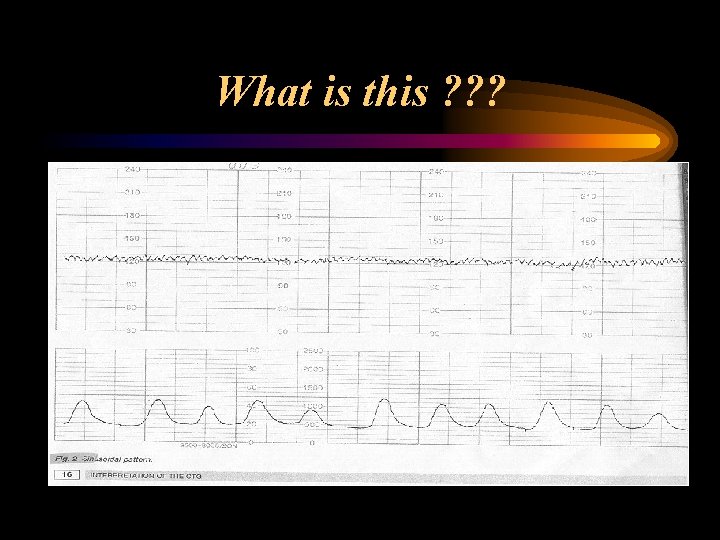
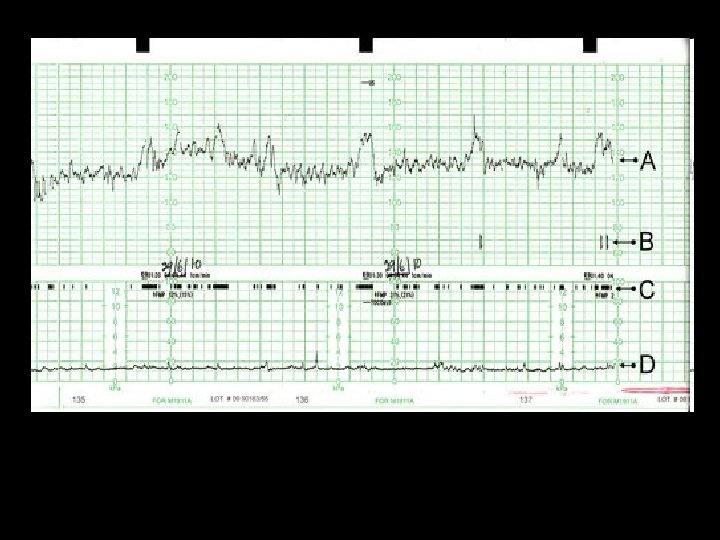
What is this ? ? ?
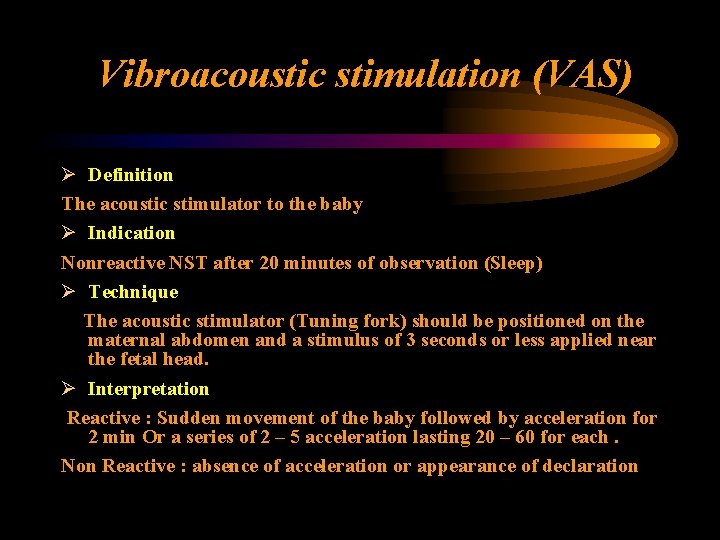
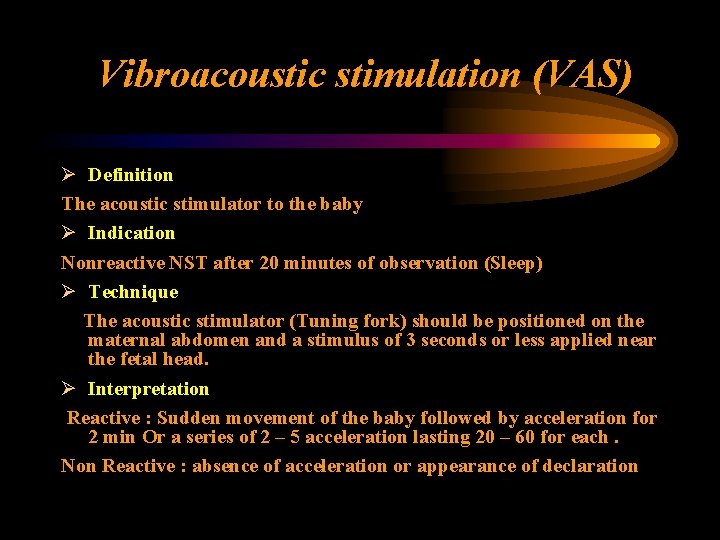
Vibroacoustic stimulation (VAS) Ø Definition The acoustic stimulator to the baby Ø Indication Nonreactive NST after 20 minutes of observation (Sleep) Ø Technique The acoustic stimulator (Tuning fork) should be positioned on the maternal abdomen and a stimulus of 3 seconds or less applied near the fetal head. Ø Interpretation Reactive : Sudden movement of the baby followed by acceleration for 2 min Or a series of 2 – 5 acceleration lasting 20 – 60 for each. Non Reactive : absence of acceleration or appearance of declaration
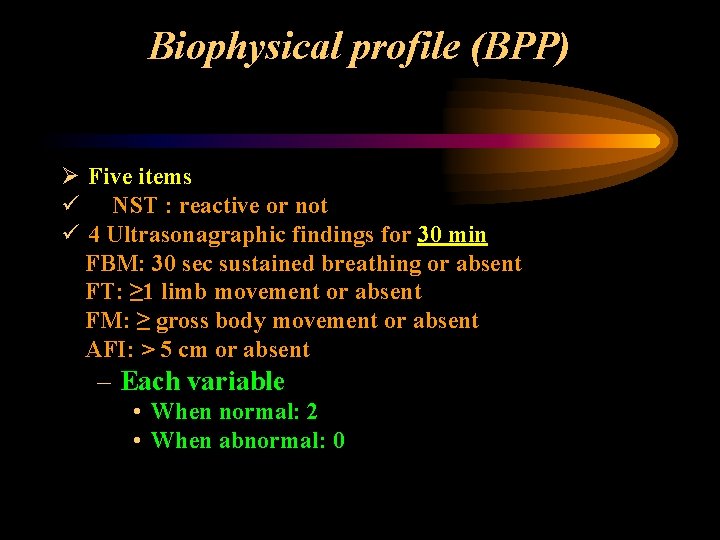
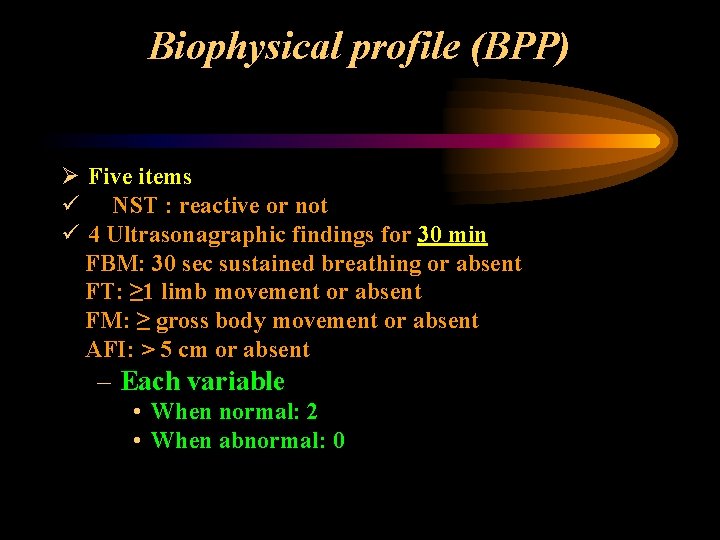
Biophysical profile (BPP) Ø Five items ü NST : reactive or not ü 4 Ultrasonagraphic findings for 30 min FBM: 30 sec sustained breathing or absent FT: ≥ 1 limb movement or absent FM: ≥ gross body movement or absent AFI: > 5 cm or absent – Each variable • When normal: 2 • When abnormal: 0
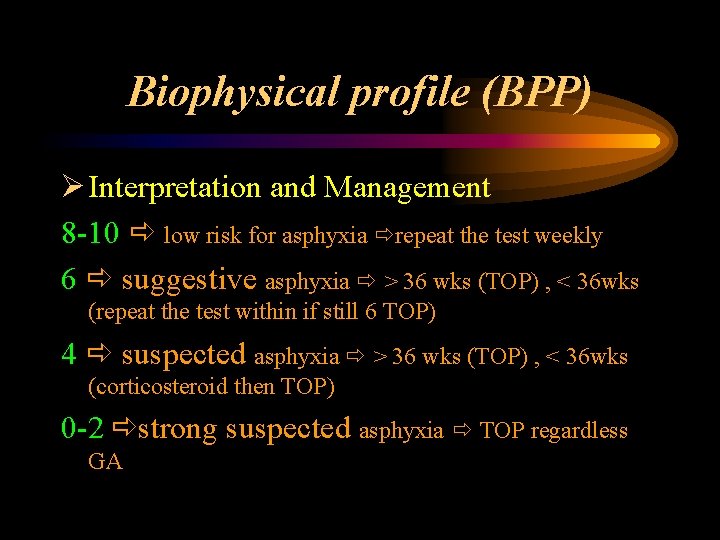
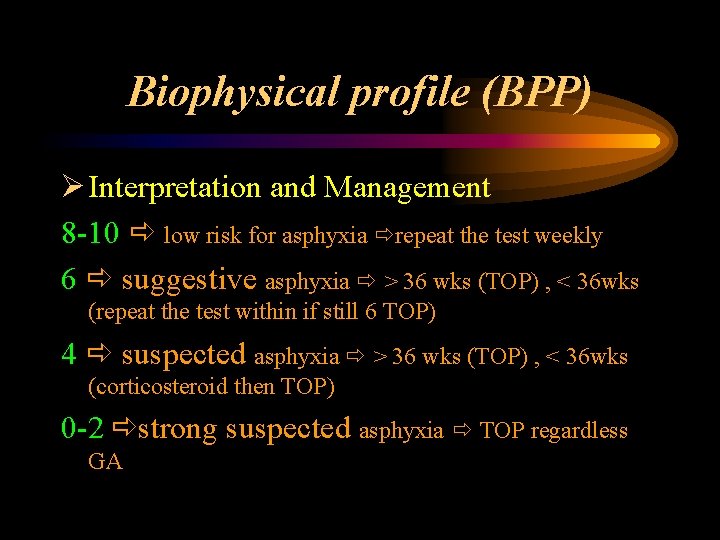
Biophysical profile (BPP) Ø Interpretation and Management 8 -10 low risk for asphyxia repeat the test weekly 6 suggestive asphyxia > 36 wks (TOP) , < 36 wks (repeat the test within if still 6 TOP) 4 suspected asphyxia > 36 wks (TOP) , < 36 wks (corticosteroid then TOP) 0 -2 strong suspected asphyxia TOP regardless GA
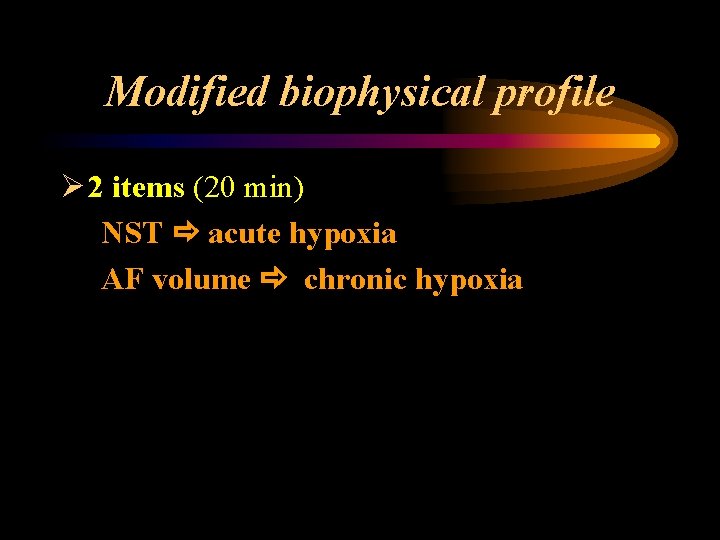
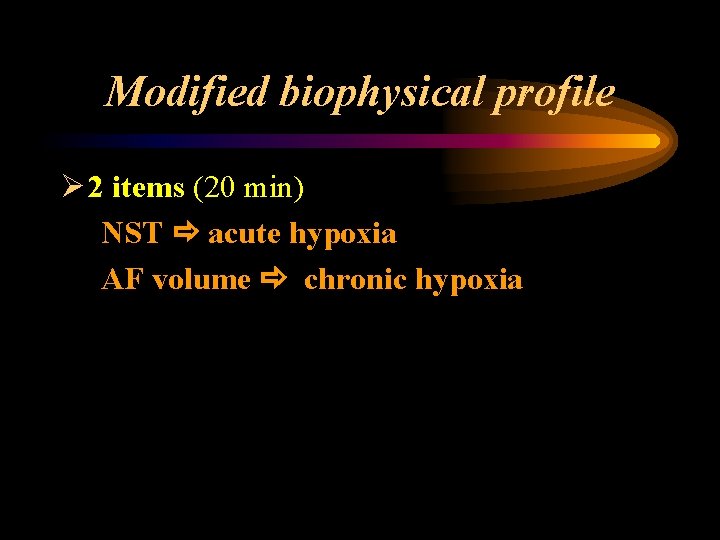
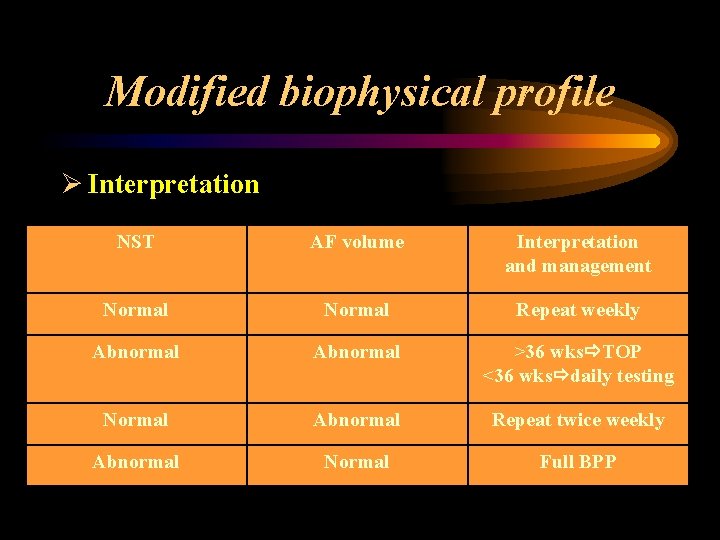
Modified biophysical profile Ø 2 items (20 min) NST acute hypoxia AF volume chronic hypoxia
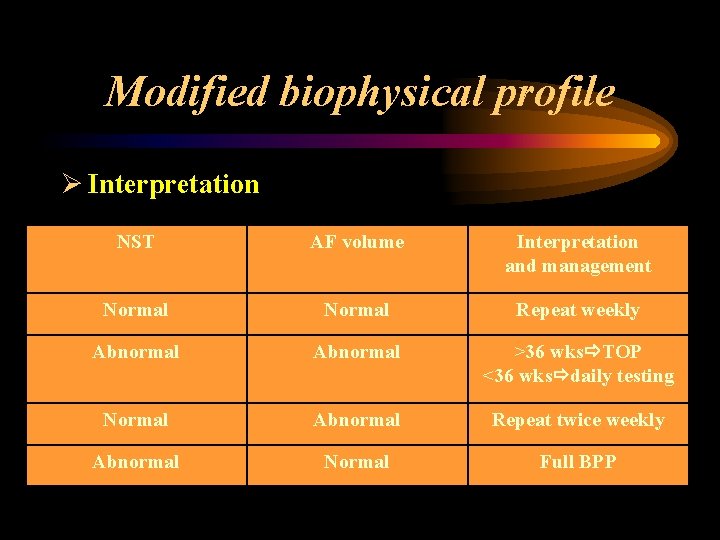
Modified biophysical profile Ø Interpretation NST AF volume Interpretation and management Normal Repeat weekly Abnormal >36 wks TOP <36 wks daily testing Normal Abnormal Repeat twice weekly Abnormal Normal Full BPP
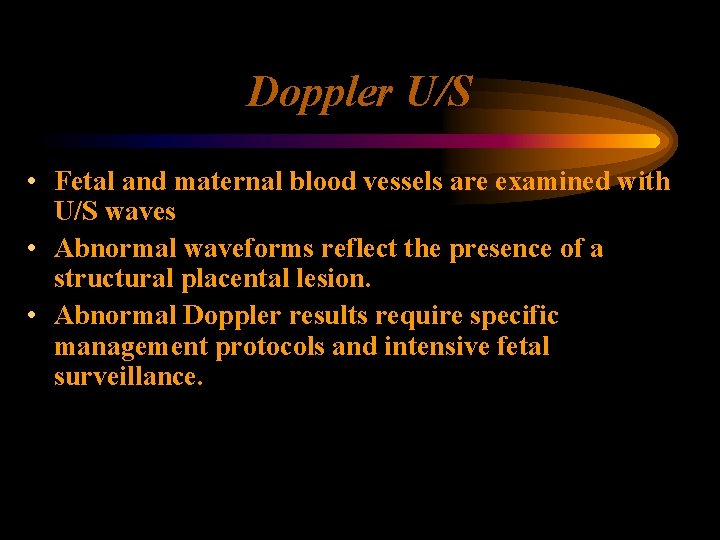
Doppler U/S • Fetal and maternal blood vessels are examined with U/S waves • Abnormal waveforms reflect the presence of a structural placental lesion. • Abnormal Doppler results require specific management protocols and intensive fetal surveillance.
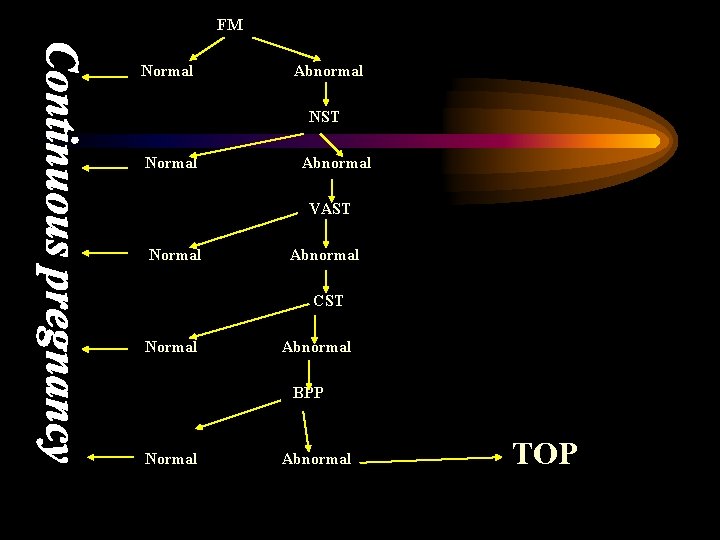
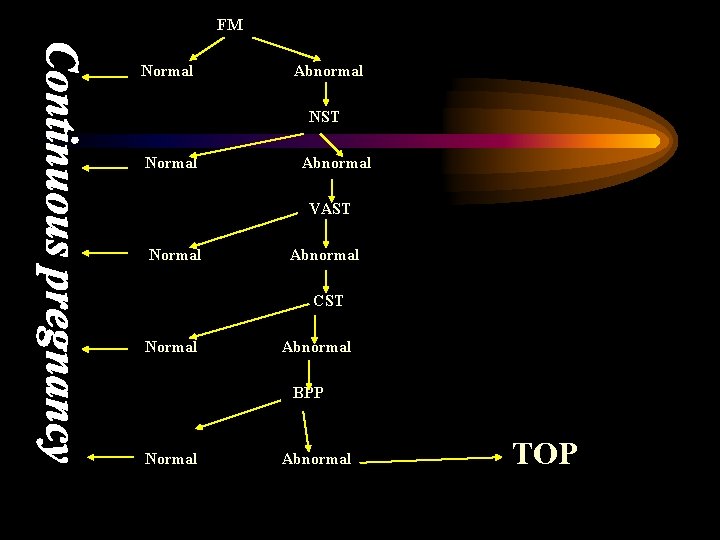
FM Normal Abnormal NST Normal Abnormal VAST Normal Abnormal CST Normal Abnormal BPP Normal Abnormal TOP

Thank you